Abstract
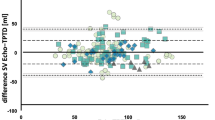
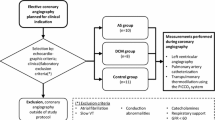
Measurement of the global end-diastolic volume index (GEDI) by transpulmonary thermodilution (TPTD) has become a useful technique for measuring preload in adults. This study aimed to investigate the hemodynamic changes in neonates during the postoperative period after arterial switch surgery. Over a 13-month period, the postoperative data of 12 neonates with transposition of the great arteries were retrospectively investigated. Arterial and central venous blood pressures were monitored, Cardiac index (CI), stroke volume index (SVI), systemic vascular resistance index (SVRI), GEDI, and extravascular lung water index (ELWI) were measured by thermodilution. The CI was significantly correlated with the SVRI only in the closed chest condition (r = −0.92; P < 0.001). The CI and SVI values were significantly lower and the ELWI and SVRI values significantly higher in both the open and closed chest conditions than the postextubation values. The relationship between change in GEDI and change in CI was stronger in the open chest condition (r = 0.93; P < 0.006) than in the closed chest condition (r = 0.75; P = 0.055). However, the latter just missed statistical significance. According to the findings, TPTD seems to be a useful tool for assessing cardiac function after neonatal arterial switch surgery. Establishment of normal values will be essential for proper guidance of therapy for this population using volumetric parameters.
Similar content being viewed by others
References
Bland JM, Altman DG (1995) Calculating correlation coefficients with repeated observations. Part 2: correlation between subjects. BMJ 310:633
Cecchetti C, Lubrano R, Cristaldi S, Stoppa F, Barbieri MA, Elli M, Masciangelo R, Perrotta D, Travasso E, Raggi C, Marano M, Pirozzi N (2008) Relationship between global end-diastolic volume and cardiac output in critically ill infants and children. Crit Care Med 36:928–932
Egan JR, Festa M, Cole AD, Nunn GR, Gillis J, Winlaw DS (2005) Clinical assessment of cardiac performance in infants and children following cardiac surgery. Intensive Care Med 4:568–573
Fakler U, Pauli Ch, Balling G, Lorenz HP, Eicken A, Hennig M, Hess J (2007) Cardiac index monitoring by pulse contour analysis and thermodilution after pediatric cardiac surgery. J Thorac Cardiovasc Surg 133:224–228
Goedje O, Peyerl M, Seebauer T, Lamm P, Mair H, Reichart B (1998) Central venous pressure, pulmonary capillary wedge pressure, and intrathoracic blood volumes as preload indicators in cardiac surgery patients. Eur J Cardiothorac Surg 13:533–539
Goepfert MS, Reuter DA, Akyol D, Lamm P, Kilger E, Goetz A (2007) Goal-directed fluid management reduces vasopressor and catecholamine use in cardiac surgery patients. Intensive Care Med 33:96–103
Hazinski MF (1999) Cardiovascular disorders. In: Hazinski MF, Bowlus BJ (eds) The manual of pediatric critical care, 1st edn. CV Mosby, St. Louis, pp 112, 284–288
Hoffman TM, Wernovsky G, Atz AM, Bailey JM, Akbary A, Kocsis JF, Nelson DP, Chang AC, Kulik TJ, Spray TL, Wessel DL (2002) Prophylactic intravenous use of milrinone after cardiac operation in pediatrics (PRIMACORP) study. Prophylactic Intravenous Use of Milrinone After Cardiac Operation in Pediatrics. Am Heart J 143:15–21
Laussen PC, Roth SJ (2003) Fast tracking: efficiently moving patients through the intensive care unit. Progr Ped Cardiol 18:149–158
López-Herce J, Rupérez M, Sánchez C, García C, García E (2006) Estimation of the parameters of cardiac function and of blood volume by arterial thermodilution in an infant animal model. Pediatr Anesth 16:635–640
Mahajan A, Shabanie A, Turner J, Sopher MJ, Marijic J (2003) Pulse contour analysis for cardiac output monitoring in cardiac surgery for congenital heart disease. Anesth Analg 97:1283–1288
Meissner U, Scharf J, Dötsch J, Schroth M (2008) Very early extubation after open-heart surgery in children does not influence cardiac function. Pediatr Cardiol. 29:317–320
Michard F (2007) Bedside assessment of extravascular lung water by dilution methods: temptations and pitfalls. Crit Care Med 35:1186–1192
Michard F, Alaja S, Zarka V, Bahloul M, Richard C, Teboul JL (2003) Global end diastolic volume as an indicator of cardiac preload in patients with septic shock. Chest 124:1900–1908
Miller-Hoover SR (2003) Pediatric and neonatal cardiovascular pharmacology. Pediatr Nurs 29:105–113
Mupanemunda RH (2006) Cardiovascular support of the sick neonate. Curr Pediatr 16:176–181
Noori S, Seri I (2005) Pathophysiology of newborn hypotension outside the transitional period. Early Hum Dev 81:399–404
Ravishankar C, Tabbutt S, Wernovsky G (2003) Critical care in cardiovascular medicine. Curr Opin Pediatr 15:443–453
Renner J, Cavus E, Meybohm P, Gruenewald M, Steinfath M, Scholz J, Boening A, Bein B (2008) Pulse pressure variation and stroke volume variation during different loading conditions in a paediatric animal model. Acta Anaesthesiol Scand 52:374–380
Rupérez M, López-Herce J, García C, Sánchez C, García E, Vigil D (2004) Comparison between cardiac output measured by the pulmonary arterial thermodilution technique and that measured by the femoral arterial thermodilution technique in a pediatric animal model. Pediatr Cardiol 25:119–123
Schiffmann H, Erdlenbruch B, Singer D, Singer S, Herting E, Hoeft A, Buhre W (2002) Assessment of cardiac output, intravascular volume status, and extravascular lung water by transpulmonary indicator dilution in critically ill neonates and infants. J Cardiothorac Vasc Anesth 16:592–599
Skowno JJ, Broadhead M (2008) Cardiac output measurement in pediatric anesthesia. Paediatr Anaesth 18:1019–1028
Smetkin AA, Kirov MY, Kuzkov VV, Lenkin AI, Eremeev AV, Slastilin VY, Borodin VV, Bjertnaes LJ (2009) Single transpulmonary thermodilution and continuous monitoring of central venous oxygen saturation during off-pump coronary surgery. Acta Anaesthesiol Scand 53:505–514
Tibby SM, Murdoch IA (2003) Monitoring cardiac function in intensive care. Arch Dis Child 88:46–52
Tibby SM, Hatherill M, Marsh MJ, Wilson P, Postle AD, Murdoch IA (1997) Clinical validation of cardiac output measurements using femoral artery thermodilution with direct Fick in ventilated children and infants. Intensive Care Med 23:987–991
Tibby SM, Hatherill M, Marsh MJ, Murdoch IA (2003) Clinicians’ abilities to estimate cardiac index in ventilated children and infants. Arch Dis Child 77:516–518
Wernovsky G, Wypij D, Jonas RA, Mayer JE Jr, Hanley FL, Hickey PR, Walsh AZ, Chang AC, Castañeda AR, Newburger JW (1995) Postoperative course and hemodynamic profile after arterial switch operation in neonates and infants. Circulation 92:2226–2235
Acknowledgments
This study was supported by grants from the Hungarian Research Foundation (OTKA-T-035169), Budapest, Hungary; the Academy of Finland, Helsinki, Finland; Biocenter Oulu, Oulu, Finland; and the Sigrid Juselius Foundation, Helsinki, Finland. No conflict of interest exists.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Székely, A., Breuer, T., Sápi, E. et al. Transpulmonary Thermodilution in Neonates Undergoing Arterial Switch Surgery. Pediatr Cardiol 32, 125–130 (2011). https://doi.org/10.1007/s00246-010-9828-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-010-9828-0