Abstract
Objective
To compare clinical assessment of cardiac performance with an invasive method of haemodynamic monitoring.
Design and setting
Prospective observational study in a 16-bed tertiary paediatric intensive care unit.
Patients and participants
Infants and children undergoing cardiopulmonary bypass and surgical repair of congenital heart lesions.
Interventions
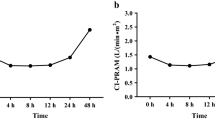
Based on physical examination and routinely available haemodynamic monitoring in the paediatric intensive care unit, medical and nursing staff assessed cardiac index, systemic vascular resistance index and volume status. Clinical assessment was compared with cardiac index, systemic vascular resistance index and global end diastolic volume index, obtained by femoral artery thermodilution.
Measurements and results
A total of 76 clinical estimations of the three parameters were made in 16 infants and children undergoing biventricular repair of congenital heart lesions. Agreement was poor between clinical and invasive methods of determining all three studied parameters of cardiac performance. Cardiac index was significantly underestimated clinically; mean difference was 0.71 l min−1 m−2 (95% range of agreement ±2.7). Clinical estimates of systemic vascular resistance (weighted κ=0.15) and volume status (weighted κ=0.04) showed poor levels of agreement with measured values and were overestimated clinically. There was one complication related to a femoral arterial catheter and one device failure.
Conclusions
Routine clinical assessment of parameters of cardiac performance agreed poorly with invasive determinations of these indices. Management decisions based on inaccurate clinical assessments may be detrimental to patients. Invasive haemodynamic monitoring using femoral artery thermodilution warrants cautious further evaluation as there is little agreement with clinical assessment which is presently standard accepted care in this patient population.




Similar content being viewed by others
References
Hoffman TM, Wernovsky G, Atz AM, Kulik TJ, Nelson DP, Chang AC, Bailey JM, Akbary A, Kocsis JF, Kaczmarek R, Spray TL, Wessel DL (2003) Efficacy and safety of milrinone in preventing low cardiac output syndrome in infants and children after corrective surgery for congenital heart disease. Circulation 107:996–1002
Tibby SM, Hatherill M, Marsh MJ, Murdoch IA (1997) Clinicians’ abilities to estimate cardiac index in ventilated children and infants. Arch Dis Child 77:516–518
Tibby SM, Hatherill M, Marsh MJ, Morrison G, Anderson D, Murdoch IA (1997) Clinical validation of cardiac output measurements using femoral artery thermodilution with direct Fick in ventilated children and infants. Intensive Care Med 23:987–991
Shann F (2001) Drug doses, 11th edn. Collective
Schiffmann H, Erdlenbruch B, Singer D, Singer S, Herting E, Hoeft A, Buhre W (2002) Assessment of cardiac output, intravascular volume status and extravascular lung water by transpulmonary indicator dilution in critically ill neonates and infants. J Cardiothorac Vasc Anesth 16:592–597
Michard F, Alaya S, Zarka V, Bahloul M, Richard C, Teboul JL (2003) Global end-diastolic volume as an indicator of cardiac preload in patients with septic shock. Chest 124:1900–1908
Kozlik-Feldmann R, Konert M, Freund M, Netz H (1998) Normal values for distribution volumes of less invasive circulation monitoring by double indicator measurement in paediatric intensive care. Z Kardiol 87:762
Sakka SG, Ruhl CC, Pfeiffer UJ, Beale R, McLuckie A, Reinhart K, Meier-Hellmann A (2000) Assessment of cardiac preload and extravascular lung water by single transpulmonary thermodilution. Intensive Care Med 26:180–187
Peat J, Mellis C, Williams K, Xuan W (2001) Health science research: a handbook of quantitative methods. Allen and Unwin, Crows Nest–
Pauli C, Fakler U, Genz T, Hennig M, Lorenz H-P, Hess J (2002) Cardiac output determination in children: equivalence of the transpulmonary thermodilution method to the direct Fick principle. Intensive Care Med 28:947–952
Ravishankar C, Tabbutt S, Wernovsky G (2003) Critical care in cardiovascular medicine. Curr Opin Pediatr 15:443–453
Richard C, Warszawski J, Anguel N, Deye N, Combes A. Harnottd D, Boulain T, Lefort Y, Fartoukh M, Baud F, Boyer A, Brochard L, Teboul J-L (2003) Early use of the pulmonary artery catheter and outcomes in patients with septic shock and acute respiratory distress syndrome. JAMA 290:2713–2720
Fowler RA, Cook DJ (2003) The arc of the pulmonary artery catheter. JAMA 290:2732–2734
Sandham JD, Hull RD, Brant RF, Knox L, Pineo GF, Doig CJ, Laporta DP, Viner S, Passerini L, Devitt H, Kirby A, Jacka M (2003) A randomized, controlled trial of the use of pulmonary-artery catheters in high-risk surgical patients. N Engl J Med 348:5–14
Morgan TJ (2004) Life without the PA catheter. Crit Care Resuscitation 6:9–12
Tibby SM, Hatherill M, Murdoch IA (1999) Capillary refill and core-peripheral temperature gap as indicators of haemodynamic status in paediatric intensive care patients. Arch Dis Child 80:163–166
Butt W, Shann F (1991) Core-peripheral temperature gradient does not predict cardiac output or systemic vascular resistance in children. Anaesth Intensive Care 19:84–87
Smith-Wright DL, Thomas PG, Lock JE, Egar MI, Fuhrman BP (1984) Complications of vascular catheterization in critically ill children. Crit Care Med 12:1015–1017
Egan J, Festa M, Winlaw D, Cole A, Gillis J, Nunn G (2003) Comparison of clinical and invasive assessments of cardiac performance following paediatric cardiac surgery. Pediatr Crit Care Med 4 [Suppl]:A101
Acknowledgements
These findings were previously presented at the 4th World Congress of Pediatric Intensive Care, 8–12 June 2003, Boston, USA [19].
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Egan, J.R., Festa, M., Cole, A.D. et al. Clinical assessment of cardiac performance in infants and children following cardiac surgery. Intensive Care Med 31, 568–573 (2005). https://doi.org/10.1007/s00134-005-2569-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-005-2569-5