Abstract
Background
Adult fibrosarcoma (AFS) is a very rare malignant soft tissue tumor, arising from malignant spindle-shaped fibroblasts. We aim to analyze the appearance of recurrent AFS with a focus on configuration and to assess the occurrence of loco-regional post-treatment changes on MRI follow-up.
Methods
One hundred sixty-eight MRI follow-up scans (1.5 T MRI) of 12 patients with histologically proven AFS were reviewed. The recurrent tumors were examined for configuration, limitation, contrast enhancement, and extent and signal intensity on MRI.
Results
The mean age of the patients was 50.2 ± 16.7 years. Forty-two percent of the patients presented recurrent AFS (n = 5). Recurrences occurred 12 ± 6.5 months after tumor resection in the mean. Patients over 55 years of age showed a significantly higher risk for recurrences (RR = 5; 95% CI, 1.8 to 31; p = 0.04). Recurrent AFS was ovoid, nodular, streaky, polycyclic, or fascicular configured with homogeneous/heterogeneous contrast enhancement and well- or ill-defined borders. The intensity of contrast enhancement ranged from rim to marked contrast enhancement. Recurrent AFS mostly showed a muscle iso-intense signal in T1-weighted and a hyperintense signal in PD-weighted/TIRM sequences. The most common post-treatment changes were subcutaneous edema (92%; p = 0.03), muscle edema (75%), and postoperative seroma (50%). Patients with the presence of muscle edema after primary tumor resection had a slightly, but not significantly higher risk for recurrences (RR = 1.75; p = 0.08).
Conclusion
Recurrent AFS shows no common configuration on MRI, as it may appear ovoid, nodular, streaky, polycyclic, or fascicular. Patients with the presence of post-treatment muscle edema have a slightly higher risk for recurrences.
Level of evidence: Level III, therapeutic study
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Adult fibrosarcoma (AFS) is a very rare malignant soft tissue tumor, arising from malignant spindle-shaped fibroblasts [1, 2]. Once AFS was considered to be the most common soft tissue sarcoma in adults [2, 3], but nowadays, AFS counts for only about 1–3.6% of all soft tissue sarcomas in adults according to recent surveys [2, 4, 5]. AFS mostly occurs in the deep soft tissues and is mostly located in the trunk and the extremities [2, 6]. AFS has to be distinguished from the infant type of fibrosarcoma, which occurs prior to 15 years of age [7]. AFS has a peak incidence in the 40s, mostly ranging from 30 to 80 years of age, but may occur in any age [6, 8]. In most patients, wide local excision is the primary therapy option, and radiotherapy/chemotherapy is generally performed in patients with unresectable, recurrent, or metastatic cases. Metastasis of AFS is reported in less than 10% of the patients [8]. Imaging studies in patients with adult fibrosarcoma are very rare. The aim of this study was to analyze the appearance of recurrent AFS with a focus on configuration and to assess the occurrence of loco-regional post-treatment changes on MRI follow-up.
Patients and methods
One hundred sixty-eight MRI follow-up scans of 15 patients with histologically proven AFS between 2012 and 2018 were retrospectively reviewed. Three patients were excluded due to insufficient data. Twelve remaining patients underwent postoperative MRI follow-up for a minimum of 1 year at our institution. The age of the patients at primary diagnosis, the localization of the recurrent tumors, and the recurrence free follow-up interval were analyzed. The recurrent tumors were radiographically examined for signal intensity, contrast agent behavior, configuration, limitation, and extent on MRI. Loco-regional post-treatment changes were divided into subcutaneous tissue and muscle edema, postoperative seroma, lymphadenopathy, and bone edema.
MR imaging was performed with a 1.5 T MRI system (MAGNETOM Symphony, Siemens Healthineers). The MRI protocol was performed with the following sequences: axial T2-weighted; axial T1-weighted; axial proton density-weighted (PDw); coronal turbo-inversion recovery-magnitude (TIRM); and axial, coronal, and sagittal T1-weighted after application of IV contrast agent.
Two dedicated sarcoma radiologists, with 18 and 9 years of sarcoma diagnostics experience, respectively, reviewed each MRI with findings reached by consensus. The reviewers were blinded to clinical and patient data and were not involved in the inclusion and exclusion process.
Statistical data
If not indicated otherwise, data are given as median values with range (minimum to maximum) or mean with standard deviation (SD). Parametric and nonparametric tests to compare group values (χ2 test, Mann-Whitney U test, ANOVA) were performed as indicated. Furthermore, risk ratios (RR) for the determination of relative risks were analyzed. Statistical significance for all tests was set at a level of p < 0.05. Statistical analysis was done using the IBM-SPSS version 22.0 software package (IBM, Armonk, NY, USA).
Ethics approval
The study was conducted in accordance with and was approved by the responsible IRB/Ethics Committee: Ethics Commission of the Medical Faculty of the Ruhr-University Bochum, Germany. Informed consent was waived by the IRB/Ethics Committee because of the retrospective nature of the study and the analysis of anonymous data.
Results
The mean age of the patients was 50.2 years (min., 22; max., 74; SD, 16.7). Primary AFS significantly most often occurred in the extremities (p < 0.05; Fig. 1). Five patients (42%) presented recurrences of AFS within MRI follow-up. Recurrences purely presented in the upper extremities and the chest wall (Fig. 1). Altogether, 9 lesions were detected with bifocal recurrences in two patients. Recurrent AFS occurred 12 months after primary tumor resection in the mean (SD, 6.5; min., 3; max., 19). All patients with recurrences were over 50 years of age. The relative risk ratio (RR) for patients over 55 years of age was 5 (95% CI, 1.8 to 31; p = 0.04). The extremities were the main localization of recurrent AFS (6 lesions). Two patients presented with recurrent AFS of the thoracic wall and one patient of the shoulder. Recurrent AFS had no common appearance on MRI. Recurrent AFS appeared nodular/homogeneous (Fig. 2a and b), ovoid/ homogeneous (Fig. 3a and b), streaky (Fig. 4a and b), and homogeneous/heterogeneous, polycyclic/heterogeneous (Fig. 5a and b), or fascicular/homogeneous. The intensity of contrast enhancement ranged from rim to marked contrast enhancement. Recurrent AFS mostly showed a muscle iso-intense signal in T1-weighted and a hyperintense signal in PD-weighted and TIRM sequences (Table 1). There were no significant differences in the configuration of recurrences between different localizations. The most common loco-regional post-treatment changes were subcutaneous edema (92%; p = 0.03), followed by muscle edema (75%) and postoperative seroma (50%). Patients with the presence of muscle edema after resection of the primary tumor had a slightly, but not significantly higher risk of recurrences (RR = 1.75; p = 0.08; Table 2). Two patients developed distant metastases with two cases of lung and one case of lymph node metastases.
Recurrent adult fibrosarcoma at 1.5 T MRI (T1FS after application of IV contrast agent) of the forearm of a 60-year-old patient. Recurrent adult fibrosarcoma (white arrow) is shown in coronal (a) and axial (b) view. The tumor presents as a well-defined, homogenous, and nodular mass with marked contrast enhancement (white arrow) and perifocal muscle edema (white arrow head), as well as subcutaneous tissue edema (black arrow head)
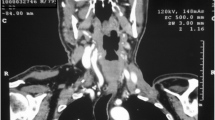
Recurrent adult fibrosarcoma at 1.5 T MRI (T1FS after application of IV contrast agent) of the thoracic wall of a 70-year-old patient. Recurrent adult fibrosarcoma (white arrow) is shown in axial (a) and coronal (b) view. The tumor presents as a well-defined, homogenous, and ovoid mass with marked contrast enhancement
Recurrent adult fibrosarcoma at 1.5 T MRI (T1FS after application of IV contrast agent) of the forearm of a 57-year-old patient. Recurrent adult fibrosarcoma (white arrow) is shown in axial (a) and coronal (b) view. The tumor presents with a streaky configuration, slightly infiltrative behavior, and homogenous and marked contrast enhancement (white arrow)
Recurrent adult fibrosarcoma at 1.5 T MRI (PD FS (a) and T1 FS after application of IV contrast agent (b)) of the upper arm of a 65-year-old male patient. Bifocal recurrent adult fibrosarcoma is shown in coronal (a) and axial (b) view. Polycyclic and heterogeneous recurrence with rim contrast enhancement (white arrow) in the axilla and a smaller recurrence with the same appearance in the distal upper arm (black arrow). Perifocal edema of the muscle and subcutaneous tissue (black arrow head) and marked post-treatment edema of the further soft tissue (white arrow head) are present
Discussion
In this study, we analyzed features of recurrent AFS and post-treatment changes on MRI follow-up. AFS of the soft tissue is a very rare neoplasm. Due to the rarity of this diagnosis, publications on AFS are rare as well, especially on imaging. We focused on the appearance of recurrent AFS, as the primary tumors are well-described, but there is no previous publication on the appearance of recurrent AFS available. Two types of fibrosarcomas have to be distinguished: infantile and adult fibrosarcoma (AFS). In this study, we dealt with adult fibrosarcoma (AFS), which is reported to occur after 15 years of age [7]. Previous studies report that AFS mostly affects elderly patients with an average age of 50 [2, 9]. The mean age of the patients in our study was around 50 years as well. The median recurrence-free MRI follow-up interval in our study was 28 months. This has to be distinguished from the clinical recurrence-free follow-up interval, which is often higher, due to the often incomplete MRI data set. In the regular postoperative setting, a postoperative MRI follow-up interval for a period of 5 years is foreseen [10]. This period seems adequate as recurrences of AFS do not occur later than 19 months after primary tumor resection in our study. From our experience, a close MRI follow-up for the first three postoperative years is recommended. Accordingly, follow-up MRI should be performed at intervals of 3 months in the first year and of 6 months in the second and third year. Afterwards, the follow-up intervals can be extended to once a year for the last 2 years. The local recurrence rate for AFS is reported to range from 12 to 79% with an average of 40–50% [2, 6]. Equally, 42% of our patients developed recurrences of AFS. Although MRI is well-suited for the follow-up screening and detection of AFS recurrences, MRI reaches its limits in the characterization of AFS. Additionally, as previously reported, AFS has no obvious MRI characteristics, making the diagnosis very difficult [2, 11]. Wand et al. describe the MRI appearance of primary AFS as lobulated and well-defined and in some cases ovoid [2]. Others describe AFS to appear with irregular margins [12]. In our study, recurrent AFS has no common appearance as well. The tumor may appear nodular, ovoid, streaky, polycyclic, or fascicular with homogeneous or heterogeneous contrast enhancement, as well as well-defined borders or infiltrative behavior. As already reported before, the extremities are the main localization of AFS [13,14,15]. Often, AFS mostly occur especially around the thigh and knee, the arm, and the trunk [6, 16]. The thigh, upper arm, forearm, and shoulder represent the most common sites of AFS in our study. Furthermore, MRI is the imaging modality of choice for post-treatment follow-up screening of soft tissue sarcoma. It plays an extraordinary role not only in the detection of sarcoma recurrences but also in the distinction to post-treatment changes. Nevertheless, the differentiation between post-treatment soft tissue changes and tumor recurrences is often difficult [17]. Previous data describe that approximately 17–19% of patients develop postoperative seroma after resection of soft tissue sarcomas [17,18,19]. Furthermore, it is reported that 37% of patients with soft tissue tumors present with bone marrow edema [20]. In our study, 92%, 75%, and 50% of the patients developed subcutaneous tissue edema, muscle edema, and postoperative seroma, respectively. In addition, our data showed that patients with the presence of muscle edema after primary tumor resection have a 1.75 times higher risk for AFS recurrences. This trend was not significantly, but nevertheless has to be investigated in further studies. Finally, opposed to our study, AFS is reported to have a high risk to metastasize, mostly to the lungs, the liver, and the bones [2, 21, 22].
Conclusion
Recurrent AFS shows no common appearance on MRI, which makes a characterization of recurrent AFS difficult. Recurrences may appear nodular, ovoid, streaky, polycyclic, or fascicular. Patients with presence of muscle edema after primary tumor resection have a slightly, but not significantly higher risk for AFS recurrences.
Change history
19 August 2021
A Correction to this paper has been published: https://doi.org/10.1007/s00238-021-01864-8
References
Orbach D, Rey A, Cecchetto G, Oberlin O, Casanova M, Thebaud E, Scopinaro M, Bisogno G, Carli M, Ferrari A (2009) Infantile fibrosarcoma: management based on the European experience. J Clin Oncol 28(2):318–323
Wang H, Nie P, Dong C, Li J, Huang Y, Hao D, Xu W (2018). CT and MRI findings of soft tissue adult fibrosarcoma in extremities. BioMed research international. https://doi.org/10.1155/2018/6075705
Meyerding HW, Broders AC, Hargrave RL (1936) Clinical aspects of fibrosarcoma of the soft tissues of the extremities. Surg Gynecol Obstet 62:1010–1019
Toro JR, Travis LB, Wu HJ, Zhu K, Fletcher CDM, Devesa SS (2006) Incidence patterns of soft tissue sarcomas, regardless of primary site, in the surveillance, epidemiology and end results program, 1978–2001: an analysis of 26,758 cases. Int J Cancer 119(12):2922–2930
Fisher C (1990) The value of electronmicroscopy and immunohistochemistry in the diagnosis of soft tissue sarcomas: a study of 200 cases. Histopathology 16(5):441–454
Augsburger D, Nelson PJ, Kalinski T, Udelnow A, Knösel T, Hofstetter M, Qin JW, Wang Y, Gupta AS, Bonifatius S, Li M, Bruns CJ, Zhao Y (2017) Current diagnostics and treatment of fibrosarcoma–perspectives for future therapeutic targets and strategies. Oncotarget 8(61):104638–104653
Muzaffar AR, Friedrich JB, Lu KK et al (2006) Infantile fibrosarcoma of the hand associated with coagulopathy. Plast Reconstr Surg 117(5):81e–86e
Lm W (2009) Soft tissues. In: Modern Surgical Pathology. WB Saunders, pp 1717–1783
Fletcher CDM, Unni KK, Mertens F (2002) Pathology and genetics of tumours of soft tissue and bone. Iarc pp. 12–14
Aga P, Singh R, Parihar A, Parashari U (2011) Imaging spectrum in soft tissue sarcomas. Indian J Surg Oncol 2(4):271–279
Vanhoenacker FM, Parizel PM, Gielen JL (2006) Imaging of soft tissue tumors. Springer Science & Business Media. pp. 3–16
Meyers SP (2008) MRI of bone and soft tissue tumors and tumorlike lesions. Thieme New York, NY, pp. 1–16
Smith SE, Kransdorf MJ (2000). Primary musculoskeletal tumors of fibrous origin. In Seminars in musculoskeletal radiology. 4(1):73–88
Coffin CM, Dehner LP, Meis-Kindblom JM (1998). Inflammatory myofibroblastic tumor, inflammatory fibrosarcoma, and related lesions: an historical review with differential diagnostic considerations. In Seminars in diagnostic pathology. 15(2):102–110
Mankin HJ, Hornicek FJ (2005) Diagnosis, classification, and management of soft tissue sarcomas. Cancer Control 12(1):5–21
Cormier JN, Pollock RE (2004) Soft tissue sarcomas. CA Cancer J Clin 54(2):94–109
James SLJ, Davies A (2008) Post-operative imaging of soft tissue sarcomas. Cancer Imaging 8(1):8–18
Poon-Chue A, Menendez L, Gerstner MM, Colletti P, Terk M (1999) MRI evaluation of post-operative seromas in extremity soft tissue sarcomas. Skelet Radiol 28(5):279–282
Skibber JM, Lotze MT, Seipp CA, Salcedo R, Rosenberg SA (1987) Limb-sparing surgery for soft tissue sarcomas: wound related morbidity in patients undergoing wide local excision. Surgery 102(3):447–452
Hwang S, Lefkowitz R, Landa J, Akin O, Schwartz LH, Cassie C, Healey JH, Alektiar KM, Panicek DM (2009) Local changes in bone marrow at MRI after treatment of extremity soft tissue sarcoma. Skelet Radiol 38(1):11–19
Scott SM, Reiman HM, Pritchard DJ, Ilstrup DM (1989) Soft tissue fibrosarcoma. A clinicopathologic study of 132 cases. Cancer 64(4):925–931
Pritchard DJ, Soule EH, Taylor WF, Ivins JC (1974) Fibrosarcoma—a clinicopathologic and statistical study of 199 tumors of the soft tissues of the extremities and trunk. Cancer 33(3):888–897
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Sam Sedaghat, Frederick Schmitz, Anne Krieger, Maya Sedaghat and Benjamin Reichardt declare that they have no conflict interest.
Ethical approval
The study was conducted in accordance with and was approved by the responsible IRB/Ethics Committee: Ethics Commission of the Medical Faculty of the Ruhr-University Bochum, Germany.
Informed consent
Informed consent was waived by the IRB/Ethics Committee because of the retrospective nature of the study and the analysis of anonymous data.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to a retrospective Open Access order.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sedaghat, S., Schmitz, F., Krieger, A. et al. Appearance of recurrent adult fibrosarcoma of the soft tissue and loco-regional post-treatment changes on MRI follow-up. Eur J Plast Surg 44, 97–102 (2021). https://doi.org/10.1007/s00238-020-01669-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00238-020-01669-1