Abstract
Purpose
Despite mounting evidence indicating that aquaporin-4 antibody-positive optic neuritis (AQP4-ON) presents a less favorable prognosis than other types of optic neuritis, there exists substantial heterogeneity in the prognostic outcomes within the AQP4-ON cohort. Considering the persistent debate over the role of MRI in assessing the prognosis of optic neuritis, we aim to investigate the correlation between the MRI appearance and long-term visual prognosis in AQP4-ON patients.
Methods
We retrospectively reviewed the ophthalmological and imaging data of AQP4-ON patients admitted to our Neuro-ophthalmology Department from January 2015 to March 2018, with consecutive follow-up visits for a minimum of 3 years.
Results
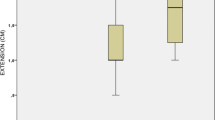
A total of 51 AQP4-ON patients (59 eyes) meeting the criteria were enrolled in this research. After assessing the initial orbital MR images of each patient at the first onset, we observed the involvement of the canalicular segment (p < 0.001), intracranial segment (p = 0.004), optic chiasm (p = 0.009), and the presence of LEON (p = 0.002) were significantly different between recovery group and impairment group. For quantitative measurement, the length of the lesions is significantly higher in the impairment group (20.1 ± 9.3 mm) than in the recovery group (12.5 ± 5.3 mm) (p = 0.001).
Conclusion
AQP4-ON patients with involvement of canalicular, intracranial segment and optic chiasm of the optic nerve, and the longer range of lesions threaten worse vision prognoses. Timely MR examination during the initial acute phase can not only exclude the intracranial or orbital mass lesions but also indicate visual prognosis in the long term.





Similar content being viewed by others
Data availability
The data that support the findings of this study are available on request from the corresponding author upon reasonable request.
References
Kolappan M, Henderson APD, Jenkins TM et al (2009) Assessing structure and function of the afferent visual pathway in multiple sclerosis and associated optic neuritis. J Neurol 256:305–319
Kale N (2012) Management of optic neuritis as a clinically first event of multiple sclerosis. Curr Opin Ophthalmol 23:472–476
Schinzel J, Schwarzlose L, Dietze H et al (2012) Efficacy of vision restoration therapy after optic neuritis (VISION study): study protocol for a randomized controlled trial. Trials 13:94
Chen JJ, Pittock SJ, Flanagan EP et al (2020) Optic neuritis in the era of biomarkers. Surv Ophthalmol 65:12–17
Toosy AT, Mason DF, Miller DH (2014) Optic neuritis. Lancet Neurol 13:83–99
Lennon VA, Wingerchuk DM, Kryzer TJ et al (2004) A serum autoantibody marker of neuromyelitis optica: distinction from multiple sclerosis. The Lancet 364:2106–2112
Kawachi I, Lassmann H (2017) Neurodegeneration in multiple sclerosis and neuromyelitis optica. J Neurol Neurosurg Psychiatry 88:137–145
Wingerchuk DM, Banwell B, Bennett JL et al (2015) International consensus diagnostic criteria for neuromyelitis optica spectrum disorders. Neurology 85:177–189
Fernandes DB, de Ramos IPR, Falcochio C et al (2012) Comparison of visual acuity and automated perimetry findings in patients with neuromyelitis optica or multiple sclerosis after single or multiple attacks of optic neuritis. J Neuroophthalmol 32:102–106
Sato DK, Callegaro D, Lana-Peixoto MA et al (2014) Distinction between MOG antibody-positive and AQP4 antibody-positive NMO spectrum disorders. Neurology 82:474–481
Akaishi T, Sato DK, Nakashima I et al (2016) MRI and retinal abnormalities in isolated optic neuritis with myelin oligodendrocyte glycoprotein and aquaporin-4 antibodies: a comparative study. J Neurol Neurosurg Psychiatry 87:446–448
Weinshenker BG, Barron G, Behne JM et al (2015) Challenges and opportunities in designing clinical trials for neuromyelitis optica. Neurology 84:1805–1815
Petzold A, Wattjes MP, Costello F et al (2014) The investigation of acute optic neuritis: a review and proposed protocol. Nat Rev Neurol 10:447–458
Soelberg K, Skejoe HPB, Grauslund J et al (2018) Magnetic resonance imaging findings at the first episode of acute optic neuritis. Mult Scler Relat Disord 20:30–36
Youl BD, Turano G, Miller DH et al (1991) The pathophysiology of acute optic neuritis. An association of gadolinium leakage with clinical and electrophysiological deficits. Brain 114(Pt 6):2437–2450
Miller DH, Newton MR, van der Poel JC et al (1988) Magnetic resonance imaging of the optic nerve in optic neuritis. Neurology 38:175–175
Dunker S, Wiegand W (1996) Prognostic value of magnetic resonance imaging in monosymptomatic optic neuritis. Ophthalmology 103:1768–1773
Kupersmith MJ, Alban T, Zeiffer B, Lefton D (2002) Contrast-enhanced MRI in acute optic neuritis: relationship to visual performance. Brain 125:812–822
Berg S, Kaschka I, Utz KS et al (2015) Baseline magnetic resonance imaging of the optic nerve provides limited predictive information on short-term recovery after acute optic neuritis. PLoS One 10:e0113961
Akaishi T, Nakashima I, Takeshita T et al (2016) Lesion length of optic neuritis impacts visual prognosis in neuromyelitis optica. J Neuroimmunol 293:28–33
Cellina M, Floridi C, Rosti C et al (2019) MRI of acute optic neuritis (ON) at the first episode: can we predict the visual outcome and the development of multiple sclerosis (MS)? Radiol Med 124:1296–1303
Petzold A, Fraser CL, Abegg M et al (2022) Diagnosis and classification of optic neuritis. Lancet Neurol 21:1120–1134
Jarius S, Paul F, Weinshenker BG et al (2020) Neuromyelitis optica. Nat Rev Dis Primers 6:85
Yu B, Qi Y, Li R et al (2021) B cell-specific XIST complex enforces X-inactivation and restrains atypical B cells. Cell 184:1790-1803.e17
Zhou H, Zhao S, Yin D et al (2016) Optic neuritis: a 5-year follow-up study of Chinese patients based on aquaporin-4 antibody status and ages. J Neurol 263:1382–1389
Kang H, Chen T, Li H et al (2017) Prognostic factors and disease course in aquaporin-4 antibody-positive Chinese patients with acute optic neuritis. J Neurol 264:2130–2140
Choi J, Kim S-J, Chang JW et al (2012) Clinical characteristics of optic neuritis in Koreans greater than 50 years of age. Korean J Ophthalmol 26:111–115
Kitley J, Leite MI, Nakashima I et al (2012) Prognostic factors and disease course in aquaporin-4 antibody-positive patients with neuromyelitis optica spectrum disorder from the United Kingdom and Japan. Brain 135:1834–1849
Saini H, Fernandez G, Kerr D, Levy M (2010) Differential expression of aquaporin-4 isoforms localizes with neuromyelitis optica disease activity. J Neuroimmunol 221:68–72
Dos Passos GR, Oliveira LM, da Costa BK et al (2018) MOG-IgG-associated optic neuritis, encephalitis, and myelitis: lessons learned from neuromyelitis optica spectrum disorder. Front Neurol 9:217
Dubey D, Pittock SJ, Krecke KN et al (2019) Clinical, radiologic, and prognostic features of myelitis associated with myelin oligodendrocyte glycoprotein autoantibody. JAMA Neurol 76:301–309
Funding
This work is supported by the Youth Fund of Shanghai Health Commission in China, 20224Y0318.
Author information
Authors and Affiliations
Contributions
Hanyu Shaw: conceptualization (lead); methodology; writing—original draft.
Chaoyi Feng: resources; data curation.
Meng Qi: formal analysis.
Yalan Deng: visualization.
Wei Chen: revise English writing.
Yiyin Zhang: software; validation.
Luxi Wang: software; investigation.
Naier Lin: funding acquisition.
Guohong Tian: conceptualization (support); supervision.
Yan Sha: writing—review and editing.
The first draft of the manuscript was written by Hanyu Shaw and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All experiments were performed in accordance with the relevant guidelines and regulations and were approved by the ethics committee of the Eye Ear Nose and Throat Hospital.
Informed consent
Informed consent from the subjects was waived by the above-mentioned ethic committee.
Human and animal rights
The study is a retrospective clinical data analysis and therefor does not involve human or animal research.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shaw, H., Feng, C., Qi, M. et al. Analysis of the initial orbital MRI in aquaporin-4 antibody-positive optic neuritis (AQP4-ON): lesion location and lesion length can be predictive of visual prognosis. Neuroradiology (2024). https://doi.org/10.1007/s00234-024-03306-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00234-024-03306-1