Abstract
Purpose
We aimed to study the association of non-contrast CT (NCCT) thrombus density with procedural and clinical outcomes in patients with acute ischemic stroke who underwent endovascular treatment (EVT). Since thrombus density is associated with thrombus location, we focused on M1 occlusions only.
Methods
Patients with available thin-slice (< 2.5 mm) NCCT were included from a nationwide registry. Regression models were used to assess the relation between thrombus density (per Hounsfield unit [HU]) and the following outcomes. For reperfusion grade, adjusted common odds ratios (acOR) indicated a 1-step shift towards improved outcome per HU increase in thrombus density. For the binary outcomes of first-pass reperfusion (first-pass extended thrombolysis in cerebral infarction [eTICI] 2C-3, FPR), functional independence [90-day modified Rankin Scale (mRS) score of 0–2] and mortality), aORs were reported. Adjusted β coefficients (aβ) were reported for 24-h NIHSS and procedure duration in minutes. Outcome differences between first-line treatment devices (stent retriever versus aspiration) were assessed with interaction terms.
Results
In 566 patients with M1 occlusions, thrombus density was not associated with reperfusion (acOR 1.01, 95% CI 0.99–1.02), FPR (aOR 1.01, 95% CI 0.99–1.03), mortality (aOR 0.98, 95% CI 0.95–1.00), 24-h NIHSS (aβ − 0.7%, 95% CI − 1.4–0.2), or procedure duration (aβ 0.27, 95% CI − 0.05–0.58). In multivariable analysis, thrombus density was associated with functional independence (aOR 1.02, 95% CI 1.00–1.05). No interaction was found between thrombus density and first-line treatment device for any outcome.
Conclusion
In patients with M1 occlusions, thrombus density was not clearly associated with procedural and clinical outcomes after EVT.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Endovascular treatment (EVT) for acute ischemic stroke is now standard of care for patients with a proximal occlusion of the anterior circulation [1]. The main goal of EVT is to retrieve the thrombus to restore the blood flow to the brain. Nevertheless, successful reperfusion is not achieved in nearly 20% of EVT-treated patients in current clinical practice [2]. Thrombus imaging characteristics could potentially guide in choosing EVT technique (e.g., stent retriever or distal aspiration) [3]. Previously, thrombus density has been reported to be associated with reperfusion in patients who underwent EVT [4,5,6,7]. However, other studies found no association between thrombus density and reperfusion and functional outcome in patients treated with EVT [8,9,10,11,12].
Histologically, hyperdense thrombi on non-contrast CT (NCCT) contain more red blood cells (RBCs) than non-hyperdense thrombi which are more fibrin- and platelet-rich [3, 13,14,15,16,17]. Fibrin-rich thrombi have been described to be stiffer and can cause more friction between the thrombus and vessel wall compared with RBC-rich thrombi. Consequently, fibrin-rich thrombi have been found to be more difficult to retrieve with EVT [3, 18]. This might explain previously reported associations between decreasing thrombus density, in Hounsfield units (HU), and a lower chance of successful reperfusion and favorable outcome [3,4,5,6]. Furthermore, RBC-rich thrombi are more sensitive to intravenous alteplase (IVT) than fibrin-rich thrombi [3]. There is heterogeneity in thrombus location in most studies investigating imaging characteristics of thrombi. Yet, hyperdense thrombi usually have a more proximal location (smaller distance from the terminus of the carotid artery [ICA-T] to proximal thrombus border) than non-hyperdense thrombi [11, 19]. Hence, this difference might affect the association between thrombus density and outcomes and could be an explanation for the conflicting results in previous studies.
We aimed to study the association between thrombus density, reperfusion, first-pass reperfusion, procedure duration, functional outcome, and mortality in a large dataset consisting of patients with occlusions of the M1 segment of the middle cerebral artery treated with EVT. We specifically focused on M1 occlusions to reduce the influence of other factors, such as vascular anatomy, clinical deficit, and procedural difficulty. Furthermore, we assessed the effect of first-line EVT device (stent retriever or aspiration) on the association between thrombus density and outcomes.
Methods
Patient selection
Patients included in this study were recruited from the MR CLEAN Registry: a nationwide prospective, observational multicenter registry that collected data of patients treated with EVT for acute ischemic stroke due to intracranial large vessel occlusion in the 17 intervention hospitals in the Netherlands, since the completion of the MR CLEAN trial in March 2014 [20]. The central medical ethics committee of the Erasmus MC gave permission to carry out the study as a registry (MEC-2014–235) [20]. Source data of this study are not available due to privacy regulations, but analytic methods and statistical code are available upon reasonable request.
The current study reports on patients treated between March 14, 2014 and November 1, 2017. All patients without contraindications received 0.9 mg/kg IVT prior to EVT. The exact EVT approach and material choice were left to the discretion of the treating neurointerventionist. EVT consisted of stent retriever thrombectomy, aspiration thrombectomy, or a combined approach, with or without administering additional intra-arterial thrombolytic agents. A combined approach of aspiration and stent retriever was not recorded separately. Therefore, these patients were included in the first-line stent retriever group. For the current study, we used the following inclusion criteria: occlusion of the M1 segment of the middle cerebral artery, age ≥ 18 years, onset to groin puncture < 6.5 h, treatment performed in a MR CLEAN trial center, and available thin-slice baseline NCCT and CT angiography (CTA) scans acquired within 30 min on the same scanner. For patients who were transferred from a primary stroke center, we used the primary stroke center’s imaging for thrombus density measurements. We excluded patients with a high chance of inaccurate measurements due to incorrigible co-registration misalignment, poor CTA contrast opacification, artifacts (movement, metal, beam hardening), excessive noise, too short or too narrow thrombi, or a thrombus located too close to bone causing bone artefacts, partial occlusions, bilateral thrombi, and incomplete field of views. Furthermore, we excluded patients with calcified cerebral emboli since the higher density values in these thrombi cause streak artefacts and partial volume artefacts. In addition, as we reported before [21], patients with calcified cerebral emboli have worse (reperfusion) outcomes than other stroke patients which could interfere with our analysis.
Imaging analyses
The following imaging characteristics were evaluated by the MR CLEAN Registry imaging core lab, whose members were blinded to all clinical data except for symptom side [20]: Alberta Stroke Program Early CT Score (ASPECTS) on baseline NCCT [22], clot burden score [23, 24], collateral score [24], presence of cervical carotid lesions, and occlusion location on baseline CTA. Ipsilateral cervical carotid lesions were classified into non-significant or significant atherosclerotic stenosis (< or > 50%), total atherosclerotic occlusion (100%), or dissection. Reperfusion status, occurrence of per-procedural embolization to a new territory (ENT), and vessel perforation were evaluated by the imaging core lab on digital subtraction angiography imaging. Reperfusion status was evaluated according to the six-point expanded thrombolysis in cerebral infarction (eTICI) scale [25]. eTICI 0 or 1 indicates no or minimal reperfusion, eTICI 2 indicates incomplete reperfusion (2A < 50% of territory; 2B ≥ 50% of territory, 2C near complete reperfusion except slow flow or a few small distal cortical emboli), and eTICI 3 indicates complete reperfusion. For the current study, thin slice NCCT and CTA images (≤ 2.5 mm) were aligned with rigid co-registration using Elastix [26]. CTA images were used as reference for vessel anatomy and contrast detection. Thrombus density in Hounsfield units (HUs) was measured by placing three spherical ROIs with a 1-mm radius in the proximal, middle, and distal parts of the thrombus on co-registered NCCT and CTA images. Thrombus density was determined as the average density of the three NCCT ROIs in HU. Distance from ICA-T to proximal thrombus border (distance to thrombus [DT]) was measured as well to investigate the effect of thrombus location on thrombus density. DT was measured by placing one ROI in the ICA-T and one ROI at the proximal thrombus border and extracting the distance in mm. If necessary, additional ROIs were placed in between, to edit the used centerline in case of a curved artery. Measurements were performed by ten trained raters (AAEB, NA, MK, BGD, JWH, JB, MLT, NAT, PRK, NB). Regular consensus readings were held with an expert neuroradiologist with more than 25 years of experience (CBLMM) to discuss and compare measurements.
Outcome assessment
Our primary outcome was final reperfusion grade as measured with the eTICI scale. Secondary outcomes were first-pass reperfusion (defined as excellent/complete reperfusion [eTICI 2C-3] in a single pass) [27], procedure duration (time between groin puncture and groin closure), 24-h National Institutes of Health Stroke Scale (NIHSS), 90-day modified Rankin Scale (mRS) [28, 29], and 90-day mortality. The mRS score was assessed at 90 days after stroke by local investigators as part of usual care. Functional independence was defined as an mRS score of 0–2.
Statistical analysis
For descriptive analyses, we compared baseline and treatment variables in patients with hyperdense (≥ 50 HU) and non-hyperdense thrombi (< 50 HU). This threshold was selected based on the median thrombus density in our study and based on previous studies in which an affected middle cerebral artery had a density between 44 and 61 HU [30, 31]. We compared thrombus density across different scanner types to assess the effect of scanner type on thrombus density. Furthermore, we compared baseline characteristics and scanner types between our cohort of patients with M1 occlusions with available thin-slice imaging and the overall cohort of patients with M1 occlusions in the MR CLEAN Registry. Group comparisons were made using the Pearson chi-squared test or Mann–Whitney U test appropriate to the type of data. For the variable first-line EVT device, we made comparisons over the years since the use of an aspiration device became more common over the years. We compared the use of first-line stent retriever versus aspiration in patients with hyperdense and non-hyperdense thrombi included between 2014 and 2016 versus patients included in 2017.
We used univariable and multivariable regression analyses to assess the association between thrombus density (per HU) and outcomes. In all regression analyses, thrombus density was assessed as continuous variable per 1 HU. Ordinal regression was only performed if the proportional odds assumption for the ordinal variable was met. This assumption was met for our primary outcome (ordinal eTICI) but not for our secondary outcome measure 90-day mRS. Therefore, we assessed 90-day mRS as binary outcome (mRS 0–2 vs mRS 3–6). eTICI was assessed with ordinal logistic regression resulting in an (adjusted) common odds ratio ([a]cOR) and 95% confidence intervals (95% CI) for a 1-step shift towards better reperfusion outcome per HU increase in thrombus density. We used linear regression for continuous outcomes, resulting in (adjusted) beta coefficients ([a]β) with 95% CI. Twenty-four-hour NIHSS was log 10 transformed, to better meet the assumption of normally distributed residuals in linear regression, and we added 1 point to the NIHSS, so an original NIHSS score of 0 was equivalent to log 10 NIHSS + 1. The resulting (a)β coefficients indicate the percentage increase or decrease of the 24-h NIHSS per HU increase in thrombus density. For procedure duration, the (a)β coefficients indicate the duration increase in minutes per HU increase in thrombus density. For dichotomous outcomes (first-pass reperfusion, functional independence and mortality), we used binary logistic regression resulting in (adjusted) odds ratios ([a]OR) with 95% CI per HU increase in thrombus density. First-pass reperfusion was compared with both multiple pass reperfusion (eTICI 2C-3 in multiple passes) and no excellent reperfusion which was defined as eTICI < 2C independent of the number of passes.
To assess the effect of thrombus density on first-line treatment device, interaction between thrombus density and first-line treatment device (first-line stent retriever versus first-line aspiration) was tested for all outcomes in separate models by adding an interaction term (first-line treatment device × thrombus density). In case of non-significant interaction, subgroup analyses were exploratory.
Based on baseline imbalances and pre-specified prognostic factors, we adjusted for age, sex, baseline NIHSS, time from onset to first CT imaging time, IVT, DT, clot burden score, ASPECTS, and > 50% stenosis of the ipsilateral carotid artery. For the regression analyses only, missing data were imputed using multiple imputation based on relevant covariates and outcomes [32]. p values < 0.05 were considered statistically significant. All statistical analyses were performed with IBM SPSS Statistics 28.0.
Results
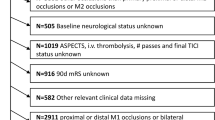
In total, 566 patients with M1 occlusions were included in the analyses (Supplemental Fig. I). A major exclusion reason was the unavailability of thin-slice imaging. Patients with hyperdense thrombi were more often male than patients with non-hyperdense thrombi (56% vs 45%, p < 0.01) (Table 1). Baseline NIHSS was higher in patients with hyperdense thrombi than in patients with non-hyperdense thrombi (median 16, IQR 13–20 vs 15, IQR 10–20; p = 0.006). Although the median ASPECTS and clot burden score were numerically similar between the two groups of patients, a significant difference was present (p = 0.005 and p = 0.02, respectively). Overall, median thrombus density was 50 HU (IQR, 44–57 HU). Thrombus density was similar across different scanner types (p = 0.08) (Supplemental Table I). Hyperdense thrombi had smaller DT than non-hyperdense thrombi: median 10 mm (IQR, 4–16 mm) vs 14 mm (IQR, 9–19 mm) (p < 0.001). High-grade stenosis of the ipsilateral carotid artery was more often present in patients with hyperdense thrombi vs non-hyperdense (p = 0.02). Time from onset to first CT imaging was significantly longer in patients with hyperdense thrombi than in patients with non-hyperdense thrombi (69 min, IQR 52–116 min vs 81 min, IQR 55–125 min; p = 0.047). Stent retrievers were more often used as first-line EVT device in patients with hyperdense than in patients with non-hyperdense thrombi: 182/233 (78%) vs 140/214 (65%) (p = 0.003) (Table 2). Overall, the use of aspiration increased over the years (p < 0.001; Supplemental Table II). In addition, we only found a difference in first-line EVT device in patients with hyperdense versus non-hyperdense thrombi included after 2016 (p = 0.01; Supplemental Table III). Occurrence of ENT was similar in both groups: 8/252 (3%) in patients with hyperdense thrombi versus 8/239 (3%) in patients with non-hyperdense thrombi (Table 2).
Significant differences were present between the cohort of patients with M1 occlusions included in this study and the overall cohort of patients with M1 occlusions included in the MR CLEAN Registry. Hypertension and hypercholesterolemia were more often present in the overall cohort of M1 patients than in our cohort: 942/1779 (53%) vs 252/552 (46%) (p < 0.001) for hypertension and 534/1730 (31%) vs 137/540 (25%) (p = 0.001) for hypercholesterolemia (Supplemental Table IV). A collateral score of 3 was more often present in the overall cohort of M1 patients (352/1766 [20%]) than in our cohort (95/557 [17%], p = 0.03). Onset to groin puncture time was significantly lower in our study cohort than in the overall cohort of M1 patients (median 185 vs 195 min, p < 0.001). This difference might be caused by the lower number of transferred patients in our study cohort when compared to the overall cohort (212/565 [38%] vs 1014/1814 [56%], p < 0.001). In addition, in our cohort of M1 occlusion patients, EVT was more often performed in a university hospital when compared to the overall cohort of M1 patients (66% vs 56%, p < 0.001) (Supplemental Table IV). Finally, imaging was performed on less different scanner types in our study cohort when compared to the overall cohort of patients with M1 occlusions (p < 0.001) (Supplemental Table V).
Outcomes
Thrombus density was not significantly associated with final reperfusion grade (acOR 1.01, 95% CI 0.99–1.02) or first-pass reperfusion (aOR 1.01, 95% CI 0.99–1.03) (Tables 2 and 3; Supplemental Fig. II). In the unadjusted analysis, thrombus density was associated with increased procedure duration (β 0.36, 95% CI 0.05–0.67 min longer per HU density increase) (p = 0.02). After adjustments, this association was not significant anymore (aβ 0.27, 95% CI − 0.05–0.58 min longer per HU density increase) (Table 3; Supplemental Fig. III). Thrombus density was not associated with 24-h NIHSS (aβ − 0.7, 95% CI − 1.4–0.2% change in NIHSS per HU increase). Only in the multivariable analysis thrombus density was associated with functional independence (aOR 1.02, 95% CI 1.00–1.05). The association between thrombus density and 90-day mRS is visualized in a mRS barplot (Fig. 1) and boxplot (Supplemental Fig. IV). No significant association was found between thrombus density and 90-day mortality (aOR 0.98, 95% CI 0.95–1.00) (Table 3).
No significant interaction was found between thrombus density and first-line treatment device for any of the outcomes. The interaction analysis results are reported in Supplemental Tables VI and VII along with an exploratory subgroup analysis.
Discussion
In our study of 566 patients with M1 occlusions who were treated with EVT, thrombus density was not associated with final reperfusion grade, first-pass reperfusion, 24-h NIHSS, or mortality. Only in multivariable analysis, thrombus density was associated with functional independence. In patients with hyperdense thrombi, a stent retriever was used more often as first-line EVT device than in patients with non-hyperdense thrombi. However, we did not find significant interaction between thrombus density and first-line EVT device for any of the outcomes.
Contrary to some small studies [5,6,7], and a meta-analysis including five small studies [4], we did not find an association between thrombus density and reperfusion after EVT. However, heterogeneity of the meta-analysis was substantial (73%) [4]. Furthermore, occlusion location varied in all the aforementioned studies which might have affected the results because thrombus density differs significantly for different occlusion locations [11, 19]. Similar, in a previous study performed in patients with M1 occlusions only who underwent EVT [9], no association was found between thrombus density and reperfusion which is in line with our results.
Several studies described associations between thrombus density on NCCT and histological composition [3, 13,14,15,16,17]. Furthermore, fibrin-rich thrombi have been described to be more difficult to retrieve with EVT [3, 18]. So, one could have expected a relation between thrombus density and reperfusion outcomes. However, this association might have been affected by a change in thrombus composition with an increasing number of device passes. A previous study demonstrated that thrombus fragments retrieved during the first two passes are more RBC-rich than fragments retrieved in subsequent passes, the latter being more fibrin-rich [33]. These fibrin-rich portions of the thrombus might have contributed to the resistance to removal. Furthermore, this heterogeneity in thrombus composition might have been missed with our measurement method using only three ROIs to calculate average thrombus density [34]. Possibly, the non-hyperdense (fibrin-rich) parts of the thrombus were not captured with these three ROIs. In addition, it is important to keep in mind that the aforementioned study and most other histological studies simplify the complexity of thrombus composition by categorizing them in RBC-rich thrombi and fibrin-rich thrombi because these are the dominant components of thrombi retrieved in patients with acute ischemic stroke [16]. However, the role of platelets and their interaction with neutrophil extracellular traps (NETs) is not taken into account, while NETs have been associated with poor outcomes [35]. Thus, categorizing thrombi in RBC-rich, hyperdense thrombi and fibrin-rich, non-hyperdense thrombi does not take into account the more complex reality of the association between thrombus composition and thrombus density. Therefore, thrombus density measured on NCCT might fail to reflect the true complexity of thrombus composition.
It is possible that the inability to detect an association between thrombus density and reperfusion in our study was caused by a baseline imbalance in first-line EVT device between patients with hyperdense and non-hyperdense thrombi. However, this imbalance only existed in patients treated after 2016 because the use of an aspiration device became more common then. In addition, no significant interaction was found between thrombus density and first-line EVT device for any of the outcomes. Apparently, first-line device choice does not affect the association between thrombus density and (reperfusion) outcomes.
Contrary to other studies, thrombus density was significantly associated with functional independence in our study [8, 11]. However, this association was only significant in multivariable analysis, and the effect of the association was only small. In line with a previous study, we did not find an association between thrombus density and 90-day mortality [11]. Additionally, we investigated the association between thrombus density and 24-h NIHSS because this is a more direct measure of the effect of EVT and more sensitive than the mRS score at 3 months [36, 37]. Nonetheless, we were not able to detect an association between thrombus density and 24-h NIHSS.
Our study has limitations. First, thrombus measurements were performed by 10 trained observers which possibly caused interobserver variability. However, regular consensus readings with an expert neuroradiologist (CBLMM) were held to discuss difficult cases and compare measurements. Furthermore, a previous study demonstrated that non-expert observers could accurately and reproducibly assess thrombus density by the use of three ROIs [38]. Second, in our nationwide registry, reperfusion rates and functional outcome after EVT improved over the years, probably caused by improved workflow times and the increased experience of neuro-interventionists [39]. As a consequence, (reperfusion) outcomes of our study cohort included between March 2014 and November 2017 are probably worse than current clinical practice. As current reperfusion rates might be higher, the impact of a thrombus imaging characteristic such as thrombus density on (reperfusion) outcomes might be even smaller than reported in this study. Third, the main exclusion reason in our study was unavailability of thin-slice imaging which limited the total number of inclusions. Although acquired raw data are thin slices, in clinical practice, they are usually reconstructed into thicker slices to facilitate reading by reducing noise, and reduce the amount of data and processing times. Larger university hospitals more often store thin-slice imaging than smaller stroke centers. This may have led to an inclusion bias in our study cohort when compared to the overall cohort of M1 patients included in the MR CLEAN Registry. While this limited the generalizability of our results, it contributed to less scanner variability increasing the uniformity of our thrombus density measurements [40]. Finally, we used three ROIs to measure thrombus density which were placed in the proximal, middle, and distal part of the thrombus. A previous study found that full thrombus segmentations allow for more accurate thrombus density measurements [34]. Furthermore, with full thrombus segmentations, it is possible to detect heterogeneity of density values across the thrombus. Since we only used three ROIs, it might be possible that we missed these inhomogeneous components of the thrombus as mentioned before. Moreover, full thrombus segmentations can be automated and therefore are more likely to be implementable in clinical practice. As such, our results could support and stimulate future research on (automated) segmentation of the complete thrombus in order to account for heterogeneity of the thrombus and to further investigate the association between thrombus density, thrombus composition, and outcomes.
Conclusion
In patients with acute ischemic stroke due to a M1 occlusion undergoing EVT, thrombus density was not clearly associated with final reperfusion grade, first-pass reperfusion, 24-h NIHSS, functional independence, and mortality. Therefore, no evidence was found that thrombus density is a useful predictor for EVT outcomes.
Data availability
Source data of this study are not available due to privacy regulations, but analytic methods, and statistical code are available upon reasonable request.
Code availability
Statistical code is available upon reasonable request.
Abbreviations
- EVT:
-
Endovascular treatment
- IVT:
-
Intravenous alteplase treatment
- eTICI:
-
Extended thrombolysis in cerebral ischemia
- mRS:
-
Modified Rankin Scale
- NIHSS:
-
National Institutes of Health Stroke Scale
- CTA:
-
Computed tomography angiography
- NCCT:
-
Non-contrast computed tomography
- HU:
-
Hounsfield units
- DT:
-
Distance to thrombus
- ASPECTS:
-
Alberta Stroke Program Early CT Score
- ICA-T:
-
Terminus of internal carotid artery
- RBC:
-
Red blood cell
- ENT:
-
Embolization to a new territory
- IQR:
-
Interquartile ranges
- aβ :
-
(Adjusted) β coefficient
- acOR:
-
(Adjusted) common odds ratio
- aOR:
-
(Adjusted) odds ratio
References
Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, Davalos A, Majoie CB, van der Lugt A, de Miquel MA, Donnan GA, Roos YB, Bonafe A, Jahan R, Diener HC, van den Berg LA, Levy EI, Berkhemer OA, Pereira VM, Rempel J, Millan M, Davis SM, Roy D, Thornton J, Roman LS, Ribo M, Beumer D, Stouch B, Brown S, Campbell BC, van Oostenbrugge RJ, Saver JL, Hill MD, Jovin TG, H collaborators (2016) Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet 387(10029):1723–1731. https://doi.org/10.1016/S0140-6736(16)00163-X
Wollenweber FA, Tiedt S, Alegiani A, Alber B, Bangard C, Berrouschot J, Bode FJ, Boeckh-Behrens T, Bohner G, Bormann A, Braun M, Dorn F, Eckert B, Flottmann F, Hamann GF, Henn KH, Herzberg M, Kastrup A, Kellert L, Kraemer C, Krause L, Lehm M, Liman J, Lowens S, Mpotsaris A, Papanagiotou P, Petersen M, Petzold GC, Pfeilschifter W, Psychogios MN, Reich A, von Rennenberg R, Rother J, Schafer JH, Siebert E, Siedow A, Solymosi L, Thonke S, Wagner M, Wunderlich S, Zweynert S, Nolte CH, Gerloff C, Thomalla G, Dichgans M, Fiehler J (2019) Functional outcome following stroke thrombectomy in clinical practice. Stroke 50(9):2500–2506. https://doi.org/10.1161/STROKEAHA.119.026005
Jolugbo P, Ariens RAS (2021) Thrombus composition and efficacy of thrombolysis and thrombectomy in acute ischemic stroke. Stroke 52(3):1131–1142. https://doi.org/10.1161/STROKEAHA.120.032810
Brinjikji W, Duffy S, Burrows A, Hacke W, Liebeskind D, Majoie C, Dippel DWJ, Siddiqui AH, Khatri P, Baxter B, Nogeuira R, Gounis M, Jovin T, Kallmes DF (2017) Correlation of imaging and histopathology of thrombi in acute ischemic stroke with etiology and outcome: a systematic review. J Neurointerv Surg 9(6):529–534. https://doi.org/10.1136/neurintsurg-2016-012391
Froehler MT, Tateshima S, Duckwiler G, Jahan R, Gonzalez N, Vinuela F, Liebeskind D, Saver JL, Villablanca JP, Investigators US (2013) The hyperdense vessel sign on CT predicts successful recanalization with the Merci device in acute ischemic stroke. J Neurointerv Surg 5(4):289–293. https://doi.org/10.1136/neurintsurg-2012-010313
Mokin M, Morr S, Natarajan SK, Lin N, Snyder KV, Hopkins LN, Siddiqui AH, Levy EI (2015) Thrombus density predicts successful recanalization with Solitaire stent retriever thrombectomy in acute ischemic stroke. J Neurointerv Surg 7(2):104–107. https://doi.org/10.1136/neurintsurg-2013-011017
Moftakhar P, English JD, Cooke DL, Kim WT, Stout C, Smith WS, Dowd CF, Higashida RT, Halbach VV, Hetts SW (2013) Density of thrombus on admission CT predicts revascularization efficacy in large vessel occlusion acute ischemic stroke. Stroke 44(1):243–245. https://doi.org/10.1161/STROKEAHA.112.674127
Spiotta AM, Vargas J, Hawk H, Turner R, Chaudry MI, Battenhouse H, Turk AS (2014) Hounsfield unit value and clot length in the acutely occluded vessel and time required to achieve thrombectomy, complications and outcome. J Neurointerv Surg 6(6):423–427. https://doi.org/10.1136/neurintsurg-2013-010765
Yilmaz U, Roth C, Reith W, Papanagiotou P (2013) Thrombus attenuation does not predict angiographic results of mechanical thrombectomy with stent retrievers. AJNR Am J Neuroradiol 34(11):2184–2186. https://doi.org/10.3174/ajnr.A3565
Jagani M, Kallmes DF, Brinjikji W (2017) Correlation between clot density and recanalization success or stroke etiology in acute ischemic stroke patients. Interv Neuroradiol 23(3):274–278. https://doi.org/10.1177/1591019917694478
Dutra BG, Tolhuisen ML, Alves H, Treurniet KM, Kappelhof M, Yoo AJ, Jansen IGH, Dippel DWJ, van Zwam WH, van Oostenbrugge RJ, da Rocha AJ, Lingsma HF, van der Lugt A, Roos Y, Marquering HA, Majoie C, Investigatorsdagger MCR (2019) Thrombus imaging characteristics and outcomes in acute ischemic stroke patients undergoing endovascular treatment. Stroke 50(8):2057–2064. https://doi.org/10.1161/STROKEAHA.118.024247
Ye GF, Cao RY, Lu J, Qi P, Chen J, Wang DM (2019) Association between thrombus density and reperfusion outcomes using different thrombectomy strategies: a single-center study and meta-analysis. Front Neurol 10:ARTN843. https://doi.org/10.3389/fneur.2019.00843
Songsaeng D, Kaeowirun T, Sakarunchai I, Cheunsuchon P, Weankhanan J, Suwanbundit A, Krings T (2019) Efficacy of thrombus density on noninvasive computed tomography neuroimaging for predicting thrombus pathology and patient outcome after mechanical thrombectomy in acute ischemic stroke. Asian J Neurosurg 14(3):795–800. https://doi.org/10.4103/ajns.AJNS_238_18
Sporns PB, Hanning U, Schwindt W, Velasco A, Buerke B, Cnyrim C, Minnerup J, Heindel W, Jeibmann A, Niederstadt T (2017) Ischemic stroke: histological thrombus composition and pre-interventional CT attenuation are associated with intervention time and rate of secondary embolism. Cerebrovasc Dis 44(5–6):344–350. https://doi.org/10.1159/000481578
Benson JC, Fitzgerald ST, Kadirvel R, Johnson C, Dai D, Karen D, Kallmes DF, Brinjikji W (2020) Clot permeability and histopathology: is a clot’s perviousness on CT imaging correlated with its histologic composition? J Neurointerv Surg 12(1):38–42. https://doi.org/10.1136/neurintsurg-2019-014979
Fitzgerald ST, Wang S, Dai D, Douglas A, Kadirvel R, Gounis MJ, Chueh J, Puri AS, Layton KF, Thacker IC, Hanel RA, Sauvageau E, Aghaebrahim A, Almekhlafi MA, Demchuk AM, Nogueira RG, Pereira VM, Kvamme P, Kayan Y, Delgado Almandoz JE, Yoo AJ, Kallmes DF, Doyle KM, Brinjikji W (2019) Platelet-rich clots as identified by Martius Scarlet Blue staining are isodense on NCCT. J Neurointerv Surg 11(11):1145–1149. https://doi.org/10.1136/neurintsurg-2018-014637
Niesten JM, van der Schaaf IC, van Dam L, Vink A, Vos JA, Schonewille WJ, de Bruin PC, Mali WPTM, Velthuis BK (2014) Histopathologic composition of cerebral thrombi of acute stroke patients is correlated with stroke subtype and thrombus attenuation. Plos One. 9(2):ARTNe88882. https://doi.org/10.1371/journal.pone.0088882
Gunning GM, McArdle K, Mirza M, Duffy S, Gilvarry M, Brouwer PA (2018) Clot friction variation with fibrin content; implications for resistance to thrombectomy. J Neurointerv Surg 10(1):34–38. https://doi.org/10.1136/neurintsurg-2016-012721
Boodt N, Compagne KCJ, Dutra BG, Samuels N, Tolhuisen ML, Alves H, Kappelhof M, Lycklama ANGJ, Marquering HA, Majoie C, Lingsma HF, Dippel DWJ, van der Lugt A, Coinvestigators MRCR (2020) Stroke etiology and thrombus computed tomography characteristics in patients with acute ischemic stroke: a MR CLEAN Registry Substudy. Stroke 51(6):1727–1735. https://doi.org/10.1161/STROKEAHA.119.027749
Jansen IGH, Mulder M, Goldhoorn RB, MCR investigators (2018) Endovascular treatment for acute ischaemic stroke in routine clinical practice: prospective, observational cohort study (MR CLEAN Registry). BMJ 360:k949. https://doi.org/10.1136/bmj.k949
Bruggeman, AAE, M Kappelhof, N Arrarte Terreros, ML Tolhuisen, PR Konduri, N Boodt, HMM van Beusekom, HM Hund, A Taha, A van der Lugt, Y Roos, A van Es, WH van Zwam, AA Postma, DWJ Dippel, HF Lingsma, HA Marquering, BJ Emmer, C Majoie, and MCR Investigators (2021) Endovascular treatment for calcified cerebral emboli in patients with acute ischemic stroke. J Neurosurg:1–11. https://doi.org/10.3171/2020.9.JNS201798
Barber PA, Demchuk AM, Zhang J, Buchan AM (2000) Validity and reliability of a quantitative computed tomography score in predicting outcome of hyperacute stroke before thrombolytic therapy. ASPECTS Study. Group Alberta Stroke Programme Early CT Score. Lancet 355(9216):1670–4. https://doi.org/10.1016/s0140-6736(00)02237-6
Puetz V, Dzialowski I, Hill MD, Subramaniam S, Sylaja PN, Krol A, O’Reilly C, Hudon ME, Hu WY, Coutts SB, Barber PA, Watson T, Roy J, Demchuk AM, Calgary CTASG (2008) Intracranial thrombus extent predicts clinical outcome, final infarct size and hemorrhagic transformation in ischemic stroke: the clot burden score. Int J Stroke 3(4):230–236. https://doi.org/10.1111/j.1747-4949.2008.00221.x
Tan IY, Demchuk AM, Hopyan J, Zhang L, Gladstone D, Wong K, Martin M, Symons SP, Fox AJ, Aviv RI (2009) CT angiography clot burden score and collateral score: correlation with clinical and radiologic outcomes in acute middle cerebral artery infarct. AJNR Am J Neuroradiol 30(3):525–531. https://doi.org/10.3174/ajnr.A1408
Tung EL, McTaggart RA, Baird GL, Yaghi S, Hemendinger M, Dibiasio EL, Hidlay DT, Tung GA, Jayaraman MV (2017) Rethinking thrombolysis in cerebral infarction 2b: which thrombolysis in cerebral infarction scales best define near complete recanalization in the modern thrombectomy era? Stroke 48(9):2488–2493. https://doi.org/10.1161/STROKEAHA.117.017182
Klein S, Staring M, Murphy K, Viergever MA, Pluim JP (2010) elastix: a toolbox for intensity-based medical image registration. IEEE Trans Med Imaging 29(1):196–205. https://doi.org/10.1109/TMI.2009.2035616
Zaidat OO, Castonguay AC, Linfante I, Gupta R, Martin CO, Holloway WE, Mueller-Kronast N, English JD, Dabus G, Malisch TW, Marden FA, Bozorgchami H, Xavier A, Rai AT, Froehler MT, Badruddin A, Nguyen TN, Taqi MA, Abraham MG, Yoo AJ, Janardhan V, Shaltoni H, Novakovic R, Abou-Chebl A, Chen PR, Britz GW, Sun CJ, Bansal V, Kaushal R, Nanda A, Nogueira RG (2018) First pass effect: a new measure for stroke thrombectomy devices. Stroke 49(3):660–666. https://doi.org/10.1161/STROKEAHA.117.020315
Banks JL, Marotta CA (2007) Outcomes validity and reliability of the modified Rankin scale: implications for stroke clinical trials: a literature review and synthesis. Stroke 38(3):1091–1096. https://doi.org/10.1161/01.STR.0000258355.23810.c6
van Swieten JC, Koudstaal PJ, Visser MC, Schouten HJ, van Gijn J (1988) Interobserver agreement for the assessment of handicap in stroke patients. Stroke 19(5):604–607. https://doi.org/10.1161/01.str.19.5.604
Abd Elkhalek YI, Elia RZ (2016) Qualitative and quantitative value of hyperdense MCA sign as a prognostic marker for infarction. Egypt J Radiol Nucl Med 47(3):1043–1048. https://doi.org/10.1016/j.ejrnm.2016.06.005
Koo CK, Teasdale E, Muir KW (2000) What constitutes a true hyperdense middle cerebral artery sign? Cerebrovasc Dis 10(6):419–423. https://doi.org/10.1159/000016101
Donders AR, van der Heijden GJ, Stijnen T, Moons KG (2006) Review: a gentle introduction to imputation of missing values. J Clin Epidemiol 59(10):1087–1091. https://doi.org/10.1016/j.jclinepi.2006.01.014
Duffy S, McCarthy R, Farrell M, Thomas S, Brennan P, Power S, O’Hare A, Morris L, Rainsford E, MacCarthy E, Thornton J, Gilvarry M (2019) Per-pass analysis of thrombus composition in patients with acute ischemic stroke undergoing mechanical thrombectomy. Stroke 50(5):1156–1163. https://doi.org/10.1161/STROKEAHA.118.023419
Santos EM, Niessen WJ, Yoo AJ, Berkhemer OA, Beenen LF, Majoie CB, Marquering HA, MC investigators (2016) Automated entire thrombus density measurements for robust and comprehensive thrombus characterization in patients with acute ischemic stroke. PLoS ONE 11(1):e0145641. https://doi.org/10.1371/journal.pone.0145641
Zhou P, Li T, Jin J, Liu Y, Li B, Sun Q, Tian J, Zhao H, Liu Z, Ma S, Zhang S, Novakovic VA, Shi J, Hu S (2020) Interactions between neutrophil extracellular traps and activated platelets enhance procoagulant activity in acute stroke patients with ICA occlusion. EBioMedicine 53:102671. https://doi.org/10.1016/j.ebiom.2020.102671
Chalos V, van der Ende NAM, Lingsma HF, Mulder M, Venema E, Dijkland SA, Berkhemer OA, Yoo AJ, Broderick JP, Palesch YY, Yeatts SD, Roos Y, van Oostenbrugge RJ, van Zwam WH, Majoie C, van der Lugt A, Roozenbeek B, Dippel DWJ, Investigators MC (2020) National Institutes of Health Stroke Scale: an alternative primary outcome measure for trials of acute treatment for ischemic stroke. Stroke 51(1):282–290. https://doi.org/10.1161/STROKEAHA.119.026791
Young FB, Weir CJ, Lees KR, GITS Committee, and Investigators (2005) Comparison of the National Institutes of Health Stroke Scale with disability outcome measures in acute stroke trials. Stroke 36(10):2187–2192. https://doi.org/10.1161/01.STR.0000181089.41324.70
Santos EM, Yoo AJ, Beenen LF, Berkhemer OA, den Blanken MD, Wismans C, Niessen WJ, Majoie CB, Marquering HA, MC investigators (2016) Observer variability of absolute and relative thrombus density measurements in patients with acute ischemic stroke. Neuroradiology 58(2):133–139. https://doi.org/10.1007/s00234-015-1607-4
Compagne, KCJ, M Kappelhof, WH Hinsenveld, J Brouwer, RB Goldhoorn, M Uyttenboogaart, RPH Bokkers, WJ Schonewille, JM Martens, J Hofmeijer, HB van der Worp, RTH Lo, K Keizer, LSF Yo, ANGJ Lycklama, HM den Hertog, EJC Sturm, P Brouwers, MAA van Walderveen, MJH Wermer, SF de Bruijn, LC van Dijk, HD Boogaarts, EJ van Dijk, JH van Tuijl, JPP Peluso, PLM de Kort, B van Hasselt, PS Fransen, T Schreuder, RJJ Heijboer, SFM Jenniskens, MES Sprengers, E Ghariq, IR van den Wijngaard, SD Roosendaal, A Meijer, LFM Beenen, AA Postma, R van den Berg, AJ Yoo, PJ van Doormaal, MP van Proosdij, MGM Krietemeijer, DG Gerrits, S Hammer, JA Vos, J Boiten, JM Coutinho, BJ Emmer, A van Es, B Roozenbeek, Y Roos, WH van Zwam, RJ van Oostenbrugge, C Majoie, DWJ Dippel, A van der Lugt, and MCR Investigators (2022) Improvements in endovascular treatment for acute ischemic stroke: a longitudinal study in the MR CLEAN Registry. Stroke:STROKEAHA121034919. https://doi.org/10.1161/STROKEAHA.121.034919
Chen-Mayer HH, Fuld MK, Hoppel B, Judy PF, Sieren JP, Guo J, Lynch DA, Possolo A, Fain SB (2017) Standardizing CT lung density measure across scanner manufacturers. Med Phys 44(3):974–985. https://doi.org/10.1002/mp.12087
Funding
The MR CLEAN Registry was partly funded by the TWIN Foundation, Erasmus MC University Medical Center, Maastricht University Medical Center, and Amsterdam UMC.
Author information
Authors and Affiliations
Consortia
Contributions
AAEB, BJE and CBLM developed the study. AAEB and NA performed the data analysis. AAEB wrote the manuscript and is responsible for the overall content of the manuscript as the guarantor. BJE, CBLM and HAM contributed to the study design. NA, MK, BGD, JWH, JB, MLT, NAT, PRK and NB performed thrombus measurements and helped with data acquisition. YBWEMR, WHvZ, RB, JM, CBLM and BJE contributed to the clinical assessment of the data. HAM, CBLM and BJE contributed to the project supervision. All authors provided feedback and contributed to the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interests
Amsterdam UMC received funds from Stryker® for consultations by Dr. Majoie and Dr. Roos. Unrelated to this study, Amsterdam UMC received grants from the Netherlands Organization for Health Research and Development, Health Holland Top Sector LSH and Nicolab B.V. Erasmus University Medical Center received funds from Stryker®, Siemens Healthineers and GE Healthcare for consultations by Dr. van der Lugt and Dr. Dippel and Bracco Imaging® for consultation by Dr. Dippel. Maastricht University Medical Center received funds from Stryker®, Cerenovus, Nicolab B.V. and Philips for consultation by Dr. van Zwam. N. Arrarte Terreros received funding from the AMC medical Research B.V. P. Konduri is funded by INSIST: a European Union’s Horizon 2020 research and innovation program. Dr. Roos is minor shareholder of Nicolab B.V. Dr. Marquering is co-founder and shareholder of Nicolab B.V. Dr Majoie reports a grant from the TWIN Foundation. Unrelated to this study, Dr. Majoie is minor shareholder of Nicolab B.V. and reports grants from CVON/Dutch Heart Foundation, European Commission, Health Evaluation Netherlands, and Stryker, all paid to institution. The other authors have no conflicts of interest.
Ethics approval
The central medical ethics committee of the Erasmus MC gave permission to carry out the study as a registry (MEC-2014–235).[1] With this approval it was approved by the research board of each participating center. At UMC Utrecht, approval to participate in the study was obtained from their own research board and ethics committee. The need for individual patient consent has been waived.
Consent to participate
The need for individual patient consent has been waived.
Consent for publication
The need for individual patient consent has been waived, therefore consent for publication is not required.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A complete list of the MR CLEAN (Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke in the Netherlands) Registry investigators can be found in the Appendix at the end of the article.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bruggeman, A.A.E., Aberson, N., Kappelhof, M. et al. Association of thrombus density and endovascular treatment outcomes in patients with acute ischemic stroke due to M1 occlusions. Neuroradiology 64, 1857–1867 (2022). https://doi.org/10.1007/s00234-022-02971-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-022-02971-4