Abstract
Mechanical thrombectomy (MT) for acute ischemic stroke with medium vessel occlusions is still a matter of debate. We sought to identify factors associated with clinical outcome after MT for M2-occlusions based on data from the German Stroke Registry-Endovascular Treatment (GSR-ET). All patients prospectively enrolled in the GSR-ET from 05/2015 to 12/2021 were analyzed (NCT03356392). Inclusion criteria were primary M2-occlusions and availability of relevant clinical data. Factors associated with excellent/good outcome (modified Rankin scale mRS 0–1/0–2), poor outcome/death (mRS 5–6) and mRS-increase pre-stroke to day 90 were determined in multivariable logistic regression. 1348 patients were included. 1128(84%) had successful recanalization, 595(44%) achieved good outcome, 402 (30%) had poor outcome. Successful recanalization (odds ratio [OR] 4.27 [95% confidence interval 3.12–5.91], p < 0.001), higher Alberta stroke program early CT score (OR 1.25 [1.18–1.32], p < 0.001) and i.v. thrombolysis (OR 1.28 [1.07–1.54], p < 0.01) increased probability of good outcome, while age (OR 0.95 [0.94–0.95], p < 0.001), higher pre-stroke-mRS (OR 0.36 [0.31–0.40], p < 0.001), higher baseline NIHSS (OR 0.89 [0.88–0.91], p < 0.001), diabetes (OR 0.52 [0.42–0.64], p < 0.001), higher number of passes (OR 0.75 [0.70–0.80], p < 0.001) and intracranial hemorrhage (OR 0.26 [0.14–0.46], p < 0.001) decreased the probability of good outcome. Additional predictors of mRS-increase pre-stroke to 90d were dissections, perforations (OR 1.59 [1.11–2.29], p < 0.05) and clot migration, embolization (OR 1.67 [1.21–2.30], p < 0.01). Corresponding to large-vessel-occlusions, younger age, low pre-stroke-mRS, low severity of acute clinical disability, i.v. thrombolysis and successful recanalization were associated with good outcome while diabetes and higher number of passes decreased probability of good outcome after MT in M2 occlusions. Treatment related complications increased probability of mRS increase pre-stroke to 90d.
Similar content being viewed by others
Introduction
Over the past few years, several randomized trials have proven safety and efficacy of mechanical thrombectomy (MT) in large vessel occlusion (LVO) stroke, which are defined as occlusions in the intracranial internal carotid artery (ICA) and the M1 segment of the middle cerebral artery (MCA)1. For patients with LVO, MT has therefore been incorporated in the daily clinical practice of stroke centers, as well as in international guidelines1,2,3.
However, despite the substantial morbidity associated with medium vessel occlusions4,5 and emerging data suggesting that MT might also be safe and effective for medium vessel occlusions4,6 guidelines have not yet been clearly defined and MT has not been definitively established as standard of care. Due to the major advances in endovascular retriever and aspiration technology, MT has been recently emphasized by an international consensus as an encouraging option for medium and distal occlusions7 and is now increasingly performed in medium vessel occlusion strokes8. A recent meta-analysis of randomized trials (RCTs) on MT that also enrolled patients with M2 occlusions confirmed improved clinical outcome for patients receiving MT (n = 195) versus best medical management (n = 322)9. Furthermore, odds ratios for functional independence were reported for subgroups differentiated by perfusion mismatch and severity of initial symptoms. However, at present, the number of studies evaluating patient-specific factors associated with functional outcome of MT after medium and distal occlusions based on actual clinical experience is relatively low and included study populations are small10,11.
We therefore sought to identify baseline clinical, imaging, and MT factors associated with good clinical outcome after MT for M2 occlusions based on data from the German Stroke Registry-Endovascular Treatment (GSR-ET), a prospective multicenter registry representing real-world clinical experience.
Methods
This multi-center registry study was approved in accordance with the Declaration of Helsinki12 by the leading ethics committee of this multi-center registry in Munich (chamber of physicians at Ludwig-Maximillians University LMU, Munich (689-15)). Approval by local ethics committees or institutional review boards was obtained for all participating sites according to local regulations. The analysis was conducted in accordance with the Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis guidelines13. Patients, if capable, or their legal representatives, if available, were asked to provide written informed consent. All information was collected within clinical routine. Informed consent was obtained at the latest prior to the follow-up assessment 90 days after stroke.
Patients
All patients with anterior circulation stroke prospectively enrolled in the German Stroke Registry-Endovascular Treatment (GSR-ET) between June 2015 and December 2021 were analyzed. GSR-ET is an ongoing, open label, prospective, multicenter registry of 25 sites in Germany collecting consecutive patients undergoing MT (NCT03356392). A detailed description of the GSR-ET study design and the major findings have been published recently14,15. The main inclusion criteria of GSR-ET are diagnosis of acute ischemic stroke due to large vessel occlusion, initiation of an endovascular procedure for treatment, and age ≥ 18 years, according to national guidelines. There are no exclusion criteria. For this analysis, all patients with primary M2 occlusion, availability of baseline clinical data, neurological status at admission and 90 days, and recanalization status were included. Patients with multiple occlusions were excluded. Occlusion location was determined according to GSR-ET protocol with differentiation of MCA occlusions into proximal and distal M1 occlusions and M2 occlusions based on admission imaging and DSA findings. The data that support the findings of this study are available from the GSR-ET but restrictions apply to the availability of these data, which are not publicly available. The corresponding author has access to the registry data acquired in the above-mentioned enrolment period.
Statistics
Standard descriptive statistics were used for all study end points. Univariable distributions of metric variables were described with means/medians and interquartile range and categorical variables with absolute and relative frequencies. We aimed to identify baseline clinical, imaging, and MT factors associated with excellent functional outcome (defined as modified Rankin scale score (mRS) of 0–1 at day 90), good functional outcome (mRS of 0–2) and poor functional outcome/death (mRS of 5–6) at day 90. Successful recanalization was defined as Thrombolysis in Cerebral Infarction (TICI) ≥ 2b. Multivariable logistic regression analysis was performed to identify the independent predictors of excellent, good and poor functional outcome available at admission until directly after treatment. To further investigate the actual patient benefit associated with MT in M2 occlusions the increase of mRS pre-stroke to 90 days was calculated in a shift analysis. Ordinal logistic regression was used to identify factors associated with an increase in mRS points. Variables for regression models were selected using Akaike information criterion (AIC)-based backward selection. Odds ratios (OR) with 95% CI and p-values were calculated for selected variables. The effect of i.v. thrombolysis on the probability of reaching good clinical outcome (mRS ≤ 2) in M2 occlusions was furthermore evaluated in a logistic regression analysis stratified for administration of i.v. thrombolysis and successful recanalization, controlled for identified relevant covariates. Results including 95% CI were plotted with NIHSS at admission as independent variable.
Results
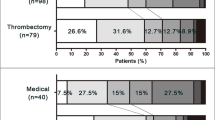
1348 patients fulfilled the inclusion criteria (Fig. 1). 1129 (84%) patients received a successful recanalization, 407 (30%) had excellent functional outcome and 595 (44%) had good functional outcome, while poor outcome and death was recorded for 402 (30%) of patients. Results of the descriptive statistical analysis are shown in Table 1. Patients with excellent (90d mRS 0–1) and good outcome (90d mRS 0–2) were younger (71y and 72y vs. 79y and 80y, p < 0.001), were less often treated with anti-coagulation (35% and 37% vs. 48% and 49%, p < 0.001), had a lower pre-stroke mRS (p < 0.001), had a lower NIHSS at admission (7 vs. 12, p < 0.001), had less often preexisting hypertension (71% and 72% vs. 82% and83%, p < 0.001), had less diabetes (16% and 17% vs. 26% and 27%, p < 0.01), had less preexisting atrial fibrillation (33% and 37% vs. 50% and 51%, p < 0.001), had higher ASPECTS (10 and 9 vs. 9 and 9, p < 0.01), were more often treated with thrombolysis (61% and 57% vs. 42% and 41%, p < 0.001), had more often conscious sedation instead of general anesthesia (30% and 28% vs. 22% and 22%, p < 0.01)were more often recanalized successfully (92% and 93% vs. 80% and 77%, p < 0.001) with fewer passes (1.7 and 1.7 vs. 2.1 and 2.2, p < 0.001). Time from symptom onset/last seen well to groin puncture was lower in patients with excellent (223 min vs. 250 min, p < 0.01) and good functional outcome (231 min vs. 248 min, p < 0.05). mRS increase pre-stroke to 90d was lower with + 0 and + 1 versus + 3 and + 3, p < 0.001.
Patients with poor outcome or death (90d mRS 5–6) were older (82y vs. 75y, p < 0.001), had a higher pre-stroke mRS (1 vs. 0, p < 0.001), had a higher NIHSS at admission (14 vs. 8, p < 0.001), were more often treated with anti-thrombotic medication (51% vs. 41%, p < 0.001) had more often preexisting hypertension (85% vs. 75%, p < 0.001) and diabetes (29% vs. 20%, p < 0.001), had more often atrial fibrillation (52% vs. 41%, p < 0.001), received less often i.v. thrombolysis (38% vs. 52%, p < 0.001), had more passes (2.2 vs. 1.9, p < 0.001), were less often recanalized successfully (71% vs. 89%, p < 0.001), had more dissections and perforations during treatment (6% vs. 2%, p < 0.01) and had higher rates of ICH during treatment (7% vs. 4%, p < 0.03) as well as higher rates of sICH at 24h (10% vs. 1%, p < 0.001). mRS-increase pre-stroke to 90d was higher with + 5 versus + 1, p < 0.001.
In patients with excellent outcome (90d mRS 0–1) the share of females was significantly lower (44% vs. 53%, p < 0.01), while in patients with poor outcome (90d mRS 5–6) the share of females was significantly higher (56% vs. 48%, p < 0.01). Furthermore, in patients with excellent outcome, the share of patients treated in the admission center was higher (74% vs. 67%, p < 0.01).
In multivariable logistic regression analysis (Fig. 2), probability of good outcome (mRS ≤ 2) was reduced by higher age (odds ratio [OR] 0.95 [95% confidence interval 0.94–0.95], p < 0.001), higher pre-stroke mRS (OR 0.36 [0.31–0.4], p < 0.001), higher baseline NIHSS (OR 0.89 [0.88–0.91], p < 0.001), comorbidity diabetes (OR 0.52 [0.42–0.64], p < 0.001), higher number of passages (OR 0.75 [0.70–0.80], p < 0.001), longer times from symptom onset/last seen well to groin puncture (OR 0.97 [0.96–0.99], p < 0.001), embolization and clot migration (OR 0.45 [0.27–0.76], p < 0.01) and intracranial hemorrhage (OR 0.26 [0.14–0.46], p < 0.001), while higher ASPECTS (OR 1.25 [1.18–1.32], p < 0.01), i.v. thrombolysis (OR 1.28 [1.07–1.54], p < 0.01) and successful recanalization (OR 4.27 [3.12–5.91], p < 0.001) increased the probability of good outcome. Correspondingly, probability of excellent outcome (mRS ≤ 1) was reduced with higher age (OR 0.96 [0.95–0.96], p < 0.001), ), higher pre-stroke mRS (OR 0.23 [0.19–0.29], p < 0.001), higher baseline NIHSS (OR 0.90 [0.88–0.91], p < 0.001), diabetes (OR 0.59 [0.47–0.74], p < 0.001), intracranial hemorrhage (OR 0.36 [0.18–0.68], p < 0.01), longer times from symptom onset/last seen well to groin puncture (OR 0.97 [0.95–0.98], p < 0.001) and higher number of passages (OR 0.77 [0.72–0.83], p < 0.001), while higher ASPECTS (OR 1.23 [1.16–1.31], p < 0.01), i.v. thrombolysis (OR 1.26 [1.04–1.53], p < 0.05) and successful recanalization (OR 3.17 [2.23–4.58], p < 0.001). In addition, excellent functional outcome was associated with dyslipidemia (OR 1.36 [1.13–1.63], p < 0.001), while atrial fibrillation (OR 1.82 [0.67–0.99], p < 0.05) reduces probability of excellent outcome.
Predictors of excellent, good and poor functional outcome after thrombectomy for M2 occlusions, multivariable logistic regression analysis. AE: Adverse events, ASPECTS: Alberta Stroke Program Early CT Score, CI: Confidence interval, mRS: modified Rankin Scale, NIHSS: National Institute of Health Stroke Scale, OR: Odds ratio, TICI: modified Thrombolysis in cerebral infarction.
Predictors of poor outcome and death after 90 days were higher age (OR 1.06 [1.05–1.06], p < 0.001), higher baseline mRS (OR 1.60 [1.50–1.71], p < 0.001), higher NIHSS at admission (OR 1.10 [1.09–1.12], p < 0.001), diabetes (OR 1.53 [1.28–1.82], p < 0.001), higher number of passages (OR 1.20 [1.14–1.26], p < 0.001), dissections and perforations (OR 1.65 [1.02–2.66], p < 0.05) and intracranial hemorrhage (OR 2.92 [1.90–4.50], p < 0.001). i.v. thrombolysis (OR 0.65 [0.56–0.76], p < 0.01), dyslipidemia (OR 0.78 [0.67–0.91], p < 0.01), higher ASPECTS (OR 0.88 [0.84–0.92], p < 0.001) and successful recanalization (OR 0.36 [0.29–0.45], p < 0.001) reduced risk of poor outcome.
Results from ordinal logistic on mRS increase pre-stroke to 90d suggest that higher age (OR 1.05 [1.05–1.06], p < 0.001), higher baseline NIHSS (OR 1.11 [1.10–1.12], p < 0.001), comorbidity diabetes (OR 1.53 [1.28–1.82], p < 0.001), higher number of passes (OR 1.18 [0.14–0.22], p < 0.001) and longer time from symptom onset/last seen well to groin puncture (OR 1.02 [1.01–1.03], p < 0.001) increase the risk of a mRS gain (per point). Furthermore, treatment related complications dissections and perforation (OR 1.59 [1.11–2.29], p < 0.05), clot migration and embolization (OR 1.67 [1.21–2.30], p < 0.01) and intracranial hemorrhage (OR 2.41 [1.71–3.40], p < 0.001) were associated with mRS gain pre-stroke to 90d. In contrast, lower baseline mRS (OR 0.60 [0.57–0.63], p < 0.001), i.v. thrombolysis (OR 0.73 [0.64–0.82], p < 0.001), dyslipidemia (OR 0.88 [0.78–0.99], p < 0.001) and successful recanalization (OR 0.38 [0.32–0.46], p < 0.001) were associated with lower risk of further neurological deterioration (Fig. 3).
Predictors of mRS increase pre-stroke to 90d after thrombectomy for M2 occlusions, multivariable ordinal logistic regression analysis. AE: Adverse events, ASPECTS: Alberta Stroke Program Early CT Score, CI: Confidence interval, mRS: modified Rankin Scale, NIHSS: National Institute of Health Stroke Scale, OR: Odds ratio, TICI: modified Thrombolysis in cerebral infarction.
Logistic regression analysis stratified for i.v. thrombolysis and recanalization success suggests that administration of i.v. thrombolysis increases probability of good outcome for all levels of initial neurological impairment. (Fig. 4A). Differentiation by recanalization success confirms these findings for patients with successful MT. At NIHSS at admission of 10, an increase of probability of good outcome from c. 40% to c. 60% was observed, equaling a 33% reduction of relative risk (Fig. 4B). In cases with TICI 0 to TICI 2a, i.v. thrombolysis might improve prognosis especially for patients with mild symptoms at admission, however, differences are not significant (Fig. 4C).
Probability of good outcome depending on recanalization status and i.v. thrombolysis in multivariable logistic regression analysis. All analysis were controlled for Age, pre-mRS, Diabetes, ASPECTS and number of passes. NIHSS: National Institute of Health Stroke Scale, mRS: modified Rankin Scale, TICI: modified Thrombolysis in cerebral infarction.
Discussion
Our registry study based on large scale clinical experience from prospectively enrolled patients showed that an older age, a higher baseline mRS, higher NIHSS at admission, preexisting diabetes and higher number of passes were strongly associated with lower chances of good clinical outcome and even higher risk of poor outcome and death at 90 days after MT for M2 occlusions. In comparison, a successful recanalization (TICI ≥ 2b) and i.v. thrombolysis were associated with higher chances of good clinical outcome at 3 months and a reduced risk for poor outcome. Ordinal logistic regression on mRS shift pre-stroke to 90 days suggests that treatment related complications like dissections, perforations, clot migration and embolization and intracranial hemorrhage are associated with higher mRS increase pre-stroke to 90d.
Descriptive statistics show that in patients with excellent outcome the share of females was significantly lower while in patients with poor outcome the share of females was significantly higher. However, this observation was not reflected in results of the multivariable regression analysis, suggesting that in our cohort female strokes might be associated with other risk factors, such as higher age.
Furthermore, in patients with excellent outcome, the share of patients treated in the admission center was higher.
Compared to results of recently published meta-analysis of randomized controlled trials including n = 195 patients receiving MT for M2 occlussions9, our clinical cohort was of higher age (77y vs. 71y) with similar rates of hypertension, dyslipidemia, atrial fibrillation and diabetes. Median NIHSS at admission in our cohort was 10 compared to 13 in the meta-analysis. However, our results suggest a lower rate of excellent outcome with 30% versus 52% and a lower rate of good outcome with 44% versus 68% in the RCT cohort. However, a direct comparison of functional outcomes is not possible as the authors did not provide information about recanalization success in the RCT cohort.
Predictors of good clinical outcome have been evaluated in MT for acute ischemic stroke with LVO15,16,17,18,19. Identified predictors for good clinical outcome in M2 occlusions are comparable to those suggested for LVO15,20. As previously reported by Wollenweber et al., predictors of good clinical outcome included younger age, smaller infarct size, lower stroke severity, alteplase use and reperfusion success. Correspondingly, in our cohort, younger age, higher ASPECTS, lower NIHSS at admission and successful recanalization were strongly associated with higher chances of good clinical outcome at 90 days after a MT for M2 occlusions. In comparison, Hulscher et al.10 did not identify admission NIHSS as a predictor of poor functional outcome in medium vessel occlusion patients treated with MT, while another study by Mokin et al.11 did find an association between baseline NIHSS and functional outcome. This association might therefore be more dependent on specific cohort characteristics, such as predefined inclusion criteria and center-specific treatment decisions21.
Recanalization rates of 84% in our study were slightly higher in comparison with previous reports of successful recanalization (final recanalization TICI score ≥ 2b) of 78% in a meta-analysis of M2 occlusions22. As it is known from LVO studies, our data also suggest that a higher number of recanalization attempts reduces the chance of good clinical outcome and even increases the chance for poor outcome after 90 days in MT for M2 occlusions23. The effect of the number of passes regarding safety and efficiency to recanalize medium vessel occlusions needs to be investigated in multicentric and larger cohorts.
It has been shown that one third of medium vessel occlusion stroke patients have a baseline NIHSS < 624. In our study only c. 20% of the patients presented with an NIHSS < 6. The subgroup of patients with mild symptoms was therefore smaller than expected. This can be explained by the fact that patients from the underlying registry data are not selected using pre-defined inclusion criteria and the decision to treat patients with M2 occlusion was made by the treating neurointerventionalist or neurologist. While cases with M2 occlusion and low clinical severity could more likely be managed only medically (and would therefore not be included in the registry), primary M2 occlusions with severe baseline NIHSS might be associated with higher willingness of neurointerventionalists for endovascular thrombectomy21,25.
Good clinical outcome at 90 days was achieved in 44% of the patients included in our study, which is below the range of rates reported in the literature for M2 occlusions between 56%11 and 62%22 but higher than rates reported for M1 occlusions.
Our results suggest that comorbidity diabetes is associated with lower chance of good outcome and increased risk of neurological deterioration. As diabetes is associated with microvascular dysfunction, higher rates of microangiopathy-related complications during treatment and post-interventional adverse events might be an explanation for our observations. It has been shown that higher blood glucose levels are associated with worse clinical outcome26, but the pathophysiological pathways are not fully understood yet. Recent studies suggest that higher blood glucose levels trigger increased edema formation and might thereby lead to worse functional outcome27,28. However, other pathways have been discussed as well: Higher serum glucose levels could alter vessel intima tissue and thrombus characteristics and lead to increased thrombogenicity. Also, higher serum glucose levels could negatively influence cellular metabolism and ischemic tolerance.
Furthermore, dyslipidemia was associated with higher probability of excellent outcome and lower risk for poor outcome and mRS increase pre-stroke to 90d. Although the role of dyslipidemia on recanalization success is not investigated in detail yet, it can be speculated that statins with their known positive effects on inflammatory processes in vessel walls might increase chances of successful recanalization and better prognosis.
It has previously been emphasized that the NIHSS and mRS scales are limited in their granularity and heavily focused on motor function and thus, unable to capture domain-specific impairment that often play a dominant role in medium vessel occlusion stroke-related disability24. Furthermore, based on a smaller area that is affected by ischemia, clinical outcomes can be expected to be better than in LVO stroke patients. Given the overall better prognosis, it has been proposed to consider more restrictive outcome measure such as excellent outcome or mRS shift analysis24. We therefore also evaluated predictors significantly associated with neurological deterioration based on point-wise shift in mRS to increase the granularity of the outcome measure and capture associations that might otherwise not be captured. Results suggest that treatment related complications are not fully captured by binarized outcome metrics but are significantly associated with mRS increase pre-stroke to 90d.
Results furthermore suggest that administration of i.v. thrombolysis in patients with M2 occlusions even in combination with MT might improve outcome, apart from the already assumed higher effectiveness of pharmacologic fibrinolysis for the smaller clot burdens of medium vessel occlusions compared to larger clot burdens of LVO29,30,31.
Our study has limitations. All clinical parameters including mRS, vessel occlusion status and location were site reported parameters that might suffer from site related bias due to limited interrater reliability. The study cohort was selected based on center assessments of the exact occlusion location. It is known that the exact anatomical M2 definition is a matter of debate. For MCA occlusions, the GSR-ET registry differentiates proximal M1, distal M1 and M2 occlusions. The study aims to identify factors leading to good or poor outcome in patients undergoing MT with medium and distal occlusions of the MCA in comparison to M1 occlusions, the study does not aim to proof safety and efficiency of a specific therapy. Due to numerous anatomical variants of the MCA, cohort definitions with exactly the same branching and vessel diameter parameters might not be possible. In addition, such cohort selected by narrow criteria would only reflect specific study settings but would not reflect clinical practice where treating physicians typically differentiate proximal, medium and distal vessel occlusions based on less narrow/specific criteria. Therefore, evaluations of outcomes of medium and distal vessel occlusions might be better generalizable to clinical practice if the in- and exclusion criteria of the study cohort match with the understanding and conduct in clinical practice. It therefore can be assumed that prospective registry data of real clinical cases ensures high consistency and generalizability of reported results to clinical practice. The registry does not include perfusion imaging results and collateral status, which are both predictors of outcome in ischemic stroke. However, perfusion imaging is not included in the standard of care in many centers. In addition, it has been shown that the predefined thresholds for penumbra and core segmentations might not reflect final infarct cores. However, the analysis includes ASPECTS scoring, which has been shown to be a valid predictor of outcome and a surrogate for the extend of the final infarct core.
Furthermore, only cases with availability of all required data points were included in the analysis. Exclusion of patients with missing data points (including lost to follow-up) might introduce bias to the reported results and might reduce generalizability of findings. Results from RCTs are needed to confirm our observations.
Three RCTs currently upcoming and enrolling (DISTAL, ESCAPE-MEVO and FRONTIER-AP) will further enhance the understanding of safety and efficiency of MT in medium and distal vessel occlusions.
Conclusion
Corresponding to results reported for LVO, younger age, low pre-stroke mRS, low severity of acute clinical disability, i.v. thrombolysis and successful recanalization were associated with good outcome while preexisting disability, diabetes and higher number of retrieval attempts decreased the probability of reaching a good functional status after MT for M2 occlusions. Treatment related complications were associated with higher risk of mRS shift towards increased neurological impairments versus pre-stroke.
Data availability
The data that support the findings of this study are available from the GSR-ET registry, but restrictions apply to the availability of these data, and so the data is not publicly available. Data are available from the corresponding author upon reasonable request and with permission of the GST-ER registry.
References
Goyal, M. et al. Endovascular thrombectomy after large-vessel ischaemic stroke: A meta-analysis of individual patient data from five randomised trials. Lancet 387(10029), 1723–1731 (2016).
Powers, W. J. et al. 2018 guidelines for the early management of patients with acute ischemic stroke: A guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 49(3), e46–e110 (2018).
Saver, J. L. et al. Stent-retriever thrombectomy after intravenous t-PA vs. t-PA alone in stroke. N. Engl. J. Med. 372(24), 2285–95 (2015).
Menon, B. K. et al. Efficacy of endovascular thrombectomy in patients with M2 segment middle cerebral artery occlusions: Meta-analysis of data from the HERMES Collaboration. J. Neurointerv. Surg. 11(11), 1065–1069 (2019).
Tian, H. et al. Influence of occlusion site and baseline ischemic core on outcome in patients with ischemic stroke. Neurology 92(23), e2626–e2643 (2019).
Grossberg, J. A. et al. Beyond large vessel occlusion strokes: Distal occlusion thrombectomy. Stroke 49(7), 1662–1668 (2018).
Saver, J. L. et al. Thrombectomy for distal, medium vessel occlusions: A consensus statement on present knowledge and promising directions. Stroke 51(9), 2872–2884 (2020).
Almekhlafi, M. et al. Endovascular treatment decisions in patients with M2 segment MCA occlusions. AJNR Am. J. Neuroradiol. 41(2), 280–285 (2020).
Sarraj, A. et al. Endovascular thrombectomy versus medical management in isolated M2 occlusions: Pooled patient-level analysis from the EXTEND-IA trials, INSPIRE, and SELECT studies. Ann. Neurol. 91(5), 629–639 (2022).
Hulscher, F. et al. Predictors of good clinical outcome after thrombectomy for distal medium vessel occlusions. World Neurosurg. 160, e566–e572 (2022).
Mokin, M. et al. Endovascular treatment of middle cerebral artery M2 occlusion strokes: Clinical and procedural predictors of outcomes. Neurosurgery 81(5), 795–802 (2017).
World Medical A. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 310(20), 2191–2194 (2013).
Collins, G. S. et al. Transparent reporting of a multivariable prediction model for individual prognosis or diagnosis (TRIPOD): The TRIPOD statement. The TRIPOD Group. Circulation 131(2), 211–219 (2015).
Alegiani, A. C. et al. Systematic evaluation of stroke thrombectomy in clinical practice: The German Stroke Registry Endovascular Treatment. Int. J. Stroke 14(4), 372–380 (2019).
Wollenweber, F. A. et al. Functional outcome following stroke thrombectomy in clinical practice. Stroke 50(9), 2500–2506 (2019).
Zaidat, O. O. et al. Health economic impact of first-pass success among patients with acute ischemic stroke treated with mechanical thrombectomy: A United States and European perspective. J. Neurointerv. Surg. 13(12), 1117–1123 (2021).
Flottmann, F. et al. Good clinical outcome decreases with number of retrieval attempts in stroke thrombectomy: Beyond the first-pass effect. Stroke 52(2), 482–490 (2021).
Nikoubashman, O. et al. True first-pass effect. Stroke 50(8), 2140–2146 (2019).
Rabinstein, A. A. et al. Factors that may contribute to poor outcome despite good reperfusion after acute endovascular stroke therapy. Int. J. Stroke 14(1), 23–31 (2019).
Meyer, L. et al. Early clinical surrogates for outcome prediction after stroke thrombectomy in daily clinical practice. J. Neurol. Neurosurg. Psychiatry 91(10), 1055–1059 (2020).
McDonough, R. et al. Patient-relevant deficits dictate endovascular thrombectomy decision-making in patients with low NIHSS scores with medium-vessel occlusion stroke. AJNR Am. J. Neuroradiol. 42(10), 1834–1838 (2021).
Chen, C. J. et al. Endovascular mechanical thrombectomy for acute middle cerebral artery M2 segment occlusion: A systematic review. World Neurosurg. 107, 684–691 (2017).
Garcia-Tornel, A. et al. When to stop. Stroke 50(7), 1781–1788 (2019).
Ospel, J. M. & Goyal, M. A review of endovascular treatment for medium vessel occlusion stroke. J. Neurointerv. Surg. 13(7), 623–630 (2021).
Cimflova, P. et al. Factors influencing thrombectomy decision making for primary medium vessel occlusion stroke. J. Neurointerv. Surg. 14(4), 350–355 (2022).
Kim, T. J. et al. Short-term glycemic variability and hemorrhagic transformation after successful endovascular thrombectomy. Transl. Stroke Res. 12, 968–975 (2021).
Broocks, G. et al. Elevated blood glucose is associated with aggravated brain edema in acute stroke. J. Neurol. 267(2), 440–448 (2020).
Broocks, G. et al. Ischemic lesion water uptake in acute stroke: Is Blood glucose related to cause and effect?. J. Stroke 21(3), 347–349 (2019).
Yoo, J. et al. Thrombus volume as a predictor of nonrecanalization after intravenous thrombolysis in acute stroke. Stroke 49(9), 2108–2115 (2018).
Kim, Y. D. et al. Time-dependent thrombus resolution after tissue-type plasminogen activator in patients with stroke and mice. Stroke 46(7), 1877–1882 (2015).
Xu, M. et al. Stroke outcomes in women: A population-based cohort study. Stroke 53(10), 3072–3081 (2022).
Acknowledgements
Authors acknowledge the German Stroke Registry (GSR) investigators and the GSR steering committee: Prof. Dr. med. Joachim Röther (Asklepios Klinik Altona, Hamburg); Prof. Dr. med. Bernd Eckert (Asklepios Klinik Altona, Hamburg); Dr. med. Michael Braun (Bezirkskrankenhaus Günzburg); Prof. Dr. med. Gerhard F. Hamann (Bezirkskrankenhaus Günzburg); PD Dr. med. Eberhard Siebert (Charité –Benjamin Franklin und Campus Charité); Prof. Dr. med. Christian Nolte (Charité –Benjamin Franklin und Campus Charité); Dr. med. Sarah Zweynert (Charité—Campus Virchow Klinikum, Berlin); Dr. med. Georg Bohner (Charité—Campus Virchow Klinikum, Berlin); Prof. Dr. med. Jörg Berrouschot (Klinikum Altenburger Land); Dr. med. Albrecht Bormann (Klinikum Altenburger Land); Dr. med. Christoffer Kraemer (Klinikum Lüneburg); PD Dr. med. Hannes Leischner (Klinikum Lüneburg); Dr. med. Jörg Hattingen (KRH Klinikum Nordstadt Hannover); Dr. med. Martina Petersen (Klinikum Osnabrück); Prof. Dr. med. Florian Stögbauer (Klinikum Osnabrück); PD Dr. med. Boeckh-Behrens (Klinikum r.d.Isar); Dr. med. Silke Wunderlich (Klinikum r.d.Isar); Dr. med. Alexander Ludolph (Sana Klinikum Offenbach); Dr. med. Karl-Heinz Henn (Sana Klinikum Offenbach); Prof. Dr. med. Christian Gerloff (UKE Hamburg-Eppendorf); Prof. Dr. med. Jens Fiehler (UKE Hamburg-Eppendorf); Prof. Dr. med. Götz Thomalla (UKE Hamburg-Eppendorf); Asklepios Klinik Altona, Hamburg (UKE Hamburg-Eppendorf); Dr. med. Anna Alegiani (Asklepios Klinik Altona, Hamburg); Dr. med. Maximilian Schell (UKE Hamburg-Eppendorf); PD Dr. med. Arno Reich (Uniklinik RWTH Aachen); Prof. Dr. med. Omid Nikoubashman (Uniklinik RWTH Aachen); Prof. Dr. med. Franziska Dorn (Uniklinik Bonn); Prof. Dr. med. Gabor Petzold (Uniklinik Bonn); Prof. Dr. med. Jan Liman (Klinikum Nürnberg); Dr. med. Jan Hendrik Schäfer (Uniklinik Frankfurt/ Main); Dr. med. Fee Keil (Uniklinik Frankfurt/ Main); Prof. Dr. med. Klaus Gröschel (Universitätsmedizin Mainz); Dr. med. Timo Uphaus (Universitätsmedizin Mainz); Prof. Dr. med. Peter Schellinger (Universitätsklinik Johannes Wesling Klinikum Minden); Prof. Dr. Jan Borggrefe (Universitätsklinik Johannes Wesling Klinikum Minden); Dr. med. Steffen Tiedt (Uniklinik München (LMU)); PD Dr. med. Lars Kellert (Uniklinik München (LMU)); PD Dr. med. Christoph Trumm (Uniklinik München (LMU)); Prof. Dr. med. Ulrike Ernemann (Universitätsklinik Tübingen); PD Dr. med. Sven Poli (Universitätsklinik Tübingen); Prof. Dr. med. Christian Riedel (Universitätsmedizin Göttingen); PD Dr. med. Marielle Sophie Ernst (Universitätsmedizin Göttingen).
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Consortia
Contributions
H.K. Designed and conceptualized the study, major role in interpretation of data, performed statistical analysis, drafted the manuscript, figures, and tables, revised the manuscript for intellectual content; L.M. Acquisition and interpretation of data, revised the manuscript for intellectual content; G.B. Acquisition and interpretation of data, revised the manuscript for intellectual content; M.B. Acquisition and interpretation of data, revised the manuscript for intellectual content; H.G. Acquisition and interpretation of data, revised the manuscript for intellectual content; L.W. Acquisition and interpretation of data, revised the manuscript for intellectual content; C.B. Acquisition and interpretation of data, revised the manuscript for intellectual content; F.F. Acquisition and interpretation of data, revised the manuscript for intellectual content; M.D. Acquisition and interpretation of data, revised the manuscript for intellectual content; A.A. Acquisition and interpretation of data, revised the manuscript for intellectual content; G.T. Acquisition and interpretation of data, revised the manuscript for intellectual content; U.H. Acquisition and interpretation of data, revised the manuscript for intellectual content; J.F. Acquisition and interpretation of data, revised the manuscript for intellectual content; S.G. Designed, conceptualized and supervised the study, major role in interpretation of data, drafted the manuscript, revised the manuscript for intellectual content.
Corresponding author
Ethics declarations
Competing interests
Helge Kniep and Fabian Flottmann are consultants for Eppdata GmbH. Helge Kniep is shareholder of Eppdata GmbH. Milani Deb-Chatterji has received research grants from the Werner Otto Stiftung and serves in the advisory board of the PRECIOUS Trial. Götz Thomalla received fees as consultant from Acandis, Boehringer Ingelheim, Bayer, and Portola, and fees as lecturer from Acandis, Alexion, Amarin, Bayer, Boehringer-Ingelheim, BMS/Pfizer, Daiichii Sankyo and Portola. He serves in the board of the TEA Stroke Study and of ESO. Jens Fiehler is consultant for Cerenovus, Medtronic, Microvention, Penumbra, Phenox, Roche and Tonbridge. He serves in the advisory board of Stryker and Phenox. He is stock holder of Tegus Medical, Eppdata and Vastrax. He serves as Associate Editor at JNIS. All other authors have nothing to declare.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kniep, H., Meyer, L., Broocks, G. et al. Predictors of functional outcome after thrombectomy for M2 occlusions: a large scale experience from clinical practice. Sci Rep 13, 18740 (2023). https://doi.org/10.1038/s41598-023-45232-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-023-45232-x
- Springer Nature Limited