Abstract
Introduction
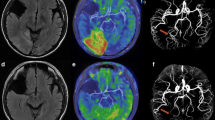
The exact mechanism of the mitochondrial myopathy, encephalopathy, lactic acidosis and stroke-like episodes (MELAS) remain unclear. Diffusion-weighted imaging (DWI) is a magnetic resonance (MR) imaging technique for studying the pathophysiologic change of the MELAS. The purpose of the study is to see whether the apparent diffusion coefficient (ADC) of MELAS in the non-affected areas is different from the ADC of the normal subjects and to speculate the pathophysiological mechanisms of the MELAS.
Methods
Sixteen cases of MELAS were retrospectively analyzed. Thirty healthy subjects were chosen to constitute the control group. All of them were performed on the 3.0T whole-body MR scanner with axial view T2 fluid attenuated inversion recovery (flair), T2-weighted imaging, T1flair, and DWI. An ADC map was reconstructed in the workstation. Two to five regions of interest were put in the non-affected frontal lobe and basal ganglia. All data took statistical analysis.
Results
There were significant differences between the ADC of the patients with MELAS and the controls in the non-affected areas, including the superior frontal gyrus, precentral gyrus, corpus striatum, thalamus, and white matter of the semi-oval centrum.
Conclusion
ADCs in the non-affected areas of the patients with MELAS are higher than those of the normal subjects. Pathological changes take place in the non-affected areas of the patients with MELAS.


Similar content being viewed by others
References
Pavlakis SG, Philips PC, DiMauro S et al (1984) Mitochondrial myopathy, encephalopathy, lactic acidosis, and strokelike episodes: a distinctive clinical syndrome. Ann Neurol 16:481–488
DiMauro S, Schon EA (2003) Mitochondrial respiratory-chain diseases. N Engl J Med 348:2656–2668
Hanna MG, Nelson IP, Morgan-Hughes JA et al (1998) MELAS: a new disease associated mitochondrial DNA mutation and evidence for further genetic heterogeneity. J Neurol Neurosurg Psychiatry 65:512–517
Rosen L, Phillips S, Enzmann D (1990) Magnetic resonance imaging in MELAS syndrome. Neuroradiology 32:168–171
Miyamoto A, Oki J, Takahashi S et al (1997) Serial imaging in MELAS. Neuroradiology 39:427–430
Castillo M, Kwock L, Green C (1995) MELAS syndrome: imaging and proton MR spectroscopic findings. Am J Neuroradiol 16:233–239
Stejskal EO, Tanner JE (1965) Spin diffusion measurements: spin echoes in the presence of a time dependent field gradient. J Chem Phys 42:288–292
Calvet D, Touzé E, Oppenheim C et al (2009) DWI lesions and TIA etiology improve the prediction of stroke after TIA. Stroke 40:187–192
Di Bonaventura C, Bonini F, Fattouch J et al (2009) Diffusion-weighted magnetic resonance imaging in patients with partial status epilepticus. Epilepsia 50(suppl 1):45–52
Schaefer PW, Buonanno FS, Gonzalez RG et al (1997) Diffusion-weighted imaging discriminates between cytotoxic and vasogenic edema in a patient with eclampsia. Stroke 28:1082–1085
Wang XY, Noguchi K, Takashima S (2003) Serial diffusion-weighted imaging in a patient with MELAS and presumed cytotoxic edema. Neuroradiology 45:640–643
Michelson DJ, Ashwal S (2004) The pathophysiology of stroke in mitochondrial disorders. Mitochondrion 4:665–674
Ohshita T, Oka M, Imon Y et al (2000) Serial diffusion-weighted imaging in MELAS. Neuroradiology 42:651–656
Pavlakis SG, Kingsley PB, Kaplan GP et al (1998) Magnetic resonance spectroscopy use in monitoring MELAS treatment. Arch Neurol 55:849–852
Iizuka T, Sakai F, Ide T et al (2007) Regional cerebral blood flow and cerebrovascular reactivity during chronic stage of stroke-like episodes in MELAS—implication of neurovascular cellular mechanism. J Neurol Sci 257:126–138
Ohama E, Ohara S, Ikuta F et al (1987) Mitochondrial angiopathy in cerebral blood vessels of mitochondrial encephalomyopathy. Acta Neuropathol (Berl) 74:226–233
Takahashi N, Shimada T, Murakami Y et al (2005) Vascular involvement in a patient with mitochondrial myopathy, encephalopathy, lactic acidosis, and stroke-like episodes. Am J Med Sci 329:265–266
Betts J, Jaros E, Perry RH et al (2006) Molecular neuropathology of MELAS: level of heteroplasmy in individual neurones and evidence of extensive vascular involvement. Neuropathol Appl Neurobiol 32:359–373
Tanahashi C, Nakayama A, Yoshida M et al (2000) MELAS with the mitochondrial DNA 3243 point mutation: a neuropathological study. Acta Neuropathol 99:31–38
Tsuchiya K, Miyazaki H, Akabane H et al (1999) MELAS with prominent white matter gliosis and atrophy of the cerebellar granular layer: a clinical, genetic, and pathological study. Acta Neuropathol 97:520–524
Ito H, Mori K, Harada M et al (2008) Serial brain imaging analysis of stroke-like episodes in MELAS. Brain Dev 30:483–488
Oppenheim C, Galanaud D, Samson Y et al (2000) Can diffusion weighted magnetic resonance imaging help differentiate stroke from stroke-like events in MELAS? J Neurol Neurosurg Psychiatry 69:248–250
Iizuka T, Sakai F, Suzuki N (2002) Neuronal hyperexcitability in stroke-like episodes of MELAS syndrome. Neurology 59:816–824
Kaufmann P, Shungu DC, Sano MC et al (2004) Cerebral lactic acidosis correlates with neurological impairment in MELAS. Neurology 62:1297–1303
Molnár MJ, Valikovics A, Molnár S et al (2000) Cerebral blood flow and glucose metabolism in mitochondrial disorders. Neurology 55:544–548
Iizuka T, Sakai F (2005) Pathogenesis of stroke-like episodes in MELAS: analysis of neurovascular cellular mechanisms. Curr Neurovasc Res 2:29–45
Reulen HJ (1976) Vasogenic brain oedema: new aspects in its formation, resolution and therapy. Br J Anaesth 48:741–752
Stummer W (2007) Mechanisms of tumor-related brain edema. Neurosurg Focus 22:E8
Möller HE, Kurlemann G, Pützler M et al (2005) Magnetic resonance spectroscopy in patients with MELAS. J Neurol Sci 229–230:131–139
Lindroos MM, Borra RJ, Parkkola R et al (2009) Cerebral oxygen and glucose metabolism in patients with mitochondrial m.3243A > G mutation. Brain 132:3274–3284
Gilchrist JM, Sikirica M, Stopa E et al (1996) Adult-onset MELAS. Evidence for involvement of neurons as well as cerebral vasculature in strokelike episodes. Stroke 27:1420–1423
Katayama Y, Maeda K, Iizuka T et al (2009) Accumulation of oxidative stress around the stroke-like lesions of MELAS patients. Mitochondrion 9:306–313
Sparaco M, Simonati A, Cavallaro T et al (2003) MELAS: clinical phenotype and morphological brain abnormalities. Acta Neuropathol 106:202–212
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Liu, Z., Liu, X., Hui, L. et al. The appearance of ADCs in the non-affected areas of the patients with MELAS. Neuroradiology 53, 227–232 (2011). https://doi.org/10.1007/s00234-010-0729-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-010-0729-y