Abstract
Purpose
To develop and validate a population pharmacokinetic model of ciprofloxacin intravenously in critically ill patients, and determine target attainment to provide guidance for more effective regimens.
Methods
Non-linear mixed-effects modelling was used for the model development and covariate analysis. Target attainment of an ƒAUC0–24/MIC ≥ 100 for different MICs was calculated for standard dosing regimens. Monte Carlo simulations were performed to define the probability of target attainment (PTA) of several dosing regimens.
Results
A total of 204 blood samples were collected from 42 ICU patients treated with ciprofloxacin 400–1200 mg/day, with median values for age of 66 years, APACHE II score of 22, BMI of 26 kg/m2, and eGFR of 58.5 mL/min/1.73 m2. The median ƒAUC0–24 and ƒCmax were 29.9 mg•h/L and 3.1 mg/L, respectively. Ciprofloxacin pharmacokinetics were best described by a two-compartment model. We did not find any significant covariate to add to the structural model. The proportion of patients achieving the target ƒAUC0–24/MIC ≥ 100 were 61.9% and 16.7% with MICs of 0.25 and 0.5 mg/L, respectively. Results of the PTA simulations suggest that a dose of ≥ 1200 mg/day is needed to achieve sufficient ƒAUC0–24/MIC ratios.
Conclusions
The model described the pharmacokinetics of ciprofloxacin in ICU patients adequately. No significant covariates were found and high inter-individual variability of ciprofloxacin pharmacokinetics in ICU patients was observed. The poor target attainment supports the use of higher doses such as 1200 mg/day in critically ill patients, while the variability of inter-individual pharmacokinetics parameters emphasizes the need for therapeutic drug monitoring to ensure optimal exposure.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Patients admitted to the intensive care unit (ICU) often need antibiotic therapy to treat infections. Timely and adequate antimicrobial treatment is essential for good clinical outcome, preventing the spread of antibiotic resistance and containing the economic impact of infections [1,2,3,4]. ICU patients represent a highly heterogeneous population with significant differences in the distribution of patients’ ages, severities of illness, durations of admission, and outcomes [5]. Due to the large variability in these patients, a “one-dose-fits-all” approach seems undesirable. Furthermore, dosing of many antibiotics was designed in an era with more susceptible micro-organisms and in healthy volunteers or patients with mild to moderate severities of illness, with reasonably predictable pharmacokinetic (PK) parameters. The pathophysiological changes in critically ill patients can cause substantial PK changes, such as an increased volume of distribution, decreased protein binding, and changes in elimination rate [6,7,8]. PK changes in critically ill patients often result in insufficient exposure, which may contribute to inadequate bacterial eradication, an increased chance of antibiotic resistance, and excess morbidity and mortality rates [8,9,10,11].
Ciprofloxacin, a fluoroquinolone antibiotic, has a wide spectrum of antimicrobial activity and is frequently used for various infections as monotherapy or in combination with other antibiotics [12]. The bactericidal action of ciprofloxacin is characterized by a rapid concentration-dependent activity against many gram-negative aerobic bacteria and to a lesser extent against gram-positive bacteria [13]. Ciprofloxacin is eliminated by various mechanisms (renal, hepatic, and transintestinal) [14].
The ratio of the area under the drug serum concentration–time curve over 24 h at steady state and the minimal inhibitory concentration (AUC0–24/MIC) is a good predictor for ciprofloxacin efficacy. The pharmacodynamic target (PDT) for optimal outcome for ciprofloxacin is AUC0–24/MIC ≥ 125, or ≥ 100 for the unbound (free) drug concentration (ƒAUC0–24/MIC) [11, 15,16,17]. The probabilities of microbiological and clinical cure for ciprofloxacin AUC0–24/MIC < 125 are poor (26% and 42%, respectively), compared with AUC0–24/MIC ≥ 125 where the probabilities are 80% (p < 0.005) and 82% (p < 0.001), respectively [15]. In addition, Cmax/MIC ratio 8–10 is suggested to be particularly important to prevent the emergence of resistance [18]. However, it is a challenging task to formulate general dose adjustments for critically ill patients and a validated approach for dose adjustment is not currently available. Therapeutic drug monitoring (TDM) combined with a population pharmacokinetic (popPK) model can be used to interpret the complex PK in critically ill patients and support in optimizing individual dosing to improve attainment of the predefined targets. To date, different ciprofloxacin popPK models have been developed for ICU patients [14, 19,20,21,22,23]. In most models, the study populations were exposed to daily doses of ≤ 1200 mg/day, and in only three models Monte Carlo simulations were performed to define dosing regimens that increase the probability of target attainment (PTA) [14, 23, 24]. The current study is one of the largest multi-centre trials describing detailed ciprofloxacin population pharmacokinetics in ICU patients. In contrast to the majority of the previous studies, pharmacokinetic data was obtained based on data from a broad dosage range (400–1200 mg).
The objective of this study was to develop a popPK model to determine inter-individual PK variability, the influence of patient characteristics, and the PTA of different high dosing regimens using Monte Carlo simulations in ICU patients. Furthermore, the model in the current study is described in detail and comprehensively validated. Such knowledge is essential for implementing model-based dosing to optimize ciprofloxacin exposure in critically ill patients.
Methods
Study design and population
The popPK model for ciprofloxacin was developed based on data from a two-centre, prospective, observational PK/PD study in the ICU departments of the Erasmus Medical Centre and Maasstad Hospital, Rotterdam, the Netherlands (EXPAT study). All patients admitted to the ICU between January and December 2016 and treated with ciprofloxacin were assessed for inclusion. Eligible for enrolment were patients aged ≥ 18 years, receiving intravenous ciprofloxacin, and treatment aimed for at least 3 days. Exclusion criteria were antibiotic cessation before sampling and burn wound patients admitted to the ICU. The initiation of ciprofloxacin, dosage, and duration of therapy were at the discretion of the attending physician.
Blood sampling and assays
On day two after start of ciprofloxacin administration, blood samples were collected before administration (trough concentration), 15–30 min after the end of the infusion (peak concentration), 1 and 3 h after infusion, and just before the start of the next dose (second trough concentration). The exact sampling time and the dosage administered were recorded. Blood samples were stored at 2–8 °C to maintain integrity, and centrifuged at 3000 rpm for 6 min within 24 h of collection. The plasma was transferred to cryo-vials for frozen storage (− 80 °C) until analysis. Plasma concentrations were determined by a multi-analyte UPLC-MS/MS. The calibration curves were linear from 0.04 up to 5.0 mg/L, giving a correlation coefficient r2 = 0.999. Samples with a concentration above 5.0 mg/L were diluted according to a standard dilution protocol. The method was comprehensively validated according to the Food and Drug Administration (FDA) guidance on bioanalytical method validation [25]. Observed concentrations were corrected for protein binding (ƒAUC = AUC ∙ 0.7), using an average plasma protein binding (PPB) value of 30% in critically ill patients [26, 27].
Model building
The popPK model was built by using non-linear mixed-effect modelling (NONMEM®, version 7.2, ICON Development Solutions, Ellicott City, MD, USA). The graphical user interface (GUI) Pirana [28] (version 2.7.0) was used for model management, execution, output generation, and interpretation of results. Pirana was also used as the GUI for PSN (version 4.7.0) and Xpose (version 4.5.3), and R-studio was used in combination with Pirana for graphical visualization. The data were analyzed using the first-order conditional estimation method with interaction (FOCE-I).
Structural model
For the initial popPK model, one-, two-, and three-compartment models were tested to fit the ciprofloxacin plasma concentration data and calculate the clearance (CL), volume of distribution of the central and peripheral compartment (respectively Vc and Vp), and the transfer of ciprofloxacin between the central and peripheral compartment (Q). The model quality and the selection were based on the precision with which the model parameters were estimated, objective function value (OFV), shrinkage values, and visual inspection of the goodness-of-fit-plots. The inter-individual variability (IIV) was estimated on each parameter by using an exponential model. For these parameters, the shrinkage was also calculated to identifying and quantifying whether an overfit is taking place. A shrinkage below 20% was considered acceptable [29]. The residual variability was incorporated as a combined proportional and additive model. The IIV of the parameters, for example clearance, can be described by the following equation:
CLj is the clearance of the jth individual and it is described by the clearance of the mean population (CLpop) and variability of mean clearance and the clearance of the jth individual (ηCL). ηCL is normally distributed with an average of zero and a variance of ω2, shortly noted as η = N(0,ω2). To further refine the model, the omega block option was used for assessment of covariance between random effects.
Covariate analysis
After the selection of the structural model, covariates were added to the model. These covariates were selected based on the possibility that they could explain the IIV in parameter estimates. This was based on relevant physiological and clinical explanations or evidence from previous research [14, 19,20,21, 30]. Covariates that were tested were serum creatinine, estimated glomerular filtration rate (eGFR), serum albumin, body mass index (BMI), weight, sex, renal replacement therapy (RRT), and age. The continuous covariates were normalized to the population median and the categorical covariates were transformed to binary covariates, respectively Eqs. 2 and 3.
θi represents the individual predicted value of any parameter calculated by the model with a covariate value covi. θpop represents the population estimate for θi, covm is the median covariate value, and θcov is the covariate effect. For Eq. 3, the covariate value is either 1 or 0. The covariates were individually added to the model and then deleted one by one according to the forward inclusion-backward elimination method [31]. For the initial covariate step, a decrease in OFV of at least 3.84 (p < 0.05 with 1 degree of freedom) from the structural model was required for the covariate to be included. Subsequently, all significant covariates were included simultaneously to the structural model and were deleted one by one. A stricter statistical significance of p < 0.001 was applied in the backward elimination step (OFV > 10.83).
Model evaluation
The evaluation of the model was done using statistical and graphical tools, including goodness-of-fit plots. Furthermore, the robustness of parameter estimates from the final model was tested using a bootstrap analysis. For the bootstrap, the dataset was resampled 1000 times to asses if the model was appropriate. Visual predictive checks (VPCs) were executed to evaluate the model [32]. A normalized prediction distribution error (NPDE) analysis, which is a simulation-based diagnostic tool that can be used to evaluate models which have different dosage regimens, was also used to evaluate the final model [33].
Pharmacodynamic target
To calculate the ƒAUC0–24/MIC and ƒCmax/MIC ratios, the clinical breakpoint of 0.5 mg/L from the EUCAST database was used [34]. This is the highest MIC from which it can be expected that ciprofloxacin under standard conditions is effective for Enterobacteriaceae, Pseudomonas spp., Acinetobacter spp., Haemophilus influenzae, Moraxella catarrhalis, and Neisseria spp. [34]. To assess the suitability of the empirical fixed dosing regimens considering ƒAUC0–24/MIC ≥ 100 and ƒCmax/MIC ≥ 8, a MIC distribution of 0.0312–8 mg/L was tested. For the targeted treatment at different MICs, the wild-type population distribution of Pseudomonas aeruginosa and the epidemiological cut-off (ECOFF) value from the EUCAST database were used [34].
Dosing simulations
To generate data for target attainment analyses, Monte Carlo simulations (n = 5000) were performed to define the PTA for ciprofloxacin 400 mg twice daily (q12h), three times daily (q8h), four times daily (q6h), 600 mg q12h, and q8h for the non-protein bound fraction using MicLab236b (Medimatics, Maastricht, the Netherlands). Monte Carlo simulations use a simulation platform to expand the sample size of a study to provide predictions of the likely result of different therapeutic approaches, such as altered drug dose or frequency, on the achievement of therapeutic targets [35].
Results
Study population
A total of 42 patients were included. Among these patients, the prescribed daily dose was 400 mg q24h in 3 patients, 400 mg q12h in 25 patients, and 400 mg q8h in 14 patients, administered as an infusion over 30–60 min. In total, 204 plasma concentrations were available, an average of 4.9 samples per patient. Other baseline characteristics of the study population were median eGFR 58.5 mL/min/1.73 m2, albumin 25 g/L, C-reactive protein 139.5 mg/L, Acute Physiology and Chronic Health Evaluation (APACHE) II score 22, Sequential Organ Failure Assessment (SOFA) score 13, and a mortality rate at day 30 of 23.8%. A summary of baseline patient characteristics is presented in Table 1.
Pharmacokinetic parameters
Box and whiskers plots of plasma ƒCmin, ƒCmax, and ƒAUC0–24 for the different dosing groups are shown in Fig. 1. Plots of the total trough and peak plasma concentrations are presented in the Supplemental material (Fig. S1). In the 400 mg q24h, q12h, and q8h groups, the mean ƒCmax were 3.10, 3.02, and 3.05 mg/L, respectively, and the mean ƒAUC0–24 were 26.6, 34.2, and 46.8 mg•h/L, respectively.
Box (median, 25th and 75th percentiles) and whisker (10th and 90th percentiles) plots of free (a) trough (ƒCmin), (b) peak (ƒCmax) plasma concentrations, and (c) area under the plasma concentration versus time curves (ƒAUC0–24) of ciprofloxacin observed in severely ill patients treated with 400 mg one (q24h), two (q12h), and three (q8h) times daily. Filled circles are outliers
Final model
The data was best described by a two-compartment model and the residual error was described by a combined additive and proportional error model. IIV was included on CL, Vc, and Q and significantly improved the model (p < 0.05). The omega block construction between CL and Vc was found to improve the model and was maintained during the model building process. The parameter estimations of the final model are presented in Table 2. The mean serum elimination half-life was 6.96 h.
Covariate analysis
The base two-compartment model with IIV on CL, Vc, and Q was used as a reference model for the covariate analysis. After graphically selecting covariates for analysis, a forward selection of covariates followed by a backward elimination was carried out. None of the covariates were found to correlate significantly.
Model evaluation
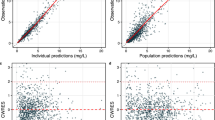
The population predictions and individual predictions of the final model were evenly distributed around the line of unity when plotted against the observations, as shown in Fig. 2. The conditional weighted residuals were normally distributed over the x-axis when plotted against the time after dose and concentration (Fig. 2). To assess the uncertainty of parameters, a bootstrap analysis with 1000 runs was performed to calculate the 95% percentile range of the final PK parameters. The median values and 95% CIs of the performed bootstrap analysis are shown in Table 2. The VPC of the final model showed good model predictability. The median observations, represented by the red line in the middle, were lying within the 95% CI of the model predictions, represented by the red shaded areas, thereby demonstrating adequate fit of the model (Fig. 3). The NPDE analysis are illustrated in the Supplement material, both graphs in Fig. S2 did not deviate significantly from a normal distribution and with the majority of the NPDEs lying between the values − 2 and 2, the model was considered appropriate.
Goodness-of-fit plots of the final model. (a) Observed concentration (OBS) plotted against predicted concentration (PRED). (b) OBS plotted against the individual predicted concentration (IPRED). (c) Conditional weighted residuals plotted against time after dose. (d) CWRES plotted against PRED. The line in A and B represents the line of identity
Observed ciprofloxacin concentration–time data and the visual predictive check (VPC) of the final model. The blue brackets are the observed concentrations. The red line is the observed median and the two blue lines are the 5th and 95th percentiles of the observed data. The red shaded area is the 95% CI of the model-predicted median and the blue shaded areas are the 95% CIs of the model-predicted 5th and 95th percentiles
Pharmacodynamic target attainment
The percentage of patients achieving the PDT ƒAUC0–24/MIC ≥ 100 and ƒCmax/MIC ≥ 8 in the three different ciprofloxacin intravenous dosing regimens groups were calculated for different MIC values (Supplemental Fig. S3). Of all patients, for the breakpoints 0.25 and 0.5 mg/L, the ƒAUC0–24/MIC ≥ 100 target was achieved in 61.9% and 16.7% of the patients, respectively. Although there was a difference in achieving the PDT between 400 mg q12h (12.0%) and q8h (28.6%) groups for the breakpoint 0.5 mg/L, this numerical difference did not reach statistical significance (p = 0.19). This can be explained by the large variation and overlap of the ƒAUC0–24 in both dosing groups (Fig. 1C). In addition, there was significant difference in baseline eGFR between the three dose groups. The median eGFR was 28.0, 52.0, and 82.5 mL/min/1.73 m2 for the 400 mg q24h, q12h, and q8h groups, respectively. Furthermore, the ƒCmax/MIC concentration ratios of ≥ 8 for the breakpoint of 0.25 and 0.5 mg/L were realized in 34 (81.0%) and 11 (26.2%) of patients, respectively.
Dosing simulations
The popPK parameters from the final model were used to conduct Monte Carlo simulations to assess the target attainment. Figure 4 shows the ƒAUC0–24/MIC ≥ 100 as a function of the MIC for several dosing regimens. In order to achieve optimal exposure (ƒAUC0–24/MIC ≥ 100) at an MIC of 0.5 mg/L, a dose of 1200 mg/day was required on average (Fig. 4C–E). Since the 95% and 99% CIs are wide, even in the highest dosage regimes, a substantial proportion of the population does not achieve the PDT.
Discussion
In this study, we present the results of intravenous ciprofloxacin PK modelling in 42 critically ill patients. Our popPK model of ciprofloxacin was best described by a two-compartment model, similar to previous studies [14, 19, 21, 23]. The final model was comprehensively evaluated by using NPDE analysis and VPCs. Our ICU population is very heterogeneous, with a great variety of primary diagnosis, and clinical and biological characteristics (Table 1). This variability is represented in the model by the relatively high IIV. The high IIV in Vc cannot be explained by fluid shifts, since ciprofloxacin volume of distribution in critically ill patients does not change over time [36]. Van Zanten et al. [21] also found up to fivefold differences in volumes of distribution. However, they concluded that patient biometry or excessive volume loading could not explain the differences in volumes of distribution.
Various covariates that could provide information on PK of ciprofloxacin in critically ill patients were tested. However, at the end of the model-building process, no significant covariates were found on Vc, CL, and Q. The lack of significant covariates can partly be explained by the high variability in the PK of ciprofloxacin in ICU patients as recurrently described in the literature [15, 19,20,21]. The estimated renal function in our population has a wide distribution, due to the presence of patients with and without acute or chronic kidney injury, and RRT (Table 1). Nevertheless, both impaired renal function and the presence of CVVH did not have a significant influence on the model and were not incorporated in the final model as a covariates. This implies that plasma ciprofloxacin exposure cannot be predicted by using serum creatinine in our ICU population. Using the creatinine to estimate renal function is known to poorly predict actual renal function, as it is affected by factors other than renal function [37]. However, in other popPK studies, the creatinine clearance was found to be a significant relevant covariate [19, 20]. Variability in ICU population characteristics (e.g. admission diagnosis and disease state) can be a likely explanation for this difference in influence of serum creatinine. While in our study, we included septic and non-septic patients (Table 1). Conil et al. [19] included only septic patients and found a significant influence of CLCr on kel. Forrest et al. [20] found a significant relationship between total ciprofloxacin clearance and CLCr estimated by the Jelliffe formula, mostly in patients with lower respiratory tract infection. Additionally, when ciprofloxacin renal clearance is compromised, the transintestinal elimination route is frequently described in the literature in humans and animals as the main compensatory elimination route [38,39,40]. In septic patients, Jones et al. [39] showed that only those patients who had liver or bowel pathology in addition to renal failure had a significantly higher serum concentration than all other patients. Nevertheless, dose reduction or interval extension have been proposed in the literature for patients with only impaired renal function [41,42,43]. Concurrently, the results of various studies show the importance of adequate dosing in ICU patients, suggesting not reducing the dose of ciprofloxacin in patients with impaired renal function [21, 39, 44]. In addition, no significant renal accumulation of ciprofloxacin in patients with an impaired renal function was observed [44, 45]. This supports ciprofloxacin TDM when dose reduction is considered in patients with impaired renal function to avoid underdosing.
Our study shows that the PDTs are seldomly reached using ciprofloxacin standard (800 mg/day) and high exposure (1200 mg/day) dosing in ICU patients. The PDT was only achieved in 16.7% of all patients at the clinical breakpoint of 0.5 mg/L. These findings are consistent with results from previous studies on exposure of ciprofloxacin in critically ill patients [15, 21, 22]. However, a breakpoint of 0.5 mg/L is only applicable when high exposure dosing is used (≥ 1200 mg/day), covering P. aeruginosa infection [34]. For microorganisms categorized as susceptible for standard dosing regimen, MICs ≤ 0.25 mg/L are appropriate to assess the probability of therapeutic success.
In this study, the PTA was simulated to identify ciprofloxacin intravenous dosing regimens that might better enable optimal target attainment. The simulations indicate that for this population of ICU patients, the variation is significant, and a PTA of at least 95% is only obtained for MIC values ≤ 0.25 mg/L. To reach a target of anƒAUC0–24/MIC ≥ 100 for these MICs, at least 1200 mg/day is required to ensure optimal exposure (> 95% PTA) in ICU patients (Fig. 4). For directed therapy against P. aeruginosa (an MIC of 0.5 mg/L) in patients with septic shock, even a higher dose of 600 mg q8h has been recommended to achieve adequate target attainment [23]. Furthermore, Roberts et al. [23] simulated an 800 mg loading dose, followed by 400 mg q8h doses, and demonstrated an increase in PTA on day 1 of therapy by 35–45%, compared with standard 400 mg q8h.
However, in clinical practice, the regular ciprofloxacin dosing falls within a relatively narrow range of 800–1200 mg/day, is not adjusted for body weight, and only moderately increased for severe infections in the ICU. Higher doses may also increase the risk of potential adverse events. Given that there is high degree of variety in PK of ciprofloxacin in critically ill patients, as demonstrated here, it follows that TDM in ICU patient is strongly recommended to increase the likelihood of therapeutic target achievement and avoid unnecessary high concentrations.
In this study, five samples per interval were used to estimate the AUC0–24, but in clinical practice this is not convenient. Thus, for TDM in clinical practice, we recommend a peak sample, or every second sample next to a trough sample to estimate the Cmax and AUC0–24 with sufficient accuracy. Considering that patients with ƒAUC0–24/MIC ≥ 100 have the highest cure rates [15], patients with infections caused by micro-organisms at higher MICs may benefit most of TDM, as traditional dosing is likely to result in inadequate exposure in the majority of ICU patients. Inadequate antibiotic exposure in ICU patients also appears to be an important independent determinant of hospital mortality [46]. Considering the increasing resistance to ciprofloxacin worldwide, at least 1200 mg/day dosing and preferably combined with TDM is warranted in critically ill patients [21, 23, 47]. However, current dosing recommendations of > 1200 mg/day are only based on simulations and have not prospectively and externally been validated. It should also be noted that the risk of adverse events for the > 1200 mg/day dosage simulated in this study has not been investigated. Furthermore, it is not clear whether toxicity is predominantly peak or AUC driven so that potential adverse effects could be reduced by altering the number of administrations per day.
The present study shows some pitfalls that should be discussed. First, the ƒAUC was calculated assuming a PPB 30%. Measuring unbound ciprofloxacin concentrations is desirable when treating ICU patients, since the ratio of bound and unbound drugs can be subject to change because of disease characteristics in critically ill patients. However, protein binding of ciprofloxacin is too low to be clinically affected by the decrease of serum albumin for instance, making the calculation of unbound concentrations from published protein binding values acceptable. We analyzed plasma protein unbound fractions in another cohort of ICU patients [48] to clarify the clinical feasibility of calculating unbound fractions using an average PPB value. The mean fraction of ciprofloxacin unbound plasma concentrations (n = 36) in the range of 0.1–12.5 mg/L was 70.5% ± 4.7% SD (data not published yet). This is comparable with the calculated free fraction used in this study and previously published data [26, 27].
Second, we used ECOFF values to calculate the PTA, since the ECOFF in many situations is similar to the clinical breakpoint [49]. Due to this approach, there is a chance that PTA is underestimated in our study. However, the use of a measured MIC obtained by a single MIC determination is debatable, since routine clinical laboratories cannot determine MICs with sufficient accuracy due to the inherent assay variation in the MIC test and the variation in any MIC determination [49].
Third, we used serum creatinine concentration as a testing covariate on clearance. The creatinine clearance is the method of reference for the estimation of the GFR. However, it is not directly measured but an estimation by equation (i.e. Cockcroft-Gault or MDRD), which is not validated for critically ill patients. Changes in serum creatinine are delayed after changes in GFR, and fluid changes in critically ill patients can seriously complicate the capability of serum creatinine to detect small changes in kidney function [50, 51].
Conclusion
Our model describes the complex PK of intravenous ciprofloxacin in critically ill patients. We found a high inter-individual variability of ciprofloxacin PK. The obtained variability of our final model parameters in combination with the presented low target attainment suggests higher initial doses of at least 1200 mg/day are needed in critically ill patients. More clinical outcome studies are necessary to support this proposal, and to support the need for therapeutic drug monitoring to ensure optimal exposure. To confirm the correlation of current PK/PD targets with optimal patient outcomes, future clinical studies should validate and evaluate outcome benefits from improved ciprofloxacin exposure using a randomized controlled trial design.
References
Friedman ND, Temkin E, Carmeli Y (2016) The negative impact of antibiotic resistance. Clin Microbiol Infect 22(5):416–422. https://doi.org/10.1016/j.cmi.2015.12.002
Giske CG, Monnet DL, Cars O, Carmeli Y (2008) Clinical and economic impact of common multidrug-resistant gram-negative bacilli. Antimicrob Agents Chemother 52(3):813–821. https://doi.org/10.1128/aac.01169-07
Campion M, Scully G (2018) Antibiotic use in the intensive care unit: optimization and de-escalation. J Intensive Care Med 33(12):647–655. https://doi.org/10.1177/0885066618762747
Roberts JA, Paul SK, Akova M, Bassetti M, De Waele JJ, Dimopoulos G, Kaukonen KM, Koulenti D, Martin C, Montravers P, Rello J, Rhodes A, Starr T, Wallis SC, Lipman J, Study D (2014) DALI: defining antibiotic levels in intensive care unit patients: are current beta-lactam antibiotic doses sufficient for critically ill patients? Clin Infect Dis 58(8):1072–1083. https://doi.org/10.1093/cid/ciu027
Ridley S, Burchett K, Gunning K, Burns A, Kong A, Wright M, Hunt P, Ross S (1997) Heterogeneity in intensive care units: fact or fiction? Anaesthesia 52(6):531–537. https://doi.org/10.1111/j.1365-2222.1997.109-az0109.x
De Waele JJ, Carrette S, Carlier M, Stove V, Boelens J, Claeys G, Leroux-Roels I, Hoste E, Depuydt P, Decruyenaere J, Verstraete AG (2014) Therapeutic drug monitoring-based dose optimisation of piperacillin and meropenem: a randomised controlled trial. Intensive Care Med 40(3):380–387. https://doi.org/10.1007/s00134-013-3187-2
Udy AA, Roberts JA, Lipman J (2013) Clinical implications of antibiotic pharmacokinetic principles in the critically ill. Intensive Care Med 39(12):2070–2082
Sime FB, Roberts MS, Peake SL, Lipman J, Roberts JA (2012) Does beta-lactam pharmacokinetic variability in critically ill patients justify therapeutic drug monitoring? A systematic review. Ann Intensive Care 2(1):35. https://doi.org/10.1186/2110-5820-2-35
Roberts JA, De Waele JJ, Dimopoulos G, Koulenti D, Martin C, Montravers P, Rello J, Rhodes A, Starr T, Wallis SC, Lipman J (2012) DALI: defining antibiotic levels in intensive care unit patients: a multi-centre point of prevalence study to determine whether contemporary antibiotic dosing for critically ill patients is therapeutic. BMC Infect Dis 12(1):152. https://doi.org/10.1186/1471-2334-12-152
Kuti JL, Nightingale CH, Nicolau DP (2004) Optimizing pharmacodynamic target attainment using the MYSTIC antibiogram: data collected in North America in 2002. Antimicrob Agents Chemother 48(7):2464–2470
Thomas JK, Forrest A, Bhavnani SM, Hyatt JM, Cheng A, Ballow CH, Schentag JJ (1998) Pharmacodynamic evaluation of factors associated with the development of bacterial resistance in acutely ill patients during therapy. Antimicrob Agents Chemother 42(3):521–527. https://doi.org/10.1128/aac.42.3.521
Dalhoff A (2012) Global fluoroquinolone resistance epidemiology and implictions for clinical use. Interdiscip Perspect Infect Dis 2012:976273. https://doi.org/10.1155/2012/976273
Cruciani M, Bassetti D (1994) The fluoroquinolones as treatment for infections caused by gram-positive bacteria. J Antimicrob Chemother 33(3):403–417
Khachman D, Conil J-M, Georges B, Saivin S, Houin G, Toutain P-L, Laffont CM (2011) Optimizing ciprofloxacin dosing in intensive care unit patients through the use of population pharmacokinetic–pharmacodynamic analysis and Monte Carlo simulations. J Antimicrob Chemother 66(8):1798–1809
Forrest A, Nix DE, Ballow CH, Goss TF, Birmingham MC, Schentag JJ (1993) Pharmacodynamics of intravenous ciprofloxacin in seriously ill patients. Antimicrob Agents Chemother 37(5):1073–1081
Preston SL, Drusano GL, Berman AL, Fowler CL, Chow AT, Dornseif B, Reichl V, Natarajan J, Corrado M (1998) Pharmacodynamics of levofloxacin: a new paradigm for early clinical trials. Jama 279(2):125–129. https://doi.org/10.1001/jama.279.2.125
Zelenitsky SA, Ariano RE (2010) Support for higher ciprofloxacin AUC24/MIC targets in treating Enterobacteriaceae bloodstream infection. J Antimicrob Chemother 65(8):1725–1732. https://doi.org/10.1093/jac/dkq211
Peloquin CA, Cumbo TJ, Nix DE, Sands MF, Schentag JJ (1989) Evaluation of intravenous ciprofloxacin in patients with nosocomial lower respiratory tract infections: impact of plasma concentrations, organism, minimum inhibitory concentration, and clinical condition on bacterial eradication. Arch Intern Med 149(10):2269–2273. https://doi.org/10.1001/archinte.1989.00390100083020
Conil J-M, Georges B, de Lussy A, Khachman D, Seguin T, Ruiz S, Cougot P, Fourcade O, Houin G, Saivin S (2008) Ciprofloxacin use in critically ill patients: pharmacokinetic and pharmacodynamic approaches. Int J Antimicrob Agents 32(6):505–510. https://doi.org/10.1016/j.ijantimicag.2008.05.019
Forrest A, Ballow CH, Nix DE, Birmingham MC, Schentag JJ (1993) Development of a population pharmacokinetic model and optimal sampling strategies for intravenous ciprofloxacin. Antimicrob Agents Chemother 37(5):1065–1072
van Zanten AR, Polderman KH, van Geijlswijk IM, van der Meer GY, Schouten MA, Girbes AR (2008) Ciprofloxacin pharmacokinetics in critically ill patients: a prospective cohort study. J Crit Care 23(3):422–430
Haeseker M, Stolk L, Nieman F, Hoebe C, Neef C, Bruggeman C, Verbon A (2013) The ciprofloxacin target AUC : MIC ratio is not reached in hospitalized patients with the recommended dosing regimens. Br J Clin Pharmacol 75(1):180–185
Roberts JA, Alobaid AS, Wallis SC, Perner A, Lipman J, Sjövall F (2019) Defining optimal dosing of ciprofloxacin in patients with septic shock. J Antimicrob Chemother 74(6):1662–1669. https://doi.org/10.1093/jac/dkz069
Roger C, Wallis SC, Louart B, Lefrant J-Y, Lipman J, Muller L, Roberts JA (2016) Comparison of equal doses of continuous venovenous haemofiltration and haemodiafiltration on ciprofloxacin population pharmacokinetics in critically ill patients. J Antimicrob Chemother 71(6):1643–1650. https://doi.org/10.1093/jac/dkw043
U.S. Food and Drug Administration (FDA) (2001) Guidance for industry: bioanalytical method validation. Available from: http://www.fda.gov/cder/guidance/4252fnl.pdf
Ulldemolins M, Roberts JA, Rello J, Paterson DL, Lipman J (2011) The effects of hypoalbuminaemia on optimizing antibacterial dosing in critically ill patients. Clin Pharmacokinet 50(2):99–110. https://doi.org/10.2165/11539220-000000000-00000
Bergogne-Bérézin E (2002) Clinical role of protein binding of quinolones. Clin Pharmacokinet 41(10):741–750. https://doi.org/10.2165/00003088-200241100-00004
Keizer RJ, Karlsson MO, Hooker A (2013) Modeling and simulation workbench for NONMEM: tutorial on Pirana, PsN, and Xpose. CPT Pharmacometrics Syst Pharmacol 2(6):50. https://doi.org/10.1038/psp.2013.24
Karlsson MO, Savic RM (2007) Diagnosing model diagnostics. Clin Pharmacol Ther 82(1):17–20. https://doi.org/10.1038/sj.clpt.6100241
Overholser BR, Kays MB, Forrest A, Sowinski KM (2004) Sex-related differences in the pharmacokinetics of oral ciprofloxacin. J Clin Pharmacol 44(9):1012–1022
Jonsson EN, Karlsson MO (1998) Automated covariate model building within NONMEM. Pharm Res 15(9):1463–1468
Bergstrand M, Hooker AC, Wallin JE, Karlsson MO (2011) Prediction-corrected visual predictive checks for diagnosing nonlinear mixed-effects models. AAPS J 13(2):143–151. https://doi.org/10.1208/s12248-011-9255-z
Comets E, Brendel K, Mentre F (2008) Computing normalised prediction distribution errors to evaluate nonlinear mixed-effect models: the npde add-on package for R. Comput Methods Prog Biomed 90(2):154–166
The European Committee on Antimicrobial Susceptibility Testing (2017) Breakpoint tables for interpretation of MICs and zone diameters. http://www.eucast.org
Roberts JA, Kirkpatrick CMJ, Lipman J (2010) Monte Carlo simulations: maximizing antibiotic pharmacokinetic data to optimize clinical practice for critically ill patients. J Antimicrob Chemother 66(2):227–231. https://doi.org/10.1093/jac/dkq449
Gous A, Lipman J, Scribante J, Tshukutsoane S, Hon H, Pinder M, Mathivha R, Verhoef L, Stass H (2005) Fluid shifts have no influence on ciprofloxacin pharmacokinetics in intensive care patients with intra-abdominal sepsis. Int J Antimicrob Agents 26(1):50–55. https://doi.org/10.1016/j.ijantimicag.2005.04.005
Bragadottir G, Redfors B, Ricksten S-E (2013) Assessing glomerular filtration rate (GFR) in critically ill patients with acute kidney injury - true GFR versus urinary creatinine clearance and estimating equations. Crit Care 17(3):R108. https://doi.org/10.1186/cc12777
Rohwedder R, Bergan T, Thorsteinsson SB, Scholl H (1990) Transintestinal elimination of ciprofloxacin. Chemotherapy 36(2):77–84
Jones EM, McMullin CM, Hedges AJ, Lovering AM, White LO, Reeves DS, MacGowan AP (1997) The pharmacokinetics of intravenous ciprofloxacin 400 mg 12 hourly in patients with severe sepsis: the effect of renal function and intra-abdominal disease. J Antimicrob Chemother 40(1):121–124
Dautrey S, Rabbaa L, Laouari D, Lacour B, Carbon C, Farinotti R (1999) Influence of renal failure on intestinal clearance of ciprofloxacin in rats. Antimicrob Agents Chemother 43(3):678–680. https://doi.org/10.1128/aac.43.3.678
Gasser TC, Ebert SC, Graversen PH, Madsen PO (1987) Ciprofloxacin pharmacokinetics in patients with normal and impaired renal function. Antimicrob Agents Chemother 31(5):709–712
Drusano GL, Weir M, Forrest A, Plaisance K, Emm T, Standiford HC (1987) Pharmacokinetics of intravenously administered ciprofloxacin in patients with various degrees of renal function. Antimicrob Agents Chemother 31(6):860–864
Webb DB, Roberts DE, Williams JD, Asscher AW (1986) Pharmacokinetics of ciprofloxacin in healthy volunteers and patients with impaired kidney function. J Antimicrob Chemother 18(Suppl D):83–87
Pea F, Poz D, Viale P, Pavan F, Furlanut M (2006) Which reliable pharmacodynamic breakpoint should be advised for ciprofloxacin monotherapy in the hospital setting? A TDM-based retrospective perspective. J Antimicrob Chemother 58(2):380–386
MacGowan AP, White LO, Brown NM, Lovering AM, McMullin CM, Reeves DS (1994) Serum ciprofloxacin concentrations in patients with severe sepsis being treated with ciprofloxacin 200 mg i.v. bd irrespective of renal function. J Antimicrob Chemother 33(5):1051–1054
Roberts JAPS, Akova M et al (2014) DALI: defining antibiotic levels in intensive care unit patients: are current b-lactam antibiotic doses sufficient for critically ill patients? Clin Infect Dis 58:1072–1083
Lipman J, Scribante J, Gous AGS, Hon H, Tshukutsoane S (1998) Pharmacokinetic profiles of high-dose intravenous ciprofloxacin in severe sepsis. Antimicrob Agents Chemother 42(9):2235–2239. https://doi.org/10.1128/aac.42.9.2235
Abdulla A, Ewoldt TMJ, Hunfeld NGM, Muller AE, Rietdijk WJR, Polinder S, van Gelder T, Endeman H, Koch BCP (2020) The effect of therapeutic drug monitoring of beta-lactam and fluoroquinolones on clinical outcome in critically ill patients: the DOLPHIN trial protocol of a multi-centre randomised controlled trial. BMC Infect Dis 20(1):57. https://doi.org/10.1186/s12879-020-4781-x
Mouton JW, Muller AE, Canton R, Giske CG, Kahlmeter G, Turnidge J (2017) MIC-based dose adjustment: facts and fables. J Antimicrob Chemother 73(3):564–568. https://doi.org/10.1093/jac/dkx427
Poggio ED, Nef PC, Wang X, Greene T, Van Lente F, Dennis VW, Hall PM (2005) Performance of the Cockcroft-Gault and modification of diet in renal disease equations in estimating GFR in ill hospitalized patients. Am J Kidney Dis 46(2):242–252. https://doi.org/10.1053/j.ajkd.2005.04.023
Sunder S, Jayaraman R, Mahapatra HS, Sathi S, Ramanan V, Kanchi P, Gupta A, Daksh SK, Ram P (2014) Estimation of renal function in the intensive care unit: the covert concepts brought to light. J Intensive Care 2(1):31–31. https://doi.org/10.1186/2052-0492-2-31
Acknowledgments
The authors are grateful to Prof. Dr. Johan W. Mouton for all his work. They also thank all the patients who participated in this study, the ICU teams that selected the patients and collected the samples, and the pharmacy laboratory of the Erasmus University Medical Center in Rotterdam for analysing the samples.
Funding
The EXPAT study was supported by the Erasmus Medical Center; no specific funding was received.
Author information
Authors and Affiliations
Contributions
AA, NGMH, TvG, and BCPK were involved in the concept and design of the study. AA, OR, and AD were involved in recruitment and screening of trial participants. AA, OR, BCMdW, and BCPK performed data analysis. All authors contributed to interpretation of the data. AA wrote the first draft of the manuscript and all authors contributed to subsequent drafts and gave final approval of the version to be published.
Corresponding author
Ethics declarations
The study was conducted in accordance with the principles of the Declaration of Helsinki and the International Conference on Harmonization (ICH) Good Clinical Practice Guidelines. Approval for the study protocol was obtained from the Erasmus MC Medical Ethics Committee (MEC-2015-502/NL53551.078.15) and the study was registered in the Netherlands Trial Registry (EXPAT trial, NTR 5632). Informed consent was obtained from the patients or their legal representative.
Conflict of interest
The authors declare that they have no conflict of interest.
Disclaimer
The Erasmus Medical Center approved the design of the trial, but had no role in the collection, analysis and interpretation of data or in the writing manuscript or the decision to publish.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
ESM 1
(PDF 143 kb)
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Abdulla, A., Rogouti, O., Hunfeld, N.G.M. et al. Population pharmacokinetics and target attainment of ciprofloxacin in critically ill patients. Eur J Clin Pharmacol 76, 957–967 (2020). https://doi.org/10.1007/s00228-020-02873-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-020-02873-5