Abstract
Background
Increased bioavailability of phenylephrine is reported when combined with paracetamol in over-the-counter formulations for the symptomatic treatment of the common cold and influenza. Such formulations could increase phenylephrine-related cardiovascular adverse events particularly in susceptible individuals. Quantification of the effect of phenylephrine concentration on blood pressure allows simulation of potential adverse combination therapy effects.
Methods
MEDLINE and EMBASE databases were searched for papers discussing or describing any adverse effect, hypersensitivity or safety concerns related to phenylephrine alone or in combination with other drugs.
The pharmacodynamic relationship between plasma phenylephrine concentration and mean arterial blood pressure was characterized using published observations of blood pressure changes after ophthalmic eye drops. The resulting pharmacokinetic and pharmacodynamic parameters were then used to predict mean arterial blood pressure (MAP) changes in that population if given an oral combination of phenylephrine and paracetamol.
Results
There were 1172 papers identified for examination. Forty-seven reports fulfilled the inclusion criteria. Increases in blood pressure and decreases in heart rate have been reported with doses over 15 mg. It has been estimated that a 20-mmHg increase in systolic blood pressure would occur with an oral dose of 45 mg phenylephrine in normotensive healthy people. Those taking monoamine oxidase inhibitors report increased systolic blood pressure of greater than 60 mmHg. Blood pressure and heart rate changes are potentiated in patients with underlying hypertension. Simulation showed a modest increase in MAP when phenylephrine 10 mg was co-administered with paracetamol 1 g (4.2 vs 12.3 mmHg).
Conclusions
Combination paracetamol phenylephrine oral therapy has potential to increase blood pressure more than phenylephrine alone in those with cardiovascular compromise.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Phenylephrine is a selective alpha-1 adrenoceptor agonist with powerful vasoconstrictive properties. Historically, its use had been restricted to the perioperative period and intensive care medicine for preparation of the surgical field and control of haemorrhage during ear nose and throat procedures, pupillary dilation and maintenance of blood pressure. Phenylephrine is commonly used now as a nasal decongestant in many over-the-counter (OTC) cold and influenza preparations.
When phenylephrine was combined with another commonly administered cold and flu medication, paracetamol, the plasma concentration of phenylephrine was, on average, twice that obtained when phenylephrine was given alone and the peak concentration approximately four times higher [1]. It is suggested that the increase in phenylephrine bioavailability is due to a reduction in the amount of phenylephrine undergoing first-pass metabolism due to saturation of the sulfation pathways by paracetamol [1]. Formulation may also have impact. Phenylephrine bioavailability was reduced when administered as a paracetamol-guaifenesin-phenylephrine syrup compared to the same combination in tablet form [2]. These findings raise the concern that phenylephrine administered as a combination with paracetamol may increase the incidence of adverse effects attributable to phenylephrine, most notably cardiovascular adverse effects particularly those with preexisting cardiovascular conditions.
Here, we provide a systematic narrative review of cardiovascular adverse effects associated with phenylephrine. We quantify the effect of phenylephrine concentration on blood pressure using published data and simulate the potential impact paracetamol phenylephrine combination oral therapy may have on cardiovascular endpoints.
Methods
Literature review of phenylephrine adverse events
Search strategy
A broad search (search terms are detailed in the Supplementary Appendix) of both MEDLINE and EMBASE databases was undertaken followed by manual selection of relevant reports based on the inclusion and exclusion criteria described below. No specific time limits were applied to the search. The time frame of the search was limited only by the coverage of the database (MEDLINE: 1946 to April 2014; EMBASE: 1947 to April 2014).
Papers discussing or describing any adverse effect, hypersensitivity or safety concern related to phenylephrine alone or in combination were included. Papers were excluded if they (1) did not describe an adverse effect for phenylephrine; (2) related to children under 12 years of age; (3) were not written in English or a full-text version was not available for purchase; (4) was not a clinical trial [either prospective or retrospective], case report or series, or a meta-analysis; and (5) did not relate to the cardiovascular system. References of identified papers were reviewed for additional relevant reports.
Simulation
Phenylephrine PKPD relationship analysis
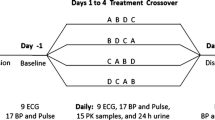
The relationship between plasma phenylephrine concentration and mean arterial blood pressure was characterized using those published data from Kumar and colleagues [3], who related the systemic absorption of phenylephrine eye drops to cardiovascular effects. Individual plasma concentrations and corresponding blood pressure changes at 0, 10, 20 and 60 min after 2.5 % (n = 10) and 10 % (n = 10) eye drops (two 32-μL drops at 5-min intervals) are contained in Tables 1 and 2 of that publication(n = 20). Further pharmacokinetic (PK) data were available from healthy volunteers given oral phenylephrine 10 mg alone, with blood for concentration assay taken at 5, 15, 30, and 45 min and 1, 2, 3, and 6 h (n = 28, data from [1, 4]). Intravenous time-concentration data were available from a study by Hengstmann and colleagues [5]. Four healthy volunteers were given phenylephrine 1 mg, and blood was taken for assay on 17 occasions over the subsequent 4 h. Pooled data for that study are presented in Table 2 of that publication(n = 1). Technical methods for population parameter estimates using nonlinear mixed effects models (NONMEM) can be found in the Supplementary Appendix.
Results
Literature search
A total of 1172 papers were identified for examination. Forty-seven reports fulfilled the inclusion criteria. The majority of literature concerning phenylephrine and cardiovascular effects related to its use as a hypertensive agent for the management of hypotension associated with shock and spinal anaesthesia. These effects are therapeutic in these scenarios, and as they are not adverse effects, they are not discussed. Case reports and studies that described unexpected or unwanted cardiovascular effects following the use of phenylephrine are listed in Table 1.
The standard OTC 10-mg dose of phenylephrine appears to be well tolerated by the majority of people; however, increases in blood pressure and decreases in heart rate are reported with doses over 15 mg [6, 7]. It has been estimated that a 20-mmHg increase in systolic blood pressure would occur with an oral dose of 45 mg phenylephrine in normotensive healthy people [8]. This situation changes considerably in people taking medications such as monoamine oxidase inhibitors where interaction with phenylephrine caused increases in systolic blood pressure of greater than 60 mmHg and required intervention [9, 10]. Blood pressure and heart rate changes also appear to be potentiated in patients with underlying hypertension. One study reports severe hypertensive episode requiring intervention in 10 % of study participants given 10 % topical drops as a mydriatic agent in ophthalmic surgery, all of whom had underlying hypertension; no episodes of hypertension were reported in normotensive participants [11]. Phenylephrine may also interact with cocaine (medical or recreational) potentiating the hypertensive effects of phenylephrine [12, 13].
Unwanted cardiovascular effects are commonly reported when phenylephrine is administered intravenously for its hypertensive effects and appear to be dose dependent [14–19]. The majority of literature relates to bradycardia and reactive hypertension when phenylephrine was used to counter the hypotensive effects of spinal anaesthesia during caesarean section [14–19]. An increase in blood pressure with associated impairment in myocardial perfusion was seen when phenylephrine was administered to patients with underlying cardiac disease (angina pectoris, old myocardial infarct or chronic coronary artery disease) [20]. Increased blood pressure [21–27], vasoconstriction resulting in worsening of orthostatic intolerance [28], atrial fibrillation after coronary artery bypass surgery [29], decreased cerebral oxygenation [30, 31], bradycardia in patients with high cervical spinal cord injury [32], cardiac arrhythmias [33], pulmonary oedema and myocardial infarction [34], and microvascular occlusion syndrome [35] have all been associated with phenylephrine use.
Cerebrovascular events have also been reported. Tark et al. report the case of an otherwise healthy 50-year-old woman who suffered intracerebral haemorrhage after oral administration of standard doses of cold medicines containing phenylephrine and paracetamol for 4 days before hospitalization [36]. Other studies have reported cerebrovascular accidents following phenylephrine use via topical and intravenous administration [37–42].
PKPD relationship analysis
The pharmacokinetic/pharmacodynamic (PKPD) analysis was based on 49 subjects (with 387 observations) who received phenylephrine ophthalmic eye drops where plasma concentrations were available for analysis. Patients had a mean age 34.3 SD 8.2 years and a mean weight 74.4 SD 3.4 kg. Pharmacokinetic and pharmacodynamic parameter estimates are reported in Table 2. The correlation of between parameter variability is shown in Table 3. PC-VPC plots, used to demonstrate goodness of fit, are shown in Fig. 1. Figure 2 demonstrates the pharmacodynamic relationship between phenylephrine concentration and MAP for a typical individual.
Visual predictive check for the PKPD model. All plots show median and 90 % intervals (solid and dashed lines). Also shown are prediction percentiles (10, 50 and 90 %) for observations (lines with symbols) and predictions (lines) with 95 % confidence intervals for prediction percentiles (grey-shaded areas). The upper panel is the pharmacokinetic fit using PK data from all formulations while the lower panel is the pharmacodynamic fit involving data only from subjects undergoing ophthalmic surgery
Simulation
Pharmacodynamic parameter estimates estimated from the phenylephrine ophthalmic study [3] were combined with derived pharmacokinetic estimates from a study in healthy volunteers given paracetamol and phenylephrine combination therapy [4] to simulate mean time-concentration and mean arterial blood pressure changes that might occur if patients were given oral phenylephrine with and without paracetamol. These simulations were performed using Berkeley Madonna™ modelling and analysis of dynamic systems software V 8.3.18 (Robert Macey and George Oster of the University of California, Berkeley, USA). We predict an increase in MAP of 16 mmHg after 45 mg phenylephrine; i.e., a person with a BP of 120/65 mmHg might increase to 140/80 mmHg, a systolic increase of 20 mmHg. Plots are presented in Fig. 3. The increased absorption rate of phenylephrine when combined with paracetamol results in higher peak concentrations than might be anticipated from increased bioavailability alone.
Pharmacodynamic parameter estimates from patients (mean age 34.3 years, 70 kg) undergoing ophthalmic surgery were combined with derived pharmacokinetic estimates from the current study to simulate mean time-concentration (solid lines) and mean arterial blood pressure changes (dashed lines) that might occur when given oral phenylephrine with and without paracetamol
Discussion
Phenylephrine has now replaced pseudoephedrine in most over-the-counter (OTC) cold and influenza medications. There are few data reporting adverse events associated with oral phenylephrine use. What little information available must be gleaned from other routes of administration where more formal studies have been conducted: phenylephrine interacts with monoamine oxidase inhibitors and possibly other drugs to potentiate its hypertensive effect; cardiovascular changes may be more pronounced in people with underlying cardiovascular disease and may lead to decreased myocardial oxygenation, cardiac arrhythmias, decreased cerebral oxygenation and exaggerated vasoconstriction and stroke.
That few adverse events following oral administration of phenylephrine are reported is not surprising, though not necessarily reflective of the actual incidence of adverse effects. Relative oral bioavailability remains poorly documented but may be as little as 0.003 [5]. Absorption is slow (Tabs 0.4 h, BSV 30.8 %), and peak concentrations will be less than that observed after rapid intravenous administration. Oral phenylephrine is generally administered in a community setting to relieve symptoms of malaise associated with colds and influenza, and as such, blood pressure changes over the short duration of phenylephrine administration are unlikely to be recorded. The few studies examining oral phenylephrine at the recommended dose of 10 mg have shown it to be well tolerated in patients suffering from nasal congestion. However, these studies focus on phenylephrine as a single agent and not in combination with paracetamol where bioavailability is increased and peak plasma concentrations doubled [1]. Furthermore, these studies have primarily been conducted in either healthy volunteers or in otherwise healthy patients with nasal congestion.
The simulation study assumes that the administration of phenylephrine with paracetamol more than doubles the bioavailability of phenylephrine and reduces the absorption half-time by 50 % resulting in a doubling of phenylephrine plasma concentration and an approximate fourfold increase in Cmax, with large between-subject variability [4, 1]. Of concern is the possibility of increased adverse effects associated with this increase in plasma concentration, particularly in people with cardiovascular compromise or on other medications that may interact with phenylephrine. Simulation using blood pressure changes after ophthalmic administration provides an example of the magnitude of blood pressure change for a typical subject: a standard 10-mg dose of phenylephrine combined with paracetamol could result in an increase in MAP of more than 10 mmHg (Fig. 2). We report considerable between-subject variability that was unexplainable from the limited cohort investigated. The impact of age, existing hypertension and ophthalmic preparation dose accuracy are covariates that require further investigation.
An important consideration is the substantial variability in Cmax [4]: a subgroup of the population would be exposed to relatively higher phenylephrine plasma concentrations than the population mean data would suggest, leading to more serious adverse events. Indeed, one case report describes haemorrhagic stroke in an otherwise healthy female taking phenylephrine and paracetamol in combination for treatment of cold and flu symptoms [36]. It is also possible that others without underlying hypertension could also be compromised. It has been estimated that a 20-mmHg increase in blood pressure would occur with a 45-mg phenylephrine dose in normotensive patients [8], an observation consistent with our current simulation. It is possible that any given individual may experience a plasma concentration similar to that seen with a 45-mg dose when 10 mg phenylephrine is combined with paracetamol. Systemic or pulmonary hypertension is also reported in children (6 months–14 years) administered 10 % ophthalmic drops [43].
When medications are administered OTC, the burden of safety should be high—with only 40 % of consumers reading the packet label when they take a medicine for the first time and only 7 % reading safety information and warnings [44], and changing labelling to reduce the risk of adverse events is ineffective. In addition, more than one third of consumers take more than the recommended dose of an OTC medication believing that it will increase the effectiveness of the medication and an additional 30 % combine different OTC medicines to treat different symptoms [44] leading to the potential for overdose of any single active ingredient and the associated adverse effects.
In 2007, the FDA determined that there was insufficient data to support increasing the dose to the higher 25 mg whilst maintaining a similar safety profile to the 10-mg dose [45]. At the same time, the committee concluded that “comparisons of the pharmacokinetics of single-ingredient products versus multiple ingredient products” and “safety evaluations of the effects of phenylephrine on blood pressure and cardiovasculature and use of phenylephrine in patients with important comorbidities such as BPH, hypertension or diabetes mellitus” be conducted [45]. Whilst there are now some data on the interaction pharmacokinetics of phenylephrine, the consequences to the population of the OTC co-administration of phenylephrine and paracetamol remain difficult to define. The literature reviewed here suggests that this increased phenylephrine exposure could be associated with many, potentially life-threatening adverse events in individuals both with underlying cardiovascular compromise and those who are otherwise healthy. Despite the FDA’s call for studies almost a decade ago, there remain no studies specifically examining the safety profile of phenylephrine in populations with underlying compromise, nor are there any studies examining the effects of chronic use of phenylephrine despite the potential safety burden.
References
Atkinson HC, Stanescu I, Anderson BJ (2014) Increased phenylephrine plasma levels with administration of acetaminophen. N Eng J Med 370(12):1171–1172
Janin A, Monnet J (2014) Bioavailability of paracetamol, phenylephrine hydrochloride and guaifenesin in a fixed-combination syrup versus an oral reference product. J Int Med Res 42(2):347–359
Kumar V, Schoenwald RD, Chien DS, Packer AJ, Choi WW (1985) Systemic absorption and cardiovascular effects of phenylephrine eyedrops. Am J Ophthalmol 99(2):180–184
Atkinson HC, Stanescu I, Salem II, Potts AL, Anderson BJ (2015) Increased bioavailability of phenylephrine by co-administration of acetaminophen: results of four open-label, crossover pharmacokinetic trials in healthy volunteers. Eur J Clin Pharmacol 71(2):151–158
Hengstmann JH, Goronzy J (1982) Pharmacokinetics of 3H-phenylephrine in man. Eur J Clin Pharmacol 21(4):335–341
Cohen BM (1972) Clinical and physiologic significance of drug-induced changes in nasal flow/resistance. Eur J Clin Pharmacol 5(2):81–86
McLaurin JW, Shipman WF, Rosedale R (1961) Oral decongestants. Laryngoscope 71(1):54–67
Keys A, Violante A (1942) The cardio-circulatory effects in man of neo-synephrin. J Clin Invest 21(1):1–12
Elis J, Laurence DR, Mattie H, Prichard BN (1967) Modification by monoamine oxidase inhibitors of the effect of some sympathomimetics on blood pressure. BMJ 2(5544):75
Lefebvre H, Richard R, Noblet C, Moore N, Wolf L (1993) Life-threatening pseudo-phaeochromocytoma after toloxatone, terbutaline, and phenylephrine. Lancet 341:555
Chin K, Law N, Chin M (1994) Phenylephrine eye drops in ophthalmic surgery—a clinical study on cardiovascular effects. Med J Malaysia 49:158–158
Singh PP, Dimich I, Shamsi A (1994) Intraoperative pulmonary oedema in a young cocaine smoker. Can J Anaesth 41(10):961–964
Ashchi M, Wiedemann HP, James KB (1995) Cardiac complication from use of cocaine and phenylephrine in nasal septoplasty. Arch Otolaryngol Head Neck Surg 121(6):681
Ngan Kee WD, Khaw KS, Ng FF (2005) Prevention of hypotension during spinal anesthesia for cesarean delivery: an effective technique using combination phenylephrine infusion and crystalloid cohydration. Anaesthesiol 103(4):744–750
Ngan Kee WD, Khaw KS, Ng FF, Lee BB (2004) Prophylactic phenylephrine infusion for preventing hypotension during spinal anesthesia for cesarean delivery. Anesth Analg 98(3):815–821
Ngan Kee W, Khaw K, Ng F (2004) Comparison of phenylephrine infusion regimens for maintaining maternal blood pressure during spinal anaesthesia for Caesarean section†. Br J Anaesth 92(4):469–474
Tanaka M, Balki M, Parkes R, Carvalho J (2009) ED95 of phenylephrine to prevent spinal-induced hypotension and/or nausea at elective cesarean delivery. J Obstet Anesth 18(2):125–130
Thomas D, Robson S, Redfern N, Hughes D, Boys R (1996) Randomized trial of bolus phenylephrine or ephedrine for maintenance of arterial pressure during spinal anaesthesia for Caesarean section. Br J Anaesth 76(1):61–65
Yadav U, Bharat K (2012) A clinical comparative study of prophylactic infusions of phenylephrine and ephedrine on maternal hemodynamics and fetal acidosis in elective caesarean section. Int J Pharm Sci Res 3(12):5056–5061
Antonopoulos A, Nikolopoulos D, Georgiou EK, Kyriakidis M, Proukakis C (2002) Blood pressure elevation after phenylephrine infusion may adversely affect myocardial perfusion in patients with coronary artery disease. J Cardiol 84(2):201–209
Ryu HG, Jung CW, Lee HC, Cho YJ (2012) Epinephrine and phenylephrine pretreatments for preventing postreperfusion syndrome during adult liver transplantation. Liver Transpl 18(12):1430–1439
Staerman F, Nouri M, Coeurdacier P, Cipolla B, Guille F, Lobel B (1995) Treatment of the intraoperative penile erection with intracavernous phenylephrine. J Urol 153(5):1478–1481
Archer TL (2009) Pulse contour analysis aids the understanding of autonomic dysreflexia: hemodynamic findings in a T5 paraplegic surgical patient treated for hypotension with phenylephrine and ephedrine. J Clin Anesth 21(5):378–381
Enohumah K, Immanuel H, Whitty R, Connolly J (2012) The adverse effects of inadvertent intraoperative intravenous phenylephrine administration: a case report: case study. S Afr J Anaesth Analg 18(4):218–220
Fredriksen A (1982) Systemic reaction to subarachnoid injection of phenylephrine. Br J Anaesth 54(12):1337–1338
Gadegbeku CA, Shrayyef MZ, Taylor TP, Egan BM (2006) Mechanism of lipid enhancement of α1-adrenoceptor pressor sensitivity in hypertension. J Hypertens 24(7):1383–1389
Goertz AW, Schmidt M, Lindner KH, Seefelder C, Georgieff M (1993) Effect of phenylephrine bolus administration on left ventricular function during postural hypotension in anesthetized patients. J Clin Anesth 5(5):408–413
Stewart JM, Munoz J, Weldon A (2002) Clinical and physiological effects of an acute α-1 adrenergic agonist and a β-1 adrenergic antagonist in chronic orthostatic intolerance. Circulation 106(23):2946–2954
Salaria V, Mehta NJ, Abdul-Aziz S, Mohiuddin SM, Khan IA (2005) Role of postoperative vasopressor use in occurrence of atrial fibrillation after coronary artery bypass grafting. Am J Cardiol 95(2):247–249
Meng L, Gelb A, Alexander B, Cerussi A, Tromberg B, Yu Z, Mantulin W (2012) Impact of phenylephrine administration on cerebral tissue oxygen saturation and blood volume is modulated by carbon dioxide in anaesthetized patients. Br J Anaesth 108(5):815–822
Nissen P, Brassard P, Jørgensen TB, Secher NH (2010) Phenylephrine but not ephedrine reduces frontal lobe oxygenation following anesthesia-induced hypotension. Neurocrit Care 12(1):17–23
Inoue T, Manley GT, Patel N, Whetstone WD (2014) Medical and surgical management after spinal cord injury: vasopressor usage, early surgerys, and complications. J Neurotrauma 31(3):284–291
Hefer D, Bukharovich I, Nasrallah EJ, Plotnikov A (2005) Prominent positive U waves appearing with high-dose intravenous phenylephrine. J Electrocardiol 38(4):378–382
Kademani D, Voiner JL, Quinn PD (2004) Acute hypertensive crisis resulting in pulmonary edema and myocardial ischemia during orthognathic surgery. J Oral Maxillofac Surg 62(2):240–243
Kalajian AH, Turpen KB, Donovan KO, Malone JC, Callen JP (2007) Phenylephrine-induced microvascular occlusion syndrome in a patient with a heterozygous factor V Leiden mutation. Arch Dermatol 143(10):1314–1317
Tark BE, Messe SR, Balucani C, Levine SR (2014) Intracerebral hemorrhage associated with oral phenylephrine use: a case report and review of the literature. J Stroke Cerebrovasc Dis 23(9):2296–2300
Cantu C, Arauz A, Murillo-Bonilla LM, Lopez M, Barinagarrementeria F (2003) Stroke associated with sympathomimetics contained in over-the-counter cough and cold drugs. Stroke 34(7):1667–1672
Chartier JP, Bousigue JY, Teisseyre A, Morel C, Delpuech-Formosa F (1997) Postpartum cerebral angiopathy of iatrogenic origin. Abstract only. Revue Neurologique (Paris) 153(3):212–214
Genonceaux S, Cosnard G, Van De Wyngaert F, Hantson P (2011) Early ischemic lesions following subarachnoid hemorrhage: common cold remedy as precipitating factor? Abstract only. Acta Neurol Belg 111(1):59–61
Cass E, Kadar D, Stein HA (1979) Hazards of phenylephrine topical medication in persons taking propranolol. Can Med Assoc J 120(10):1261–1262
Weisberg LA (1993) Intracerebral hemorrhage after topical administration of mydriatic agents. South Med J 86(9):1064–1066
Ranasinghe JS, Kafi S, Oppenheimer J, Birnbach DJ (2008) Hemorrhagic stroke following elective cesarean delivery. J Obstet Anesth 17(3):271–274
Sbaraglia F, Mores N, Garra R, Giuratrabocchetta G, Lepore D, Molle F, Savino G, Piastra M, Pulitano S, Sammartino M (2014) Phenylephrine eye drops in pediatric patients undergoing ophthalmic surgery: incidence, presentation, and management of complications during general anesthesia. Paediatr Anaesth 24(4):400–405
Boelle PY, Garnerin P, Sicard JF, Clergue F, Bonnet F (2000) Voluntary reporting system in anaesthesia: is there a link between undesirable and critical events? Qual Health Care 9(4):203–209
FDA Summary Minutes of the Nonprescription Drugs Advisory Committee Meeting. Summary Minutes of the Nonprescription Drugs Advisory Committee Meeting. (2007). http://www.fda.gov/ohrms/dockets/ac/07/minutes/2007-4335m1-Final.pdf. Accessed 19 Sep 2013
Burton BT, Rice M, Schmertzler LE (1985) Atrioventricular block following overdose of decongestant cold medication. J Emerg Med 2(6):415–419
Kenawy N, Jabir M (2003) Phenylephrine 2.5% and 10% in phacoemulsification under topical anaesthesia: is there an effect on systemic blood pressure? Br J Ophthalamol 87(4):505–506
Lam PT, Poon B, Wu WK, Chi SC, Lam DS (2003) Randomized clinical trial of the efficacy and safety of tropicamide and phenylephrine in preoperative mydriasis for phacoemulsification. Clin Experiment Ophthalamol 31(1):52–56
Malhotra R, Banerjee G, Brampton W, Price N (1998) Comparison of the cardiovascular effects of 2.5% phenylephrine and 10% phenylephrine during ophthalmic surgery. Eye 12(6):973–975
Motta MM, Coblentz J, Fernandes BF, Burnier MN Jr (2009) Mydriatic and cardiovascular effects of phenylephrine 2.5% versus phenylephrine 10%, both associated with tropicamide 1%. Ophthalmic Res 42(2):87–89
Lai Y (1989) Adverse effect of intraoperative phenylephrine 10%: case report. Br J Ophthalamol 73(6):468–469
Macmillan M, Barker K (2008) Phenylephrine toxicity. Eur J Anaesth 25(5):426–427
Stewart A, Fernando R, McDonald S, Hignett R, Jones T, Columb M (2010) The dose-dependent effects of phenylephrine for elective cesarean delivery under spinal anesthesia. Anesth Analg 111(5):1230–1237
Lai F, Jenkins J (2007) Ventricular bigeminy during phenylephrine infusion used to maintain normotension during caesarean section under spinal anaesthesia. J Obstet Anesth 16(3):288–290
Acknowledgments
We would like to thank Mrs. I Stanescu for her assistance in reviewing and commenting on this manuscript.
Author contributions
H Atkinson supervised this manuscript and was involved in the design of the simulation, interpretation of the data and writing of the manuscript. A Potts reviewed the literature for the review and contributed to the design of the simulation study, interpretation and writing of the manuscript. B Anderson was involved in the design and conduct of the simulation study, interpretation and writing of the manuscript. All authors had full access to all the data.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 26 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Atkinson, H.C., Potts, A.L. & Anderson, B.J. Potential cardiovascular adverse events when phenylephrine is combined with paracetamol: simulation and narrative review. Eur J Clin Pharmacol 71, 931–938 (2015). https://doi.org/10.1007/s00228-015-1876-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-015-1876-1