Abstract
Components of the renin–angiotensin–aldosterone system (RAAS) are present on bone cells. One measure of RAAS activity, the aldosterone-renin-ratio (ARR), is used to screen for primary aldosteronism. Associations between ARR and bone mineral density are conflicting. This study investigated associations between ARR and peripheral quantitative computed tomography (pQCT) and impact microindentation (IMI). Male participants (n = 431) were from the Geelong Osteoporosis Study. “Likely” primary aldosteronism was defined as ARR ≥ 70 pmol/mIU. Another group, “possible” primary aldosteronism, was defined as either ARR ≥ 70 pmol/mIU or taking a medication that affects the RAAS, but not a beta blocker, and renin < 15 mU/L. Using pQCT, images at 4% and 66% of radial (n = 365) and tibial (n = 356) length were obtained. Using IMI measurements, bone material strength index (BMSi; n = 332) was determined. Associations between ARR or likely/possible primary aldosteronism and IMI or pQCT-derived bone parameters were tested using median regression. ARR and aldosterone values were not associated with any of the pQCT-derived bone variables in either unadjusted or adjusted analyses. Men with likely primary aldosteronism (n = 16), had lower adjusted total bone area (radial 66% site, − 12.5%). No associations were observed for men with possible primary aldosteronism (unadjusted or adjusted). No associations with BMSi were observed (p > 0.05). There were no associations between ARR or aldosterone and pQCT-derived bone parameters. Men with likely primary aldosteronism had lower bone area, suggesting clinically high levels of ARR may have a negative impact on bone health.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The renin–angiotensin–aldosterone system (RAAS) is responsible for maintaining blood pressure as well as fluid and electrolyte balance. Aldosterone activates the mineralocorticoid receptors in the renal tubules to increase sodium reabsorption, which leads to an increase in blood pressure [1]. Excess aldosterone occurs in primary or secondary hyperaldosteronism. Overproduction of aldosterone in the latter is triggered by its physiologic regulatory factors: renin, angiotensin II, corticotropin and potassium. Conversely, primary aldosteronism is caused by autonomous and unregulated aldosterone production by adrenal glomerulosa cells and is a common but under-diagnosed form of secondary hypertension [2]. Screening for primary aldosteronism is performed by measuring plasma levels of two components of the RAAS; aldosterone and renin, and calculating the aldosterone-to-renin ratio (ARR). The ARR value is important for differentiating between primary and secondary aldosteronism. In primary aldosteronism, excess aldosterone results in negative feedback and suppressed renin concentration, whereas in secondary aldosteronism, excess activation of the RAAS results in higher renin and a concomitant increase in aldosterone. Although the threshold for abnormal ARR varies, it is generally agreed that values ≥ 70 (pmol/mIU) indicate that primary aldosteronism may be present [3, 4].
Elements of the RAAS are present in bone cells, hence, dysregulation of aldosterone may impact bone health. In particular, mineralocorticoid receptors are present in bone tissue [5] and could affect bone through several possible mechanisms [6, 7]. Osteoblasts and osteocytes express 11β-hydroxysteroid dehydrogenase-2, an enzyme that inactivates cortisol and allows aldosterone to function [8]. Circulating cortisol concentrations are 1000 times higher than circulating aldosterone and in tissues that do not express 11β-hydroxysteroid dehydrogenase-2, mineralocorticoid receptors bind almost exclusively to cortisol. For bone cells that do express 11β-hydroxysteroid dehydrogenase-2, cortisol is inactivated, allowing aldosterone to bind to the mineralocorticoid receptors. Therefore, aldosterone may directly affect the differentiation, proliferation and function of osteoclasts, osteoblasts and osteocytes through mineralocorticoid receptors present on these cells [5]. Another possible mechanism is by increasing parathyroid hormone concentrations through binding to mineralocorticoid receptors located in the parathyroid glands or indirectly through increasing urinary calcium excretion [6, 9]. Both mechanisms result in a negative calcium balance, leading to a potential decrease in calcium in bone. Aldosterone may also affect bone by increasing oxidative stress, which can lead to increased osteoblast and osteocyte apoptosis [6]. Additionally, previous studies have reported that individuals with primary aldosteronism have lower vitamin D concentrations [7, 10], which is important for calcium and phosphorus homeostasis [11]. Currently the reason for this observation is not clear [10].
Few studies have investigated associations between aldosterone, renin or ARR and bone health. Two studies reported that although risk of fracture was higher in patients with primary aldosteronism, the differences in bone mineral density (BMD) were conflicting [9, 12]. Another study has demonstrated that trabecular bone score, which reflects bone microarchitecture [13], was lower for women, but not men, with primary aldosteronism compared to those without the condition, which may assist in explaining the increased risk of fracture [14]. The study also reported no differences in BMD for men or women. These studies suggest that other components of bone strength may be affected by changes in ARR, such as bone quality, rather than bone mass.
Alternative measures of bone that could be useful for investigating the effect of aldosterone, renin or ARR include peripheral quantitative computed tomography (pQCT) and impact microindentation (IMI). The pQCT technique provides information about bone microarchitecture at the radius and tibia [15]. It can differentiate between cortical and trabecular bone and provides important three-dimensional (volumetric) rather than two-dimensional (areal) BMD values. To our knowledge, only one study on this topic has used pQCT [16], showing that renin and ARR were associated with greater trabecular density, but no associations with aldosterone were observed. IMI is a technique that measures the fracture resistance of cortical bone at the mid-tibia using a device known as the OsteoProbe [17]. The device works by measuring the microindentation distance of the device tip and comparing it to the indentation distance in a polymethyl methacrylate control material [17, 18]. The ratio of these distances is calculated and expressed as a unitless variable known as the bone material strength index (BMSi). A bone that is more resistant to microcracks will have a smaller indentation depth relative to the control and will have a higher BMSi. We are not aware of any studies that have used IMI to study the effect of varying ARR values on bone.
Previous literature has indicated that individuals with primary aldosteronism may have deficits in bone quality rather than bone mass [14], and this may be better captured by these alternative measures of bone health. Therefore, the aim of this study was to investigate associations between a marker of primary aldosteronism, the ARR, and bone measures derived from pQCT and IMI techniques in a population-based sample of men.
Methods
Participants
Participants for this study were drawn from the Geelong Osteoporosis Study, a longitudinal cohort study situated in south-eastern Australia [19]. Participants were randomly recruited from the Australian electoral roll using an age-stratified sampling method. This study used data from the most recent assessment phase for men, the 15-year follow-up (data collected between 2016 and 2022). This was the first visit where pQCT and IMI techniques were performed. There were 448 men who provided blood samples at the 15-year follow-up and had data for pQCT and/or IMI.
Biochemical Data
Blood samples were collected in the morning following an overnight fast. Aldosterone (pmol/L) and renin (mIU/L) were measured in plasma and the aldosterone-renin-ratio (ARR; pmol/mIU) was calculated. Plasma aldosterone concentration (PAC) and direct renin concentration (DRC) measurements were performed using the DiaSorin LIAISON® chemiluminescent immunoassays on the Liaison XL analyser (DiaSorin, Saluggia, Italy). PAC by the LIAISON® aldosterone assay was reported in pmol/L; the quoted between-run analytical coefficients of variation (CV) were 9.5% at 188 pmol/L and 5.6% at 798 pmol/L. The DRC was reported in mU/L; the quoted between-run analytical CV were 10.0% at 5.1 mU/L and 4.3% at 82.4 mU/L.
Other biochemical measurements were: estimated glomerular filtration rate (eGFR), serum calcium, parathyroid hormone, 25-hydroxy vitamin D (25OHD), sodium, potassium and bone turnover markers; C-terminal telopeptide (CTx) and procollagen type 1 N propeptide (P1NP).
Peripheral Quantitative Computed Tomography (pQCT) Measurements
A peripheral computed tomography instrument (XCT 2000, Stratec Medizintechnik, Pforzheim, Germany) was used to obtain standard transverse scans at 4% and 66% of radial and tibial length from the distal end of the bone. The standard software (BonAlyse Oy, Jyvaskyla, Finland) was then used to analyse the scans and determine bone parameters. The quality of all scans was assessed using published protocols [20, 21] by at least two of the authors. The in-vivo CV for pQCT variables on this scanner were in the range of 0.9–3.9% for radial measures and 0.3–3.4% for tibial measures.
The pQCT-derived bone variables included in this study for the 4% site included Bone Mineral Content (g/cm), Total Area (mm2), Total Density (mg/cm3), Trabecular Area (mm2), Trabecular Density (mg/cm3), Cortical Area (mm2) and Cortical Density (mg/cm3). For the 66% site: Bone Mineral Content (g/cm), Total Area (mm2), Total Density (mg/cm3), Cortical Area (mm2), Cortical Density (mg/cm3), Cortical Thickness (mm) and Polar Stress Strain Index (mm3). Polar Stress Strain Index provides data regarding bone bending and torsional strength.
Impact Microindentation (IMI)
An OsteoProbe device (Active Life Technologies, Santa Barbara, CA, USA) was used to perform IMI measurements at the mid-tibia and determine BMSi. The location of the measurements was determined by measuring the midpoint from the medial border of the tibial plateau to the distal edge of the medial malleolus. The measurement area was then disinfected and a local anaesthesia was applied. The probe tip was inserted through the skin to rest on the bone surface. The operator then pressed down on the outer housing of the device to perform the measurements. These measurements were conducted using the international recommended guidelines [22]. As we have reported previously [23], participants experienced minimal discomfort during measurements.
The first measurement was systematically discarded for each participant as it is commonly affected by insufficient penetration through the periosteum. Then at least ten measurements were performed, with the probe tip being moved approximately 2 mm between each one. At the time of data collection, there was no automated system for removal of invalid measurements and therefore we followed the recommended guidelines [22]. Measurements were removed if they appeared outside the “green zone” area indicated by the software, or if the operator reported abnormal bone “texture” during the measurements. There were three trained operators performing IMI measurements during the relevant follow-up phase, however, the majority (90.7%) were performed by a single operator (PR-M). The in-vivo CV for microindentation was 2% for repeated measures. This was calculated by performing the IMI measurement twice for 10 different participants. For each participant, the CV was calculated, showing precision between the two measurements performed. The final CV was expressed as the average of (%) SD/mean for all participants.
Other Data
Weight was measured using electronic scales to the nearest 0.1 kg. Height was measured using a Harpenden stadiometer to the nearest 0.001 m. Body mass index (BMI) was calculated as weight (kg)/height(m)2. Systolic and diastolic blood pressure (mmHg) were measured using an automated device (Takeda Medical UA-751) while the participant was in a seated position. Hypertension was defined as systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg.
The following data were obtained by self-report: Mobility data were collected as previously described [19], using a seven-point scale which included very active, active, sedentary, limited, inactive, chair or bedridden and bedfast. These categories were dichotomised into “high” mobility (very active and active) and “low” mobility (all other categories). Smoking status was categorised as currently smoking or not. Alcohol consumption was collected using a Food Frequency Questionnaire, developed by the Victorian Cancer Council [24]. This was dichotomised into “low” or “high” consumption; < 30 g or ≥ 30 g of alcohol per day, respectively. Prior low trauma fractures were determined by self-report and confirmed using radiological reports where possible, with 71.4% of fractures able to be confirmed. Fractures of the skull, face and digits were excluded. Medication use was self-reported and included angiotensin-converting enzyme inhibitors (ACEI), angiotensin II receptor blockers (ARB), diuretics, dihydropyridine calcium channel blockers (amlodipine, lercanipidine and felodipine), beta blockers and calcium supplements. Men taking oral glucocorticoids (n = 9) or anti-fracture medications (n = 8) were excluded from this study, leaving a total sample size of n = 431. One participant taking spironolactone was included in this study.
A combination of self-reported, measured and linkage data was used to calculate the Charlson comorbidity index (CCI) [25]. Non self-reported data included diabetes status, which was classified as fasting plasma glucose ≥ 7.0 mmol/L (126 mg/dL), self-reported diabetes and/or use of antihyperglycemic medications. Data linkage with the Victorian Cancer Registry provided all data on cancers from 1986 onwards. Rheumatoid arthritis (considered under connective tissue disease) was self-reported and confirmed using medication and medical record data from the major public hospital in the study region, the University Hospital Geelong. Acquired immunodeficiency syndrome was ascertained first through examination of self-reported medications, followed by University Hospital Geelong records. The remaining data for the CCI data were obtained via self-report.
Participant address details at a street level were used to ascertain socioeconomic status using the Index of Relative Socio-Economic Advantage and Disadvantage (IRSAD), which accounts for both disadvantage and advantage and includes income and occupation [26]. The IRSAD scores were divided into quintiles, where quintile 1 represented the most disadvantaged and quintile five the most advantaged.
Study data were collected and managed using REDCap electronic data capture tools hosted at Barwon Health [27, 28]. REDCap (Research Electronic Data Capture) is a secure, web-based software platform designed to support data capture for research studies, providing (1) an intuitive interface for validated data capture; (2) audit trails for tracking data manipulation and export procedures; (3) automated export procedures for seamless data downloads to common statistical packages; and (4) procedures for data integration and interoperability with external sources.
Statistical Analysis
A total of 431 men were included in this study. The Shapiro–Wilk test, examination of box-plots and histograms were used to determine the normality for continuous variables. Weight, height, systolic and diastolic blood pressure and serum calcium were normally distributed and hence were described using means and standard deviations (SD). The remaining continuous variables were described using medians with 25th and 75th percentile (P25 and P75 respectively). Categorical variables were described using frequency and percentage. Differences between groups (those with and without likely primary aldosteronism as well as those with and without possible primary aldosteronism) were determined using t-tests for normally distributed continuous variables, Mann–Whitney tests for skewed continuous variables and chi-squared test for categorical variables.
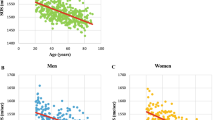
Scatterplots of bone measures and ARR indicated a possible non-linear association, hence ARR values were natural log transformed prior to analyses. Associations between ARR and bone parameters (derived from pQCT or IMI) were assessed using median regression. Both unadjusted and adjusted estimates were reported together with their 95% confidence intervals (CI). The adjusted multivariable median regression models included the following likely confounders: age, weight, height, mobility, smoking status, alcohol consumption, prior fracture, CCI and medications affecting blood pressure (ACEI, ARB, diuretics and dihydropyridine calcium channel blockers). Since weight and height are likely to be correlated, we also performed the analyses using BMI and height instead. Other variables in this study were not included in the models as they were likely to be involved in the causal pathway for the association between ARR and bone parameters (e.g. hypertension and biochemical data). Additionally, due to the small number of men with high ARR values, we avoided including an excessive number of confounders in the models. Analyses were also performed excluding prior fracture to examine if including this variable resulted in over-adjustment in the models.
Additional analyses were conducted comparing bone parameters for men with likely or possible primary aldosteronism, as described in criteria used by Chee et al. [29]. An abnormal screening test for primary aldosteronism (henceforth referred to as “likely” primary aldosteronism), was defined as ARR ≥ 70 pmol/mIU [3], versus those without. Another analysis was also completed which included men categorised as having (i) “likely” primary aldosteronism (ARR ≥ 70 pmol/mIU) or ii) “possible” primary aldosteronism, defined as the presence of low renin concentration (< 15mIU/L) while taking RAAS-active medications that are known to increase renin concentration (ACEIs, ARBs, diuretics, dihydropyridine calcium channel blockers) but not taking a beta blocker, as these tend to reduce renin. These two groups of men [(i) and (ii)] were combined (henceforth referred to as “possible” primary aldosteronism) and compared to those who did not meet either criteria. Median (P25, P75) values for bone parameters were presented and differences between groups were identified using median regression analyses as described above.
An analysis was also completed to examine the association between aldosterone concentration (as a continuous variable) and bone parameters using the same methods as described above.
Bonferroni correction for multiple comparisons was applied, which adjusted the pre-specified level of statistical significance (alpha = 0.05) to alpha = 0.007. Analyses were completed using Minitab (Minitab, version 19, State College, PA, USA) and Stata (Version 17. StataCorp. 2017. Stata Statistical Software: Release 17. College Station, TX: StataCorp LLC).
Results
Descriptive Statistics
A description of participants is shown in Table 1. The median age was 64.7 years, with a range of 33 to 92 years. Overall, participants were in the overweight category for BMI (mean 27.7 kg/m2). Few men were current smokers, and few used calcium supplements (both < 10%). Approximately one in five were “high” consumers of alcohol, one in nine had suffered a previous low trauma fracture and one in ten (9.5%) were taking a beta blocker. Of the whole cohort, 16 (3.7%) had ARR ≥ 70 pmol/mIU.
Some men (38.8%) were taking at least one medication that affects the RAAS system (ACEI, ARB, diuretic and/or dihydropyridine calcium channel blocker). Of these men, 19.2% were also taking a beta blocker. Among men taking a medication that affects the RAAS system and not taking a beta blocker (n = 135), two (1.5%) had ARR ≥ 70 pmol/mIU and 18 (13.3%) had renin < 15 mIU/L. Additionally, there were 48 men with hypertension, and of these, six (12.5%) had ARR ≥ 70 pmol/mIU.
Men with likely primary aldosteronism (ARR ≥ 70 pmol/mIU) were taller (mean ± SD; 177.2 ± 4.8 vs 174.4 ± 6.9 cm, p = 0.035), more likely to have hypertension (37.5% vs 10.1%, p < 0.001) and had lower vitamin D (median P25, P75: 52.0; 37.0–65.8 vs 64.0; 48.0–78.0 nmol/L, p = 0.032) compared to men without likely primary aldosteronism (Supplementary Table 1).
Men with possible primary aldosteronism were more likely to have hypertension (21.9% vs 10.3%, p = 0.045) and higher systolic blood pressure (mean ± SD: 148.8 ± 16.6 vs 139.9 ± 16.4 mmHg, p = 0.006) than men who did not meet the criteria for possible primary aldosteronism (Supplementary Table 2). These men were also older (median P25, P75: 69.1; 61.1–81.9 vs 64.4; 53.7–73.5 years, p = 0.014), had higher sodium blood concentration (median P25, P75: 141; 140–143 vs 140; 139–141 mmol/L, p = 0.016), higher CTx (median P25, P75: 426; 338–626 vs 357; 269–459 ng/L, p = 0.007) and higher P1NP (median P25, P75: 54; 44–67 vs 46; 37–58 mcg/L, p = 0.032). There was also some evidence that these men had higher parathyroid hormone concentration (median P25, P75: 6.2; 4.9–7.9 vs 5.4; 4.3–6.9 pmol/L, p = 0.073) and lower vitamin D (median P25, P75: 53.5; 41.0–71.5 vs 64.0; 48.0–78.0 nmol/L, p = 0.057), but these did not reach statistical significance.
Peripheral Quantitative Computed Tomography (pQCT)
For pQCT measurements, 397 men had a radial scan. Of these, 32 were excluded due to movement (n = 3) or measurement error (e.g. inability to determine the correct reference location, n = 29). There were 386 men who completed a tibial scan. Of these, 30 were excluded due to measurement error. This left 365 radius and 356 tibia scans available for analysis.
ARR as a continuous variable was not associated with any of the bone parameters derived from pQCT in either unadjusted or adjusted analyses. However, there was a trend towards lower adjusted bone mineral content at the tibia 4% site (Table 2).
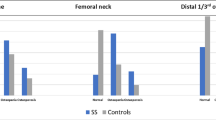
Men with likely primary aldosteronism (ARR ≥ 70 pmol/mIU, n = 16) had lower adjusted total area at the 66% radial site (− 12.5% compared to median for those without primary aldosteronism, Table 3). There were also trends towards lower adjusted bone mineral content at the 4% radial and tibial sites as well as the 66% radial site.
There were no differences observed between men with and without possible primary aldosteronism (ARR ≥ 70 pmol/mIU or taking a RAAS affecting medication except beta blocker and renin < 15 mU/L, n = 32). However, there was a trend towards lower adjusted bone mineral content at the radial and tibial 4% sites, as well as polar stress strain index at the tibial 66% site (Table 4).
There were no associations observed between aldosterone concentration as a continuous variable and any of the bone parameters derived from pQCT (Table 5).
Impact Microindentation (IMI)
For IMI, 332 men completed the measurement. Exclusions for 99 men were: excessive soft tissue over the tibia (n = 65), skin condition (n = 14), needle phobia (n = 7), discomfort during measurement (pressure, not pain, n = 4), no reason given (n = 8) and unable to provide informed consent (n = 1).
The median BMSi among all men was 83.1 (P25, P75: 78.5 to 87.3). There was no association detected between ARR (continuous variable) and BMSi in unadjusted (β = 0.671 95%CI − 0.086, 1.428; p = 0.082) or adjusted analyses (β = − 0.029 95%CI − 0.756, 0.698; p = 0.938).
The median BMSi for men with likely primary aldosteronism (n = 10) was comparable to those with lower ARR (83.3 [P25, P75: 75.4–86.6] vs 83.1 [P25, P75: 78.5–87.3], p = 0.643). In adjusted analyses, no differences were observed (β = − 0.124 95%CI − 4.751, 4.503; p = 0.958).
The median BMSi for men with possible primary aldosteronism (ARR ≥ 70 pmol/mIU or taking a RAAS affecting medication except beta blocker and renin < 15 mU/L, n = 19) was also similar to those who did not meet the criteria (85.7 [P25, P75: 79.6–87.4] vs 83.0 [P25, P75: 78.5–87.3], p = 0.459). In adjusted analyses, no differences were observed (β = 1.054 95%CI − 2.300, 4.408; p = 0.537).
For aldosterone concentration (continuous variable), there was no association with BMSi in unadjusted (β = 1.008 95%CI − 0.828, 2.844; p = 0.281) or adjusted (β = 0.177 95%CI − 1.460, 1.813; p = 0.832) analyses.
For models (both pQCT and IMI) that included BMI and height instead of weight and height, the results were similar (data not shown). Excluding prior fracture also did not change the results.
Discussion
This study investigated associations between ARR and bone parameters derived from pQCT and IMI techniques. The ARR as a continuous variable was not associated with any pQCT-derived bone parameters. Additionally, no associations were observed for aldosterone concentration as a continuous variable with any of the bone parameters. However, the men who had likely primary aldosteronism (ARR ≥ 70 pmol/mIU [3]) had lower bone total area (66% radial site) compared to those who did not have likely primary aldosteronism. There were also trends towards lower bone mineral content (4% radial and tibial, 66% radial sites). When we also included men who had low renin concentrations (< 15 mU/L) despite taking RAAS-active medications which should increase renin (those taking beta blockers were excluded), the results were similar, with trends towards lower bone mineral content (4% radial and tibial sites) and polar stress strain index (66% tibial site) in men who met these criteria. The association for lower adjusted bone area in men with likely primary aldosteronism was only observed following adjustment for other variables, in particular height, which was different between those with and without likely primary aldosteronism (Supplementary Table 1). Overall, the data may suggest that an ARR above the physiologic range could have deleterious effects on bone health.
The reason for the trends in bone deficits observed for men with likely/possible primary aldosteronism are not clear. However, compared to men without likely primary aldosteronism, those with likely primary aldosteronism had lower vitamin D. For the group of men meeting the definition for possible primary aldosteronism, there was a trend towards elevated parathyroid hormone and lower vitamin D. Similar observations with elevated parathyroid hormone and reduced vitamin D for individuals with primary aldosteronism have also been reported in other studies [6, 9, 10]. Additionally, a clinical trial [30] following men over an 8 year period, showed that for those with vitamin D deficiency (≤ 20 ng/mL), total BMD, cortical BMD, cortical area and cortical thickness measured using high-resolution pQCT at the distal radius all declined faster over time than for men with sufficient vitamin D. The study also reported that men in the two highest quartiles of parathyroid hormone had a faster decline in total BMD, cortical thickness, cortical area and cortical BMD at the distal radius than those in the lowest quartile of parathyroid hormone.
Another potential mechanism could be similar to that observed in primary hyperparathyroidism, characterised by chronically elevated parathyroid hormone concentrations, resulting in increased bone turnover, favouring bone resorption [31]. Elevated bone resorption can lead to bone loss and result in a lower bone mineral content. Men with possible primary aldosteronism also had higher levels of bone turnover markers, which supports this potential mechanism. Due to a lack of literature on this topic, we do not have a clear mechanism for the observed results, particularly for the changes in bone area. However, if these results are replicated in future work, novel research studies would be valuable to determine the mechanisms involved in associations between bone parameters and elevated ARR values.
Of note, IMI was not different between the groups. This might be explained either by the point of measurement, at the tibia, where the impact of the ARR seems less pronounced, or by an undetectable effect on the properties measured by the technique.
Only one previous study has examined associations between aldosterone, renin and ARR values with pQCT-derived bone parameters [16]. The study, which included 373 participants of African ancestry, reported that higher renin activity was associated with an increased trabecular BMD. These results are similar to our study, since higher renin activity corresponds to a lower ARR and there was a trend towards greater ARR and lower bone mineral content (tibia 4% site). The authors of the previous study suggested that since their participants were not selected on the basis of disease, BMD may not be affected unless the RAAS has been disrupted substantially. The ARR as a continuous variable may not have been associated with any of the pQCT bone parameters since the participants in our study were not selected on the basis of disease and most had ARR within the physiological range. Indeed, the analysis including men with and without likely primary aldosteronism showed that outside the normal physiological range of ARR, bone area was lower.
There are few studies investigating associations between ARR or primary aldosteronism and bone health. Individuals with primary aldosteronism have been reported to have a higher risk of fracture [9, 12] and poorer trabecular bone score [14]. Further studies are needed to confirm these observations, conduct similar analyses in women as well as explore the possible mechanisms for the bone health deficits for individuals with primary aldosteronism.
In cases where aldosterone concentrations are outside the normal range, treatments targeting these elevated concentrations may also result in improved bone health. In a review article describing primary aldosteronism and bone metabolism [9], the authors highlighted that bone loss in primary aldosteronism can be reversed with treatment (either medication or surgery). Additionally, a study by Hu et al. showed that anti-osteoporosis therapy was associated with altered concentrations of aldosterone and renin [32]. The study included postmenopausal women with osteoporosis, who were treated with either alendronate or parathyroid hormone for 48 weeks. The results showed that aldosterone and renin decreased after the treatment period. The authors also highlighted that women with postmenopausal osteoporosis can often have false-positive ARR screening and care should be taken when interpreting ARR levels. Zhang et al. [33] have described how treatment with a renin inhibitor resulted in increased trabecular bone in ovariectomised mice. Further investigation of the effects of excess aldosterone on bone may improve the understanding of osteopenia or osteoporosis that cannot be explained by another known cause [6].
This study has a number of strengths and limitations. One strength is that the participants were randomly selected from the population and the results are thus more generalisable than if the participants were selected on the basis of disease. An advantage of using a population-based sample was also a large sample size. However, there may be a bias towards healthier individuals participating in the study, which may have affected the results. The measurement of aldosterone and renin (and thus the calculated ARR values) may have been affected by several factors that we were not able to control, including posture, time of day, salt intake and medication [3]. Some of these factors were managed well in this study; for example, participants were asked to fast prior to providing a blood sample and thus 90% had their blood withdrawn in the morning, likely in a seated position. We did not ask participants to change their diet and thus salt intake was not controlled. Urinary sodium values as a marker of salt intake were not available, nor were urinary calcium values. Additionally, participants were not asked to modify their medications, but data for several important medication types were included in the analyses (ACEIs, ARBs, diuretics, dihydropyridine calcium channel blockers, beta blockers). Another limitation is that only one measurement of aldosterone and renin was performed and the number of participants with likely primary aldosteronism was small (N = 16). We used the criterion of ARR ≥ 70 pmol/mIU to categorise “likely” primary aldosteronism, however, it has been reported that ARR in the range 70–100 pmol/mIU is a “grey zone” [3] and that a value ≥ 100 pmol/mIU is a more robust cut-point. Unfortunately in this study we did not have a sufficient number of participants with ARR ≥ 100 pmol/mIU to use this higher cut-point. However, we also performed analyses with a larger group of men who had possible primary aldosteronism, specifically including those with a low renin concentration despite using medications which should increase renin, while excluding those taking beta blockers which tend to lower renin and increase the ARR. Although we included a range of potential confounders in the adjusted models, it is possible that there was residual confounding. The study included only men, which is important because there is likely a sex difference in the effect of aldosterone and renin on bone [34], and future studies will need to include female participants. At the time of writing, data are still being collected for pQCT and IMI in the next follow-up phase for women enrolled in the Geelong Osteoporosis Study (2022 onwards). Since this is a cross-sectional study, the effect on longitudinal outcomes such as fracture risk is unknown and would be an important research question for future studies.
Conclusion
There were no associations detected between ARR or aldosterone concentration and bone parameters derived from pQCT. However, men with likely primary aldosteronism (ARR ≥ 70 pmol/mIU) had lower total bone area. The observations suggest that bone may be adversely affected when the ARR is above physiological levels. Future work should include women and longitudinal studies with larger sample size to determine the risk of fracture for individuals with elevated ARR.
References
Ferreira NS, Tostes RC, Paradis P, Schiffrin EL (2021) Aldosterone, inflammation, immune system, and hypertension. Am J Hypertens 34:15–27. https://doi.org/10.1093/ajh/hpaa137
Loh HH, Sukor N (2020) Associations between primary aldosteronism and diabetes, poor bone health, and sleep apnea—what do we know so far? J Hum Hypertens 34:5–15. https://doi.org/10.1038/s41371-019-0294-8
Stowasser M, Taylor P, Pimenta E et al (2010) Laboratory investigation of primary aldosteronism. Clin Biochem Rev 31:39–56
Funder JW, Carey RM, Mantero F et al (2016) The management of primary aldosteronism: case detection, diagnosis, and treatment: an endocrine society clinical practice guideline. J Clin Endocrinol Metab 101:1889–1916. https://doi.org/10.1210/jc.2015-4061
Beavan S, Horner A, Bord S et al (2001) Colocalization of glucocorticoid and mineralocorticoid receptors in human bone. J Bone Miner Res 16:1496–1504. https://doi.org/10.1359/jbmr.2001.16.8.1496
Altieri B, Muscogiuri G, Paschou SA et al (2018) Adrenocortical incidentalomas and bone: from molecular insights to clinical perspectives. Endocrine 62:506–516. https://doi.org/10.1007/s12020-018-1696-z
Mo C, Ke J, Zhao D, Zhang B (2020) Role of the renin–angiotensin–aldosterone system in bone metabolism. J Bone Miner Metab 38:772–779. https://doi.org/10.1007/s00774-020-01132-y
Liu D, Wang Y, Pan Z et al (2020) cAMP regulates 11β-hydroxysteroid dehydrogenase-2 and Sp1 expression in MLO-Y4/MC3T3-E1 cells. Exp Ther Med 20:2166–2172. https://doi.org/10.3892/etm.2020.8942
Shi S, Lu C, Tian H et al (2020) Primary aldosteronism and bone metabolism: a systematic review and meta-analysis. Front Endocrinol. https://doi.org/10.3389/fendo.2020.574151
Armanini D, Andrisani A, Ambrosini G et al (2016) Interrelationship between vitamin D insufficiency, calcium homeostasis, hyperaldosteronism, and autoimmunity. J Clin Hypertens 18:614–616. https://doi.org/10.1111/jch.12822
Papandreou D, Malindretos P, Karabouta Z, Rousso I (2010) Possible health implications and low vitamin D status during childhood and adolescence: an updated mini review. Int J Endocrinol doi 10:11
Wu V-C, Chang C-H, Wang C-Y et al (2017) Risk of fracture in primary aldosteronism: a population-based cohort study. J Bone Miner Res 32:743–752. https://doi.org/10.1002/jbmr.3033
Hans D, Barthe N, Boutroy S et al (2011) Correlations between trabecular bone score, measured using anteroposterior dual-energy X-ray absorptiometry acquisition, and 3-dimensional parameters of bone microarchitecture: an experimental study on human cadaver vertebrae. J Clin Densitom 14:302–312. https://doi.org/10.1016/j.jocd.2011.05.005
Kim B-J, Kwak MK, Ahn SH et al (2018) Lower trabecular bone score in patients with primary aldosteronism: human skeletal deterioration by aldosterone excess. J Clin Endocrinol Metab 103:615–621. https://doi.org/10.1210/jc.2017-02043
Pawlowska M, Bilezikian JP (2016) Beyond DXA: advances in clinical applications of new bone imaging technology. Endocr Pr 22:990–998. https://doi.org/10.4158/ep151019.ra
Kuipers AL, Kammerer CM, Pratt JH et al (2016) Association of circulating renin and aldosterone with osteocalcin and bone mineral density in African ancestry families. Hypertension 67:977–982. https://doi.org/10.1161/HYPERTENSIONAHA.115.06837
Bridges D, Randall C, Hansma PK (2012) A new device for performing reference point indentation without a reference probe. Rev Sci Instrum 83:44301
Randall C, Bridges D, Guerri R et al (2013) Applications of a new handheld reference point indentation instrument measuring bone material strength. J Med Device 7:41005
Pasco JA, Nicholson GC, Kotowicz MA (2012) Cohort profile: geelong osteoporosis study. Int J Epidemiol 41:1565–1575
Blew RM, Lee VR, Farr JN et al (2014) Standardizing evaluation of pQCT image quality in the presence of subject movement: qualitative versus quantitative assessment. Calcif Tissue Int 94:202–211. https://doi.org/10.1007/s00223-013-9803-x
Wong AK (2016) A comparison of peripheral imaging technologies for bone and muscle quantification: a technical review of image acquisition. J Musculoskelet Neuronal Interact 16:265–282
Diez-Perez A, Bouxsein ML, Eriksen EF et al (2016) Technical note: recommendations for a standard procedure to assess cortical bone at the tissue-level in vivo using impact microindentation. Bone Rep 5:181–185. https://doi.org/10.1016/j.bonr.2016.07.004
Rufus-Membere PG, Holloway-Kew KL, Diez-Perez A et al (2018) Feasibility and tolerability of bone impact microindentation testing: a cross-sectional, population-based study in Australia. BMJ Open 8:e023959. https://doi.org/10.1136/bmjopen-2018-023959
Giles GG, Ireland PD (1996) Dietary questionnaire for epidemiological studies (Version 2), Melbourne. Cancer Counc Victoria
Charlson ME, Pompei P, Ales KL, MacKenzie CR (1987) A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40:373–383
Australian Bureau of Statistics (2016) Census of population and housing: socio-economic indexes for areas (SEIFA), Australia, 2016. https://www.abs.gov.au/ausstats/abs@.nsf/Lookup/bySubject/2033.0.55.001~2016~MainFeatures~IRSAD~20
Harris PA, Taylor R, Minor BL et al (2019) The REDCap consortium: Building an international community of software platform partners. J Biomed Inform 95:103208. https://doi.org/10.1016/j.jbi.2019.103208
Harris PA, Taylor R, Thielke R et al (2009) Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform 42:377–381. https://doi.org/10.1016/j.jbi.2008.08.010
Chee MR, Hoo J, Libianto R et al (2021) Prospective screening for primary aldosteronism in patients with suspected obstructive sleep Apnea. Hypertens 77:2094–2103. https://doi.org/10.1161/HYPERTENSIONAHA.120.16902
Bobillier A, Wagner P, Whittier DE et al (2022) Association of vitamin D and parathyroid hormone status with the aging-related decline of bone microarchitecture in older men: the prospective structure of aging men’s bones (STRAMBO) study. J Bone Miner Res 37:1903–1914. https://doi.org/10.1002/jbmr.4657
Makras P, Anastasilakis AD (2018) Bone disease in primary hyperparathyroidism. Metabolism 80:57–65. https://doi.org/10.1016/j.metabol.2017.10.003
Hu Q, Liao K, Zhang L et al (2020) Effects of anti-osteoporosis therapy on plasma aldosterone and renin. J Renin Angiotensin Aldosterone Syst 21:1470320320928874
Zhang Y, Wang L, Song Y et al (2016) Renin inhibitor aliskiren exerts beneficial effect on trabecular bone by regulating skeletal renin-angiotensin system and kallikrein-kinin system in ovariectomized mice. Osteoporos Int 27:1083–1092. https://doi.org/10.1007/s00198-015-3348-y
Komukai K, Mochizuki S, Yoshimura M (2010) Gender and the renin–angiotensin–aldosterone system. Fundam Clin Pharmacol 24:687–698. https://doi.org/10.1111/j.1472-8206.2010.00854.x
Acknowledgements
This study was funded by grant support of Amgen Inc. and the National Health and Medical Research Council (NHMRC; grants 251638, 299831, 628582), but they played no role in the collection or interpretation of data. KLH-K is supported by an Alfred Deakin Postdoctoral Research Fellowship; KBA by an Australian Government Research Training Program Scholarship; PR-M by a Deakin University Postgraduate Industry Research Scholarship; MT by a Deakin Postgraduate Scholarship; SXS and NKH by Dean’s Research Postdoctoral Fellowships (Deakin University). SMG received an Institute for Mental and Physical Health and Clinical Translation Seed Funding Grant which supported the measurement of aldosterone and renin. AD-P owns shares of Active Life Scientific, Inc., the manufacturer of the reference point indentation device. MH supports his research activities from his own savings. MAK, W-HL, MH and JAP declare they have no conflict of interest. The Hudson Institute is supported by the Victorian Government’s Operational Infrastructure Scheme. The authors thank Professor Graham Giles of the Cancer Epidemiology Centre of The Cancer Council Victoria, for permission to use the Dietary Questionnaire for Epidemiological Studies (Version 2), Melbourne: The Cancer Council Victoria 1996. The authors also thank the Victorian Cancer Register for data linkage.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. Amgen Inc., National Health and Medical Research Council, 251638, Julie A Pasco, 299831, Julie A Pasco, 628582, Julie A Pasco, Alfred Deakin Postdoctoral Research Fellowship, Australian Government Research Training Program Scholarship, Deakin University Postgraduate Industry Research Scholarship, Deakin Postgraduate Scholarship, Dean’s Research Postdoctoral Fellowship (Deakin University), Institute for Mental and Physical Health and Clinical Translation Seed Funding Grant, Victorian Government Operational Infrastructure Scheme.
Author information
Authors and Affiliations
Contributions
Conceptualisation: KLH-K, SMG, MH, W-HL. Data curation: JAP. Formal Analysis: KLH-K, SMG. Funding acquisition: KLH-K, SMG, JY, JAP. Investigation: KLH-K, KBA, PR-M, MCT, SXS, NKH, JY. Methodology: KLH-K, SMG, JY. Project administration: JAP. Resources: MAK, JAP. Supervision: JAP. Validation: KLH-K. Visualisation: KLH-K. Writing – original draft: KLH-K. Writing – review & editing: KLH-K, KBA, PR-M, MCT, SXS, NKH, MAK, SMG, JY, AD-P, MH, W-HL and JAP.
Corresponding author
Ethics declarations
Competing Interest
AD-P owns shares of Active Life Scientific, Inc., the manufacturer of the reference point indentation device. KLH-K, KBA, PR-M, MCT, SXS, NKH, MAK, SMG, JY, MH, W-HL and JAP have no competing interests to declare.
Ethical Approval
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Barwon Health Human Research Ethics Committee (project 00/56). Each participant provided informed consent to participate in the study and allow access to their medical records.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent for Publication
For this type of study formal consent is not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Holloway-Kew, K.L., Anderson, K.B., Rufus-Membere, P. et al. Associations Between Aldosterone-Renin-Ratio and Bone Parameters Derived from Peripheral Quantitative Computed Tomography and Impact Microindentation in Men. Calcif Tissue Int 113, 496–510 (2023). https://doi.org/10.1007/s00223-023-01131-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-023-01131-x