Abstract
Summary
Sheehan’s syndrome (SS) is a rare but well-characterized cause of hypopituitarism. Data on skeletal health is limited and on microarchitecture is lacking in SS patients.
Purpose
We aimed to explore skeletal health in SS with bone mineral density (BMD), turnover, and microarchitecture.
Methods
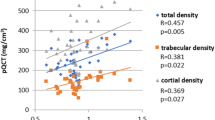
Thirty-five patients with SS on stable replacement therapy for respective hormone deficiencies and 35 age- and BMI-matched controls were recruited. Hormonal profile and bone turnover markers (BTMs) were measured using electrochemiluminescence assay. Areal BMD and trabecular bone score were evaluated using DXA. Bone microarchitecture was assessed using a second-generation high-resolution peripheral quantitative computed tomography.
Results
The mean age of the patients was 45.5 ± 9.3 years with a lag of 8.3 ± 7.2 years prior to diagnosis. Patients were on glucocorticoid (94%), levothyroxine (94%), and estrogen–progestin replacement (58%). None had received prior growth hormone (GH) replacement. BTMs (P1NP and CTX) were not significantly different between patients and controls. Osteoporosis (26% vs. 16%, p = 0.01) and osteopenia (52% vs. 39%, p = 0.007) at the lumbar spine and femoral neck (osteoporosis, 23% vs. 10%, p = 0.001; osteopenia, 58% vs. 29%, p = 0.001) were present in greater proportion in SS patients than matched controls. Bone microarchitecture analysis revealed significantly lower cortical volumetric BMD (vBMD) (p = 0.02) at the tibia, with relative preservation of the other parameters.
Conclusion
Low areal BMD (aBMD) is highly prevalent in SS as compared to age- and BMI-matched controls. However, there were no significant differences in bone microarchitectural measurements, except for tibial cortical vBMD, which was lower in adequately treated SS patients.


Similar content being viewed by others
Data Availability
The data that support the findings of this study are available on reasonable request from the corresponding author.
References
Das L, Dutta P (2023) Approach to the patient: a case with an unusual cause of hypopituitarism. J Clin Endocrinol Metab 108(6):1488–1504
Ramiandrasoa C, Castinetti F, Raingeard I, Fenichel P, Chabre O, Brue T, Courbiere B (2013) Delayed diagnosis of Sheehan’s syndrome in a developed country: a retrospective cohort study. Eur J Endocrinol 169(4):431–438
Das L, Sahoo J, Dahiya N, Taneja S, Bhadada SK, Bhat MH, Singh P, Suri V, Laway BA, Dutta P (2022) Long-term hepatic and cardiac health in patients diagnosed with Sheehan’s syndrome. Pituitary 25(6):971–981
Laway BA, Rasool A, Baba MS, Misgar RA, Bashir MI, Wani AI, Choh N, Shah O, Lone A, Shah Z (2023) High prevalence of coronary artery calcification and increased risk for coronary artery disease in patients with Sheehan syndrome-a case-control study. Clin Endocrinol (Oxf) 98(3):375–382. https://doi.org/10.1111/cen.14871
Laway BA, Ramzan M, Allai MS, Wani AI, Misgar RA (2016) Cardiac structural and functional abnormalities in females with untreated hypopituitarism due to Sheehan syndrome: response to hormone replacement therapy. Endocr Pract 22(9):1096–1103
Chihaoui M, Yazidi M, Chaker F, Belouidhnine M, Kanoun F, Lamine F, Ftouhi B, Sahli H, Slimane H (2016) Bone mineral density in Sheehan’s syndrome; prevalence of low bone mass and associated factors. J Clin Densitom 19(4):413–418
Agarwal P, Gomez R, Bhatia E, Yadav S (2019) Decreased bone mineral density in women with Sheehan’s syndrome and improvement following oestrogen replacement and nutritional supplementation. J Bone Miner Metab 25(37):171–178
Gokalp D, Tuzcu A, Bahceci M, Arikan S, Ozmen CA, Cil T (2009) Sheehan’s syndrome and its impact on bone mineral density. Gynecol Endocrinol 25(5):344–349
Ragnar Agnarsson H, Johannsson G, Ragnarsson O (2014) The impact of glucocorticoid replacement on bone mineral density in patients with hypopituitarism before and after 2 years of growth hormone replacement therapy. J Clin Endocrinol Metab 99(4):1479–1485
Ragnarsson O, Nyström HF, Johannsson G (2012) Glucocorticoid replacement therapy is independently associated with reduced bone mineral density in women with hypopituitarism. Clin Endocrinol 76(2):246–252
Zaidi M, Yuen T, Kim SM (2023) Pituitary crosstalk with bone, adipose tissue and brain. Nat Rev Endocrinol 15:1–4
Wang J, Zhang W, Yu C, Zhang X, Zhang H, Guan Q, Zhao J, Xu J (2015) Follicle-stimulating hormone increases the risk of postmenopausal osteoporosis by stimulating osteoclast differentiation. PLoS One 10(8):e0134986
Seeman EH, Wahner HW, Offord KP, Kumar R, Johnson WJ, Riggs BL (1982) Differential effects of endocrine dysfunction on the axial and the appendicular skeleton. J Clin Investig 69(6):1302–1309
Whittier DE, Boyd SK, Burghardt AJ, Paccou J, Ghasem-Zadeh A, Chapurlat R, Engelke K, Bouxsein ML (2020) Guidelines for the assessment of bone density and microarchitecture in vivo using high-resolution peripheral quantitative computed tomography. Osteoporos Int 31:1607–1627
Agarwal S, Rosete F, Zhang C, McMahon DJ, Guo XE, Shane E, Nishiyama KK (2016) In vivo assessment of bone structure and estimated bone strength by first-and second-generation HR-pQCT. Osteoporos Int 27:2955–2966
Sode M, Burghardt AJ, Pialat JB, Link TM, Majumdar S (2011) Quantitative characterization of subject motion in HR-pQCT images of the distal radius and tibia. Bone 48(6):1291–1297
Mikolajewicz N, Bishop N, Burghardt AJ, Folkestad L, Hall A, Kozloff KM, Lukey PT, Molloy-Bland M, Morin SN, Offiah AC, Shapiro J (2020) HR-pQCT measures of bone microarchitecture predict fracture: systematic review and meta-analysis. J Bone Miner Res 35(3):446–459
Das L, Dutta P (2023) Unusual and lesser-known rare causes of adult growth hormone deficiency. Best Pract Res Clin Endocrinol Metab 28:101820
Kandemir N, Gone EN, Yord N (2002) Responses of bone turnover markers and bone mineral density to growth hormone therapy in children with isolated growth hormone deficiency and multiple pituitary hormone deficiencies. J Pediatr Endocrinol Metab 15(6):809–816
Behan LA, Kelleher G, Hannon MJ, Brady JJ, Rogers B, Tormey W, Smith D, Thompson CJ, McKenna MJ, Agha A (2014) Low-dose hydrocortisone replacement therapy is associated with improved bone remodelling balance in hypopituitary male patients. Eur J Endocrinol 170(1):141–150
Ragnarsson O, Nyström HF, Johannsson G (2012) Glucocorticoid replacement therapy is independently associated with reduced bone mineral density in women with hypopituitarism. Clin Endocrinol 76(2):246–252
Hardy RS, Zhou H, Seibel MJ, Cooper MS (2018) Glucocorticoids and bone: consequences of endogenous and exogenous excess and replacement therapy. Endocr Rev 39(5):519–548
Toogood AA, Taylor NF, Shalet SM, Monson JP (2000) Modulation of cortisol metabolism by low-dose growth hormone replacement in elderly hypopituitary patients. J Clin Endocrinol Metab 85(4):1727–1730. https://doi.org/10.1210/jcem.85.4.6505
Frey KR, Kienitz T, Schulz J, Ventz M, Zopf K, Quinkler M (2018) Prednisolone is associated with a worse bone mineral density in primary adrenal insufficiency. Endocr Connect 7(6):811–818
Vestergaard P, Rejnmark L, Mosekilde L (2008) Fracture risk associated with different types of oral corticosteroids and effect of termination of corticosteroids on the risk of fractures. Calcif Tissue Int 82:249–257
Garton M, Reid I, Loveridge N, Robins S, Murchison L, Beckett G, Reid D (1994) Bone mineral density and metabolism in premenopausal women taking l-thyroxine replacement therapy. Clin Endocrinol 41(6):747–755
Sheng N, Xing F, Wang J, Duan X, Xiang Z (2023) T4 rather than TSH correlates with BMD among euthyroid adults. Front Endocrinol 9(13):1039079
de Bakker CM, Tseng WJ, Li Y, Zhao H, Liu XS (2017) Clinical evaluation of bone strength and fracture risk. Curr Osteoporos Rep 15:32–42
Riggs BL, Melton LJ III, Robb RA, Camp JJ, Atkinson EJ, Peterson JM, Rouleau PA, McCollough CH, Bouxsein ML, Khosla S (2004) Population-based study of age and sex differences in bone volumetric density, size, geometry, and structure at different skeletal sites. J Bone Miner Res 19(12):1945–1954
Mazziotti G, Frara S, Giustina A (2018) Pituitary diseases and bone. Endocr Rev 39(4):440–488
Giustina A, Mazziotti G, Canalis E (2008) Growth hormone, insulin-like growth factors, and the skeleton. Endocr Rev 29(5):535–559
Hyldstrup L, Conway GS, Racz K, Keller A, Chanson P, Zacharin M, Lysgaard AL, Andreasen AH, Kappelgaard AM (2012) Growth hormone effects on cortical bone dimensions in young adults with childhood-onset growth hormone deficiency. Osteoporos Int 23:2219–2226
Tanriverdi F, Unluhizarci KÜ, Kula MU, Guven M, Bayram FA, Kelestimur F (2005) Effects of 18-month of growth hormone (GH) replacement therapy in patients with Sheehan’s syndrome. Growth Hormon IGF Res 15(3):231–237
Balducci R, Toscano V, Pasquino AM, Mangiantini A, Municchi G, Armenise P, Terracina S, Prossomariti G, Boscherini B (1995) Bone turnover and bone mineral density in young adult patients with panhypopituitarism before and after long-term growth hormone therapy. Eur J Endocrinol 132(1):42–46
Clarke B (2008) Normal bone anatomy and physiology. Clin J Am Soc Nephrol 3(Supplement 3):S131–S139
Cheung WH, Hung VW, Cheuk KY, Chau WW, Tsoi KK, Wong RM, Chow SK, Lam TP, Yung PS, Law SW, Qin L (2021) Best Performance parameters of HR-pQCT to predict fragility fracture: systematic review and meta-analysis. J Bone Miner Res 36(12):2381–2398
Acknowledgements
We wish to acknowledge Mr. Nipun Chawla and Mr. Raman Saini for helping in the HRpQCT data acquisition.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Das, L., Laway, B.A., Sahoo, J. et al. Bone mineral density, turnover, and microarchitecture assessed by second-generation high-resolution peripheral quantitative computed tomography in patients with Sheehan’s syndrome. Osteoporos Int 35, 919–927 (2024). https://doi.org/10.1007/s00198-024-07062-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-024-07062-z