Abstract
Autoimmune polyendocrine syndrome type-1 (APS1) is characterized by autoimmune manifestations affecting different organs from early childhood on. Immunological abnormalities, the resulting endocrinopathies, and their treatments may compromise bone health. For the first time in APS1, we analyzed transiliac bone biopsy samples by bone histomorphometry and quantitative backscattered electron imaging in three adult patients (female P1, 38 years; male P2, 47 years; male P3, 25 years). All had biallelic mutations in the autoimmune regulator gene and in addition to endocrinopathies, also significant bone fragility. Histomorphometry showed bone volume in the lower normal range for P1 (BV/TV, − 0.98 SD) and P3 (− 1.34 SD), mainly due to reduced trabecular thickness (TbTh, − 3.63 and − 2.87 SD). In P1, osteoid surface was low (OS/BS, − 0.96 SD); active osteoblasts and double labeling were seen only on cortical bone. P3 showed a largely increased bone turnover rate (BFR/BV, + 4.53 SD) and increased mineralization lag time (Mlt, + 3.40 SD). Increased osteoid surface (OS/BS, + 2.03 and + 4.71 SD for P2 and P3) together with a large proportion of lowly mineralized bone area (Trab CaLow, + 2.22 and + 9.81 SD for P2 and P3) and focal mineralization defects were consistent with abnormal mineralization. In all patients, the density and area of osteocyte lacunae in cortical and trabecular bone were similar to healthy adults. The bone tissue characteristics were variable and included decreased trabecular thickness, increased amount of osteoid, and abnormal mineralization which are likely to contribute to bone fragility in patients with APS1.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
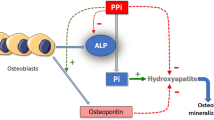
Autoimmune polyendocrine syndrome type 1 (APS1, OMIM #240,300), also known as autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy is a rare autoimmune disease with mutations in the autoimmune regulator (AIRE) gene. These lead to impaired expression of tissue-specific proteins in thymus, resulting in failure of negative selection of self-reactive T cells [1] and impaired regulatory T cell function [2]. Defects translate into organ-specific autoimmune diseases [3]. Majority of patients develop hypoparathyroidism and/or adrenocortical insufficiency during childhood requiring lifelong treatment [3].
Immunological abnormalities, endocrinopathies, and their treatments may impact bone health in patients with APS1. Our previous study associated impaired bone characteristics with disease severity [4]. We found multiple non-spinal fractures in 23% and spinal compression fractures in 7% of patients. Peripheral quantitative computer tomography (pQCT) showed reduced cortical thickness and trabecular volumetric bone mineral density (BMD) in patients with ≥ 7 disease manifestations while in more mildly affected patients these values were similar to controls [4].
We therefore set out to further examine the bone properties in patients with APS1. Here we provide a histomorphometric, mineral content, and osteocyte lacunae analysis of bone tissue in transiliac bone biopsy samples of three APS1 patients with osteoporotic BMD or vertebral compression fractures.
Patients and Methods
Patients
During a cross-sectional study on APS1, we evaluated comprehensively bone health in 44 patients. Osteoporotic BMD was found in four adults, and vertebral fractures in three additional patients [4]. Four of these seven patients were eligible for a bone biopsy procedure for research purposes, and three of them gave the informed consent to participate in the study. This study followed the principles of the Declaration of Helsinki and was approved by the Helsinki University Hospital ethics committee (HUS/1088/2016).
Clinical Studies
Data on disease manifestations, their treatments, and fracture history were reviewed. Biochemical parameters were evaluated on the day of biopsy from peripheral blood obtained in the morning after an overnight fast. BMD was measured with dual-energy x-ray assessment and bone characteristics with pQCT as described previously [4]. T-scores for the total volumetric BMD (vBMD) and trabecular vBMD at distal site as well as for cortical vBMD at proximal radial site were calculated according to references [5, 6].
Bone Biopsies
Transiliac bone biopsy samples of the anterior superior iliac crest were obtained with a trephine having an inner diameter of 7.5 mm (Rochester Bone Biopsy; Medical Innovations International, Rochester, MN, USA). The preceding tetracycline labeling followed a routine protocol: two courses of oral tetracycline (500 mg twice daily for 2 consecutive days), with a 12-day interval, with biopsy obtained 5 days after the second course.
Sample Preparation and Bone Histomorphometry
Samples were fixed in ethanol (70%), gradually dehydrated with increasing concentrations of ethanol and embedded in polymethylmethacrylate according to standard protocols[7]. 5-μm-thick sections were stained with modified Masson Goldner trichrome stain. Quantitative bone histomorphometry was performed on the complete cancellous bone area using Osteomeasure system (OsteoMetrics, Atlanta, GA, USA). The nomenclature and parameters follow the recommendations by the American Society for Bone and Mineral Research [8]. Each sample was evaluated under bright light, polarized light, and fluorescence microscopy using a magnification of 200-fold. Z-values for histomorphometric parameters were calculated according to Rehman et al. [9].
Bone Mineralization Density Distribution (BMDD)
The procedure to obtain BMDD curves using quantitative backscattered electron imaging (qBEI) is described in detail elsewhere [10]. The BMDD curve is the frequency distribution of measured calcium content normalized to 100% bone area. The curve is characterized by 5 parameters: (i) CaMean, the mean calcium content, (ii) CaPeak, the most frequent calcium concentration, (iii) CaWidth, the full width at half maximum of the curve reflecting the mineralization heterogeneity, (iv) CaLow and (v) CaHigh measure the amount of bone area mineralized below the 5th and above the 95th percentile of the adult trabecular reference curve, respectively. BMDD curves were obtained separately for trabecular and cortical compartments and compared to healthy adult reference curves published by Hartmann et al. [10].
Osteocyte Lacunae Sections
Osteocyte lacunae sections (OLS) were analyzed on images obtained from calibrated qBEI measurements with a resolution increased to 0.88 µm per pixel. The size of the OLS was determined by setting a calcium threshold of 5.2 wt%. Parameters calculated were OLS-density (the number of osteocyte lacunae per bone area) and OLS-area (the mean area of OLS). OLS were defined as pores between 5 and 200 µm2 in size—see detailed description in Mähr et al. [11]. Data were compared against results from two healthy adults published previously [12].
Results
Clinical Data
The clinical characteristics of the three adult patients with APS1 (female P1: 38 years; male P2: 47 years; male P3: 25 years) are shown in Table 1. As signs of osteoporosis, P1 had experienced a vertebral compression fracture, whereas P2 and P3 had osteoporotic BMD. P3 had experienced five fractures due to high-energy accidents; all the fractures had been treated successfully with immobilization 4–12 years before bone biopsy. None of the patients were treated with bisphosphonates or other osteoporosis medications prior to biopsy.
All patients had biallelic AIRE mutations and 7–10 disease manifestations. P1 and P2 had both hypoparathyroidism and adrenal insufficiency, while P3 did not have hypoparathyroidism and needed hydrocortisone substitution only in the case of stress for early adrenal insufficiency. P1 and P3 had hypergonadotropic hypogonadism treated with contraceptive pills containing ethinylestradiol and with testosterone, respectively. P3 had stable renal tubular acidosis treated adequately with sodium substitution and sodium bicarbonate. Exocrine pancreas insufficiency was treated with enzyme substitution at meals in P3. Due to intestinal dysfunction, P1 had used lactobacillus supplement for years and P2 avoided dairy products.
P1 and P2 had short stature, whereas P3 was under-weighted. P1 and P2 had ionized calcium level slightly below normal range, but within the target range for patients with hypoparathyroidism. Whole body BMD T-scores were + 1.2, − 2.8, and − 3.5 for P1, P2, and P3, respectively.
Bone Histomorphometry
In bone biopsies, bone volume (BV/TV) was in the normal range for all patients (Table 2, Fig. 1). Nevertheless, it was in the lower range for P1 and P3, which was mainly due to reduced trabecular thickness, but partly reversed by an increase in trabecular number.
Typical microarchitectures of iliac crest specimens under light microscopy (1.1–1.2; 2.1–2.2; 3.1–3.2) and fluorescence microscopy (1.3; 2.3; 3.3) are exemplified from patients 1, 2 and 3 with APS1. The blue arrows indicated the peri-trabecular fibrosis and the double tetracycline labels seen in cortical bone were shown by yellow arrows in patient 1. The magnified images (highlighted by red rectangle) demonstrated the normal double labeling in cancellous bone of patient 2 and patient 3. Masson Goldner trichrome stain
In P1, the amount of osteoid was low; active osteoblasts and tetracycline double labels were seen only on cortical bone. Bone resorption was increased (Table 2), and there was peritrabecular fibrosis of bone marrow (Fig. 1). Dynamic parameters in cancellous bone could be measured in P2 and P3. In P2, dynamic parameters were within the normal range. In P3, no osteoclast was seen, and increased bone turnover rate (BFR/BV + 4.53 SD) associated with an increase in osteoid tissue was observed (Fig. 1). Double labels were seen in P3 ruling out the presence of pronounced osteomalacia. However, focal mineralization defects were identified as the presence of “osteoid islands” surrounded by mineralized bone (online resource).
BMDD and OLS
The three samples showed different bone matrix mineralization characteristics. Figure 2A shows the trabecular BMDD curves obtained for the three patients, as well as the adult reference curve for comparison [10]; online resource shows the resulting BMDD parameters for trabecular and cortical compartment. P1 showed a slight hypermineralization for the trabecular and cortical compartment as well as a decrease in the width of the BMDD (CaMeanTrab + 1.75 SD, CaWidthTrab − 2.04 SD, CaMeanCort + 1.59 SD, CaWidthCort − 1.53 SD) denoting a more homogenous mineralization compared to reference. In contrast, the trabecular BMDDs from P2 and P3 showed a considerable broadening of the curve. In P3, it was accompanied with a pronounced hypomineralization reflected in a large decrease in CaMean and CaPeak and a large increase in CaLow, respectively. The findings of qBEI were also reflected in the results from histomorphometry. The amount of osteoid volume and osteoid surface (Table 2) were consistent with the mineralization results, as a high turnover rate pointed towards a reduced degree of mineralization. Furthermore, similar with the histology pronounced focal mineralization defects could be spotted in P2 and P3 (online resource).
A shows the BMDD curves for trabecular bone of patients 1, 2, and 3, respectively. The black dashed line corresponds to the adult reference BMDD curve, the grey band depicts the corresponding standard deviation[10]. B show the results of the OLS analysis for OLS-density and OLS-area for cortical and trabecular compartments. Data are compared against results from 2 healthy women aged 36 and 42 years[12]
The OLS-density and OLS-area were similar to reference samples obtained from two healthy adults in both cortical and trabecular bone (Fig. 2B).
Discussion
Our earlier study showed that recurrent fractures and spinal compression fractures were more prevalent in patients with APS1 than in their age- and gender-matched controls, although osteoporosis was rare [4]. This led us to investigate the bone histomorphometry and mineral properties in bone biopsies from three adults with APS1. Our findings indicated reduced trabecular thickness in all patients. Furthermore, the amount of osteoid was increased in P2 and P3, which together with hypomineralization measured by qBEI suggests a mineralization defect.
The reduced trabecular thickness was partly reversed by an increase in trabecular number. Therefore, bone volume was in the normal range for all patients. Increased trabecular number was not explained by any artifacts from the sampling procedure. Based on this cross-sectional study, we cannot define if the altered microstructure was formed by the modeling of growing skeleton or by remodeling during adulthood. The patients had multiple disease manifestations that could contribute to bone tissue abnormalities during their lifetime. Hypoparathyroidism is the most prevalent endocrinopathy in APS1 [13]. Deficiency of parathyroid hormone and low serum calcium levels lead to low bone turnover that has been associated with structural skeletal alterations, including higher cancellous bone volume and trabecular thickness [14, 15]. Cancellous BMDD is shifted to higher mineralization densities in patients with hypoparathyroidism [16]. In our study, P1 with longer duration of hypoparathyroidism (33 years) showed higher cancellous BMDD than P2 (5 years), but none showed higher cancellous bone volume or an increase in trabecular thickness. Lack of double strand labeling in cancellous bone in P1 resembles the significantly reduced cancellous bone formation in patients with hypoparathyroidism, whereas the increased eroded surface was in contrast to decreased resorptive activity reported previously [14].
Adrenal insufficiency and long-term glucocorticoid replacement may have had opposing effects on bone metabolism in comparison to hypoparathyroidism in P1 and P2. Their current hydrocortisone equivalent doses are near the recommended dose corresponding endogenous production of glucocorticoids [17]. Glucocorticoids act on osteoblasts, osteocytes, and osteoclasts as well as their precursors. Reduced bone formation at trabecular bone sites and increased endocortical resorption are the most consistent pathological findings of glucocorticoid excess [18]. Although meta-analysis showed that patients receiving glucocorticoid replacement due to adrenal insufficiency have a higher fracture risk [19], only modest data exist on the effects of glucocorticoid replacement on bone. Thus far no study has explored bone properties in the patients with adrenal insufficiency by bone histomorphometry.
In addition to lack of glucocorticoids and mineralocorticoids, adrenal insufficiency may lead to lack of adrenal androgens which act as precursors for peripheral conversion to more potent androgens and estrogens. P1 had used contraceptive pills for ovarian insufficiency and no DHEA supplementation. DHEA supplementation has been associated with higher areal BMD in female patients with adrenal insufficiency [20]. Placebo controlled trial with DHEA reversed ongoing loss of bone mineral density [21]. Androgens are important for the periosteal bone growth, whereas estrogens are crucial for the attainment and maintenance of trabecular bone mass in both females and males by affecting the differentiation and function of osteoblasts as well as osteoclasts [22,23,24]. Both our patients with hypogonadism showed decreased trabecular thickness and in female P1 increased eroded surface was evident. The early onset of hypogonadism may have decreased the accrual of peak bone mass in both patients. In male patients with hypogonadism, bone histomorphometry shows marked alterations in trabecular microarchitecture with decreased trabecular connectivity [25]. No study has explored the bone histomorphometry in patients with premature ovarian insufficiency.
In addition to endocrinopathies, altered kidney function and malabsorption may affect the mineral homeostasis. P3 had stable renal tubular acidosis since childhood. A previous study on bone histomorphometry in adult patients with longstanding renal tubular acidosis suggested that chronic metabolic acidosis may result in suppression of bone formation and resorption. BMD and bone formation rates were found to be lower, while osteoid volume and surface were increased [26]. Because of the multiple contributing factors, we were not able to determine whether renal tubular acidosis, hypogonadism, or exocrine pancreas insufficiency had had most impact on bone parameters in P3. All three patients had either exocrine pancreas insufficiency or intestinal dysfunction. Although all patients had adequate 25-hydroxy vitamin D levels, their intestinal absorption capacity of necessary nutrients may have been compromised during attainment of peak bone mass and afterwards.
The small number of participants and the lack of control subjects are the major limitations of the study. All three patients present with the severe phenotype of APS1, and the results may not apply to patients with milder disease severity.
In conclusion, we demonstrate variable and significant bone pathology on the tissue level in three patients with severe APS1 and osteoporosis. Altered mineralization and bone metabolism reflected some features of hormonal defects but the large number of endocrinopathies, often with opposing effects make it difficult to identify the main cause of observed pathologies and to identify potential primary skeletal effects. Osteoporosis treatment in patients with APS1 should consider the possibility of a mineralization defect.
Data Availability
Restrictions apply to the availability of data generated or analyzed during this study to preserve patient confidentiality. The corresponding author will on request detail the restrictions and any conditions under which access to some data may be provided.
References
Anderson MS, Venanzi ES, Klein L et al (2002) Projection of an immunological self shadow within the thymus by the aire protein. Science 298:1395–1401. https://doi.org/10.1126/science.1075958
Kekäläinen E, Tuovinen H, Joensuu J et al (1950) (2007) A defect of regulatory T cells in patients with autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy. J Immunol Baltim Md 178:1208–1215
Husebye ES, Anderson MS, Kämpe O (2018) Autoimmune polyendocrine syndromes. N Engl J Med 378:1132–1141. https://doi.org/10.1056/NEJMra1713301
Laakso S, Borchers J, Toiviainen-Salo S et al (2020) Severe phenotype of APECED (APS1) increases risk for structural bone alterations. Front Endocrinol 11:109. https://doi.org/10.3389/fendo.2020.00109
Rauch F, Schoenau E (2005) Peripheral quantitative computed tomography of the distal radius in young subjects—new reference data and interpretation of results. J Musculoskelet Neuronal Interact 5:119–126
Rauch F, Schoenau E (2008) Peripheral quantitative computed tomography of the proximal radius in young subjects–new reference data and interpretation of results. J Musculoskelet Neuronal Interact 8:217–226
Raum K (2008) Microelastic imaging of bone. IEEE Trans Ultrason Ferroelectr Freq Control 55:1417–1431. https://doi.org/10.1109/TUFFC.2008.817
Dempster DW, Compston JE, Drezner MK et al (2013) Standardized nomenclature, symbols, and units for bone histomorphometry: A 2012 update of the report of the ASBMR Histomorphometry Nomenclature Committee. J Bone Miner Res 28:2–17. https://doi.org/10.1002/jbmr.1805
Rehman MT, Hoyland JA, Denton J, Freemont AJ (1994) Age related histomorphometric changes in bone in normal British men and women. J Clin Pathol 47:529–534. https://doi.org/10.1136/jcp.47.6.529
Hartmann MA, Blouin S, Misof BM et al (2021) Quantitative backscattered electron imaging of bone using a thermionic or a field emission electron source. Calcif Tissue Int 109:190–202. https://doi.org/10.1007/s00223-021-00832-5
Mähr M, Blouin S, Behanova M et al (2021) Increased osteocyte lacunae density in the hypermineralized bone matrix of children with osteogenesis imperfecta type I. Int J Mol Sci 22:4508. https://doi.org/10.3390/ijms22094508
Hadzimuratovic B, Haschka J, Hartmann MA et al (2021) Impact of tenofovir disoproxil-induced Fanconi syndrome on bone material quality: a case report. JBMR Plus. https://doi.org/10.1002/jbm4.10506
Perheentupa J (2006) Autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy. J Clin Endocrinol Metab 91:2843–2850
Langdahl BL, Mortensen L, Vesterby A et al (1996) Bone histomorphometry in hypoparathyroid patients treated with vitamin D. Bone 18:103–108
Rubin MR, Dempster DW, Kohler T et al (2010) Three dimensional cancellous bone structure in hypoparathyroidism. Bone 46:190–195. https://doi.org/10.1016/j.bone.2009.09.020
Misof BM, Roschger P, Dempster DW et al (2016) PTH(1–84) administration in hypoparathyroidism transiently reduces bone matrix mineralization. J Bone Miner Res 31:180–189. https://doi.org/10.1002/jbmr.2588
Seibel MJ, Cooper MS, Zhou H (2013) Glucocorticoid-induced osteoporosis: mechanisms, management, and future perspectives. Lancet Diabetes Endocrinol 1:59–70. https://doi.org/10.1016/S2213-8587(13)70045-7
Hardy RS, Zhou H, Seibel MJ, Cooper MS (2018) Glucocorticoids and bone: consequences of endogenous and exogenous excess and replacement therapy. Endocr Rev 39:519–548. https://doi.org/10.1210/er.2018-0009717
Li L, Bensing S, Falhammar H (2021) Rate of fracture in patients with glucocorticoid replacement therapy: a systematic review and meta-analysis. Endocrine 74:29–37. https://doi.org/10.1007/s12020-021-02723-z
Koetz KR, Ventz M, Diederich S, Quinkler M (2012) Bone mineral density is not significantly reduced in adult patients on low-dose glucocorticoid replacement therapy. J Clin Endocrinol Metab 97:85–92. https://doi.org/10.1210/jc.2011-2036
Gurnell EM, Hunt PJ, Curran SE et al (2008) Long-term DHEA replacement in primary adrenal insufficiency: a randomized, controlled trial. J Clin Endocrinol Metab 93:400–409
Noirrit-Esclassan E, Valera M-C, Tremollieres F et al (2021) Critical role of estrogens on bone homeostasis in both male and female: From physiology to medical implications. Int J Mol Sci 22:1568. https://doi.org/10.3390/ijms22041568
Mills EG, Yang L, Nielsen MF et al (2021) The relationship between bone and reproductive hormones beyond estrogens and androgens. Endocr Rev 42:691–719. https://doi.org/10.1210/endrev/bnab015
Russell N, Grossmann M (2019) Mechanisms in endocrinology: estradiol as a male hormone. Eur J Endocrinol 181:R23–R43. https://doi.org/10.1530/EJE-18-1000
Legrand E, Audran M, Guggenbuhl P et al (2007) Trabecular bone microarchitecture is related to the number of risk factors and etiology in osteoporotic men. Microsc Res Tech 70:952–959. https://doi.org/10.1002/jemt.20501
Domrongkitchaiporn S, Pongsakul C, Stitchantrakul W et al (2001) Bone mineral density and histology in distal renal tubular acidosis. Kidney Int 59:1086–1093. https://doi.org/10.1046/j.1523-1755.2001.0590031086.x
Acknowledgements
We thank the patients for their participation. We acknowledge the work of research nurse Nea Boman. We thank Sonja Lueger and Phaedra Messmer for careful sample preparation and measurements. SL acknowledges financial support from Helsinki University Hospital, Finnish Foundation for Pediatric Research, and Finnish Medical Foundation. OM acknowledges financial support from Sigrid Jusélius Foundation, Novo Nordisk Foundation, Academy of Finland, Foundation for Pediatric Research, and Folkhälsan Research Foundation. SB, PK, and MH acknowledge financial support from the Austrian workers compensation board AUVA and the Austrian Social Health Insurance Fund OEGK.
Funding
Open Access funding provided by University of Helsinki including Helsinki University Central Hospital. Terveyden Tutkimuksen Toimikunta, Austrian social health insurance fund OEGK, Helsinki University Hospital, Lastentautien Tutkimussäätiö,Suomen Lääketieteen Säätiö, Folkhälsanin Tutkimussäätiö, Novo Nordisk Fonden, Austrian workers compensation board AUVA, Sigrid Juséliuksen Säätiö
Author information
Authors and Affiliations
Contributions
Authors SL and OM designed the study. SL prepared the first draft of the paper, and she is guarantor. Authors SL, TX, SB, PK, and VVV contributed to the experimental work. Authors SL, SB, and MH were responsible for statistical analysis of the data. All authors revised the paper critically for intellectual content and approved the final version. All authors agree to be accountable for the work and to ensure that any questions relating to the accuracy and integrity of the paper are investigated and properly resolved.
Corresponding author
Ethics declarations
Competing interests
Saila Laakso, Tong Xiaoyu, Stéphane Blouin, Petra Keplinger, Ville-Valtteri Välimäki, Heikki Kröger, Outi Mäkitie, Markus A. Hartmann, the authors declare no competing interests.
Human and Animal Rights and Informed Consent
All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration. Informed consent was obtained from all patients for being included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Laakso, S., Xiaoyu, T., Blouin, S. et al. Bone Tissue Evaluation Indicates Abnormal Mineralization in Patients with Autoimmune Polyendocrine Syndrome Type I: Report on Three Cases. Calcif Tissue Int 112, 675–682 (2023). https://doi.org/10.1007/s00223-023-01077-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00223-023-01077-0