Abstract
Macrophages are crucial for the development of atherosclerotic plaques. Classically activated macrophages contribute to plaque growth and destabilization, while alternatively activated macrophages increase plaque stability. Here, we assessed the influence of ezetimibe on the activation of monocyte-derived macrophages isolated from patients with hypercholesterolemia (total cholesterol 263.4 ± 12.5 mg/dl, low-density lipoprotein cholesterol 179.7 ± 11.3 mg/dl, triglycerides 123.9 ± 11.4 mg/dl). Cells were stimulated with 1 μg/ml lipopolysaccharide (LPS) or 1 μg/ml LPS plus 22 ng/ml ezetimibe. Control cells were left unstimulated. The expression of classical activation markers (interleukin-1β (IL-1β), nitric oxide (NO), and inducible nitric oxide synthase (iNOS)) and alternative activation markers (mannose receptor (MR) and arginase-1 (Arg1)) was determined after 48 h. The employed analytical methods included enzyme-linked immunosorbent assay, Griess reaction, real-time polymerase chain reaction, and Western blotting. LPS increased the secretion of IL-1β and NO and the expression of iNOS mRNA, iNOS protein, and Arg1 protein. It did not affect the expression of MR or Arg1 mRNA. In comparison to LPS stimulation, co-stimulation with ezetimibe decreased the secretion of IL-1β and the expression of iNOS mRNA and protein, while it increased MR mRNA and protein expression. Co-stimulation with ezetimibe did not change the secretion of NO or the expression of Arg1. The results suggest that ezetimibe in inflammatory in vitro conditions contributes to the suppression of classical and promotion of the alternative macrophage activation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Monocytes, along with granulocytes and natural killer cells, belong to the cellular elements of the innate, nonspecific immune system. Monocytes also link innate and adaptive immunity through antigen presentation and cytokine production (Auffray et al. 2009). After infiltration of surrounding tissues, monocytes differentiate into macrophages whose primary function is to uphold homeostasis by scavenging senescent cells and repairing injured areas undergoing inflammatory processes (Gordon and Taylor 2005). However, macrophages do not constitute a homogenous population. Depending on the stimulus, these cells undergo different activation and consequently present distinct properties. According to the most recent divisions, there are two major types of activated macrophages: the classically activated macrophages (M1) and the alternatively activated macrophages (M2). In vitro, there are in total five subpopulations: M1a, M1b, M2a, M2b, and M2c. However, there is no certainty regarding whether they constitute separate entities or if they represent subsequent stages of the development continuum. The M1a and M2a macrophages have also been identified in vivo. The existence of the other subpopulations in vivo is presently of minor probability (Rees 2010).
Macrophages are key cells involved in the process of atherogenesis (Auffray et al. 2009). As well as the differences in the roles of the given subpopulations, they also exert contrasting effects regarding the development and stability of the atherosclerotic plaque (Auffray et al. 2009; Wilson 2010). The M1 subpopulation effectively combats pathogens. However, the M1 macrophages also promote atherosclerotic plaque growth due to pro-inflammatory properties, damage of tissues, and absorption of low-density lipoproteins (LDLs). The M1 cells contribute to increased plaque vulnerability and susceptibility to cracking, which raises the risk of thrombotic changes, and hence this subpopulation is often called “atherogenic.” In contrast to the M1 subpopulation, the M2 macrophages produce anti-inflammatory cytokines, inhibit inflammatory reactions, and extinguish inflammatory states. The M2 macrophages promote tissue repair processes and stabilize atherosclerotic plaques, even leading to their regression, and hence the M2 macrophages are often referred to as being “atheroprotective” (Wilson 2010). Both M1 and M2 macrophages produce characteristic markers that are related to their functions. Among other markers, the M1 macrophages produce significant amounts of nitric oxide (NO) due to elevated expression of inducible nitric oxide synthase (iNOS), which is necessary for effective antimicrobial activity. They also secrete large quantities of interleukin-1β (IL-1β), a major pro-inflammatory cytokine (Gordon and Taylor 2005). On the other hand, the M2 macrophage subpopulation is characterized by increased activity of arginase-1 (Arg1), which is crucial during the final stages of inflammatory-state quenching. These cells also demonstrate a higher expression of mannose receptors (MRs), resulting in changes in phagocytosis and membrane transport (Varin and Gordon 2009).
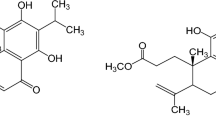
Considering the properties of the macrophage subpopulations, investigations of the immunomodulative properties of various pharmacologically active substances are underway. From this point of view, the drugs used to treat hypercholesterolemia are of special interest. One of the newest therapeutic agents used to treat this disease is ezetimibe, a potent cholesterol and phytosterol absorption inhibitor that acts in the small intestine lumen. Ezetimibe blocks the Nieman-Pick C1-Like 1 (NPC1L1) transporter protein in the brush border of enterocytes (Suchy et al. 2011). At the daily oral dose of 10 mg, it reduces the absorption of cholesterol by about 54 % and decreases the plasma level of LDL cholesterol by about 15–20 %. Beside the influence on lipid parameters, ezetimibe also exerts additional effects such as reducing the level of C-reactive protein (CRP), which is a global inflammatory marker (Suchy et al. 2011). Ezetimibe also directly affects properties of monocytes and macrophages. The drug modifies the functioning of monocyte lipid rafts and reduces the absorption of oxidized LDLs in macrophages. In this way, it reduces the formation of foam cells and the gathering of lipids in the atherosclerotic plaques. Ezetimibe in macrophages undergoes endocytosis and, after being absorbed into these cells, is also able to modify the expression of several genes (Suchy et al. 2011). However, whether the drug influences macrophage activation pathways has not yet been investigated.
The aim of this study was to assess the in vitro impact of ezetimibe on the activation of monocyte-derived macrophages isolated from patients with hypercholesterolemia and thereby its potential stabilizing effect on the atherosclerotic plaque.
Methods
Materials
Ezetimibe, (3R,4S)-1-(4-fluorophenyl)-3-[(3S)-3-(4-fluorophenyl)-3-hydroxypropyl]-4-(4-hydroxyphenyl)-azetidin-2-one, was purchased from LKT Laboratories, Inc. (USA). Lipopolysaccharide (LPS, Escherichia coli serotype 0111:B4), polysaccharose Histopaque 1077, dimethyl sulfoxide (DMSO) Hybri-Max, trypan blue 0.4 % solution, TRIzol/TRI reagent, chloroform, isopropanol, protease inhibitor cocktail, Bradford reagent, Laemmli sample buffer concentrate, 40 % bis-acrylamide, tetramethylethylenediamine (TEMED), Trizma base (Tris), sodium dodecyl sulfate (SDS), ammonium persulfate (APS), sodium chloride, hydrochloric acid, Tween 20, glycine, bovine serum albumin (BSA), and primary rabbit anti-human antibody anti-Arg1 (307-322) were from Sigma-Aldrich Co. (USA). RPMI 1640 (without phenol red, with glutamine), 1 M 4-(2-hydroxyethyl)-1-piperazineethanesulfonic acid (HEPES) buffer, Hank's balanced salt solution (HBSS; without calcium, magnesium, and phenol red), and Dulbecco’s phosphate-buffered saline (PBS) were bought from PAA Laboratories GmbH (Austria). Glutamine was purchased from Gibco-BRL (USA). Low-endotoxin fetal bovine serum (FBS), antibiotic-antimycotic anti-anti solution, and glycogen were from Invitrogen (USA). Absolute ethanol and methanol were bought from Merck Millipore (Germany). Magnetic beads (pan-T (anti-CD2) and pan-B (anti-CD19)) were purchased from Dynal Biotech ASA (Norway). Monoclonal mouse anti-human antibody anti-CD14 (CD14-FITC) was bought from Thermo Fisher Scientific Inc. (USA). Nitrate/Nitrite Colorimetric Assay Kit was purchased from Cayman Chemical Company (USA). The enzyme-linked immunosorbent assay (ELISA) kit for human IL-1β was from R&D Systems, Inc. (USA). Primers (Table 1) for the real-time polymerase chain reaction (RT-PCR) were obtained from Genomed S.A. (Poland). Affinity Script QPCR cDNA Synthesis Kit and PCR Brilliant II SYBR Green QPCR Master Mix with Low ROX were purchased from Agilent Technologies (USA). ColorPlus Prestained Protein Markers (Broad Range (97–175 kDa) P7709V and Broad Range (10–230 kDa) P7711S) were from New England Biolabs Inc. (USA). Radioimmunoprecipitation assay (RIPA) lysis buffer, SuperSignal Molecular Weight Protein Ladder, Western blot polyvinylidene fluoride (PVDF) transfer membrane, primary rabbit anti-human antibody anti-β-actin (PA1-21167), and Restore Plus Western Blot stripping buffer were from Thermo Fisher Scientific Inc. (USA). Primary rabbit anti-human antibodies anti-MR (ab64693) and anti-iNOS (ab15323) were from Abcam (USA). Amersham ECL Western Blotting Analysis System was purchased from GE Healthcare (UK).
Isolation of human monocytes
The study was accepted by the Bioethical Committee of the Medical University of Silesia in Katowice, Poland. The investigation conformed to the principles of the Declaration of Helsinki. Human whole-blood samples were taken from 20 yet untreated patients with primary hypercholesterolemia (total cholesterol 263.4 ± 12.5 mg/dl, LDL cholesterol 179.7 ± 11.3 mg/dl, triglycerides 123.9 ± 11.4 mg/dl) registered at the Independent Public Central Clinical Hospital of the Medical University of Silesia in Katowice, Poland (Table 2). Later therapy of the patients was not altered as the samples were taken only once. Peripheral blood monocytic cells (PBMCs) were obtained by density-gradient centrifugation using polysaccharose (Okopień et al. 2005). Monocytes were isolated from the mixed population of PBMCs using the negative immunomagnetic method (Flø et al. 1991), which excludes T, B, and NK cells with magnetic beads coated with the relevant antibodies. The mean (±standard deviation, SD) purity of the obtained monocytes determined by fluorescent antibody labeling with anti-CD14 was 92.02 ± 2.37 %. Next, the monocytes obtained from each of the patients were diluted in HBSS containing 2 % (v/v) FBS to obtain a cell density of 1 × 106/ml. Three 1-ml suspension portions were placed in a 24-well culture dish (Nunclon Delta Surface, Nunc, Denmark) and incubated for 3 h at 37 °C in air containing 5.2 % (v/v) carbon dioxide and 95 % (v/v) relative humidity in order to allow the monocytes to adhere. After that time, the cells were gently washed to remove the remaining nonadherent cells. Three wells containing cells from one patient constituted one series of cultures. The cells in each of the wells underwent different stimulations.
Cell cultures
Monocytes were cultured in RPMI 1640 supplemented with 10 % (v/v) FBS, 25 mM HEPES, 2 mM glutamine, 100 U/ml penicillin, 100 μg/ml streptomycin, and 10 μg/ml amphotericin B as in the above conditions. The cells were adapted to the conditions for 24 h, after which the medium was replaced with either (1) regular medium, (2) medium supplemented with 1 μg/ml (submaximal dose) LPS, or (3) medium supplemented with 1 μg/ml LPS plus 22 ng/ml ezetimibe. The concentration of ezetimibe was equivalent to that measured in the serum of patients chronically taking the drug at the oral daily dose of 10 mg (Suchy et al. 2013). Ezetimibe as a lipophilic substance was dissolved in DMSO to facilitate its introduction into the aqueous culture medium (Cheng et al. 2009). The final concentration of DMSO in the culture media (including those not supplemented with ezetimibe solution) was equal to 0.05 % (v/v). The cells were incubated for 48 h, after which cell culture supernates were collected and the cells were harvested by vigorous pipetting with ice-cold PBS. The cell culture supernates were centrifuged and immediately frozen at −80 °C. They were subsequently used for the determination of NO and IL-1β concentrations. The harvested cells from each well were divided into two portions: one was subjected to Western blotting analysis and the other to RT-PCR analysis in order to determine the expression of iNOS, Arg1, and MR.
Assessment of cell viability
The viability of the cells was examined after the isolation of monocytes from human whole-blood samples (to evaluate their suitability for culture) and after harvesting the macrophages (to determine whether the results were affected by disturbances during incubation). The viability was assessed by staining the cells with trypan blue solution. The suspended cells were incubated for 5 min in the above conditions with 0.2 % (v/v) dye diluted in the cell culture medium. After that time, the percentage of dead, blue-stained cells was counted using a Bürker's chamber.
Assessment of NO production
The concentration of NO produced by the cells after different stimulations was calculated as the sum of nitrites and nitrates, which are its stable derivatives. The assessments were carried out according to the instructions of the kit manufacturer. Briefly, initially all the cell culture supernates were diluted twofold. Next, the nitrates present in 80-μl samples were reduced into nitrites with the use of nitrate reductase. The amount of nitrites in the samples of culture media was determined through reaction with an equal volume of Griess reagent. After 10 min of incubation, the absorbances at 540 nm were measured in a microplate reader (xMark Microplate Spectrophotometer, Bio-Rad Laboratories, Inc., USA). Fresh culture medium was used as a blank in all the measurements. The amount of nitrites in the samples was calculated using the calibration curve based on serial dilutions of sodium nitrite standard.
Assessment of IL-1β secretion
The concentration of IL-1β produced by the cells after different stimulations was measured using a commercially available ELISA kit according to the manufacturer's instructions. Briefly, 200-μl samples of cell culture supernates were incubated in the anti-IL-1β-antibody-covered wells of a 96-well plate. After washing the wells, equal volumes of antibody conjugate were added. Subsequently, the wells were washed again and substrate solutions were added. After stopping the reaction, the absorbances at 450 nm (with correction at 540 nm) were measured in a microplate reader (xMark Microplate Spectrophotometer, Bio-Rad Laboratories, Inc., USA). The amount of IL-1β in the samples was calculated using the calibration curve based on serial dilutions of IL-1β standard.
Assessment of iNOS, Arg1, and MR mRNA expression
The expression of marker genes was analyzed using the RT-PCR method. Total RNA was extracted with TRIzol reagent according to the manufacturer's instructions based on a previously developed method (Chomczyński and Sacchi 1987). The RNA extracts were supplemented with 2 μg of glycogen. Reverse transcription was performed in a MJ Mini Personal Thermal Cycler (Bio-Rad Laboratories, Inc., USA) with 0.5 μg total RNA using a cDNA synthesis kit according to the manufacturer's instructions. RT-PCR was performed using SYBR Green QPCR Master Mix with Low ROX with a RT-PCR LightCycler 480 II (Roche Applied Science, USA). PCR primers for iNOS (E.C. 1.14.13.39), Arg1 (E.C. 3.5.3.1), and MR used in this study are listed in Table 1. Glyceraldehyde 3-phosphate dehydrogenase (GAPDH, E.C. 1.2.1.12) was used as a reference gene. The relative expression values were calculated using the comparative threshold cycle (ΔΔC t) method.
Assessment of iNOS, Arg1, and MR protein expression
The expression of marker proteins was analyzed using the Western blotting method. Whole-cell extracts were obtained by lysing the cells with RIPA buffer with the addition of protease inhibitors (104 mM AEBSF, 80 μM aprotinin, 4 mM bestatin, 1.4 mM E-64, 2 mM leupeptin, 1.5 mM pepstatin A in the stock solution). The concentration of proteins was assessed using Bradford's reagent (Bradford 1976) by reading the absorbance at 595 nm in a microplate reader (xMark Microplate Spectrophotometer, Bio-Rad Laboratories, Inc., USA) and comparing the values with a calibration curve based on serial dilutions of BSA. Equal amounts (25 μg) of total proteins were run on SDS-PAGE (10 % separating gel) in a Mighty Small II electrophoretic chamber (Hoefer, USA) and transferred to a PVDF membrane in a TE22 Mighty Small Transphor Unit (Hoefer, USA). The membrane was blocked for 1 h at room temperature in 1 % (v/v) BSA solution in Tris-buffered saline containing 0.08 % (v/v) Tween 20 (TTBS). After blocking, the membrane was incubated with subsequent specific primary antibodies (dilution 1:1,000) for 1 h at room temperature and further incubated for 1 h with a secondary antibody (dilution 1:10,000) conjugated with horseradish peroxidase. The addition of substrate solution resulted in the formation of a chemiluminescent product. The chemiluminescence was read in a ChemiDoc-It 410 camera (UVP, USA) and analyzed densitometrically. β-Actin was used as a reference protein. Independent expression analyses of respective proteins (iNOS, Arg1, MR, and β-actin) were preceded by membrane stripping to remove the adsorbed primary antibodies.
Statistical analysis
The statistical analysis was performed with GraphPad Prism 6 for Windows (GraphPad Software Inc., USA). The normality of continuous variable distributions was checked with the Shapiro-Wilk's test. The results are presented as means ± SD. Significant differences between experimental groups were determined using the one-way ANOVA analysis with Tukey's post hoc test. The homogeneity of variance, which is an assumption of ANOVA, was checked with Brown-Forsythe’s and Bartlett’s tests. The differences were considered significant at the level of p < 0.05. The levels of significance are marked as follows: *p < 0.05, **p < 0.01, ***p < 0.001, and ****p < 0.0001. The sample sizes (number of replicates, n) are given with the relevant analysis results. The n values lower than 20 (approved by the Bioethical Committee) resulted from independent external causes affecting the performance of the experiment, resulting in the rejection of the whole series.
Results
The influence of culture preparation procedures and different types of stimulation on the viability of the cells
The viability of isolated monocytes was assessed each time before beginning a series of cultures. The mean viability of the cells obtained from all the participants of the experiment (n = 20) was 96.42 ± 3.35 %.
The viability of cultured cells, including the control cultures, the cultures stimulated with LPS (1 μg/ml), and stimulated with LPS (1 μg/ml) plus ezetimibe (22 ng/ml) (n = 3 for each), was tested at the beginning, during, and at the end of the study. The mean viabilities of macrophages from the respective types of cultures were 95.08 ± 5.09, 93.16 ± 4.51, and 94.86 ± 4.04. The given values were not significantly different (p = 0.9784), indicating that neither LPS nor ezetimibe at the concentrations used affected the cell viability. The results of viability testing also indicated that this parameter did not have any influence on the outcome of the experiments.
LPS promotes the classical activation pathway of monocyte-derived macrophages isolated from hypercholesterolemic patients
The stimulation of macrophages with LPS significantly increased expression of classical activation markers. LPS treatment raised the total amount of nitrates and nitrites in the cell culture supernates by 55 % (Fig. 1). Additionally, we observed an 18 % elevation in IL-1β concentration (Fig. 2). The increase in NO production was accompanied by the upregulation of its main producer, iNOS. The expression of the enzyme was increased by more than twofold, both at the mRNA and protein levels. In contrast, the levels of alternative macrophage activation markers under the influence of LPS remained unaffected with the exception of the expression of Arg1 protein, which was significantly elevated. Concomitantly, the expression of Arg1 mRNA was higher in comparison to the control cells but the difference was not significant. The expression of MR was not altered significantly. Both mRNA and protein levels of MR were about 15 % lower (Figs. 3, 4, and 5). These observations suggest that LPS promotes the classical activation of macrophages obtained from hypercholesterolemic patients, which may resemble the state occurring in growing atherosclerotic plaques.
The influence of ezetimibe and/or LPS on the concentration of NO derivatives. The cells were treated with LPS (1 μg/ml) or LPS (1 μg/ml) plus ezetimibe (22 ng/ml) or were left untreated (control), for 48 h. The total concentration of nitrates and nitrites produced by the cells was measured by the Griess reaction. Each value represents mean ± SD. The sample size (n) represents the number of replicates measured for each of the markers in each group in the given experiment. The levels of significance are marked as follows: *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001
The influence of ezetimibe and/or LPS on the concentration of IL-1β. The cells were treated with LPS (1 μg/ml) or LPS (1 μg/ml) plus ezetimibe (22 ng/ml) or were left untreated (control), for 48 h. The concentration of secreted IL-1β was assessed by ELISA. Each value represents mean ± SD. The sample size (n) represents the number of replicates measured for each of the markers in each group. The levels of significance are marked as follows: *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001. IL-1β interleukin-1β
The influence of ezetimibe and/or LPS on the mRNA expression of macrophage activation markers. The cells were treated with LPS (1 μg/ml) or LPS (1 μg/ml) and ezetimibe (22 ng/ml) or were left untreated (control), for 48 h. The mRNA levels of iNOS, Arg1, and MR were determined by RT-PCR and analyzed by the comparative threshold cycle (ΔΔC t) method. GAPDH was used as a housekeeping gene. Each value represents mean ± SD. The sample size (n) represents the number of replicates measured for each of the markers in each group in the given experiment. The levels of significance are marked as follows: *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001. GAPDH glyceraldehyde 3-phosphate dehydrogenase, iNOS inducible nitric oxide synthase, Arg1 arginase-1, MR is mannose receptor
The influence of ezetimibe and/or LPS on the protein expression of macrophage activation markers. The cells were treated with LPS (1 μg/ml) or LPS (1 μg/ml) plus ezetimibe (22 ng/ml) or were left untreated (control), for 48 h. The protein levels of iNOS, Arg1, and MR were determined by Western blotting and analyzed densitometrically. β-Actin was used as a reference protein. Each value represents mean ± SD. The sample size (n) represents the number of replicates measured for each of the markers in each group. The levels of significance are marked as follows: *p < 0.05; **p < 0.01; ***p < 0.001; ****p < 0.0001. iNOS inducible nitric oxide synthase, Arg1 arginase-1, MR mannose receptor
Ezetimibe silences the classical activation pathway of monocyte-derived macrophages isolated from hypercholesterolemic patients
Co-stimulation of cultured macrophages with LPS and ezetimibe decreased the expression of classical activation markers. The most significant change regarded the expression of iNOS mRNA and protein: the relative expression values were decreased by over 50 % in comparison to the expression observed in LPS-stimulated cells. The expression of iNOS mRNA and protein was comparable to that of control macrophages (p = 0.8260 and p = 0.9862, respectively; Figs. 3, 4, and 5). The reduction of iNOS expression was accompanied by changes in NO secretion. The concentration of NO derivatives in the co-stimulated macrophages was 9 % lower than in the LPS-stimulated cells (Fig. 1). However, the observed difference was not significant (p = 0.5844). The amount of generated NO was significantly higher (43 %) than in the control group, but the difference was less significant (p < 0.01 vs. p < 0.001). Simultaneous stimulation of macrophages with LPS and ezetimibe resulted in a 20 % reduction in the secretion of IL-1β compared to the LPS-stimulated cells (Fig. 2). The amount of the cytokine measured in the supernates from the co-stimulated cells was comparable to that of the control cells (6 % lower, p = 0.6117). The above results indicate that the addition of ezetimibe to the culture medium silences the classical pathway of macrophage activation evoked by LPS.
Ezetimibe contributes to the alternative activation pathway of monocyte-derived macrophages isolated from hypercholesterolemic patients
The co-stimulation of macrophages with LPS and ezetimibe increased the expression of alternative activation markers. The addition of LPS to the medium resulted in the elevation of Arg1 mRNA expression; however, it was the addition of ezetimibe that induced a statistically significant change. The expression of Arg1 mRNA in the co-stimulated cells was 42 % higher than in the control group. Also, the expression of Arg1 protein was significantly increased (more than twofold) compared to the control cells. Of note, the expression of Arg1 was only slightly higher than in the LPS-stimulated macrophages. The most evident changes were observed regarding the MR. The expression of MR in the co-stimulated cells compared to the control cells was 63 and 45 % higher at the mRNA and protein levels, respectively. The elevation was even more pronounced when compared to the LPS-stimulated cells: the expression of the MR mRNA was almost twofold higher and the expression of the MR protein was 66 % higher (Figs. 3, 4, and 5). The noticed alterations suggest that ezetimibe at the concentration that can be found in serum after chronic administration promotes the alternative activation of macrophages obtained from hypercholesterolemic patients.
Discussion
Macrophages gathering in the arterial walls are key cells in the pathogenesis of atherosclerotic lesions. Depending on their activation type, macrophages may have opposing impacts on the development and stability of plaques (Łabuzek et al. 2013; McLaren et al. 2011). Atherosclerosis is a major complication in hypercholesterolemia, and thus we decided to isolate monocytes from newly diagnosed hypercholesterolemic patients. During several days of incubation (Lovren et al. 2010; Zhou and Amar 2007) and LPS stimulation (Lovren et al. 2010; Panda et al. 2012), the monocytes were differentiated into macrophages. The use of LPS at a submaximal concentration of 1 μg/ml was intended to imitate the inflammatory state of atherosclerotic lesions, to induce M1 polarization, and to facilitate the determination of the qualitative and quantitative effects of ezetimibe. In this way, the effect of priming the macrophages with the chosen LPS concentration could potentially be decreased or increased by the study drug. We decided not to use common macrophage-differentiating factors such as granulocyte-macrophage colony-stimulating factor (GM-CSF) or macrophage colony-stimulating factor (M-CSF) as they have been reported to induce M1 and M2 polarization, respectively, but do not have a direct influence on inflammatory-state generation (Fleetwood et al. 2009; Van der Plas et al. 2009). We also did not use phorbol-12-myristate-13-acetate (PMA) based on information that ezetimibe impairs the differentiation process evoked by PMA (Muñoz-Pacheco et al. 2012). Furthermore, we did not evaluate the effect of ezetimibe alone as atherosclerosis is an inflammatory disease and—being aware of the model's imperfections—we chose the co-stimulation to resemble the actual conditions in which the drug is therapeutically used.
The markers used to determine the phenotype of macrophages were chosen based on their significance for the process of atherogenesis and/or their credibility. IL-1β is not only a well-accepted M1 macrophage marker but also contributes to M1 macrophage generation. The cytokine also promotes foam-cell formation because it reduces ABCA1/ABCG1 transporter mRNA expression and increases intracellular lipid deposition. It was found to potentiate atherosclerotic changes in mice in vivo (McLaren et al. 2011). iNOS is present in tissues undergoing inflammatory processes, including atherosclerotic lesions, and its expression magnitude correlates with severity of the disease. The in vitro experiments revealed that NO produced by iNOS in activated macrophages causes apoptotic and necrotic cell death (Tripathi 2007). Peroxynitrites originating from NO induce protein nitration and apoptosis of vascular smooth muscle cells (VSMCs), which in turn leads to atherosclerotic plaque instability. Increased NO production in M1 macrophages worsens atherogenic conditions. On the other hand, iNOS expression blockade in hypercholesterolemic mice suppresses atherogenesis development (Feig and Feig 2012). In turn, Arg1 is responsible for promitotic properties of M2 macrophages, i.e., inducing VSMC proliferation, leading to increased atherosclerotic plaque stability. Arg1 competes with iNOS for the common substrate l-arginine (l-Arg). Arg1 metabolizes l-Arg into l-ornithine, which is a precursor of polyamines and proline. Polyamines play a crucial role in cell growth, differentiation, and division, while proline is a key component of collagen. Arg1 expression is typical for the M2 macrophages (Khallou-Laschet et al. 2010). Arg1 is currently regarded as a new therapeutic target in atherosclerosis prevention. In the experiments on animals, it reduced atherosclerotic processes irrespective of the LDL level. In contrast, generation of foam cells was linked with suppression of Arg1 expression (Feig and Feig 2012). MRs are reliable markers of alternative macrophage activation in humans and mice (Martinez-Pomares 2012). It was observed that macrophages expressing MR were localized in regions far from the lipidous necrotic core of atherosclerotic plaque but their presence in the core itself was significantly lower. During in vitro investigations, these macrophages were filled with lipid droplets smaller than macrophages not expressing MR, which demonstrated their decreased ability to scavenge LDL and oxidized LDL and, in turn, their lower probability of developing into foam cells (Chinetti-Gbaguidi et al. 2011).
By modulating macrophage activation, the dynamics of atherosclerosis progression can be altered (Johnson and Newby 2009; Khallou-Laschet et al. 2010). Previous investigations proved that inhibition of the classical activation pathway with CD40 antagonists and induction of the alternative activation with peroxisome proliferator-activated receptor-γ (PPARγ) agonists contributes to a restriction of atherosclerotic processes (Lutgens et al. 2010; Sica and Mantovani 2012). Considering these facts, we set out to assess the changes in the expression of macrophage activation markers in order to determine potential immunomodulative properties of ezetimibe, which is used in hypercholesterolemia treatment, in terms of the influence on atherosclerosis.
Numerous studies have demonstrated that stimulation of monocytic cells of various origins (human, animal, cell lines) with LPS results in an increase in IL-1β secretion (Netea et al. 2009; Okopień et al. 2005). In experiments on isolated human monocytes/macrophages stimulated with LPS in conditions similar to ours, the cells secreted comparable amounts of cytokine (Okopień et al. 2005). However, the influence of ezetimibe on IL-1β secretion in vitro is not well established. Until now, the drug has been observed to reduce the secretion of IL-1β in vivo (Alvarez-Sala et al. 2008; Undas et al. 2011). Despite obtaining information on the systemic inflammatory state in this way, it is not possible to precisely determine the source of the cytokine. In the experiments in which the patients were administered ezetimibe for 30 and 90 days, followed by isolation of monocytes, the secretion of the cytokine by the cells was reduced by 17 and 18 %, respectively. However, the observed differences were not statistically significant. Only the addition of simvastatin to ezetimibe was found to result in a significant reduction of IL-1β secretion (Krysiak and Okopień 2011). Nevertheless, in these experiments, ezetimibe was not used to stimulate the monocytes after isolation, which might have affected the final outcome. In recent in vitro experiments on isolated monocytes (Krysiak and Okopień 2011; Moutzouri et al. 2012), cells were not stimulated with ezetimibe thus interrupting their constant contact with the drug. The investigations in this study allowed for direct determination of the influence of ezetimibe on the IL-1β level in the inflammatory conditions in vitro and confirmed that the drug reduces its secretion.
As in the case of IL-1β, information on the influence of ezetimibe on the NO-iNOS-Arg1 balance is limited. Mostly, the impact of the drug on the endothelial NOS (eNOS) isoform has been reported. In the animal model, ezetimibe inhibited atherosclerosis progression and the effect was related with marked eNOS mRNA and protein expression upregulation (Nakagami et al. 2009). The data concerning iNOS expression was obtained in experiments on rats suffering from nonalcoholic fatty liver disease. Administering ezetimibe to the animals receiving a cholesterol-rich diet reduced liver iNOS expression (Ibrahim et al. 2010), which is in agreement with our results; however, the authors did not assess the expression of the enzyme, in particular types of cells, and they used whole-tissue homogenates.
Interestingly, in our experiments, ezetimibe did not influence the generated NO concentration in comparison to LPS stimulation. Simultaneously, at the 48-h timepoint, the expression of iNOS was more than twofold lower. This may suggest that LPS was initially predominant in the inflammatory reactions, thus resulting in increased iNOS expression and NO production. Next, during later timepoints of stimulation, ezetimibe restricted iNOS expression, but the derivatives of the generated NO still remained in the cell culture medium. As the concentration of NO produced in the co-stimulated cultures after 48 h was slightly (but not yet significantly) lower than in the LPS-stimulated cultures and the iNOS expression was markedly decreased, we conclude that this was probably the moment from which the activity of the drug overwhelmed the activity of LPS in this aspect. To confirm this, it will be necessary to perform a time-dependent study of iNOS expression and NO production.
As in our experiments, it was previously noted that LPS contributes to elevated Arg1 expression, which is an alternative macrophage activation marker (Rajaiah et al. 2013). It has been established by other authors that LPS is a classical macrophage activator. Despite this fact, they have also observed that, to some extent, LPS contributes to increased Arg1 expression. Furthermore, Arg1 expression in macrophages increases along with increasing LPS concentration (Sonoki et al. 1997). Concomitant iNOS and Arg1 expression upregulation is explained as a protection mechanism of the cells from iNOS overexpression and toxic NO influence. Arg1 is considered to be an enzyme that limits the NO concentration in the cell (Mielczarek-Puta et al. 2008). Interestingly, in our study, ezetimibe did not significantly increase the expression of Arg1 in the co-stimulated cells compared to the LPS stimulation. We consider this effect to be related to the reported lack of ezetimibe influence on the activity of the central pro-inflammatory regulator nuclear factor-κB (NF-κB) in human mononuclear cells, expression of which markedly increases after LPS treatment (Rudofsky et al. 2012). Apart from the pro-inflammatory features of NF-κB, its phosphorylation also contributes to elevated Arg1 expression (Mielczarek-Puta et al. 2008). This may explain the minor influence of ezetimibe on Arg1 expression compared to the LPS effect. However, the action of ezetimibe on NF-κB requires further investigation. Finally, it should be noted that for a significant increase in Arg1 mRNA expression, it was necessary to stimulate the cells with both LPS and ezetimibe, indicating that ezetimibe has an additional effect on the expression of this macrophage alternative activation marker.
The influence of LPS on the MR expression was insignificant (Ferrante et al. 2013; Rajaiah et al. 2013), which we also observed in our experiments. Importantly, elevated MR expression was noted in the alternatively activated macrophages localized in the atherosclerotic plaques (Wilson 2010). As yet, the influence of ezetimibe in vitro or in vivo on the expression of this marker has not been assessed. Other pharmacologically active substances such as eplerenone have demonstrated that induction of alternative macrophage activation is related to increased MR expression. Similarly to ezetimibe, the mineralosteroid receptor antagonist, elevated the expression of MR mRNA and protein in human monocyte-derived macrophages (Łabuzek et al. 2013). Moreover, administering eplerenone to Apo-E-knockout mice resulted in a restriction of the area with early atherosclerotic changes in the arch of the aorta, which was attributed to the change in the macrophage phenotype towards alternative activation (Raz-Pasteur et al. 2012). We observed that ezetimibe strongly increased MR expression in human monocyte-derived monocytes in vitro.
The quantitative and qualitative effects of macrophage stimulation by LPS observed in our study were similar to those noted in recent studies. This study is the first assessment of the influence of ezetimibe on the magnitude of macrophage activation marker expression. We confirmed that the drug presents anti-inflammatory properties, in particular resulting from a direct influence on macrophages. It can be assumed that ezetimibe may exert a local anti-inflammatory effect in growing atherosclerotic plaques, where the macrophages reside. We also presume that in the in vivo conditions—in which the atherosclerotic plaque is affected by constantly circulating fluids—the NO, once produced, would not accumulate locally. As further production of NO would be hampered due to decreased iNOS expression caused by ezetimibe, generation of reactive nitrogen species (RNS), which contribute to the modification of LDLs, would also be restricted. Therefore, the drug is probably able to restrict atherogenic conditions, stating an extra-lipid effect. Additionally, ezetimibe is likely to alter transmembrane trafficking due to reduction of MR expression. The drug may then not only effectively decrease the LDL level but may also exert a direct extra-lipid effect on the cells taking part in atherosclerotic plaque growth and stability modulation. Partial in vivo confirmation of the outcome of our investigations was observed in the experiments on rabbits. Administering ezetimibe to the animals resulted in the reduction of the atherosclerotic change areas in the femoral arteries. The drug also decreased the number of macrophages and the expression of monocyte chemoattractant protein-1 (MCP-1) in the atherosclerotic plaques. Additionally, ezetimibe was observed to reduce lipid-rich areas, preserving the collagen content (Gómez-Garre et al. 2009).
The analyzed markers are essential for the determination of macrophage activation pathways and also have an influence on atherosclerotic plaque stability. However, the biochemical mechanisms of macrophage phenotype alternation by ezetimibe still remain vague. Based on our current knowledge, macrophage phenotype modulation by ezetimibe might be due to its influence on the expression of Toll-like receptors (TLRs). The drug decreases TLR2 and TLR4 expression in the cell membranes of hypercholesterolemic patients. Signaling via both the receptors promotes inflammatory responses and progression of atherosclerosis. Furthermore, TLR2 and TLR4 expression is elevated in the monocytes of atherosclerotic patients (Moutzouri et al. 2012). Investigation of further activation markers such as tumor necrosis factor alpha, IL-6, IL-12, and reactive oxygen species for the classical activation and IL-10, tumor growth factor-β1, and prostaglandin-E2 for the alternative activation would be helpful to clarify the effect of ezetimibe and elucidate its potential mechanism.
Conclusions
In summary, our study indicates that ezetimibe, used in vitro at a concentration that occurs in serum, is likely to induce the alternative activation of monocyte-derived macrophages isolated from patients with hypercholesterolemia, concomitantly suppressing the classical activation. Earlier studies additionally demonstrated that the drug increases the stability of atherosclerotic plaques in animals. Taken together, it is probable that the substance may stabilize the plaques in hypercholesterolemic patients. It is essential to carry out further clinical studies to assess the latter.
References
Alvarez-Sala LA, Cachofeiro V, Masana L, Suarez C, Pinilla B, Plana N et al (2008) Effects of fluvastatin extended-release (80 mg) alone and in combination with ezetimibe (10 mg) on low-density lipoprotein cholesterol and inflammatory parameters in patients with primary hypercholesterolemia: a 12-week, multicenter, randomized, open-label, parallel-group study. Clin Ther 30:84–97
Auffray C, Sieweke H, Geissmann F (2009) Blood monocytes: development, heterogeneity, and relationship with dendritic cells. Annu Rev Immunol 27:669–692
Bradford MM (1976) A rapid and sensitive method for the quantification of microgram quantities of protein utilizing the principle of protein dye-binding. Anal Biochem 72:248–251
Cheng Y, Liu F, Wu J, Zhang Y, Nilsson A, Duan RD (2009) Ezetimibe inhibits expression of acid sphingomyelinase in liver and intestine. Lipids 44:897–906
Chinetti-Gbaguidi G, Baron M, Bouhlel MA, Vanhoutte J, Copin C, Sebti Y et al (2011) Human atherosclerotic plaque alternative macrophages display low cholesterol handling but high phagocytosis because of distinct activities of the PPARγ and LXRα pathways. Circ Res 108:985–995
Chomczyński P, Sacchi N (1987) Single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction. Anal Biochem 162:156–159
Feig JE, Feig JL (2012) Macrophages, dendritic cells, and regression of atherosclerosis. Front Physiol 3:286
Ferrante CJ, Pinhal-Enfield G, Elson G, Cronstein BN, Hasko G, Outram S, Leibovich SJ (2013) The adenosine-dependent angiogenic switch of macrophages to an M2-like phenotype is independent of interleukin-4 receptor alpha (IL-4Rα) signaling. Inflammation 36:921–931
Fleetwood AJ, Dinh H, Cook AD, Hertzog PJ, Hamilton JA (2009) GM-CSF- and M-CSF-dependent macrophage phenotypes display differential dependence on type I interferon signaling. J Leukoc Biol 86:411–421
Flø RW, Naess A, Lund-Johansen F, Maehle BO, Sjursen H, Lehmann V, Solberg CO (1991) Negative selection of human monocytes using magnetic particles covered by anti-lymphocyte antibodies. J Immunol Methods 137:69–94
Gómez-Garre D, Muñoz-Pacheco P, González-Rubio ML, Aragoncillo P, Granados R, Fernández-Cruz A (2009) Ezetimibe reduces plaque inflammation in a rabbit model of atherosclerosis and inhibits monocyte migration in addition to its lipid-lowering effect. Br J Pharmacol 156:1218–1227
Gordon S, Taylor PR (2005) Monocyte and macrophage heterogeneity. Nat Rev Immunol 5:953–964
Ibrahim M, Farghaly E, Gomaa W, Kelleni M, Abdelrahman A (2010) Ezetimibe inhibits proinflammatory mediators involved in the pathogenesis of non alcoholic fatty liver disease. Egypt J Med Sci 31:247–269
Johnson JL, Newby AC (2009) Macrophage heterogeneity in atherosclerotic plaques. Curr Opin Lipidol 20:370–378
Khallou-Laschet J, Varthaman A, Fornasa G, Compain C, Gaston AT, Clement M et al (2010) Macrophage plasticity in experimental atherosclerosis. PLoS One 5:e8852
Krysiak R, Okopień B (2011) The effect of ezetimibe and simvastatin on monocyte cytokine release in patients with isolated hypercholesterolemia. J Cardiovasc Pharmacol 57:505–512
Łabuzek K, Liber S, Bułdak L, Machnik G, Liber J, Okopień B (2013) Eplerenone promotes alternative activation in human monocyte-derived macrophages. Pharmacol Rep 65:226–234
Lovren F, Pan Y, Quan A, Szmitko PE, Singh KK, Shukla PC et al (2010) Adiponectin primes human monocytes into alternative anti-inflammatory M2 macrophages. Am J Physiol Heart Circ Physiol 299:H656–H663
Lutgens E, Lievens D, Beckers L, Wijnands E, Soehnlein O, Zernecke A et al (2010) Deficient CD40-TRAF6 signaling in leukocytes prevents atherosclerosis by skewing the immune response toward an antiinflammatory profile. J Exp Med 207:391–404
Martinez-Pomares L (2012) The mannose receptor. J Leukoc Biol 92:1177–1186
McLaren JE, Michael DR, Ashlin TG, Ramji DP (2011) Cytokines, macrophage lipid metabolism and foam cells: implications for cardiovascular disease therapy. Prog Lipid Res 50:331–347
Mielczarek-Puta M, Chrzanowska A, Graboń W, Barańczyk-Kuźma A (2008) New insights into arginase. Part II Role in physiology and pathology. Postepy Hig Med Dosw (Online) 62:214–221
Moutzouri E, Tellis CC, Rousouli K, Liberopoulos EN, Milionis HJ, Elisaf MS, Tselepis AD (2012) Effect of simvastatin or its combination with ezetimibe on Toll-like receptor expression and lipopolysaccharide-induced cytokine production in monocytes of hypercholesterolemic patients. Atherosclerosis 225:381–387
Muñoz-Pacheco P, Ortega-Hernández A, Miana M, Cachofeiro V, Fernández-Cruz A, Gómez-Garre D (2012) Ezetimibe inhibits PMA-induced monocyte/macrophage differentiation by altering microRNA expression: a novel anti-atherosclerotic mechanism. Pharmacol Res 66:536–543
Nakagami H, Osako MK, Takami Y, Hanayama R, Koriyama H, Mori M et al (2009) Vascular protective effects of ezetimibe in ApoE-deficient mice. Atherosclerosis 203:51–58
Netea MG, Nold-Petry CA, Nold MF, Joosten LA, Opitz B, van der Meer JH et al (2009) Differential requirement for the activation of the inflammasome for processing and release of IL-1beta in monocytes and macrophages. Blood 113:2324–2335
Okopień B, Kowalski J, Krysiak R, Łabuzek K, Stachura-Kułach A et al (2005) Monocyte suppressing action of fenofibrate. Pharmacol Rep 57:367–372
Panda SK, Kumar S, Tupperwar NC, Vaidya T, George A, Rath S et al (2012) Chitohexaose activates macrophages by alternate pathway through TLR4 and blocks endotoxemia. PLoS Pathog 8:e1002717
Rajaiah R, Perkins DJ, Polumuri SK, Zhao A, Keegan AD, Vogel SN (2013) Dissociation of endotoxin tolerance and differentiation of alternatively activated macrophages. J Immunol 190:4763–4772
Raz-Pasteur A, Gamliel-Lazarovich A, Coleman R, Keidar S (2012) Eplerenone reduced lesion size in early but not advanced atherosclerosis in apolipoprotein E-deficient mice. J Cardiovasc Pharmacol 60:508–512
Rees AJ (2010) Monocyte and macrophage biology: an overview. Semin Nephrol 30:216–233
Rudofsky G, Reismann P, Groener JB, Djuric Z, Fleming T, Metzner C et al (2012) Identical LDL-cholesterol lowering but non-identical effects on NF-κB activity: high dose simvastatin vs combination therapy with ezetimibe. Atherosclerosis 223:190–196
Sica A, Mantovani A (2012) Macrophage plasticity and polarization: in vivo veritas. J Clin Invest 122:787–795
Sonoki T, Nagasaki A, Gotoh T, Takiguchi M, Takeya M, Matsuzaki H, Mori M (1997) Coinduction of nitric-oxide synthase and arginase I in cultured rat peritoneal macrophages and rat tissues in vivo by lipopolysaccharide. J Biol Chem 272:3689–3693
Suchy D, Łabuzek K, Stadnicki A, Okopień B (2011) Ezetimibe—a new approach in hypercholesterolemia management. Pharmacol Rep 63:1335–1348
Suchy D, Łabuzek K, Pierzchała O, Okopień B (2013) RP-HPLC-UV determination of ezetimibe in serum: method development, validation and application to patients chronically receiving the drug. Acta Chromatogr 25:483–502
Tripathi P (2007) Nitric oxide and immune response. Indian J Biochem Biophys 44:310–319
Undas A, Machnik A, Potaczek DP, Wypasek E, Zmudka K, Tracz W (2011) Ezetimibe combined with simvastatin compared with simvastatin alone results in a greater suppression of oxidative stress and enhanced fibrinolysis in patients after acute coronary events. J Cardiovasc Pharmacol 58:167–172
Van der Plas MJ, van Dissel JT, Nibbering PH (2009) Maggot secretions skew monocyte-macrophage differentiation away from a pro-inflammatory to a pro-angiogenic type. PLoS One 4:e8071
Varin A, Gordon S (2009) Alternative activation of macrophages: immune function and cellular biology. Immunobiology 214:630–641
Wilson HM (2010) Macrophages heterogeneity in atherosclerosis—implications for therapy. J Cell Mol Med 14:2055–2065
Zhou Q, Amar S (2007) Identification of signaling pathways in macrophage exposed to Porphyromonas gingivalis or to its purified cell wall components. J Immunol 179:7777–7790
Acknowledgments
The authors would like to thank Ms. Jarosława Sprada and Ms. Halina Klimas for their excellent technical cooperation. This work was supported by a doctoral student KNW-1-003/D/2/0 research grant from the Medical University of Silesia, Katowice, Poland. The study was sponsored by Polpharma Scientific Foundation.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution License which permits any use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Suchy, D., Łabuzek, K., Machnik, G. et al. The influence of ezetimibe on classical and alternative activation pathways of monocytes/macrophages isolated from patients with hypercholesterolemia. Naunyn-Schmiedeberg's Arch Pharmacol 387, 733–742 (2014). https://doi.org/10.1007/s00210-014-0982-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-014-0982-4