Abstract
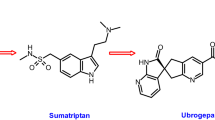
Migraine is a recurrent incapacitating neurovascular disorder characterized by unilateral and throbbing headaches associated with photophobia, phonophobia, nausea, and vomiting. Current specific drugs used in the acute treatment of migraine interact with vascular receptors, a fact that has raised concerns about their cardiovascular safety. In the past, α-adrenoceptor agonists (ergotamine, dihydroergotamine, isometheptene) were used. The last two decades have witnessed the advent of 5-HT1B/1D receptor agonists (sumatriptan and second-generation triptans), which have a well-established efficacy in the acute treatment of migraine. Moreover, current prophylactic treatments of migraine include 5-HT2 receptor antagonists, Ca2+ channel blockers, and β-adrenoceptor antagonists. Despite the progress in migraine research and in view of its complex etiology, this disease still remains underdiagnosed, and available therapies are underused. In this review, we have discussed pharmacological targets in migraine, with special emphasis on compounds acting on 5-HT (5-HT1–7), adrenergic (α1, α2, and β), calcitonin gene-related peptide (CGRP1 and CGRP2), adenosine (A1, A2, and A3), glutamate (NMDA, AMPA, kainate, and metabotropic), dopamine, endothelin, and female hormone (estrogen and progesterone) receptors. In addition, we have considered some other targets, including gamma-aminobutyric acid, angiotensin, bradykinin, histamine, and ionotropic receptors, in relation to antimigraine therapy. Finally, the cardiovascular safety of current and prospective antimigraine therapies is touched upon.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Migraine is a complex paroxysmal disorder affecting a substantial proportion of the population (Rasmussen et al. 1991), with a 2–3-fold higher prevalence in females than in males (15–18% vs. 6%; Stewart et al. 1992). Migraine is characterized by episodes of usually throbbing, unilateral, and severe headaches, which are in about 15% of patients preceded by reversible focal neurological (mostly visual) ‘aura’ symptoms that tend to develop gradually over 5 to 20 min and last for less than 60 min (Olesen and Lipton 1994). Migraine attacks may be associated with nausea, vomiting, sensitivity to light and sounds, or movement and, without treatment, typically last 4 to 72 h (Ferrari and Saxena 1993; Olesen and Lipton 1994).
The pathogenesis of migraine headache is not completely understood, but it is thought to involve three key factors, namely, (a) the cranial blood vessels, (b) the trigeminal innervation of these vessels, and (c) the reflex connection of the trigeminovascular system (Fig. 1) in the cranial parasympathetic outflow (Goadsby et al. 2002a). Although the brain is insensitive to pain, nociceptive stimuli can be generated by large cranial and proximal intracranial blood vessels, as well as by the dura mater. Evidence for peripheral trigeminal activation in migraine is provided by the release of calcitonin gene-related peptide (CGRP; Arulmani et al. 2004; Goadsby and Lance 1990) even though the mechanism of generation of pain is not clear. Studies in animals have suggested that the pain may be caused by a sterile neurogenic inflammatory process in the dura mater (Moskowitz and Cutrer 1993), but this mechanism has not been clearly established to correlate in humans (May et al. 1998). The pain may be an amalgamation of an altered perception—as a result of peripheral and/or central sensitization of craniovascular input that is not usually painful (Burstein et al. 2000) and the activation of a feed-forward neurovascular dilator mechanism that is functionally explicit for the first (ophthalmic) division of the trigeminal nerve (May et al. 2001). Nitric oxide (NO) also seems to be involved in migraine pathophysiology, and inhibition of its synthesis may have therapeutic relevance (Lassen et al. 1998). Cranial vasodilatation during a migraine attack would lead to an enhanced blood volume following each cardiac stroke, with a resultant augmentation in pulsations within the affected blood vessels. The increased pulsations can then be sensed by “stretch” receptors in the vascular wall, and the resultant boost in perivascular (trigeminal) sensory nerve activity provokes headache and other symptoms (Fig. 1; Saxena and Tfelt-Hansen 2006). This trigeminal stimulation may also release neuropeptides, thus reinforcing vasodilatation and perivascular nerve activity (Moskowitz et al. 1989; Villalón et al. 2002).
Schematic representation of the pathophysiology of migraine. The pathophysiologic changes in migraine putatively stem from ion leakage through channels in the brain stem, leading to a decreased cerebral blood flow (CBF), possibly owing to cortical spreading depression and, subsequently, neuropeptide release and dilatation of cranial extracerebral blood vessels. The increased pulsation in these blood vessels stimulates the trigeminovascular system, setting in peripheral and central sensitization and leading to headache and associated symptoms (nausea, vomiting, phonophonophobia, and/or photophobia). CTZ: Chemoreceptor trigger zone. Redrawn from Saxena and Tfelt-Hansen (2006)
Receptor subtypes involved in pharmacological treatments of migraine
Both basic research and clinical studies provide evidence for several receptor targets in antimigraine therapy. Several migraine models, based on vascular and neuronal involvement, show that different receptors could be targeted for the development of antimigraine compounds (Arulmani et al. 2006; De Vries et al. 1999b). In this context, it should be emphasized that the currently available migraine models do not entail all facets of this clinically heterogeneous disorder but are rather based on some of the symptoms observed in migraine (e.g., focus on only neuronal or vascular aspects). Thus, no model that mimics all aspects of a migraine attack is available yet. An important vascular in vivo model determines blood flow in porcine carotid arteriovenous anastomoses (Fig. 2). This model is based on the observation from Heyck (1969) that the oxygen saturation difference between the arterial and external jugular venous blood (OSDA-V) was abnormally small during the headache phase of migraine, being consistent with (a) dilatation of carotid arteriovenous anastomoses, (b) the facial paleness and the increase in temporal artery pulsations and swelling of the frontal vein on the side of the headache (Drummond and Lance 1983; Drummond and Lance 1984), and (c) normalization of the decreased OSDA-V after spontaneous or ergotamine-induced headache relief (Heyck 1969). Other models utilize electrical stimulation of the trigeminal ganglion/nerve to study neurogenic dural inflammation, while the superior sagittal sinus stimulation model takes into account the transmission of trigeminal nociceptive input in the brainstem. More recently, the introduction of integrated models, namely electrical stimulation of the trigeminal ganglion or systemic administration of capsaicin, has allowed studies on the activation of the trigeminal system and its effects on the cranial vasculature (for review, see Arulmani et al. 2006). This review also contains data on the ability of several drugs to inhibit plasma protein extravasation (e.g., Weiss et al. 2006), although it should be kept in mind that extravasation inhibitors, such as CP-122,288 (Roon et al. 2000), the neurokinin-1 receptor antagonist lanepitant (Goldstein et al. 2001a; Goldstein et al. 1997), and the mixed ETA/ETB receptor antagonist bosentan (May et al. 1996) proved ineffective in the treatment of migraine. Thus, the relevance of plasma protein extravasation in migraine is no longer tenable (Peroutka 2005).
A schematic representation of a vascular bed containing an arteriovenous anastomosis (AVA), which is a precapillary communication between artery and veins. When AVAs are dilated, as proposed to be the case during migraine (Heyck 1969), arterial blood flow will be shunted to the venous side
On this basis, the present review focuses on recent pharmacological advances in the treatment of migraine, while new therapeutic principles are also presented. The pharmacological targets that will be discussed seem to be promising because of their involvement in either reducing total carotid conductance in porcine or canine migraine models or because of their effects on trigeminovascular nociceptive pathways.
5-HT receptors
Serotonin [5-hydroxytryptamine (5-HT)], being present in high concentrations in enterochromaffin cells of gastrointestinal mucosa and blood platelets, was identified and isolated from the gastrointestinal tract (as enteramine) by Erspamer and colleagues in Italy (Erspamer 1954) and from the blood (as serotonin) by Page and colleagues in the United States (Page 1954). In 1948, the American group deduced that the vasoconstrictor substance serotonin was chemically 5-HT (Rapport et al. 1948) and, shortly afterward, the Italians established that enteramine and 5-HT were identical (Erspamer and Asero 1952). Since then, a number of 5-HT receptors (5-HT1–7 and their subtypes) have been identified (Hoyer et al. 1994; Saxena et al. 1998; Saxena and Villalón 1990) as being responsible for a wide host of effects (Villalón and Centurión 2007).
Migraine has been described as a “low 5-HT syndrome”, suggesting that 5-HT may play an important role in its pathophysiology and treatment (Anthony and Lance 1989). In this respect, (a) there is an elevation of urinary excretion of 5-hydroxyindole acetic acid, the major metabolite of 5-HT, during migraine attacks (Curran et al. 1965); (b) platelet 5-HT levels were found to drop rapidly during the onset of a migraine attack (Anthony et al. 1967); (c) reserpine, which depletes 5-HT (and noradrenaline), precipitates migraine attacks (Carroll and Hilton 1974); and (d) intravenous injection of 5-HT reduces headache intensity in migraineurs (Anthony et al. 1967; Kimball et al. 1960).
5-HT1 receptor subtypes
The 5-HT1 receptor class comprises five different receptor subtypes, which share 41–63% overall sequence identity and couple preferentially to Gi/Go to inhibit cAMP formation (Lesch and Lerer 1991). One of these, the 5-ht1E receptor, is given a lower-case appellation to denote that, although gene products encoding putative receptors have been identified, no functional role has yet been found.
A number of well-defined selective agonists and antagonists are available to delineate 5-HT1A receptors. The 5-HT1A agonist buspirone was reported to have a prophylactic effect in migraine with anxiety disorder, which was not secondary to its anxiolytic effect (Lee et al. 2005). Further lines of evidence support the hypothesis that migraine without aura is associated with a relative hypersensitivity of central 5-HT1A receptors. This is of relevance given the role of the 5-HT1A receptor in controlling raphe 5-HT neuronal tone and the possible association between migraine, anxiety, and depression (Cassidy et al. 2003). Furthermore, most antimigraine drugs display high affinity for 5-HT1A and/or 5-HT2 receptor subtypes in human brain (Peroutka 1988). For example, tertatolol, which is a β-adrenoceptor antagonist with 5-HT1A receptor agonist property, decreased porcine carotid blood flow and conductance, indicating active arteriovenous anastomotic constriction. It has therefore been suggested that tertatolol may prove effective in the treatment of migraine (Saxena et al. 1992). However, antimigraine efficacy cannot be explained by drug interactions with a single 5-HT receptor subtype (Peroutka 1988) and, most importantly, several lines of evidence argue against 5-HT1A receptor involvement in the constriction of porcine arteriovenous anastomoses, namely, (a) ipsapirone, a selective 5-HT1A receptor partial agonist, did not induce carotid vasoconstriction (Bom et al. 1988); (b) indorenate, another 5-HT1A receptor agonist, induced porcine carotid vasoconstriction, but metergoline, a drug with higher affinity for 5-HT1A, 5-HT1B, and 5-HT1D receptors, failed to significantly antagonize the responses to indorenate, thus concluding that the effect of indorenate was not due to its agonist action on 5-HT1A receptors (Villalón et al. 1990). Therefore, it appears that 5-HT1A receptors do not mediate vasoconstriction in the porcine carotid model and the vascular effects mediated by 5-HT1A receptors seem to be rather limited (if any), while the role of central activation of 5-HT1A receptors in migraine remains speculative.
The unambiguous differentiation of 5-HT1B and 5-HT1D receptor-mediated effects was hampered by the close pharmacological identity of these receptors. However, two antagonists can pharmacologically discriminate between these receptor subtypes, namely, BRL15572 with a 60-fold selectivity for 5-HT1D over 5-HT1B receptors and SB224289 with a 75-fold selectivity for 5-HT1B over 5-HT1D receptors (Price et al. 1997). 5-HT1B/1D receptor agonists induce selective carotid vasoconstriction (Saxena et al. 1998). The 5-HT1B receptor is primarily involved in sumatriptan-induced contractions of human cranial, as well as certain peripheral blood vessels, as illustrated by the observation that vasoconstriction induced by 5-carboxamidotryptamine and sumatriptan is antagonized by SB224289, but not by BRL15572 (van den Broek et al. 2002; Villalón and Centurión 2007; Wackenfors et al. 2005). Moreover, 5-HT1D and 5-HT1F receptors induce presynaptic inhibition of the trigeminovascular inflammatory responses implicated in migraine (Cutrer et al. 1997b; Villalón et al. 2002).
Selective agonists at 5-HT1D (PNU 142633, McCall et al. 2002) and 5-HT1F (LY334370, Phebus et al. 1997) receptors inhibit the trigeminovascular system without inducing vasoconstriction. In addition, a central mechanism of action in blocking the transmission of nociceptive impulses within the trigeminal nucleus caudalis may contribute to the antimigraine effect of LY334370 (Shepheard et al. 1999). Nevertheless, PNU-142633 proved to be ineffective in the acute treatment of migraine (Gómez-Mancilla et al. 2001), while LY334370 did show some efficacy in high doses that may have interacted with 5-HT1B receptors (Goldstein et al. 2001b; Villalón et al. 2002).
There is a high correlation between the potency of various 5-HT1 receptor agonists in the guinea-pig dural plasma protein extravasation assay and their 5-HT1F receptor binding affinity (Ramadan et al. 2003). However, as previously pointed out, the relevance of plasma protein extravasation in migraine is no longer tenable (Peroutka 2005). Also, 5-HT1F receptors are located on glutamate-containing neurons, and their activation might inhibit glutamate release (Ma 2001), which may be relevant to its antimigraine action (Martínez et al. 1993). Indeed, most triptans show high pK i values for 5-HT1F receptors (De Vries et al. 1999a; Goadsby and Classey 2003). Thus, although the clinical efficacy of 5-HT1F receptor agonists has not yet unequivocally been demonstrated, some preclinical experiments and clinical observations argue in favor of the potential effectiveness of selective 5-HT1F agonists in migraine.
Since second-generation triptans may be more brain penetrant than sumatriptan (Millson et al. 2000), the relevance of central effects of the triptans should be considered. Although the second-generation triptans have not proven more efficacious than sumatriptan (Saxena and Tfelt-Hansen 2006), they do inhibit trigeminovascular input to the nucleus tractus solitarius via activation of 5-HT1B/1D receptors (Hoskin et al. 2004). In addition, inhibitory actions of 5-HT1B, 5-HT1D and 5-HT1F receptors in the trigeminocervical complex of the cat have been documented, and 5-HT1B receptor-mediated inhibition is the most potent of the three in terms of inhibition of trigeminovascular nociceptive traffic (Goadsby and Classey 2003). Thus, the 5-HT1B receptor subtype is highly explored in the drug development for migraine, and the present drugs for the acute treatment of migraine (namely triptans) potently stimulate 5-HT1B receptors.
A major disadvantage of triptans is the threat of coronary vasoconstriction (MaassenVanDenBrink et al. 1998), implying that these drugs should not be administered to patients with coronary or cerebrovascular disease (Dodick et al. 2004; Tepper 2001).
5-HT2 receptor subtypes
The 5-HT2 receptor class comprises three receptor subtypes (i.e., 5-HT2A, 5-HT2B, and 5-HT2C), which exhibit 46–50% overall sequence identity and couple preferentially to Gq/G11 to increase the hydrolysis of inositol phosphates elevating cytosolic [Ca2+] (Shih et al. 1991). The anatomical distribution and physiological function of these three receptors appear to be discrete. The 5-HT2B and 5-HT2C receptors display a higher affinity for 5-HT than the 5-HT2A subtype. Although antagonists for each of these receptors are now available, only BW723C86 is known as a selective 5-HT2B receptor agonist. This agonist elicits hypertensive (rather than hypotensive) responses in vagosympathectomized rats (Centurión et al. 2004).
Decreased 5-HT concentrations, as well as an upregulation of 5-HT2 receptors in platelets, have been observed in patients with chronic headache, which may be caused by abuse of analgesic substances (Sarchielli et al. 1999). Involvement of the 5-HT2 receptor in migraine is suggested by the 5-HT2 receptor antagonist methysergide, which is also a partial agonist at 5-HT1 receptors, and is used for migraine prophylaxis in severe cases where other preventive drugs are not effective (Silberstein 1998). The 5-HT2A/2C receptor genes have been studied as candidate genes for migraine (Buchwalder et al. 1996), but no mutations in the deduced amino acid sequence of either receptor in the sample of migraineurs was observed. Thus, the authors concluded that DNA-based mutations in the 5-HT2A and 5-HT2C receptors are not generally involved in the pathogenesis of migraine. In contrast, Erdal et al. (2001) reported that the T102C polymorphism of the 5-HT2A receptor gene is related to migraine with aura. Since the sample size used in this study was small, the role of the 5-HT2A receptor in the pathophysiology of migraine or the aura should be considered with caution.
Concerning the 5-HT2C receptor, alternative splicing events yield non-functional isoforms of the 5-HT2C receptor, and as many as seven functional isoforms of the 5-HT2C receptor are produced by adenine deaminase editing of the receptor messenger RNA (mRNA). Although these receptor isoforms show no gross differences in their operational characteristics, they are differentially distributed throughout central and peripheral tissues. The purpose of these isoforms remains speculative, but they may be important in determining cell differences in receptor desensitization, cell-surface distribution, and/or the trafficking of agonist responses through different effector pathways. Thus, there is a need to explore the functions of these isoforms, which might serve as new targets for future antimigraine drugs.
Activation of the 5-HT2A receptor leads to an enhancement of NO production in the trigeminovascular pathway. This NO production may trigger migraine attacks by inducing cerebral vasodilation and sensitization of the perivascular nociceptors and central nociceptive neurons in the trigeminovascular system. Thus, the upregulation of this pronociceptive receptor can increase headache attacks and may contribute to the development of chronic daily headache (Srikiatkhachorn et al. 2002). Also, 5-HT2B receptors, located on endothelial cells of meningeal blood vessels, may trigger migraine headache via the formation of NO. Indeed, 5-HT2B receptor stimulation relaxes the porcine cerebral artery via the release of NO (Schmuck et al. 1996). However, if 5-HT2B receptor antagonists are used in migraine patients, this might lead to coronary side effects as inhibition of NO production may also induce coronary vasoconstriction. Indeed, 5-HT2B receptor mRNA has been demonstrated in human coronary artery (Ishida et al. 1999), and activation of 5-HT2B receptors in human coronary artery induces NO release (Ishida et al. 1998). Selective 5-HT2B receptor antagonists have been described (Forbes et al. 1995; Johnson et al. 2003) and proven efficacious in blocking plasma protein extravasation (Johnson et al. 2003). In addition, 8′-hydroxy-dihydroergotamine, the major metabolite of the antimigraine drug dihydroergotamine, may induce a persistent desensitization of 5-HT2B receptors, which may contribute to its therapeutic efficacy (Schaerlinger et al. 2003). The study of 5-HT2B receptor blockade in migraine prophylaxis is awaited to substantiate the presumed hypersensitivity of these receptors in migraine and, hence, their suspected role in the initiation of the neurogenic inflammatory response (Cohen et al. 1996; Fozard and Kalkman 1994; Kalkman 1994; Schmuck et al. 1996).
5-HT3, 5-HT4, 5-ht5A/5B, 5-HT6, and 5-HT7 receptors
The 5-HT3 receptor is unique among existing 5-HT receptors in being the only member to belong to the ligand-gated cation channel super-family of receptors (Hoyer 1990; Hoyer et al. 1994). It appears to be located exclusively in neuronal tissue, where it mediates fast depolarization. The receptors are expressed in the central nervous system, as well as in the periphery, where 5-HT3 receptors are found on autonomic neurons and on neurons of the sensory and enteric nervous system (Barnes and Sharp 1999). Although the 5-HT4, 5-HT6, and 5-HT7 receptors all couple preferentially to Gs and promote cAMP formation, they are classified as distinct receptor classes because they exhibit <40% overall sequence identity with other 5-HT receptors (Hoyer et al. 1994). The 5-ht5 receptors include two subtypes, namely, (a) the 5-ht5A subtype, which is preferentially coupled to the Gi/G0 family causing adenylyl cyclase inhibition (Francken et al. 1998; Hurley et al. 1998); (it could also be coupled to inwardly rectifying potassium channels); and (b) the 5-ht5B subtype, the transductional system of which is unknown (see Thomas 2006).
5-HT receptor diversity is increased by the existence of isoforms produced by post-translational modifications. Alternative splicing events yield four functional variants of the 5-HT4 receptor, i.e., 5-HT4(a)–5-HT4(d) (Medhurst et al. 2001; Pindon et al. 2002), and four functional variants of the 5-HT7 receptor, i.e., 5-HT7(a)–5-HT7(d) (Krobert and Levy 2002). The purpose of these isoforms remains speculative, but they may be important in determining cell differences in receptor desensitization, cell-surface distribution, or the trafficking of agonist responses through different effector pathways.
The receptor types mentioned above are not much explored for the development of antimigraine compounds. However, some studies have assessed their role in the carotid circulation. In one such study, intravenously administered 5-HT was found to be a vasodilator in vivo in the cat dural circulation, and the authors showed that the dilation is not mediated by 5-HT1, 5-HT2, 5-HT4, or 5-HT7 receptors but primarily mediated by a vagal reflex, initiated via 5-HT3 receptor activation, and brought about by an increase in parasympathetic tone to the middle meningeal artery as part of the Von Bezold–Jarisch reflex (Lambert et al. 2004). Based on the hypothesis that 5-HT3 receptor antagonists might well inhibit neurogenic dural inflammation, 5-HT3 receptor antagonists have been assessed for the treatment of migraine but were unfortunately found to be ineffective (Ferrari 1991). This lack of effectiveness could possibly be explained by their complex, bell-shaped, dose–response relationship, but further trials with adjusted doses were prevented by their alleged toxicity upon chronic administration (Ferrari 1991). A clinical indication of 5-HT3 receptor antagonists is the prevention of emesis (Hasler 1999). Indeed, control of migraine-associated nausea and vomiting is often achieved with the benzamide dopamine D2 receptor antagonist metoclopramide (Dahlöf and Hargreaves 1998), which also has 5-HT3 receptor antagonist activity and reproducibly stimulates gastric motility to increase the availability of orally administered drugs and is thus used in the treatment of migraine (Dahlöf and Hargreaves 1998).
There is evidence to suggest that 5-HT7 receptors may play a role in central nervous system disorders, including anxiety and cognitive disturbances and also migraine, probably via both peripheral and central mechanisms (Thomas and Hagan 2004). Indeed, mRNA of 5-HT7 receptors is present in trigeminal ganglia (Terrón et al. 2001). Since dilatation of cranial blood vessels has been proposed to play an important role in the pathogenesis of a migraine attack (Villalón et al. 2002), 5-HT7 receptor antagonists could well be effective as prophylactic antimigraine agents (Terrón et al. 2001). A number of 5-HT7 receptor-selective antagonists, including SB-269970A, SB-258741, and SB-656104A, have been developed (Pouzet 2002; Thomas and Hagan 2004) but, obviously, clinical trials are needed to accept or reject their proposed mechanism of action.
Adrenoceptors
The endogenous catecholamines noradrenaline and adrenaline, which are released upon activation of the sympathetic nervous system, play an essential role in the regulation of a host of physiological responses. Several decades ago, adrenoceptors were introduced to explain the difference in actions of noradrenaline and adrenaline (see Hein and Kobilka 1995). Adrenoceptors are found in nearly all peripheral tissues and on many neuronal populations within the central nervous system. Both noradrenaline and adrenaline play important roles in the control of blood pressure, myocardial contractile rate and force, airway reactivity, and a variety of metabolic and central nervous system functions (Hoffman 2001). Agonists and antagonists interacting with adrenoceptors have proven useful in the treatment of a variety of diseases, including hypertension, angina pectoris, congestive heart failure, asthma, depression, benign prostatic hypertrophy, and glaucoma (Hoffman 2001).
Adrenoceptors can be divided into two major types, the α- and β-adrenoceptors (Bylund et al. 1994), which can be further subdivided into several subtypes based on molecular and pharmacological characteristics, although species orthologs of some adrenoceptor subtypes have been identified (Bylund et al. 1995). α1-Adrenoceptors mediate their actions through stimulation of inositol phosphate release (Michelotti et al. 2000), while β-adrenoceptors stimulate (Stiles et al. 1984) and α2-adrenoceptors inhibit (Limbird 1988) adenylyl cyclase.
α1A- α1B-, and α1D-adrenoceptor subtypes
Cloning has identified three α1-adrenoceptor subtypes. The α1B-adrenoceptor from the DDT cell line (hamster smooth muscle) was cloned first (Cotecchia et al. 1988), followed by the α1A subtype (Ford et al. 1994; Hieble et al. 1995). A third α1-adrenoceptor was cloned from rat cortex and designated as the α1A-adrenoceptor (Lomasney et al. 1991). However, an identical recombinant rat α1-adrenoceptor subtype was independently identified by Perez et al. (1991) and denoted the α1D-adrenoceptor. A fourth α1-adrenoceptor subtype has been postulated and is designated as α1L based on its low affinity for prazosin (Oshita et al. 1991).
α1-Adrenoceptors are G-protein-coupled receptors and mediate their responses via a Gq/11 mechanism (Michelotti et al. 2000). This involves activation of phospholipase C-dependent hydrolysis of phosphatidyl 4,5-biphosphate generating inositol 1,4,5 -trisphosphate (IP3), which acts on the IP3 receptor in the endoplasmic reticulum to release stored Ca2+ and diacylglycerol that (together with Ca2+) can activate protein kinase C. Production of these second messengers activates both voltage-dependent and voltage-independent Ca2+ -channels, leading to smooth muscle contraction in both vascular and non-vascular tissues (e.g., prostate, vas deferens, and heart).
In line with the findings suggesting that carotid arteriovenous anastomoses dilate and could play an important role in the pathogenesis of migraine (Heyck 1969), it is reasonable to assume that compounds that induce a cranioselective vasoconstriction may have potential therapeutic use in the treatment of migraine (Willems et al. 2003). The α1A-adrenoceptor is the main subtype of α1-adrenoceptors regulating systemic vascular resistance and blood pressure (Docherty 1998; Vargas and Gorman 1995). In view of its widespread distribution, it is rather unlikely that a selective α1A-adrenoceptor agonist would be useful in the treatment of migraine. Considering this standpoint, the α1B-adrenoceptor is a motivating target for future antimigraine drugs, especially when considering that this receptor does not seem to be much involved in the constriction of the systemic vasculature (Piascik et al. 1997; Vargas and Gorman 1995), and, predominantly, α1A-, but not α1B- (or α1D-), adrenoceptors mediate the hypertensive effect induced by intravenous administration of phenylephrine in anesthetized pigs. Figure 3 (left panel) depicts the involvement of α1-adrenoceptor subtypes in the carotid vasculature (Willems et al. 2001b). In addition, studies in mice have provided several clues to help elucidate subtype-specific physiological functions, for instance, α1A-and α1D-adrenoceptor subtypes play an important role in the regulation of blood pressure (Tanoue et al. 2003). Thus, these subtypes should not be explored for the development of novel antimigraine drugs, although such subtype-selective antagonists might be desirable antihypertensive agents. Therefore, a selective α1B-adrenoceptor agonist could have advantages over the currently available acute antimigraine drugs, which all constrict the human isolated coronary artery (MaassenVanDenBrink et al. 1998; MaassenVanDenBrink et al. 2000).
The effect of α1 (phenylephrine)- and α2 (BHT933)-adrenoceptor agonists inducing vasoconstriction in the canine external carotid circulation. Animals were pretreated with the α1-adrenoceptor antagonists 5-methylurapidil (5MU) and BMY 7378 (BMY) or the α2-adrenoceptor antagonists BRL44408 (BRL) and MK-912 (MK; Willems et al. 2001a). *, P<0.05 vs. corresponding dose of agonist in control curve. **, P<0.05 vs. corresponding dose of agonist after administration of the first antagonist (i.e. BMY 7378 in the left panel and BRL44408 in the right panel)
Using a closed cranial window model, the rat dural vasodilatation in response to electrical stimulation is not affected by pretreatment with an α1-adrenoceptor agonist (phenylephrine) or its antagonist (corynanthine; Akerman et al. 2001). Although these results suggest that the adrenergic system does not play a significant role in neurogenic dural vasodilatation, the porcine studies mentioned above do suggest that α-adrenoceptor agonists should still be considered for the development of potential antimigraine drugs. Moreover, studies on human subjects suggest that migraineurs have sympathetic hypofunction (Boccuni et al. 1989; Peroutka 2004). Accordingly, drugs targeting on subtypes of α1-adrenoceptors, which lack systemic vasoconstriction, could hold a promising future in antimigraine therapy.
α2A, α2B, and α2C-adrenoceptor subtypes
Evidence for the existence of α2-adrenoceptor subtypes has come from binding and functional studies in various tissues and cell lines and, more recently, from cells transfected with the cDNA for the receptors (Bylund 1992). On the basis of these studies, three genetic and four pharmacologically distinct α2-adrenoceptor subtypes have been defined. The α2A-adrenoceptor subtype, for which prazosin has a relatively low affinity and oxymetazoline a relatively high affinity (Bylund 1988), has been cloned from humans (Kobilka et al. 1987). The second subtype, the α2B-adrenoceptor, has been identified in neonatal rat lung and in NG108 cells (Bylund et al. 1988). This subtype has a relatively high affinity for prazosin and a low affinity for oxymetazoline (Weinshank et al. 1990). A third subtype, the α2C-adrenoceptor, has been identified in an opossum kidney cell line and cloned from human kidney (Murphy and Bylund 1988; Regan et al. 1988). Although this subtype has a relatively high affinity for prazosin and a low affinity for oxymetazoline, it is pharmacologically distinct from the α2B subtype (Blaxall et al. 1991). A fourth pharmacological subtype, the α2D, has been identified in the rat salivary gland (Michel et al. 1989) and in the bovine pineal gland (Simonneaux et al. 1991) and has been cloned from the rat (Lanier et al. 1991). On the basis of the predicted amino acid sequence, the α2D is a species orthologue of the human α2A subtype, and thus, it is not considered to be a separate subtype.
The role of these subtypes as potential targets in the treatment of migraine has been elucidated in porcine and canine migraine models. Studies on these models showed that the canine carotid vascular responses to the α2-adrenoceptor agonist BHT933 were markedly attenuated by the α2A-adrenoceptor antagonist BRL44408 or the α2C-adrenoceptor antagonist MK912 (given either alone or in combination) but remained unaffected after administration of the α2B-adrenoceptor antagonist imiloxan. Figure 3 (right panel) illustrates the effect of α2-adrenoceptor subtypes in the canine carotid vascular bed (Willems et al. 2001a). Similarly, the carotid vasoconstrictor responses produced by BHT933 in anesthetized pigs were markedly attenuated by MK912, while the other antagonists were ineffective (Willems et al. 2003). These results suggest that mainly α2C-adrenoceptors mediate vasoconstriction in the carotid circulation of both species (Willems et al. 2002). We also demonstrated the functional role, as well as the mRNA of α2C-adrenoceptors, in the porcine isolated meningeal artery (Mehrotra et al. 2006). Thus, α2C-adrenoceptor agonists could be useful targets for the development of potential antimigraine drugs.
Additionally, other studies have shown the lack of response to clonidine in menstrual migraine, where the authors speculated about a postsynaptic α2-adrenoceptor hyposensitivity during the premenstrual period (Facchinetti et al. 1989). Indeed, we have demonstrated an increased function of α2-adrenoceptors in ovariectomized rats suggesting that, if this phenomenon also occurs in humans, it may contribute to the decreased frequency of migraine after menopause (Mehrotra et al. 2007). Furthermore, it has recently been reported that α2-adrenoceptors produce a specific NMDA-induced nociception in the trigeminal region in male and ovariectomized female rats, while this response was absent in female rats with circulating estrogen (Nag and Mokha 2006). Thus, a transient vulnerability of the neuroendocrine/neurovegetative systems in female migraine patients could be a factor that facilitates the precipitation of migraine attacks. Clearly, more studies are required in this direction and could possibly open new avenues for the pharmaceutical companies to develop subtype-selective agonists.
β-Adrenoceptors
In 1967, two subtypes of the β-adrenoceptor were identified by comparing the rank orders of agonist potency (Ahlquist 1967; Lands et al. 1967). The β1-adrenoceptor, the dominant receptor in heart and adipose tissue, was equally sensitive to noradrenaline and adrenaline, whereas the β2-adrenoceptor, responsible for relaxation of vascular, uterine, and airway smooth muscle, was much less sensitive to noradrenaline in comparison with adrenaline (Lands et al. 1967). Highly selective antagonists for both β1- and β2-adrenoceptors have been developed, as well as many potent and selective β2-adrenoceptor agonists. Subsequently, it has become apparent that not all β-adrenoceptor-mediated responses can be classified as either β1 or β2, suggesting the existence of at least the β3-adrenoceptor subtype (Arch et al. 1984; Bond and Clarke 1988). The β3-adrenoceptor is insensitive to the commonly used β-antagonists and has often been referred to as the ‘atypical’ β-adrenoceptor. It is unlikely that all of the atypical β-adrenoceptor responses observed have characteristics consistent with those of the β3-adrenoceptor and, hence, the possibility of additional subtypes cannot be excluded. Pharmacological evidence has been accumulated for a fourth β-adrenoceptor localized in cardiac tissues of various species (Kaumann 1997). This β4-adrenoceptor is activated with a low potency by noradrenaline and adrenaline and is blocked by β-adrenoceptor antagonists, such as bupranolol and CGP20712A (Galitzky et al. 1997; Sarsero et al. 1998).
Among all β-adrenoceptor blockers, propranolol and, to a lesser extent, metoprolol, underwent the most extensive clinical testing for cardiac disease and served in many clinical trials as reference drugs when β-adrenoceptor blockers were compared with non-adrenergic drugs (Limmroth and Michel 2001). The efficacy of β-adrenoceptor blockers for the prophylaxis of migraine was discovered by chance when patients with migraine, who received β-adrenoceptor blockers for cardiac disorders, observed a significant reduction of migraine frequency (Rabkin et al. 1966). On the other hand, it still remains controversial whether all β-adrenoceptor blockers have a prophylactic efficacy in migraine or it is limited to individual members of this drug class with specific characteristics. β-blockade results in (a) inhibition of noradrenaline release by blocking prejunctiononal β-adrenoceptors (Lakhlani et al. 1994) and (b) a delayed reduction in tyrosine hydroxylase activity, the rate-limiting step in noradrenaline synthesis, in the superior cervical ganglia (Hieble 2000). It is also suggested that lipophilicity (penetration into the central nervous system), membrane-stabilizing effects and intrinsic sympathomimetic activity are relevant for antimigraine efficacy. Moreover, some β-adrenoceptor blockers have high affinity for certain 5-HT receptor subtypes (Cruickshank and Prichard 1994). The β1-adrenoceptor affinity appears to play a major role in determining prophylactic efficacy since nonselective agents such as propranolol, moderately β1-selective agents such as metoprolol, and highly β1-selective drugs such as bisoprolol (van de Ven et al. 1997; Würz et al. 1991) all are effective prophylactics. Thus, concomitant blockade of β2-adrenoceptors does not appear to be required for effective migraine prophylaxis. While propranolol, metoprolol, oxprenolol, and alprenolol are very lipophilic and, hence, penetrate well into the central nervous system, atenolol, nadolol, and practolol are only slightly or not at all lipophilic (Cruickshank and Prichard 1994). As several members of the latter group, including atenolol (Forssman et al. 1983; Johannsson et al. 1987) and nadolol (Freitag and Diamond 1984; Sudilovsky et al. 1987), have been reported to be effective in the prophylactic treatment of migraine attacks, high lipophilicity and, hence, penetration into the central nervous system does not appear to be required for prophylactic efficacy. The reports on prophylactic efficacy of atenolol (Forssman et al. 1983; Johannsson et al. 1987), nadolol (Freitag and Diamond 1984; Sudilovsky et al. 1987), and timolol (Stellar et al. 1984; Tfelt-Hansen et al. 1984) suggest that membrane-stabilizing effects are not required to reduce the frequency of migraine attacks. Finally, it should be noted that only β-adrenoceptor antagonists without partial agonist activity are effective in the prophylactic treatment of migraine (Tfelt-Hansen and Rolan 2006).
CGRP receptors
CGRP is one of the most potent endogenous vasodilators. On the basis of pharmacological criteria, it is known that CGRP may act mainly on CGRP1 and CGRP2 receptors (Arulmani et al. 2004), with h-αCGRP8–37 being a 10-fold more potent antagonist at CGRP1 receptors than at CGRP2 receptors (Quirion et al. 1992). While CGRP1 receptors are widely distributed, CGRP2 receptors have only been described in rat vas deferens and are more sensitive to the linear agonists [ethylamide-Cys2,7]h-αCGRP and [acetimidomethyl-Cys2,7]h-αCGRP than CGRP1 receptors (Dumont et al. 1997). CGRP1 receptors consist of at least three main different entities, namely, the calcitonin receptor-like receptor (CLR), receptor-activity-modifying protein-1 (RAMP-1; McLatchie et al. 1998), and receptor component protein (RCP; Luebke et al. 1996; Poyner et al. 2002), whereas CGRP2 receptors have not yet been molecularly characterized. The molecular components of CGRP1 receptors that have been demonstrated in the human meningeal artery include CLR, RCP, and RAMPs 1, 2, and 3 (Durham 2004; Gupta et al. 2006a; Jansen-Olesen et al. 2003; Oliver et al. 2002). The results from our laboratory also advocate the presence of CGRP1 receptors in human meningeal (Gupta et al. 2006a) and coronary (Gupta et al. 2006b) arteries, while in human distal coronary artery, there seems to be an additional population of CGRP receptors not complying with the current classification of CGRP1 or CGRP2 receptors (Gupta et al. 2006b). Furthermore, RAMP-1 seems to be functionally rate limiting for CGRP receptor activity in the trigeminal ganglion, suggesting that the increase in function of RAMP-1 might sensitize some individuals to the actions of CGRP in migraine (Zhang et al. 2007).
In the recent past, there has been an upsurge in CGRP research and its notable role in migraine pathophysiology. CGRP immunoreactive fibers originating in the trigeminal ganglion innervate cranial blood vessels (Uddman et al. 1985). In animals, stimulation of these sensory nerve fibers has been shown to cause antidromic release of CGRP and subsequent vasodilatation in the cranial vasculature (Brain and Grant 2004; Goadsby et al. 1988). Indeed, CGRP induces a concentration-dependent relaxation in the middle cerebral artery in a pressurized arteriography model in rats only when CGRP was administered abluminally. This suggests that CGRP-mediated vasodilatation is not mediated by luminally situated receptors but by receptors on the smooth muscle cells (Petersen et al. 2005a). Moreover, CGRP receptor antagonists could also act at a central level, as exemplified by the fact that it modulates nociceptive trigeminovascular transmission in the cat (Storer et al. 2004a). Hence, inhibition of CGRP release or antagonism of CGRP receptors could be a viable therapeutic target for the pharmacological treatment of migraine (Edvinsson 2004).
Further evidence for a role of CGRP in migraine is provided by the observations that plasma concentrations of CGRP, but not of other neuropeptides, in the jugular venous blood are elevated during the headache phase of migraine (Edvinsson and Goadsby 1994). Furthermore, in migraine patients, (a) a strong correlation was found between plasma CGRP concentrations and migraine headache as the changes in plasma CGRP levels during migraine attacks significantly correlated with the headache intensity (Durham 2004; Iovino et al. 2004; Petersen et al. 2005b); (b) infusion of CGRP produced a migraine-like headache (Olesen et al. 2004); and (c) baseline CGRP levels were increased in migraineurs (Fusayasu et al. 2007).
An important breakthrough in the field of CGRP was the development of the potent and selective CGRP receptor antagonist olcegepant (BIBN4096BS; Doods et al. 2000). In in vivo animal models of migraine, olcegepant attenuated the vasodilation induced by trigeminal stimulation and capsaicin-induced carotid arteriovenous anastomotic dilatation (Doods et al. 2000; Edvinsson 2004; Kapoor et al. 2003; Petersen et al. 2005b). In addition, olcegepant has been shown to prevent CGRP-induced headache and extracerebral vasodilatation (Petersen et al. 2005b) but does not significantly affect the induced cerebral hemodynamic changes (Fig. 4). Data from a clinical proof-of-concept study demonstrate the effectiveness of olcegepant in the acute treatment of migraine, with the response rate being similar to oral triptans (Olesen et al. 2004). These lines of evidence are in accordance with recent findings in a larger, ramdomized controlled trial of the orally available CGRP receptor antagonist MK-0974 (Ho et al. 2008), which, similar to olcegepant, is a potent antagonist of the human CGRP receptors (Salvatore et al. 2008). Since olcegepant does not induce vasoconstriction per se, this CGRP receptor antagonist has been argued to be safer than triptans, particularly in migraineurs suffering from cardiovascular pathologies. However, it must be highlighted that CGRP has a protective function during coronary ischemia, which was blocked by olcegepant in a Langendorff rat heart model (Chai et al. 2006). Thus, if these findings hold for humans as well, CGRP receptor antagonists, like the triptans, may also be contraindicated in patients with coronary artery disease.
Diameter of superficial temporal (squares) and radial (circles) arteries after treatment with placebo (open symbols) or olcegepant (2.5 mg, closed symbols) measured by high-frequency ultrasound in ten healthy volunteers in double-blind, placebo-controlled crossover study. Asterisks denote significant difference (P < 0.05) between pretreatment with placebo and olcegepant on human α-calcitonin gene-related peptide (h-αCGRP)-induced vasodilatation (Petersen et al. 2005b)
Adenosine receptors
Adenosine is present in all body fluids and it differs from ATP in that it is not stored by and released from secretory vesicles. Rather, it exists freely in the cytosol of all cells and is transported in and out of cells mainly via membrane transporters. Adenosine in tissues comes partly from membrane transporters and partly from released ATP or ADP. Adenosine produces many pharmacological effects, both in the periphery and in the central nervous system (Brundege and Dunwiddie 1997). One of its functions appears to be as a protective agent when tissues are threatened (e.g., cardiac or cerebral ischemia), based on its ability to inhibit cell functions and thus minimize the metabolic requirements of the cells. Under less extreme conditions, variations in the adenosine release may play a role in controlling blood flow, matching it to the metabolic needs of the tissue. Adenosine acts on four well-defined G-protein-coupled receptors. These receptors are denoted as adenosine receptors but may also be called P1-receptors to distinguish them from the receptors for nucleotides, which belong either to the family of transmitter-gated ion channels (P2X receptors) or the family of G-protein-coupled receptors (P2Y receptors). The P1 receptors are classified as four adenosine receptors, called A1, A2A, A2B, and A3, which have been cloned from several mammalian species, including humans (Fredholm et al. 2001). Several studies on knockout and transgenic mice have shown various roles of each of these subtypes (IUPHAR 2006).
Whereas adenosine A2 receptor gene variation may contribute to the pathogenesis of migraine with aura (Hohoff et al. 2007), adenosine A1 receptor agonists such as GR79236 seem to have a role in inhibiting trigeminal nociception in humans (Giffin et al. 2003) and could therefore be useful in the treatment of migraine. In the cat, GR79236 induced neuronal inhibition without concomitant vasoconstriction (Goadsby et al. 2002b). In the rat, the adenosine A1 receptor antagonist DPCPX prevented the inhibitory effect of GR79236 on neurogenic vasodilatation, which was primarily mediated by prejunctional A1-receptors (Honey et al. 2002). GR79236 has no effect on resting meningeal artery diameter in rats (Honey et al. 2002) and inhibits forskolin-stimulated CGRP release in rats (Carruthers et al. 2001). Likewise, in cats, GR79236 has been shown to significantly reduce the CGRP levels in the external jugular vein (Fig. 5; Goadsby et al. 2002b). However, in pigs, GR79236 has no effect on capsaicin-induced CGRP release (Arulmani et al. 2005), and, consequently, the authors concluded that the antimigraine potential of GR79236 could be due to its postjunctional effects (carotid vasoconstriction) rather than to prejunctional inhibition of trigeminal CGRP release. Thus, although the underlying mechanisms have not yet completely been elucidated, there is evidence that adenosine receptor agonists may be beneficial in the treatment of migraine via neuronal or vascular effects. In view of the latter effects, adenosine receptor stimulation may lead to delayed Ca2+ uptake and could, hence, contribute to a delayed cardioprotective effect of adenosine (Ghelardoni et al. 2005), which may have implications for the cardiovascular safety of these compounds.
Cranial CGRP release in anesthetized cats under basal conditions (control), after stimulation of the superior sagittal sinus (SSS), and after SSS in animals pretreated with the adenosine A1 receptor agonist GR79236 (30 μg/kg, i.v.). #P < 0.05 compared to control; *P < 0.05 compared to SSS (Goadsby et al. 2002b)
ATP and its breakdown products adenosine monophosphate and adenosine are potent dilatators of cerebral blood vessels. During ischemia, ATP binding to metabotropic P2Y-receptors on endothelial cells results in release of NO, which diffuses to the vascular smooth muscles causing vasodilatation and hyperemia (Burnstock 2000). Additionally, ATP contributes to pain in migraine by activating nociceptive terminals of primary afferents located near the basal cerebral and dural vasculature where P2X-receptor subtypes, which are sensitive to the lowered extracellular pH, are suggested to be responsible for excitatory effects on trigeminal sensory neurons (Cook and McCleskey 1997; Cook et al. 1997; Hamilton and McMahon 2000). Furthermore, Zimmermann et al. (2002) showed that ATP (a) has a poor, if any, direct CGRP releasing effect on trigeminal nerve endings in the dura; (b) may contribute to pain in migraine by facilitating nociceptor responses to tissue acidosis via the P2Y-receptor; and (c) may involve release of endogenous prostaglandins. Recently, P2X3-receptors have been shown to be upregulated in trigeminal neurons by CGRP; thus, this mechanism might contribute to pain sensitization and could represent a model of neuronal plasticity in response to a migraine mediator (Fabbretti et al. 2006). Therefore, further research in migraine should focus on the role of P2-receptors, their subtypes, and how they are implicated in migraine pathophysiology.
Glutamate receptors
Glutamate and its receptors play a major excitatory role in the brain (for references, see Cyr et al. 2001). The effects of glutamate on brain excitability are mediated via the ionotropic NMDA, AMPA, and kainate receptors, as well as the metabotropic glutamate receptor (Sang et al. 2004). Glutamate-like immunoreactivity has been seen in the dental pulp neurons that project to the trigeminal nucleus caudalis (TNC) in the rat (Clements et al. 1991). Indeed, all the major receptor classes of glutamate have been identified in the superficial lamina of the rat trigeminal nucleus caudalis (Tallaksen-Greene et al. 1992). Stimulation of the trigeminal nerve increases extracellular glutamate, which in turn excites TNC neurons (Quartu et al. 2002; Sahara et al. 1997). As glutamate receptors are co-localized in neurons in the trigeminal ganglion with 5-HT1B, 5-HT1D, and 5-HT1F receptors, 5-HT1 autoreceptors may presynaptically inhibit the release of glutamate (Ma 2001). Since glutamate may be involved in the cortical hyperexcitability typical of migraine (Goadsby 2005), the above ionotropic glutamate receptors are being studied as potential antimigraine targets (Sang et al. 2004).
The NMDA receptor antagonist MK-801 and the AMPA receptor antagonist GYKI-52466 are effective in blocking trigeminovascular nociception in the trigeminocervical nucleus (Classey et al. 2001; Goadsby and Classey 2000; Storer and Goadsby 1999). In addition, the NMDA receptor antagonists MK-801 and AP-5 reduce capsaicin-evoked CGRP release (Garry et al. 2000), pointing to potential vascular effects of glutamate receptor antagonists (Jackson and Hargreaves 1999).
Blockade of both NMDA and non-NMDA ionotropic receptors reduces the c-fos protein expression in the trigeminal nucleus caudalis after intracisternal capsaicin injection (Mitsikostas et al. 1999; Mitsikostas et al. 1998). Indeed, the mixed AMPA/kainate receptor antagonist LY293558 has been shown to be effective in the acute treatment of migraine (Sang et al. 2004). Also lamotrigine, a sodium channel blocker with antiglutamatergic actions, seemed highly effective in reducing migraine aura and migraine attacks in a controlled open study (Lampl et al. 2005). Similarly, the anticonvulsant topiramate is effective in migraine prophylaxis (Brandes et al. 2004; Diener et al. 2004; Silberstein et al. 2004). This effect may be mediated by blockade on voltage-activated Na+ and Ca2+ channels and/or blockade of AMPA and kainate receptors.
Interestingly, patients taking nitroglycerin for reducing the risk of developing cardiac ischemia or infarction often complain of headache. In these patients, infusion of ketamine, a NMDA receptor antagonist, in concurrence with fentanyl for postoperative pain relief, was proposed to be effective against this NO-induced headache (Roffey et al. 2001). Moreover, in a small open-label study, intranasal ketamine was reported to reproducibly reduce the severity and duration of the neurologic deficits due to the aura in five out of 11 patients with familial hemiplegic migraine (FHM; Kaube et al. 2000). Remarkably, in a subpopulation of patients with FHM, a mutation in the gene encoding for the glutamate transporter, which decreases the expression of the transporter, has been reported (Jen et al. 2005). This mutation may increase the levels of glutamate, leading to cortical hyperexcitability. On the other hand, there is ample evidence, both from basic and clinical studies, that decreased concentrations of ionized magnesium (Mg2+) are associated with a decreased threshold for triggering a migraine attack (Mody et al. 1987; Ramadan et al. 1989; Sarchielli et al. 1992). Decreased Mg2+ concentrations also can activate NMDA receptors and, thus, can increase neuronal excitability. In agreement with this hypothesis, the infusion of Mg2+ provided sustained headache relief (Bigal et al. 2002), and oral Mg2+ has been demonstrated to be an effective prophylactic in menstrual migraine (Facchinetti et al. 1991). Thus, glutamate receptor modulators seem to be of benefit in migraine treatment; indeed, the NMDA receptor antagonist memantine and the NR2B subunit containing antagonist, CP-101,606, decreased spreading depression (Peeters et al. 2007), a potentially important factor in migraine pathophysiology. However, stronger basic and clinical evidence for the delineation of their exact role in the pathogenesis of migraine, as well as their cardiovascular safety, is awaited with great interest.
Dopamine receptors
Dopamine is a catecholamine that serves as a neurotransmitter in the brain (Carlsson et al. 1957; Carlsson et al. 1958). Dopamine is synthesized from tyrosine, which is sequentially converted to l-dihydroxyphenylalanine (l-DOPA) by the enzyme tyrosine hydroxylase. l-DOPA is then converted to dopamine in cytoplasm by the enzyme DOPA decarboxylase (Hoffman 2001). The distribution of dopamine in the brain is highly non-uniform and more restricted than the distribution of noradrenaline. A large proportion of the dopamine content in the brain is found in the corpus striatum and the limbic system. Dopaminergic neurons lack dopamine β-hydroxylase and thus do not produce noradrenaline. Pharmacological evidence suggests that dopaminergic neurons have a role in the production of nausea and vomiting. Dopamine exerts its action by five receptor subtypes that have been cloned. The D1-like receptors (D1 and D5) are closely related G-protein-coupled receptors (Gsα-protein subunit) that stimulate adenylyl cyclase activity. In contrast, D2-like receptors (D2, D3, and D4) are coupled to Giα-protein subunits with a similar pharmacology and inhibit the formation of cAMP. Their isoforms are encoded by homologous genes displaying several introns (Alexander et al. 2007).
The vascular and nervous systems, both likely to be involved in migraine pathophysiology, both respond to dopamine (Akerman and Goadsby 2007). Dopamine and related receptor agonists have vasoactive effects on blood vessels in vitro and in vivo, inducing vasoconstriction or vasodilatation, depending on the species, vascular bed, and dose (Hughes et al. 1986; Smith et al. 1990; Takenaka et al. 1993; Villalón et al. 2003; Yu et al. 2002).
The dopamine agonist lisuride is useful in the prophylaxis of migraine (Del Bene et al. 1983; Herrmann et al. 1978; Somerville and Herrmann 1978), although its exact mechanism of action is still to be unraveled. As lisuride is an extremely potent 5-HT2B receptor antagonist (Hofmann et al. 2006), it is reasonable to assume that the antimigraine action of this drug could be mediated, at least partly, via blockade of 5-HT2B receptors. More recently, haloperidol, which blocks D1, D2, 5-HT2, H1, and α2-adrenergic receptors in the brain, was reported to be effective in the acute treatment of migraine in a randomized, double-blind, placebo-controlled study, although the majority of patients suffered from side effects (Honkaniemi et al. 2006). Dopamine causes vasoconstriction in rat dural arteries, but this effect is most likely mediated by α2-adrenoceptors and not dopamine receptors (Akerman and Goadsby 2005). In addition, dopamine-containing neurons may play a role in modulating trigeminovascular nociception; when dopamine was administered microiontophoretically (and not intravenously), it inhibited the activation of trigeminocervical neurons in response to middle meningeal artery stimulation (Bergerot et al. 2007). Furthermore, pharmacological studies with dopaminergic agonists like apomorphine suggest that migraineurs may present a dopaminergic hypersensitivity, even interictally (Blin et al. 1991; Cerbo et al. 1997; Peroutka 1997). The increased density of D5, D3, and D4 receptors in blood lymphocytes in migraine patients may reflect the dopaminergic hypersensitivity and may thus represent a relatively simple and reliable peripheral marker of altered dopaminergic function (Barbanti et al. 1996; Barbanti et al. 2000). In addition, high platelet levels of dopamine have been observed in migraineurs (D’Andrea et al. 2006). Several association studies on D2-like receptors and migraine with or without aura have been reported, but with contradictory results (Maude et al. 2001; Mochi et al. 2003; Peroutka et al. 1998; Peroutka et al. 1997). Thus, it appears that if dopamine and its receptors are at all involved in the pathophysiology of migraine, the exact mechanism of action still remains unclear.
Endothelin receptors
Endothelin was identified by Yanagisawa et al. (1988), who isolated, analyzed, and cloned the gene of this potent vasoconstrictor in a very short space of time. There are three isoforms of endothelin, namely, ET-1, ET-2, and ET-3, which are variably distributed and derived from separate genes. ET-1 is the main isoform and is produced in the cardiovascular system, ET-2 is mainly produced in the kidney and intestines, whereas ET-3 is predominant in the central nervous system. ET-1 mediates its action through binding to specific G-protein-coupled receptors, ETA and ETB. ETA receptors are mainly present in vascular smooth muscle and mediate vasoconstriction and cell proliferation, whereas activation of ETB receptors present in endothelial cells causes NO-induced vasodilatation and prostacyclin release (Attina et al. 2005).
Increased peripheral plasma levels of ET-1 (Hasselblatt et al. 1999; Kallela et al. 1998), even several hours after a migraine attack (Farkkila et al. 1992), led to suggest the involvement of ET-1 in migraine pathogenesis. Evidence of association of migraine and the ETA receptor gene polymorphism (ETA-231 A/G) in a French population-based study (Tzourio et al. 2001) has added a new candidate gene for migraine. In rats, ET-1 is one of the most potent inducers of Leão’s spreading depression (Dreier et al. 2002), but Goadsby et al. (1996) reported no effect of endothelin receptor antagonists in preventing spreading depression in cats. The major setback for the hypothesis of involvement of ET-1 in migraine pathogenesis comes from a study showing the lack of efficacy of the mixed ETA/ETB receptor antagonist bosentan in migraine (May et al. 1996). However, the ETA and ETB receptors are likely to mediate opposite effects, and it is feasible that more selective endothelin receptor antagonists may be effective in the acute treatment of migraine. In addition, the efficacy of endothelin receptor antagonists in migraine prophylaxis is still to be evaluated.
Female sex hormone (estrogen and progesterone) receptors
The female sex steroid hormones estrogen and progesterone regulate numerous biological functions via two main mechanisms, which are mediated by genomic (transcription-dependent) and/or non-genomic (transcription independent) pathways (Kelly and Levin 2001; Lau 2002; Orshal and Khalil 2004). Ovarian steroids are lipophilic in nature, and their low molecular weight allows them to cross the blood–brain barrier by passive diffusion (Aloisi 2003). In the central nervous system, these hormones induce a wide array of physiological effects.
The genomic actions of sex steroids encompass two different receptors (ERα and ERβ) for estrogens (Enmark and Gustafsson 1999), as well as two receptors (PR-A and PR-B) for progesterone (Kastner et al. 1990). While female sex steroids do not seem to be involved in the pathogenesis of migraine per se, they may modulate several mediators and/or receptor systems via both genomic and non-genomic mechanisms. These actions may be perpetuated at the central nervous system, as well as at the peripheral (neuro) vascular level (Gupta et al. 2007). The receptors of both estrogen and progesterone alter receptor expression and release, as well as synthesis of various neurotransmitters and hormones. For example, CGRP, a facilitator of pain transmission and a potent vasodilator (Bennett et al. 2000; Powell et al. 2000), neuropeptide Y, a regulator of inflammation and central nociception (Silva et al. 2002), as well as the neurotransmitters glutamate (Zhang and Bhavnani 2005), and 5-HT (Smith et al. 2004) have been reported to be genomically modulated by sex steroids. Remarkably, progesterone can act in a synergistic, antagonistic, or neutral manner compared to the effects of estrogens (Attali et al. 1997; Becker and Rudick 1999; Dluzen and Ramírez 1989; Fernández-Ruíz et al. 1990; Hernández et al. 1991). The receptors and mechanisms involved in their non-genomic action are not yet completely deciphered (Gupta et al. 2007; Martin and Behbehani 2006).
Primary evidence for the involvement of female sex hormones in migraine pathogenesis comes from the facts that the prevalence of migraine is 2–3-fold higher in women than in men (Lipton et al. 2001; Stewart et al. 1992) and that reproductive milestones such as menarche, pregnancy, and menopause are associated with changes in migraine frequency and/or severity (Silberstein 2000). Interestingly, individuals with a polymorphism at G594 (exon 8) of the estrogen receptor-1 (ESR1) gene are twice more likely to suffer from migraine than those with the wild-type gene (Colson et al. 2004). Similarly, individuals carrying the PROGINS inserts of the progesterone receptor gene polymorphism are twice as likely to suffer from migraine than control subjects (Colson et al. 2005). It is worth mentioning that the estrogen receptor polymorphism increases its expression (Colson et al. 2004), whereas the progesterone receptor polymorphism negatively impacts its expression. Furthermore, it is interesting that the PROGINS allele of the progesterone receptor acts synergistically with the 594A allele of ESR1 to increase the risk of migraine by 3.2 times (Colson et al. 2005).
Hormonal interventions have been explored as a prophylactic treatment of menses-related migraine or migraine experienced during the pill-free period. Oral estrogens (Calhoun 2004; Somerville 1975) and percutaneous estradiol showed benefit during perimenstrual treatment, which was balanced when delayed by estrogen withdrawal, triggering post-dosing migraine immediately after the gel was stopped (MacGregor et al. 2006a). Furthermore, rising levels of estrogen appear to offer some protection against migraine (MacGregor et al. 2006b). Thus, estrogen patches have been utilized to prevent the rapid decline of estrogen levels during the menstrual cycle (MacGregor 2006; MacGregor et al. 2006a; MacGregor et al. 2006b; MacGregor and Hackshaw 2002; Magos et al. 1983), which is thought to be the main trigger of migraine in these patients (MacGregor 2006). These studies have reported mixed results ranging from no improvement to 80% improvement and are also based on a relatively limited number of patients (n = 11–38). Taken collectively, there is a strong evidence for the involvement of female sex steroids, especially that of estrogens, but the therapeutic role of estrogen supplements for conditions like menstrual migraine remains to be established.
Miscellaneous receptors and ion channels
GABA receptors
Gamma-aminobutyric acid (GABA) is the major inhibitory neurotransmitter in the mammalian central nervous system. GABA induces inhibitory hyperpolarization effects in neurons, although excitatory responses can be found at certain loci in embryonic and postnatal life, as well as in adult hippocampal pyramidal neurons. GABA exerts its effects through GABAA and GABAB receptors. GABAA receptors are ligand-gated ion channels sensitive to bicuculline (Barnard et al. 1998), whereas GABAB receptors are G-protein-coupled receptors insensitive to bicuculline and stimulated by baclofen (Bowery et al. 2002). Also, GABAC receptors, which are insensitive to bicuculline, benzodiazepines, or barbiturates, have been described, but these receptors are not yet completely characterized (Barnard et al. 1998; Spedding et al. 2002).
GABA may be involved in the pathophysiology of migraine since (a) increased GABA concentrations in cerebrospinal fluid have been reported during a migraine attack (Welch et al. 1975); (b) increased platelet levels of GABA have been observed in patients with tension-type headache (Kowa et al. 1992), although it should be kept in mind that the pathophysiology of migraine and tension-type headache are obviously different; and (c) sodium valproate and muscimol dose dependently inhibit plasma protein extravasation induced by electrical stimulation of the trigeminal ganglion, and these effects are blocked by the GABAA receptor antagonist bicuculline (Lee et al. 1995). It thus appears that selective agonists of GABAA receptors could be clinically effective in the treatment of migraine. Consistent with this view, several agonists at GABA receptors have been used as prophylactic antimigraine drugs. In this context, valproate (Cutrer et al. 1997a; Shaygannejad et al. 2006), baclofen in a small open study (Hering-Hanit 1999), and gabapentin (Di Trapani et al. 2000) may prevent migraine attacks, while valproate has also been suggested to be effective in the acute treatment of migraine in another small open trial (Mathew et al. 2000). Despite the above clinical evidence, it should be kept in mind that not all of the aforementioned compounds are selective in their action at GABA receptors, and the mechanisms involved in their antimigraine effect remain unclear. Several studies have shown that valproate inhibits GABA transaminase and activates glutamic acid decarboxylase to increase brain GABA levels. Moreover, GABA may suppress the hyperexcitability observed in aura (Palmer et al. 2000), probably by blocking Na+ and/or Ca2+ channels (Cutrer 2001). Recently, it has been suggested that GABAA receptors can inhibit trigeminovascular nociceptive transmission in the cat (Storer et al. 2004b). These findings suggest that the development of more selective GABAA receptor agonists may be fruitful in the treatment of migraine.
Angiotensin receptors
Angiotensin II is an octapeptide derived from angiotensinogen. Angiotensinogen, released from the liver, is converted to angiotensin I by renin released by the kidney. Then, angiotensin I is converted by angiotensin converting enzyme (ACE), mainly located in the lungs, to angiotensin II. Angiotensin II activates two receptor types, AT1 and AT2. The AT1 receptor is involved in the regulation of arterial blood pressure (vasoconstriction), electrolyte balance (anti-natriuresis), thirst, hormone secretion (aldosterone), and renal function (De Gasparo et al. 2000). In contrast, AT2 receptors can produce opposite effects to those by the AT1 receptor, i.e., natriuresis and vasodilatation (Widdop et al. 2003).
Although the role of angiotensin II in the pathogenesis of migraine is not established, clinical evidence suggests that several ACE inhibitors such as lisinopril and enalapril can be effective in migraine (Bender 1995; Schrader et al. 2001). Moreover, the angiotensin AT1 receptor antagonist candesartan (Tronvik et al. 2003) also seems to be effective as prophylactic antimigraine drug, which may be generalized to other drugs from the same class as suggested by an open-label study in 24 patients using olmesartan (Charles et al. 2006). In addition, genetic studies suggest an association between ACE gene polymorphisms and migraine (Paterna et al. 2000). Further, ACE activity in migraine with aura is reported to be significantly higher than in migraine without aura and control subjects (Fusayasu et al. 2007). Despite the above evidence, the role of angiotensin II in the pathophysiology of migraine should be clarified in animal models to understand the mechanism(s) of action involved. This could be useful to rationally develop more selective antimigraine drugs interacting with the renin–angiotensin system.
Bradykinin receptors
The nonapeptide bradykinin belongs to the kinin family and is synthesized by cleavage of high and low molecular weight kininogens through serine proteases (kininogenases; Moreau et al. 2005). Plasma and tissue kallikrein are the two main kininogenases. Once released, bradykinin can activate two main receptors (B1 and B2), which are G-protein-coupled and linked to activation of phospholipase C (Marceau and Regoli 2004). The B1 receptor is generally induced during inflammation by lipopolysaccharide and cytokines such as interleukin-1β, interleukin-6, and tumor necrosis factorα, while the B2 receptor is constitutive and widely distributed in blood vessels. B1-receptor-mediated effects include vasodilatation, plasma protein extravasation, inflammatory pain, activation of leukocyte-endothelial cell interactions, and leukocyte accumulation.
Bradykinin is involved in inflammatory responses and locally induces release of NO and PGI2 (prostacyclin) from the endothelium, as well as substance P and CGRP from neurones. Although this peptide could be involved in neurogenic inflammation during a migraine attack (Geppetti et al. 1990), its precise role in migraine pathophysiology is not well established. Since B1 receptors are expressed following noxious stimuli and mediate vasodilatation and neurogenic plasma extravasation, B1-receptor antagonists may be useful as antimigraine drugs. Moreover, several B2-receptor antagonists have analgesic properties (Moreau et al. 2005), which could be explained by the capability of bradykinin to stimulate primary afferent nerves during inflammation. Thus, both B1- and B2-receptor antagonists might potentially be useful in the treatment of migraine.
Histamine receptors
Histamine is a monoamine mainly stored in mast cells in most tissues. Histamine plays an important role on allergic responses and in the central nervous system as a neurotransmitter. The effects of histamine are mediated by four receptors (H1, H2, H3, and H4). The H1 receptor is positively coupled to phospholipase C and mediates, among other effects, smooth muscle contraction, release of NO, and increased vascular permeability. The H2 receptor stimulates adenylyl cyclase and produces smooth muscle relaxation, positive inotropic and chronotropic effects in the heart, and stimulation of gastric secretion. The H3 and H4 receptors are both G-protein-coupled receptors mediating inhibition of adenylyl cyclase, but much of their functional role remains to be determined (IUPHAR 2006).
Clinical evidence has suggested that histamine is involved in the pathogenesis of migraine. Intravenous infusion of histamine induces headache, which is blocked by the H1 receptor antagonist, mepyramine (Lassen et al. 1995). This effect of histamine could be due to activation of endothelial H1 receptors that release NO (Lassen et al. 1996). Consistent with these views, histamine produces rat dural vasodilatation, which is sensitive to mepyramine (H1 antagonist), famotidine (H2 antagonist), and l-NAME, an NO synthase inhibitor (Akerman et al. 2002). In addition, clinical studies indicate that the histamine metabolite and H1/2/3 receptor agonist, N-α-methyl-histamine (Hill et al. 1997), can be used as a prophylactic antimigraine drug (Millán-Guerrero et al. 2006; Millán-Guerrero et al. 2003). N-α-methyl-histamine can block the plasma protein extravasation induced by electrical trigeminal ganglion stimulation (Matsubara et al. 1992) or by capsaicin in rats and guinea pigs. Moreover, the selective H3 receptor agonist (R)-α-methyl-histamine inhibits capsaicin-induced dural plasma extravasation in the rat (Rouleau et al. 1997). Taken together, it appears that antagonists at H1/2 receptors or agonists at H3 receptors could be useful as acute and/or prophylactic antimigraine drugs.
Ion channels
Recently, knowledge on the role of mutant ion channels in the pathogenesis of episodic neurological disorders has emerged (Hanna 2006). Molecular characteristics of genetic channelopathies have contributed to a better understanding of episodic diseases such as migraine, where new mutations in the P/Q-type voltage-gated Ca2+ channel gene CACNA1A, the Na+ /K+-ATPase gene ATP1A2, as well as the Na+ channel gene SCN1A have been demonstrated in FHM (for review, see van den Maagdenberg et al. 2007). Ion concentrations may modulate vascular constriction and relaxation, as well as cortical excitability. For example, decreased Mg2+ concentrations are associated with cortical spreading depression in animals (Mody et al. 1987). Indeed, there is evidence for low Mg2+ levels in brain during (Ramadan et al. 1989) and between (Lodi et al. 1997) migraine attacks. As mentioned above, Ca2+ seems to be involved in the pathogenesis of migraine as mutations in P/Q-type Ca2+ channels are related to FHM (Ophoff et al. 1996) and, possibly, also to migraine with and without aura (Terwindt et al. 2001). Further, L-type Ca2+ channels modulate the release of CGRP in trigeminal neurons innervating the cranial vasculature (Akerman et al. 2003). Ca2+ channel blockers such as verapamil (Ramadan et al. 1997) and flunarizine (Buchanan et al. 2004) are used for the prophylactic treatment of migraine. However, the mechanism of action of these Ca2+ channel blockers is yet poorly understood.
Implications, future directions, and conclusions
Disregarding the limitations of basic research, a multidisciplinary approach encompassing both basic and clinical observations will inevitably be needed to understand the role of different receptor systems in migraine. As the pathophysiology of migraine has not yet been completely deciphered, experimental models employed in migraine research are based on only a few symptoms observed in the clinical situation. Thus, there is a need to integrate several neuronal and vascular experimental models, as well as clinical observations in migraine research. To investigate the involvement of certain receptors in migraine, multiple agonists and antagonists should be used.
In view of the concern about coronary vasoconstriction induced by vasoactive antimigraine drugs and stimulated by the discovery of genetic ion channel abnormalities in migraine, research has recently focused on the development of neuronally acting antimigraine drugs. More knowledge on the mechanism of action of these (prospective) neuronally active antimigraine drugs may substantially contribute to the (prophylactic) treatment of migraine. On the other hand, many of these drugs are likely to exert (indirect) vascular effects as well, which may contribute to the therapeutic efficacy but also may lead to cardiovascular side effects.
In conclusion, the results obtained with various (pre)clinical models studying the targets mentioned in the present review, such as CGRP receptor antagonists, adenosine receptor agonists, and glutamate receptor antagonists, are eagerly awaited and will undoubtedly shed further light on the pathophysiology of migraine.
References
Ahlquist RP (1967) Development of the concept of alpha and beta adrenotropic receptors. Ann N Y Acad Sci 139:549–552
Akerman S, Goadsby PJ (2005) The role of dopamine in a model of trigeminovascular nociception. J Pharmacol Exp Ther 314:162–169
Akerman S, Goadsby PJ (2007) Dopamine and migraine: biology and clinical implications. Cephalalgia 27:1308–1314
Akerman S, Williamson DJ, Hill RG, Goadsby PJ (2001) The effect of adrenergic compounds on neurogenic dural vasodilatation. Eur J Pharmacol 424:53–58
Akerman S, Williamson DJ, Kaube H, Goadsby PJ (2002) The role of histamine in dural vessel dilation. Brain Res 956:96–102
Akerman S, Williamson DJ, Goadsby PJ (2003) Voltage-dependent calcium channels are involved in neurogenic dural vasodilatation via a presynaptic transmitter release mechanism. Br J Pharmacol 140:558–566
Alexander SP, Mathie A, Peters JA (2007) Guide to receptors and channels, 2nd edition (2007 revision). Br J Pharmacol 150(Suppl 1):S1
Aloisi AM (2003) Gonadal hormones and sex differences in pain reactivity. Clin J Pain 19:168–174
Anthony M, Lance JW (1989) Plasma serotonin in patients with chronic tension headaches. J Neurol Neurosurg Psychiatry 52:182–184
Anthony M, Hinterberger H, Lance JW (1967) Plasma serotonin in migraine and stress. Arch Neurol 16:544–552
Arch JR, Ainsworth AT, Cawthorne MA, Piercy V, Sennitt MV, Thody VE, Wilson C, Wilson S (1984) Atypical β-adrenoceptor on brown adipocytes as target for anti-obesity drugs. Nature 309:163–165
Arulmani U, MaassenVanDenBrink A, Villalón CM, Saxena PR (2004) Calcitonin gene-related peptide and its role in migraine pathophysiology. Eur J Pharmacol 500:315–330
Arulmani U, Heiligers JPC, Centurión D, Garrelds IM, Villalón CM, Saxena PR (2005) Lack of effect of the adenosine A1 receptor agonist, GR79236, on capsaicin-induced CGRP release in anaesthetized pigs. Cephalalgia 25:1082–1090
Arulmani U, Gupta S, MaassenVanDenBrink A, Centurión D, Villalón CM, Saxena PR (2006) Experimental migraine models and their relevance in migraine therapy. Cephalalgia 26:642–659
Attali G, Weizman A, Gil-Ad I, Rehavi M (1997) Opposite modulatory effects of ovarian hormones on rat brain dopamine and serotonin transporters. Brain Res 756:153–159
Attina T, Camidge R, Newby DE, Webb DJ (2005) Endothelin antagonism in pulmonary hypertension, heart failure, and beyond. Heart 91:825–831
Barbanti P, Bronzetti E, Ricci A, Cerbo R, Fabbrini G, Buzzi MG, Amenta F, Lenzi GL (1996) Increased density of dopamine D5 receptor in peripheral blood lymphocytes of migraineurs: a marker for migraine? Neurosci Lett 207:73–76
Barbanti P, Fabbrini G, Ricci A, Pascali MP, Bronzetti E, Amenta F, Lenzi GL, Cerbo R (2000) Migraine patients show an increased density of dopamine D3 and D4 receptors on lymphocytes. Cephalalgia 20:15–19
Barnard EA, Skolnick P, Olsen RW, Mohler H, Sieghart W, Biggio G, Braestrup C, Bateson AN, Langer SZ (1998) International Union of Pharmacology. XV. Subtypes of gamma-aminobutyric acidA receptors: classification on the basis of subunit structure and receptor function. Pharmacol Rev 50:291–313
Barnes NM, Sharp T (1999) A review of central 5-HT receptors and their function. Neuropharmacology 38:1083–1152
Becker JB, Rudick CN (1999) Rapid effects of estrogen or progesterone on the amphetamine-induced increase in striatal dopamine are enhanced by estrogen priming: a microdialysis study. Pharmacol Biochem Behav 64:53–57
Bender WI (1995) ACE inhibitors for prophylaxis of migraine headaches. Headache 35:470–471
Bennett AD, Chastain KM, Hulsebosch CE (2000) Alleviation of mechanical and thermal allodynia by CGRP(8–37) in a rodent model of chronic central pain. Pain 86:163–175
Bergerot A, Storer RJ, Goadsby PJ (2007) Dopamine inhibits trigeminovascular transmission in the rat. Ann Neurol 61:251–262
Bigal ME, Bordini CA, Tepper SJ, Speciali JG (2002) Intravenous magnesium sulphate in the acute treatment of migraine without aura and migraine with aura. A randomized, double-blind, placebo-controlled study. Cephalalgia 22:345–353
Blaxall HS, Murphy TJ, Baker JC, Ray C, Bylund DB (1991) Characterization of the α2C- adrenergic receptor subtype in the opossum kidney and in the OK cell line. J Pharmacol Exp Ther 259:323–329
Blin O, Azulay JP, Masson G, Aubrespy G, Serratrice G (1991) Apomorphine-induced yawning in migraine patients: enhanced responsiveness. Clin Neuropharmacol 14:91–95
Boccuni M, Alessandri M, Fusco BM, Cangi F (1989) The pressor hyperresponsiveness to phenylephrine unmasks sympathetic hypofunction in migraine. Cephalalgia 9:239–245
Bom AH, Saxena PR, Verdouw PD (1988) Further characterization of the 5-HT1-like receptors in the carotid circulation of the pigs. Br J Pharmacol 94:327P
Bond RA, Clarke DE (1988) Agonist and antagonist characterization of a putative adrenoceptor with distinct pharmacological properties from the α- and β-subtypes. Br J Pharmacol 95:723–734
Bowery NG, Bettler B, Froestl W, Gallagher JP, Marshall F, Raiteri M, Bonner TI, Enna SJ (2002) International Union of Pharmacology. XXXIII. Mammalian gamma-aminobutyric acid(B) receptors: structure and function. Pharmacol Rev 54:247–264
Brain SD, Grant AD (2004) Vascular actions of calcitonin gene-related peptide and adrenomedullin. Physiol Rev 84:903–934
Brandes JL, Saper JR, Diamond M, Couch JR, Lewis DW, Schmitt J, Neto W, Schwabe S, Jacobs D (2004) Topiramate for migraine prevention: a randomized controlled trial. JAMA 291:965–973
Brundege JM, Dunwiddie TV (1997) Role of adenosine as a modulator of synaptic activity in the central nervous system. Adv Pharmacol 39:353–391
Buchanan TM, Ramadan NM, Aurora S (2004) Future pharmacologic targets for acute and preventive treatments of migraine. Expert Rev Neurother 4:391–430
Buchwalder A, Welch SK, Peroutka SJ (1996) Exclusion of 5-HT2A and 5-HT2C receptor genes as candidate genes for migraine. Headache 36:254–258
Burnstock G (2000) P2X receptors in sensory neurones. Br J Anaesth 84:476–488
Burstein R, Cutrer MF, Yarnitsky D (2000) The development of cutaneous allodynia during a migraine attack clinical evidence for the sequential recruitment of spinal and supraspinal nociceptive neurons in migraine. Brain 123(Pt 8):1703–1709
Bylund DB (1988) Subtypes of α2-adrenoceptors: pharmacological and molecular biological evidence converge. Trends Pharmacol Sci 9:356–361
Bylund DB (1992) Subtypes of α1- and α2-adrenergic receptors. Faseb J 6:832–839
Bylund DB, Ray-Prenger C, Murphy TJ (1988) α-2A and α-2B adrenergic receptor subtypes: antagonist binding in tissues and cell lines containing only one subtype. J Pharmacol Exp Ther 245:600–607
Bylund DB, Eikenberg DC, Hieble JP, Langer SZ, Lefkowitz RJ, Minneman KP, Molinoff PB, Ruffolo RR Jr, Trendelenburg U (1994) International Union of Pharmacology nomenclature of adrenoceptors. Pharmacol Rev 46:121–136
Bylund DB, Regan JW, Faber JE, Hieble JP, Triggle CR, Ruffolo RR Jr (1995) Vascular α-adrenoceptors: from the gene to the human. Can J Physiol Pharmacol 73:533–543
Calhoun AH (2004) A novel specific prophylaxis for menstrual-associated migraine. South Med J 97:819–822
Carlsson A, Lindqvist M, Magnusson M (1957) 3,4-Dihydroxyphenylalanine and 5-hydroxytryptophan as reserpine antagonists. Nature 180:1200
Carlsson A, Lindqvist M, Magnusson T, Walbeck B (1958) On the presence of 3-hydroxytyramine in brain. Science 127:471
Carroll JD, Hilton BP (1974) The effects of reserpine injection on methysergide treated control and migrainous subjects. Headache 14:149–156
Carruthers AM, Sellers LA, Jenkins DW, Jarvie EM, Feniuk W, Humphrey PPA (2001) Adenosine 1 receptor-mediated inhibition of protein kinase A-induced calcitonin gene-related peptide release from rat trigeminal neurons. Mol Pharmacol 59:1533–1541
Cassidy EM, Tomkins E, Dinan T, Hardiman O, O’Keane V (2003) Central 5-HT receptor hypersensitivity in migraine without aura. Cephalalgia 23:29–34
Centurión D, Glusa E, Sanchez-Lopez A, Valdivia LF, Saxena PR, Villalón CM (2004) 5-HT7, but not 5-HT2B, receptors mediate hypotension in vagosympathectomized rats. Eur J Pharmacol 502:239–242
Cerbo R, Barbanti P, Buzzi MG, Fabbrini G, Brusa L, Roberti C, Zanette E, Lenzi GL (1997) Dopamine hypersensitivity in migraine: role of the apomorphine test. Clin Neuropharmacol 20:36–41
Chai W, Mehrotra S, Danser AHJ, Schoemaker RG (2006) The role of calcitonin gene-related peptide (CGRP) in ischemic preconditioning in isolated rat hearts. Eur J Pharmacol 531:246–253
Charles JA, Jotkowitz S, Byrd LH (2006) Prevention of migraine with olmesartan in patients with hypertension/prehypertension. Headache 46:503–507
Classey JD, Knight YE, Goadsby PJ (2001) The NMDA receptor antagonist MK-801 reduces Fos-like immunoreactivity within the trigeminocervical complex following superior sagittal sinus stimulation in the cat. Brain Res 907:117–124
Clements JR, Magnusson KR, Hautman J, Beitz AJ (1991) Rat tooth pulp projections to spinal trigeminal subnucleus caudalis are glutamate-like immunoreactive. J Comp Neurol 309:281–288
Cohen Z, Bonvento G, Lacombe P, Hamel E (1996) Serotonin in the regulation of brain microcirculation. Prog Neurobiol 50:335–362
Colson NJ, Lea RA, Quinlan S, MacMillan J, Griffiths LR (2004) The estrogen receptor 1 G594A polymorphism is associated with migraine susceptibility in two independent case/control groups. Neurogenetics 5:129–133
Colson NJ, Lea RA, Quinlan S, MacMillan J, Griffiths LR (2005) Investigation of hormone receptor genes in migraine. Neurogenetics 6:17–23
Cook SP, McCleskey EW (1997) Desensitization, recovery and Ca(2+)-dependent modulation of ATP-gated P2X receptors in nociceptors. Neuropharmacology 36:1303–1308
Cook SP, Vulchanova L, Hargreaves KM, Elde R, McCleskey EW (1997) Distinct ATP receptors on pain-sensing and stretch-sensing neurons. Nature 387:505–508
Cotecchia S, Schwinn DA, Randall RR, Lefkowitz RJ, Caron MG, Kobilka BK (1988) Molecular cloning and expression of the cDNA for the hamster α1-adrenergic receptor. Proc Natl Acad Sci USA 85:7159–7163
Cruickshank JM, Prichard BN (1994) Beta-adrenoceptors.. In: Cruickshank JM, Prichard BNC (eds) B-blockers in clinical practice. Churchill Livingstone, Edinburgh, pp 9–86
Curran DA, Hinterberger H, Lance JW (1965) Total plasma serotonin, 5-hydroxyindoleacetic acid and p-hydroxy-m-methoxymandelic acid excretion in normal and migrainous subjects. Brain 88:997–1010
Cutrer FM (2001) Antiepileptic drugs: how they work in headache. Headache 41(Suppl. 1):S3–10
Cutrer FM, Limmroth V, Moskowitz MA (1997a) Possible mechanisms of valproate in migraine prophylaxis. Cephalalgia 17:93–100
Cutrer FM, Limmroth V, Waeber C, Yu X, Moskowitz MA (1997b) New targets for antimigraine drug development. In: Goadsby PJ, Silberstein S (eds) Headache. Butterworth-Heinemann, Philadelphia, pp 59–72
Cyr M, Ghribi O, Thibault C, Morissette M, Landry M, Di Paolo T (2001) Ovarian steroids and selective estrogen receptor modulators activity on rat brain NMDA and AMPA receptors. Brain Res Rev 37:153–161
Dahlöf CG, Hargreaves RJ (1998) Pathophysiology and pharmacology of migraine. Is there a place for antiemetics in future treatment strategies. Cephalalgia 18:593–604
D’Andrea G, Granella F, Perini F, Farruggio A, Leone M, Bussone G (2006) Platelet levels of dopamine are increased in migraine and cluster headache. Headache 46:585–591
De Gasparo M, Catt KJ, Inagami T, Wright JW, Unger T (2000) International union of pharmacology. XXIII. The angiotensin II receptors. Pharmacol Rev 52:415–472
De Vries P, Villalón CM, Saxena PR (1999a) Pharmacology of triptans. Emerging Drugs 4:107–125
De Vries P, Villalón CM, Saxena PR (1999b) Pharmacological aspects of experimental headache models in relation to acute antimigraine therapy. Eur J Pharmacol 375:61–74
Del Bene E, Poggioni M, Michelacci S (1983) Lisuride as a migraine prophylactic in children: an open clinical trial. Int J Clin Pharmacol Res 3:137–141
Di Trapani G, Mei D, Marra C, Mazza S, Capuano A (2000) Gabapentin in the prophylaxis of migraine: a double-blind randomized placebo-controlled study. Clin Ter 151:145–148
Diener HC, Tfelt-Hansen P, Dahlof C, Lainez MJ, Sandrini G, Wang SJ, Neto W, Vijapurkar U, Doyle A, Jacobs D (2004) Topiramate in migraine prophylaxis—results from a placebo-controlled trial with propranolol as an active control. J Neurol 251:943–950
Dluzen DE, Ramírez VD (1989) Progesterone enhances l-dopa-stimulated dopamine release from the caudate nucleus of freely behaving ovariectomized-estrogen-primed rats. Brain Res 494:122–128
Docherty JR (1998) Subtypes of functional α1- and α2-adrenoceptors. Eur J Pharmacol 361:1–15
Dodick DW, Martin VT, Smith T, Silberstein S (2004) Cardiovascular tolerability and safety of triptans: a review of clinical data. Headache 44(Suppl 1):S20–S30
Doods H, Hallermayer G, Wu D, Entzeroth M, Rudolf K, Engel W, Eberlein W (2000) Pharmacological profile of BIBN4096BS, the first selective small molecule CGRP antagonist. Br J Pharmacol 129:420–423
Dreier JP, Kleeberg J, Petzold G, Priller J, Windmuller O, Orzechowski HD, Lindauer U, Heinemann U, Einhaupl KM, Dirnagl U (2002) Endothelin-1 potently induces Leao’s cortical spreading depression in vivo in the rat: a model for an endothelial trigger of migrainous aura. Brain 125:102–112
Drummond PD, Lance JW (1983) Extracranial vascular changes and the source of pain in migraine headache. Ann Neurol 13:32–37
Drummond PD, Lance JW (1984) Facial temperature in migraine, tension-vascular and tension headache. Cephalalgia 4:149–158
Dumont Y, Fournier A, St-Pierre S, Quirion R (1997) A potent and selective CGRP2 agonist, [Cys(Et)2,7]hCGRP alpha: comparison in prototypical CGRP1 and CGRP2 in vitro bioassays. Can J Physiol Pharmacol 75:671–676
Durham PL (2004) CGRP-receptor antagonists—a fresh approach to migraine therapy. N Engl J Med 350:1073–1075
Edvinsson L (2004) Blockade of CGRP receptors in the intracranial vasculature: a new target in the treatment of headache. Cephalalgia 24:611–622
Edvinsson L, Goadsby PJ (1994) Neuropeptides in migraine and cluster headache. Cephalalgia 14:320–327
Enmark E, Gustafsson JA (1999) Oestrogen receptors—an overview. J Intern Med 246:133–138
Erdal ME, Herken H, Yilmaz M, Bayazit YA (2001) Association of the T102C polymorphism of 5-HT2A receptor gene with aura in migraine. J Neurol Sci 188:99–101
Erspamer V (1954) Pharmacology of indolealkylamines. Pharmacol Rev 6:425–487
Erspamer V, Asero B (1952) Identification of enteramine, the specific hormone of the enterochromaffin cell system, as 5-hydroxytryptamine. Nature 169:800–801
Fabbretti E, D’Arco M, Fabbro A, Simonetti M, Nistri A, Giniatullin R (2006) Delayed upregulation of ATP P2X3 receptors of trigeminal sensory neurons by calcitonin gene-related peptide. J Neurosci 26:6163–6171
Facchinetti F, Martignoni E, Nappi G, Fioroni L, Sances G, Genazzani AR (1989) Premenstrual failure of α-adrenergic stimulation on hypothalamus–pituitary responses in menstrual migraine. Psychosom Med 51:550–558
Facchinetti F, Sances G, Borella P, Genazzani AR, Nappi G (1991) Magnesium prophylaxis of menstrual migraine: effects on intracellular magnesium. Headache 31:298–301
Farkkila M, Palo J, Saijonmaa O, Fyhrquist F (1992) Raised plasma endothelin during acute migraine attack. Cephalalgia 12:383–384, discussion 340
Fernández-Ruíz JJ, de Miguel R, Hernández ML, Ramos JA (1990) Time-course of the effects of ovarian steroids on the activity of limbic and striatal dopaminergic neurons in female rat brain. Pharmacol Biochem Behav 36:603–606
Ferrari MD (1991) 5-HT3 receptor antagonists and migraine therapy. J Neurol 238 Suppl 1:S53–56
Ferrari MD, Saxena PR (1993) Clinical and experimental effects of sumatriptan in humans. Trends Pharmacol Sci 14:129–133
Forbes IT, Ham P, Booth DH, Martin RT, Thompson M, Baxter GS, Blackburn TP, Glen A, Kennett GA, Wood MD (1995) 5-Methyl-1-(3-pyridylcarbamoyl)-1,2,3,5-tetrahydropyrrolo[2,3-f]indole: a novel 5-HT2C/5-HT2B receptor antagonist with improved affinity, selectivity, and oral activity. J Med Chem 38:2524–2530
Ford AP, Williams TJ, Blue DR, Clarke DE (1994) α1-Adrenoceptor classification: sharpening Occam’s razor. Trends Pharmacol Sci 15:167–170
Forssman B, Lindblad CJ, Zbornikova V (1983) Atenolol for migraine prophylaxis. Headache 23:188–190
Fozard JR, Kalkman HO (1994) 5-Hydroxytryptamine (5-HT) and the initiation of migraine: new perspectives. Naunyn-Schmiedeberg‘s Arch Pharmacol 350:225–229
Francken BJ, Jurzak M, Vanhauwe JF, Luyten WH, Leysen JE (1998) The human 5-ht5A receptor couples to Gi/Go proteins and inhibits adenylate cyclase in HEK 293 cells. Eur J Pharmacol 361:299–309
Fredholm BB, Ijzerman AP, Jacobson KA, Klotz KN, Linden J (2001) International Union of Pharmacology. XXV. Nomenclature and classification of adenosine receptors. Pharmacol Rev 53:527–552
Freitag FG, Diamond S (1984) Nadolol and placebo comparison study in the prophylactic treatment of migraine. J Am Osteopath Assoc 84:343–347
Fusayasu E, Kowa H, Takeshima T, Nakaso K, Nakashima K (2007) Increased plasma substance P and CGRP levels, and high ACE activity in migraineurs during headache-free periods. Pain 128:209–214
Galitzky J, Langin D, Verwaerde P, Montastruc JL, Lafontan M, Berlan M (1997) Lipolytic effects of conventional β3-adrenoceptor agonists and of CGP 12,177 in rat and human fat cells: preliminary pharmacological evidence for a putative β4-adrenoceptor. Br J Pharmacol 122:1244–1250
Garry MG, Walton LP, Davis MA (2000) Capsaicin-evoked release of immunoreactive calcitonin gene-related peptide from the spinal cord is mediated by nitric oxide but not by cyclic GMP. Brain Res 861:208–219
Geppetti P, Del Bianco E, Santicioli P, Lippe IT, Maggi CA, Sicuteri F (1990) Release of sensory neuropeptides from dural venous sinuses of guinea pig. Brain Res 510:58–62
Ghelardoni S, Carnicelli V, Frascarelli S, Lankford A, Masala I, Ronca-Testoni S, Matherne GP, Zucchi R (2005) Effects of A1 adenosine receptor stimulation on the expression of genes involved in calcium homeostasis. J Mol Cell Cardiol 39:964–971
Giffin NJ, Kowacs F, Libri V, Williams P, Goadsby PJ, Kaube H (2003) Effect of the adenosine A1 receptor agonist GR79236 on trigeminal nociception with blink reflex recordings in healthy human subjects. Cephalalgia 23:287–292
Goadsby PJ (2005) New targets in the acute treatment of headache. Curr Opin Neurol 18:283–288
Goadsby PJ, Lance JW (1990) Physiopathology of migraine. Rev Prat 40:389–393
Goadsby PJ, Classey JD (2000) Glutamatergic transmission in the trigeminal nucleus assessed with local blood flow. Brain Res 875:119–124
Goadsby PJ, Classey JD (2003) Evidence for serotonin 5-HT1B, 5-HT1D and 5-HT1F receptor inhibitory effects on trigeminal neurons with craniovascular input. Neuroscience 122:491–498
Goadsby PJ, Edvinsson L, Ekman R (1988) Release of vasoactive peptides in the extracerebral circulation of humans and the cat during activation of the trigeminovascular system. Ann Neurol 23:193–196
Goadsby PJ, Adner M, Edvinsson L (1996) Characterization of endothelin receptors in the cerebral vasculature and their lack of effect on spreading depression. J Cereb Blood Flow Metab 16:698–704
Goadsby PJ, Lipton RB, Ferrari MD (2002a) Migraine—current understanding and treatment. N Engl J Med 346:257–270
Goadsby PJ, Hoskin KL, Storer RJ, Edvinsson L, Connor HE (2002b) Adenosine A1 receptor agonists inhibit trigeminovascular nociceptive transmission. Brain 125:1392–1401
Goldstein DJ, Wang O, Saper JR, Stoltz R, Silberstein SD, Mathew NT (1997) Ineffectiveness of neurokinin-1 antagonist in acute migraine: a crossover study. Cephalalgia 17:785–790
Goldstein DJ, Offen WW, Klein EG, Phebus LA, Hipskind P, Johnson KW, Ryan RE Jr (2001a) Lanepitant, an NK-1 antagonist, in migraine prevention. Cephalalgia 21:102–106
Goldstein DJ, Roon KI, Offen WW, Ramadan NM, Phebus LA, Johnson KW, Schaus JM, Ferrari MD (2001b) Selective serotonin 1F (5-HT1F) receptor agonist LY334370 for acute migraine: a randomised controlled trial. Lancet 358:1230–1234
Gómez-Mancilla B, Cutler NR, Leibowitz MT, Spierings EL, Klapper JA, Diamond S, Goldstein J, Smith T, Couch JR, Fleishaker J, Azie N, Blunt DE (2001) Safety and efficacy of PNU-142633, a selective 5-HT1D agonist, in patients with acute migraine. Cephalalgia 21:727–732
Gupta S, Mehrotra S, Avezaat CJJ, Villalón CM, Saxena PR, MaassenVanDenBrink A (2006a) Characterisation of CGRP receptors in the human isolated middle meningeal artery. Life Sci 79:265–271
Gupta S, Mehrotra S, Villalón CM, Garrelds IM, de Vries R, van Kats JP, Sharma HS, Saxena PR, MaassenVanDenBrink A (2006b) Characterisation of CGRP receptors in human and porcine isolated coronary arteries: evidence for CGRP receptor heterogeneity. Eur J Pharmacol 530:107–116
Gupta S, Mehrotra S, Villalón CM, Perusquía M, Saxena PR, MaassenVanDenBrink A (2007) Potential role of female sex hormones in the pathophysiology of migraine. Pharmacol Ther 113:321–340
Hamilton SG, McMahon SB (2000) ATP as a peripheral mediator of pain. J Auton Nerv Syst 81:187–194
Hanna MG (2006) Genetic neurological channelopathies. Nat Clin Pract Neurol 2:252–263
Hasler WL (1999) Serotonin receptor physiology: relation to emesis. Dig Dis Sci 44:108S–113S
Hasselblatt M, Kohler J, Volles E, Ehrenreich H (1999) Simultaneous monitoring of endothelin-1 and vasopressin plasma levels in migraine. Neuroreport 10:423–425
Hein L, Kobilka BK (1995) Adrenergic receptor signal transduction and regulation. Neuropharmacology 34:357–366
Hering-Hanit R (1999) Baclofen for prevention of migraine. Cephalalgia 19:589–591
Hernández ML, Fernández-Ruíz JJ, de Miguel R, Ramos JA (1991) Time-dependent effects of ovarian steroids on tyrosine hydroxylase activity in the limbic forebrain of female rats. J Neural Transm Gen Sect 83:77–84
Herrmann WM, Kristof M, Sastre M (1978) Preventive treatment of migraine headache with a new isoergolenyl derivative. J Int Med Res 6:476–482
Heyck H (1969) Pathogenesis of migraine. Research clinical studies Headache 2:1–28
Hieble JP (2000) Adrenoceptor subclassification: an approach to improved cardiovascular therapeutics. Pharm Acta Helv 74:163–171
Hieble JP, Bylund DB, Clarke DE, Eikenburg DC, Langer SZ, Lefkowitz RJ, Minneman KP, Ruffolo RR Jr (1995) International Union of Pharmacology. X. Recommendation for nomenclature of α1-adrenoceptors: consensus update. Pharmacol Rev 47:267–270
Hill SJ, Ganellin CR, Timmerman H, Schwartz JC, Shankley NP, Young JM, Schunack W, Levi R, Haas HL (1997) International union of pharmacology. XIII. Classification of histamine receptors. Pharmacol Rev 49:253–278
Ho TW, Mannix LK, Fan X, Assaid C, Furtek C, Jones CJ, Lines CR, Rapoport AM (2008) Randomized controlled trial of an oral CGRP antagonist, MK-0974, in acute treatment of migraine. Neurology 70:1304–1312
Hoffman BB (2001) Catecholamines, sympathomimetic drugs, and adrenergic receptor antagonists, 10th edn. McGraw-Hill, New York
Hofmann C, Penner U, Dorow R, Pertz HH, Jahnichen S, Horowski R, Latte KP, Palla D, Schurad B (2006) Lisuride, a dopamine receptor agonist with 5-HT2B receptor antagonist properties: absence of cardiac valvulopathy adverse drug reaction reports supports the concept of a crucial role for 5-HT2B receptor agonism in cardiac valvular fibrosis. Clin Neuropharmacol 29:80–86
Hohoff C, Marziniak M, Lesch KP, Deckert J, Sommer C, Mossner R (2007) An adenosine A2A receptor gene haplotype is associated with migraine with aura. Cephalalgia 27:177–181
Honey AC, Bland-Ward PA, Connor HE, Feniuk W, Humphrey PPA (2002) Study of an adenosine A1 receptor agonist on trigeminally evoked dural blood vessel dilation in the anaesthetized rat. Cephalalgia 22:260–264
Honkaniemi J, Liimatainen S, Rainesalo S, Sulavuori S (2006) Haloperidol in the acute treatment of migraine: a randomized, double-blind, placebo-controlled study. Headache 46:781–787
Hoskin KL, Lambert GA, Donaldson C, Zagami AS (2004) The 5-hydroxytryptamine1B/1D/1F receptor agonists eletriptan and naratriptan inhibit trigeminovascular input to the nucleus tractus solitarius in the cat. Brain Res 998:91–99
Hoyer D (1990) Serotonin 5-HT3, 5-HT4, and 5-HT-M receptors. Neuropsychopharmacology 3:371–383
Hoyer D, Clarke DE, Fozard JR, Hartig PR, Martin GR, Mylecharane EJ, Saxena PR, Humphrey PPA (1994) International Union of Pharmacology classification of receptors for 5-hydroxytryptamine (serotonin). Pharmacol Rev 46:157–203
Hughes A, Thom S, Martin G, Redman D, Hasan S, Sever P (1986) The action of a dopamine (DA1) receptor agonist, fenoldopam in human vasculature in vivo and in vitro. Br J Clin Pharmacol 22:535–540
Hurley PT, McMahon RA, Fanning P, O’Boyle KM, Rogers M, Martin F (1998) Functional coupling of a recombinant human 5-HT5A receptor to G-proteins in HEK-293 cells. Br J Pharmacol 124:1238–1244
Iovino M, Feifel U, Yong CL, Wolters JM, Wallenstein G (2004) Safety, tolerability and pharmacokinetics of BIBN 4096 BS, the first selective small molecule calcitonin gene-related peptide receptor antagonist, following single intravenous administration in healthy volunteers. Cephalalgia 24:645–656
Ishida T, Kawashima S, Hirata K, Yokoyama M (1998) Nitric oxide is produced via 5-HT1B and 5-HT2B receptor activation in human coronary artery endothelial cells. Kobe J Med Sci 44:51–63
Ishida T, Hirata K, Sakoda T, Kawashima S, Akita H, Yokoyama M (1999) Identification of mRNA for 5-HT1 and 5-HT2 receptor subtypes in human coronary arteries. Cardiovasc Res 41:267–274
IUPHAR (2006) 3rd Major update to IUPHAR receptor database. http://www.iuphar-db.org/GPCR/ReceptorFamiliesForward.
Jackson DL, Hargreaves KM (1999) Activation of excitatory amino acid receptors in bovine dental pulp evokes the release of iCGRP. J Dent Res 78:54–60
Jansen-Olesen I, Jorgensen L, Engel U, Edvinsson L (2003) In-depth characterization of CGRP receptors in human intracranial arteries. Eur J Pharmacol 481:207–216
Jen JC, Wan J, Palos TP, Howard BD, Baloh RW (2005) Mutation in the glutamate transporter EAAT1 causes episodic ataxia, hemiplegia, and seizures. Neurology 65:529–534
Johannsson V, Nilsson LR, Widelius T, Javerfalk T, Hellman P, Akesson JA, Olerud B, Gustafsson CL, Raak A, Sandahl G et al (1987) Atenolol in migraine prophylaxis a double-blind cross-over multicentre study. Headache 27:372–374
Johnson KW, Nelson DL, Dieckman DK, Wainscott DB, Lucaites VL, Audia JE, Owton WM, Phebus LA (2003) Neurogenic dural protein extravasation induced by meta-chlorophenylpiperazine (mCPP) involves nitric oxide and 5-HT2B receptor activation. Cephalalgia 23:117–123
Kalkman HO (1994) Is migraine prophylactic activity caused by 5-HT2B or 5-HT2C receptor blockade. Life Sci 54:641–644
Kallela M, Farkkila M, Saijonmaa O, Fyhrquist F (1998) Endothelin in migraine patients. Cephalalgia 18:329–332
Kapoor K, Arulmani U, Heiligers JPC, Garrelds IM, Willems EW, Doods H, Villalón CM, Saxena PR (2003) Effects of the CGRP receptor antagonist BIBN4096BS on capsaicin-induced carotid haemodynamic changes in anaesthetised pigs. Br J Pharmacol 140:329–338
Kastner P, Krust A, Turcotte B, Stropp U, Tora L, Gronemeyer H, Chambon P (1990) Two distinct estrogen-regulated promoters generate transcripts encoding the two functionally different human progesterone receptor forms A and B. EMBO J 9:1603–1614
Kaube H, Herzog J, Kaufer T, Dichgans M, Diener HC (2000) Aura in some patients with familial hemiplegic migraine can be stopped by intranasal ketamine. Neurology 55:139–141
Kaumann AJ (1997) Four β-adrenoceptor subtypes in the mammalian heart. Trends Pharmacol Sci 18:70–76
Kelly MJ, Levin ER (2001) Rapid actions of plasma membrane estrogen receptors. Trends Endocrinol Metab 12:152–156
Kimball RW, Friedman AP, Vallejo E (1960) Effect of serotonin in migraine patients. Neurology 10:107–111
Kobilka BK, Matsui H, Kobilka TS, Yang-Feng TL, Francke U, Caron MG, Lefkowitz RJ, Regan JW (1987) Cloning, sequencing, and expression of the gene coding for the human platelet α2-adrenergic receptor. Science 238:650–656
Kowa H, Shimomura T, Takahashi K (1992) Platelet gamma-aminobutyric acid levels in migraine and tension-type headache. Headache 32:229–232
Krobert KA, Levy FO (2002) The human 5-HT7 serotonin receptor splice variants: constitutive activity and inverse agonist effects. Br J Pharmacol 135:1563–1571
Lakhlani PP, Amenta F, Napoleone P, Felici L, Eikenburg DC (1994) Pharmacological characterization and anatomical localization of prejunctional beta-adrenoceptors in the rat kidney. Br J Pharmacol 111:1296–1308
Lambert GA, Donaldson C, Hoskin KL, Boers PM, Zagami AS (2004) Dilatation induced by 5-HT in the middle meningeal artery of the anaesthetised cat. Naunyn-Schmiedeberg’s Arch Pharmacol 369:591–601
Lampl C, Katsarava Z, Diener HC, Limmroth V (2005) Lamotrigine reduces migraine aura and migraine attacks in patients with migraine with aura. J Neurol Neurosurg Psychiatry 76:1730–1732
Lands AM, Arnold A, McAuliff JP, Luduena FP, Brown TG Jr (1967) Differentiation of receptor systems activated by sympathomimetic amines. Nature 214:597–598
Lanier SM, Downing S, Duzic E, Homcy CJ (1991) Isolation of rat genomic clones encoding subtypes of the α2-adrenergic receptor. Identification of a unique receptor subtype. J Biol Chem 266:10470–10478
Lassen LH, Thomsen LL, Olesen J (1995) Histamine induces migraine via the H1-receptor. Support for the NO hypothesis of migraine. Neuroreport 6:1475–1479
Lassen LH, Thomsen LL, Kruuse C, Iversen HK, Olesen J (1996) Histamine-1 receptor blockade does not prevent nitroglycerin induced migraine. Support for the NO-hypothesis of migraine. Eur J Clin Pharmacol 49:335–339
Lassen LH, Ashina M, Christiansen I, Ulrich V, Grover R, Donaldson J, Olesen J (1998) Nitric oxide synthase inhibition: a new principle in the treatment of migraine attacks. Cephalalgia 18:27–32
Lau YT (2002) Receptor-dependent and genomic-independent actions of estrogen in vascular protection. Chang Gung Med J 25:636–644
Lee WS, Limmroth V, Ayata C, Cutrer FM, Waeber C, Yu X, Moskowitz MA (1995) Peripheral GABAA receptor-mediated effects of sodium valproate on dural plasma protein extravasation to substance P and trigeminal stimulation. Br J Pharmacol 116:1661–1667
Lee ST, Park JH, Kim M (2005) Efficacy of the 5-HT1A agonist, buspirone hydrochloride, in migraineurs with anxiety: a randomized, prospective, parallel group, double-blind, placebo-controlled study. Headache 45:1004–1011
Lesch KP, Lerer B (1991) The 5-HT receptor-G-protein–effector system complex in depression. I. Effect of glucocorticoids. J Neural Transm Gen Sect 84:3–18
Limbird LE (1988) Receptors linked to inhibition of adenylate cyclase: additional signaling mechanisms. Faseb J 2:2686–2695
Limmroth V, Michel MC (2001) The prevention of migraine: a critical review with special emphasis on β-adrenoceptor blockers. Br J Clin Pharmacol 52:237–243
Lipton RB, Stewart WF, Diamond S, Diamond ML, Reed M (2001) Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache 41:646–657
Lodi R, Kemp GJ, Montagna P, Pierangeli G, Cortelli P, Iotti S, Radda GK, Barbiroli B (1997) Quantitative analysis of skeletal muscle bioenergetics and proton efflux in migraine and cluster headache. J Neurol Sci 146:73–80
Lomasney JW, Cotecchia S, Lorenz W, Leung WY, Schwinn DA, Yang-Feng TL, Brownstein M, Lefkowitz RJ, Caron MG (1991) Molecular cloning and expression of the cDNA for the α1A-adrenergic receptor. The gene for which is located on human chromosome 5. J Biol Chem 266:6365–6369
Luebke AE, Dahl GP, Roos BA, Dickerson IM (1996) Identification of a protein that confers calcitonin gene-related peptide responsiveness to oocytes by using a cystic fibrosis transmembrane conductance regulator assay. Proc Natl Acad Sci USA 93:3455–3460
Ma QP (2001) Co-localization of 5-HT1B/1D/1F receptors and glutamate in trigeminal ganglia in rats. Neuroreport 12:1589–1591
MaassenVanDenBrink A, Reekers M, Bax WA, Ferrari MD, Saxena PR (1998) Coronary side-effect potential of current and prospective antimigraine drugs. Circulation 98:25–30
MaassenVanDenBrink A, van den Broek RWM, de Vries R, Bogers AJC, Avezaat CJJ, Saxena PR (2000) Craniovascular selectivity of eletriptan and sumatriptan in human isolated blood vessels. Neurology 55:1524–1530
MacGregor EA (2006) Migraine and the menopause. J Br Menopause Soc 12:104–108
MacGregor EA, Hackshaw A (2002) Prevention of migraine in the pill-free interval of combined oral contraceptives: a double-blind, placebo-controlled pilot study using natural oestrogen supplements. J Fam Plann Reprod Health Care 28:27–31
MacGregor EA, Frith A, Ellis J, Aspinall L, Hackshaw A (2006a) Prevention of menstrual attacks of migraine: a double-blind placebo-controlled crossover study. Neurology 67:2159–2163
MacGregor EA, Frith A, Ellis J, Aspinall L, Hackshaw A (2006b) Incidence of migraine relative to menstrual cycle phases of rising and falling estrogen. Neurology 67:2154–2158
Magos AL, Zilkha KJ, Studd JW (1983) Treatment of menstrual migraine by oestradiol implants. J Neurol Neurosurg Psychiatry 46:1044–1046
Marceau F, Regoli D (2004) Bradykinin receptor ligands: therapeutic perspectives. Nat Rev Drug Discov 3:845–852
Martin VT, Behbehani M (2006) Ovarian hormones and migraine headache: understanding mechanisms and pathogenesis—part I. Headache 46:3–23
Martínez F, Castillo J, Rodríguez JR, Leira R, Noya M (1993) Neuroexcitatory amino acid levels in plasma and cerebrospinal fluid during migraine attacks. Cephalalgia 13:89–93
Mathew NT, Kailasam J, Meadors L, Chernyschev O, Gentry P (2000) Intravenous valproate sodium (depacon) aborts migraine rapidly: a preliminary report. Headache 40:720–723
Matsubara T, Moskowitz MA, Huang Z (1992) UK-14,304, R(−)-alpha-methyl-histamine and SMS 201-995 block plasma protein leakage within dura mater by prejunctional mechanisms. Eur J Pharmacol 224:145–150
Maude S, Curtin J, Breen G, Collier D, Russell G, Shaw D, Clair DS (2001) The −141C Ins/Del polymorphism of the dopamine D2 receptor gene is not associated with either migraine or Parkinson’s disease. Psychiatr Genet 11:49–52
May A, Gijsman HJ, Wallnofer A, Jones R, Diener HC, Ferrari MD (1996) Endothelin antagonist bosentan blocks neurogenic inflammation, but is not effective in aborting migraine attacks. Pain 67:375–378
May A, Shepheard SL, Knorr M, Effert R, Wessing A, Hargreaves RJ, Goadsby PJ, Diener HC (1998) Retinal plasma extravasation in animals but not in humans: implications for the pathophysiology of migraine. Brain 121(Pt 7):1231–1237
May A, Buchel C, Turner R, Goadsby PJ (2001) Magnetic resonance angiography in facial and other pain: neurovascular mechanisms of trigeminal sensation. J Cereb Blood Flow Metab 21:1171–1176
McCall RB, Huff R, Chio CL, TenBrink R, Bergh CL, Ennis MD, Ghazal NB, Hoffman RL, Meisheri K, Higdon NR, Hall E (2002) Preclinical studies characterizing the anti-migraine and cardiovascular effects of the selective 5-HT1D receptor agonist PNU-142633. Cephalalgia 22:799–806
McLatchie LM, Fraser NJ, Main MJ, Wise A, Brown J, Thompson N, Solari R, Lee MG, Foord SM (1998) RAMPs regulate the transport and ligand specificity of the calcitonin-receptor-like receptor. Nature 393:333–339
Medhurst AD, Lezoualc, h F, Fischmeister R, Middlemiss DN, Sanger GJ (2001) Quantitative mRNA analysis of five C-terminal splice variants of the human 5-HT4 receptor in the central nervous system by TaqMan real time RT-PCR. Brain Res Mol Brain Res 90:125–134
Mehrotra S, Gupta S, Garrelds IM, Villalón CM, Saxena PR, Bogers AJJC, MaassenVanDenBrink A (2006) Effects of current and prospective antimigraine drugs on the porcine isolated meningeal artery. Naunyn-Schmiedeberg’s Arch Pharmacol 374:163–175
Mehrotra S, Gupta S, Villalón CM, Boomsma F, Saxena PR, MaassenVanDenBrink A (2007) Rat carotid artery responses to α-adrenergic receptor agonists and 5-HT after ovariectomy and hormone replacement. Headache 47:236–246
Michel AD, Loury DN, Whiting RL (1989) Differences between the α2-adrenoceptor in rat submaxillary gland and the α2A- and α2B-adrenoceptor subtypes. Br J Pharmacol 98:890–897
Michelotti GA, Price DT, Schwinn DA (2000) α1-adrenergic receptor regulation: basic science and clinical implications. Pharmacol Ther 88:281–309
Millán-Guerrero RO, Pineda-Lucatero AG, Hernández-Benjamin T, Tene CE, Pacheco MF (2003) N-alpha-methylhistamine safety and efficacy in migraine prophylaxis: phase I and phase II studies. Headache 43:389–394
Millán-Guerrero RO, Isais-Millán R, Benjamin TH, Tene CE (2006) N-alpha-methyl histamine safety and efficacy in migraine prophylaxis: phase III study. Can J Neurol Sci 33:195–199
Millson DS, Tepper SJ, Rapoport AM (2000) Migraine pharmacotherapy with oral triptans: a rational approach to clinical management. Expert Opin Pharmacother 1:391–404
Mitsikostas DD, Sanchez del Rio M, Waeber C, Moskowitz MA, Cutrer FM (1998) The NMDA receptor antagonist MK-801 reduces capsaicin-induced c-fos expression within rat trigeminal nucleus caudalis. Pain 76:239–248
Mitsikostas DD, Sanchez del Rio M, Waeber C, Huang Z, Cutrer FM, Moskowitz MA (1999) Non-NMDA glutamate receptors modulate capsaicin induced c-fos expression within trigeminal nucleus caudalis. Br J Pharmacol 127:623–630
Mochi M, Cevoli S, Cortelli P, Pierangeli G, Soriani S, Scapoli C, Montagna P (2003) A genetic association study of migraine with dopamine receptor 4, dopamine transporter and dopamine-beta-hydroxylase genes. Neurol Sci 23:301–305
Mody I, Lambert JD, Heinemann U (1987) Low extracellular magnesium induces epileptiform activity and spreading depression in rat hippocampal slices. J Neurophysiol 57:869–888
Moreau ME, Garbacki N, Molinaro G, Brown NJ, Marceau F, Adam A (2005) The kallikrein–kinin system: current and future pharmacological targets. J Pharmacol Sci 99:6–38
Moskowitz MA, Cutrer FM (1993) Sumatriptan: a receptor-targeted treatment for migraine. Annu Rev Med 44:145–154
Moskowitz MA, Buzzi MG, Sakas DE, Linnik MD (1989) Pain mechanisms underlying vascular headaches. Progress Report 1989. Rev Neurol 145:181–193
Murphy TJ, Bylund DB (1988) Characterization of α2–adrenergic receptors in the OK cell, an opossum kidney cell line. J Pharmacol Exp Ther 244:571–578
Nag S, Mokha SS (2006) Activation of α2-adrenoceptors in the trigeminal region produces sex-specific modulation of nociception in the rat. Neuroscience 142:1255–1262
Olesen J, Lipton RB (1994) Migraine classification and diagnosis. International Headache Society criteria. Neurology 44:S6–10
Olesen J, Diener HC, Husstedt IW, Goadsby PJ, Hall D, Meier U, Pollentier S, Lesko LM (2004) Calcitonin gene-related peptide receptor antagonist BIBN4096BS for the acute treatment of migraine. N Engl J Med 350:1104–1110
Oliver KR, Wainwright A, Edvinsson L, Pickard JD, Hill RG (2002) Immunohistochemical localization of calcitonin receptor-like receptor and receptor activity-modifying proteins in the human cerebral vasculature. J Cereb Blood Flow Metab 22:620–629
Ophoff RA, Terwindt GM, Vergouwe MN, van Eijk R, Oefner PJ, Hoffman SM, Lamerdin JE, Mohrenweiser HW, Bulman DE, Ferrari M, Haan J, Lindhout D, van Ommen GJ, Hofker MH, Ferrari MD, Frants RR (1996) Familial hemiplegic migraine and episodic ataxia type-2 are caused by mutations in the Ca2+ channel gene CACNL1A4. Cell 87:543–552
Orshal JM, Khalil RA (2004) Gender, sex hormones, and vascular tone. Am J Physiol Regul Integr Comp Physiol 286:R233–249
Oshita M, Kigoshi S, Muramatsu I (1991) Three distinct binding sites for [3H]-prazosin in the rat cerebral cortex. Br J Pharmacol 104:961–965
Page IH (1954) Serotonin (5 Hydroxytryptamine). Physiol Rev 34:563–588
Palmer JE, Chronicle EP, Rolan P, Mulleners WM (2000) Cortical hyperexcitability is cortical under-inhibition: evidence from a novel functional test of migraine patients. Cephalalgia 20:525–532
Paterna S, Di Pasquale P, D, Angelo A, Seidita G, Tuttolomondo A, Cardinale A, Maniscalchi T, Follone G, Giubilato A, Tarantello M, Licata G (2000) Angiotensin-converting enzyme gene deletion polymorphism determines an increase in frequency of migraine attacks in patients suffering from migraine without aura. Eur Neurol 43:133–136
Peeters M, Gunthorpe MJ, Strijbos PJ, Goldsmith P, Upton N, James MF (2007) Effects of pan- and subtype-selective NMDA receptor antagonists on cortical spreading depression in the rat: therapeutic potential for migraine. J Pharmacol Exp Ther 312:564–572
Pérez DM, Piascik MT, Graham RM (1991) Solution-phase library screening for the identification of rare clones: isolation of an α1D-adrenergic receptor cDNA. Mol Pharmacol 40:876–883
Peroutka SJ (1988) Antimigraine drug interactions with serotonin receptor subtypes in human brain. Ann Neurol 23:500–504
Peroutka SJ (1997) Dopamine and migraine. Neurology 49:650–656
Peroutka SJ (2004) Migraine: a chronic sympathetic nervous system disorder. Headache 44:53–64
Peroutka SJ (2005) Neurogenic inflammation and migraine: implications for the therapeutics. Mol Interv 5:304–311
Peroutka SJ, Wilhoit T, Jones K (1997) Clinical susceptibility to migraine with aura is modified by dopamine D2 receptor (DRD2) NcoI alleles. Neurology 49:201–206
Peroutka SJ, Price SC, Wilhoit TL, Jones KW (1998) Comorbid migraine with aura, anxiety, and depression is associated with dopamine D2 receptor (DRD2) NcoI alleles. Mol Med 4:14–21
Petersen KA, Nilsson E, Olesen J, Edvinsson L (2005a) Presence and function of the calcitonin gene-related peptide receptor on rat pial arteries investigated in vitro and in vivo. Cephalalgia 25:424–432
Petersen KA, Lassen LH, Birk S, Lesko L, Olesen J (2005b) BIBN4096BS antagonizes human α-calcitonin gene related peptide-induced headache and extracerebral artery dilatation. Clin Pharmacol Ther 77:202–213
Phebus LA, Johnson KW, Zgombick JM, Gilbert PJ, Van Belle K, Mancuso V, Nelson DL, Calligaro DO, Kiefer AD Jr, Branchek TA, Flaugh ME (1997) Characterization of LY344864 as a pharmacological tool to study 5-HT1F receptors: binding affinities, brain penetration and activity in the neurogenic dural inflammation model of migraine. Life Sci 61:2117–2126
Piascik MT, Hrometz SL, Edelmann SE, Guarino RD, Hadley RW, Brown RD (1997) Immunocytochemical localization of the α1B-adrenergic receptor and the contribution of this and the other subtypes to vascular smooth muscle contraction: analysis with selective ligands and antisense oligonucleotides. J Pharmacol Exp Ther 283:854–868
Pindon A, van Hecke G, van Gompel P, Lesage AS, Leysen JE, Jurzak M (2002) Differences in signal transduction of two 5-HT4 receptor splice variants: compound specificity and dual coupling with Gas- and Gai/o-proteins. Mol Pharmacol 61:85–96
Pouzet B (2002) SB-258741: a 5-HT7 receptor antagonist of potential clinical interest. CNS Drug Rev 8:90–100
Powell KJ, Ma W, Sutak M, Doods H, Quirion R, Jhamandas K (2000) Blockade and reversal of spinal morphine tolerance by peptide and non-peptide calcitonin gene-related peptide receptor antagonists. Br J Pharmacol 131:875–884
Poyner DR, Sexton PM, Marshall I, Smith DM, Quirion R, Born W, Muff R, Fischer JA, Foord SM (2002) International Union of Pharmacology. XXXII. The mammalian calcitonin gene-related peptides, adrenomedullin, amylin, and calcitonin receptors. Pharmacol Rev 54:233–246
Price GW, Burton MJ, Collin LJ, Duckworth M, Gaster L, Gothert M, Jones BJ, Roberts C, Watson JM, Middlemiss DN (1997) SB-216641 and BRL-15572-compounds to pharmacologically discriminate h5-HT1B and h5-HT1D receptors. Naunyn-Schmiedeberg’s Arch Pharmacol 356:312–320
Quartu M, Serra MP, Ambu R, Lai ML, Del Fiacco M (2002) AMPA-type glutamate receptor subunits 2/3 in the human trigeminal sensory ganglion and subnucleus caudalis from prenatal ages to adulthood. Mech Ageing Dev 123:463–471
Quirion R, Van Rossum D, Dumont Y, St-Pierre S, Fournier A (1992) Characterization of CGRP1 and CGRP2 receptor subtypes. Ann N Y Acad Sci 657:88–105
Rabkin R, Stables DP, Levin NW, Suzman MM (1966) The prophylactic value of propranolol in angina pectoris. Am J Cardiol 18:370–383
Ramadan NM, Halvorson H, Vande-Linde A, Levine SR, Helpern JA, Welch KMA (1989) Low brain magnesium in migraine. Headache 29:590–593
Ramadan NM, Schultz LL, Gilkey SJ (1997) Migraine prophylactic drugs: proof of efficacy, utilization and cost. Cephalalgia 17:73–80
Ramadan NM, Skljarevski V, Phebus LA, Johnson KW (2003) 5-HT1F receptor agonists in acute migraine treatment: a hypothesis. Cephalalgia 23:776–785
Rapport MM, Green AA, Page IH (1948) Serum vasoconstrictor (serotonin). IV. Isolation and characterization. J Biol Chem 176:1243–1251
Rasmussen BK, Jensen R, Schroll M, Olesen J (1991) Epidemiology of headache in a general population—a prevalence study. J Clin Epidemiol 44:1147–1157
Regan JW, Kobilka TS, Yang-Feng TL, Caron MG, Lefkowitz RJ, Kobilka BK (1988) Cloning and expression of a human kidney cDNA for an α2-adrenergic receptor subtype. Proc Natl Acad Sci USA 85:6301–6305
Roffey P, Mikhail M, Thangathurai D (2001) NMDA receptor blockade prevents nitroglycerin-induced headaches. Headache 41:733
Roon KI, Olesen J, Diener HC, Ellis P, Hettiarachchi J, Poole PH, Christianssen I, Kleinermans D, Kok JG, Ferrari MD (2000) No acute antimigraine efficacy of CP-122,288, a highly potent inhibitor of neurogenic inflammation: results of two randomized, double-blind, placebo-controlled clinical trials. Ann Neurol 47:238–241
Rouleau A, Garbarg M, Ligneau X, Mantion C, Lavie P, Advenier C, Lecomte JM, Krause M, Stark H, Schunack W, Schwartz JC (1997) Bioavailability, antinociceptive and antiinflammatory properties of BP 2–94, a histamine H3 receptor agonist prodrug. J Pharmacol Exp Ther 281:1085–1094
Sahara Y, Noro N, Iida Y, Soma K, Nakamura Y (1997) Glutamate receptor subunits GluR5 and KA-2 are coexpressed in rat trigeminal ganglion neurons. J Neurosci 17:6611–6620
Salvatore CA, Hershey JC, Corcoran HA, Fay JF, Johnston VK, Moore EL, Mosser SD, Burgey CS, Paone DV, Shaw AW, Graham SL, Vacca JP, Williams TM, Koblan KS, Kane SA (2008) Pharmacological characterization of MK-0974 [N-[(3R,6S)-6-(2,3-difluorophenyl)-2-oxo-1-(2,2,2-trifluoroethyl)azepan-3- yl]-4-(2-oxo-2,3-dihydro-1H-imidazo[4,5-b]pyridin-1-yl)piperidine-1-carbox amide], a potent and orally active calcitonin gene-related peptide receptor antagonist for the treatment of migraine. J Pharmacol Exp Ther 324:416–421
Sang CN, Ramadan NM, Wallihan RG, Chappell AS, Freitag FG, Smith TR, Silberstein SD, Johnson KW, Phebus LA, Bleakman D, Ornstein PL, Arnold B, Tepper SJ, Vandenhende F (2004) LY293558, a novel AMPA/GluR5 antagonist, is efficacious and well-tolerated in acute migraine. Cephalalgia 24:596–602
Sarchielli P, Coata G, Firenze C, Morucci P, Abbritti G, Gallai V (1992) Serum and salivary magnesium levels in migraine and tension-type headache. Results in a group of adult patients. Cephalalgia 12:21–27
Sarchielli P, Alberti A, Russo S, Codini M, Panico R, Floridi A, Gallai V (1999) Nitric oxide pathway, Ca2+, and serotonin content in platelets from patients suffering from chronic daily headache. Cephalalgia 19:810–816
Sarsero D, Molenaar P, Kaumann AJ (1998) Validity of (−)-[3H]-CGP 12177A as a radioligand for the ‘putative β4-adrenoceptor’ in rat atrium. Br J Pharmacol 123:371–380
Saxena PR, Villalón CM (1990) Cardiovascular effects of serotonin agonists and antagonists. J Cardiovasc Pharmacol 15(Suppl 7):S17–S34
Saxena PR, Tfelt-Hansen P (2006) Triptans, 5-HT1B/1D receptor agonists in the acute treatment of migraines. In: Olesen J, Goadsby PJ, Ramadan NM, Tfelt-Hansen P, Welch KMA (eds) The headaches. Lippincott Williams & Wilkins, Philadelphia, pp 411–38
Saxena PR, Heiligers JPC, Villalón CM, Ferrari MD (1992) Effects of tertatolol, a ß-adrenoceptor antagonist with agonist affinity at 5-HT1A receptors, in an animal model of migraine: comparison with propranolol and pindolol. Eur J Pharmacol 220:79–86
Saxena PR, De Vries P, Villalón CM (1998) 5-HT1-like receptors: a time to bid goodbye. Trends Pharmacol Sci 19:311–316
Schaerlinger B, Hickel P, Etienne N, Guesnier L, Maroteaux L (2003) Agonist actions of dihydroergotamine at 5-HT2B and 5-HT2C receptors and their possible relevance to antimigraine efficacy. Br J Pharmacol 140:277–284
Schmuck K, Ullmer C, Kalkman HO, Probst A, Lubbert H (1996) Activation of meningeal 5-HT2B receptors: an early step in the generation of migraine headache. Eur J Neurosci 8:959–967
Schrader H, Stovner LJ, Helde G, Sand T, Bovim G (2001) Prophylactic treatment of migraine with angiotensin converting enzyme inhibitor (lisinopril): randomised, placebo controlled, crossover study. Brit Med J 322:19–22
Shaygannejad V, Janghorbani M, Ghorbani A, Ashtary F, Zakizade N, Nasr V (2006) Comparison of the effect of topiramate and sodium valporate in migraine prevention: a randomized blinded crossover study. Headache 46:642–648
Shepheard S, Edvinsson L, Cumberbatch M, Williamson D, Mason G, Webb J, Boyce S, Hill RG, Hargreaves RJ (1999) Possible antimigraine mechanisms of action of the 5HT1F receptor agonist LY334370. Cephalalgia 19:851–858
Shih JC, Yang W, Chen K, Gallaher T (1991) Molecular biology of serotonin 5-HT receptors. Pharmacol Biochem Behav 40:1053–1058
Silberstein SD (1998) Methysergide. Cephalalgia 18:421–435
Silberstein SD (2000) Sex hormones and headache. Rev Neurol 156(Suppl 4):4S30–4S41
Silberstein SD, Neto W, Schmitt J, Jacobs D (2004) Topiramate in migraine prevention: results of a large controlled trial. Arch Neurol 61:490–495
Silva AP, Cavadas C, Grouzmann E (2002) Neuropeptide Y and its receptors as potential therapeutic drug targets. Clin Chim Acta 326:3–25
Simonneaux V, Ebadi M, Bylund DB (1991) Identification and characterization of α2D-adrenergic receptors in bovine pineal gland. Mol Pharmacol 40:235–241
Smith GW, Farmer JB, Ince F, Matu K, Mitchell PD, Naya I, Springthorpe B (1990) FPL 63012AR: a potent D1-receptor agonist. Br J Pharmacol 100:295–300
Smith LJ, Henderson JA, Abell CW, Bethea CL (2004) Effects of ovarian steroids and raloxifene on proteins that synthesize, transport, and degrade serotonin in the raphe region of macaques. Neuropsychopharmacology 29:2035–2045
Somerville BW (1975) Estrogen-withdrawal migraine. II. Attempted prophylaxis by continuous estradiol administration. Neurology 25:245–250
Somerville BW, Herrmann WM (1978) Migraine prophylaxis with lisuride hydrogen maleate—a double blind study of Lisuride versus placebo. Headache 18:75–79
Spedding M, Bonner TI, Watson SP (2002) International Union of Pharmacology. XXXI. Recommendations for the nomenclature of multimeric G protein-coupled receptors. Pharmacol Rev 54:231–232
Srikiatkhachorn A, Suwattanasophon C, Ruangpattanatawee U, Phansuwan-Pujito P (2002) 5-HT2A receptor activation and nitric oxide synthesis: a possible mechanism determining migraine attacks. Headache 42:566–574
Stellar S, Ahrens SP, Meibohm AR, Reines SA (1984) Migraine prevention with timolol. A double-blind crossover study. JAMA 252:2576–2580
Stewart WF, Lipton RB, Celentano DD, Reed ML (1992) Prevalence of migraine headache in the United States. Relation to age, income, race, and other sociodemographic factors. JAMA 267:64–69
Stiles GL, Caron MG, Lefkowitz RJ (1984) β-adrenergic receptors: biochemical mechanisms of physiological regulation. Physiol Rev 64:661–743
Storer RJ, Goadsby PJ (1999) Trigeminovascular nociceptive transmission involves N-methyl-d-aspartate and non-N-methyl-d-aspartate glutamate receptors. Neuroscience 90:1371–1376
Storer RJ, Akerman S, Goadsby PJ (2004a) Calcitonin gene-related peptide (CGRP) modulates nociceptive trigeminovascular transmission in the cat. Br J Pharmacol 142:1171–1181
Storer RJ, Akerman S, Shields KG, Goadsby PJ (2004b) GABAA receptor modulation of trigeminovascular nociceptive neurotransmission by midazolam is antagonized by flumazenil. Brain Res 1013:188–193
Sudilovsky A, Elkind AH, Ryan RE Sr, Saper JR, Stern MA, Meyer JH (1987) Comparative efficacy of nadolol and propranolol in the management of migraine. Headache 27:421–426
Takenaka T, Forster H, Epstein M (1993) Characterization of the renal microvascular actions of a new dopaminergic (DA1) agonist, YM435. J Pharmacol Exp Ther 264:1154–1159
Tallaksen-Greene SJ, Young AB, Penney JB, Beitz AJ (1992) Excitatory amino acid binding sites in the trigeminal principal sensory and spinal trigeminal nuclei of the rat. Neurosci Lett 141:79–83
Tanoue A, Koshimizu TA, Shibata K, Nasa Y, Takeo S, Tsujimoto G (2003) Insights into α1-adrenoceptor function in health and disease from transgenic animal studies. Trends Endocrinol Metab 14:107–113
Tepper SJ (2001) Safety and rational use of the triptans. Med Clin North Am 85:959–970
Terrón JA, Bouchelet I, Hamel E (2001) 5-HT7 receptor mRNA expression in human trigeminal ganglia. Neurosci Lett 302:9–12
Terwindt GM, Ophoff RA, van Eijk R, Vergouwe MN, Haan J, Frants RR, Sandkuijl LA, Ferrari MD (2001) Involvement of the CACNA1A gene containing region on 19p13 in migraine with and without aura. Neurology 56:1028–1032
Tfelt-Hansen P, Rolan P (2006) β-Adrenoceptor blocking drugs in migraine prophylaxis. In: Olesen J, Goadsby PJ, Ramadan NM, Tfelt-Hansen P, Welch KMA (eds) The headaches. Lippincott Williams & Wilkins, Philadelphia, pp 519–528
Tfelt-Hansen P, Standnes B, Kangasneimi P, Hakkarainen H, Olesen J (1984) Timolol vs propranolol vs placebo in common migraine prophylaxis: a double-blind multicenter trial. Acta Neurol Scand 69:1–8
Thomas DR (2006) 5-ht5A receptors as a therapeutic target. Pharmacol Ther 111:707–714
Thomas DR, Hagan JJ (2004) 5-HT7 receptors. Curr Drug Targets CNS Neurol Disord 3:81–90
Tronvik E, Stovner LJ, Helde G, Sand T, Bovim G (2003) Prophylactic treatment of migraine with an angiotensin II receptor blocker: a randomized controlled trial. JAMA 289:65–69
Tzourio C, El Amrani M, Poirier O, Nicaud V, Bousser MG, Alperovitch A (2001) Association between migraine and endothelin type A receptor (ETA −231 A/G) gene polymorphism. Neurology 56:1273–1277
Uddman R, Edvinsson L, Ekman R, Kingman T, McCulloch J (1985) Innervation of the feline cerebral vasculature by nerve fibers containing calcitonin gene-related peptide: trigeminal origin and co-existence with substance P. Neurosci Lett 62:131–136
van de Ven LL, Franke CL, Koehler PJ (1997) Prophylactic treatment of migraine with bisoprolol: a placebo-controlled study. Cephalalgia 17:596–599
van den Broek RWM, Bhalla P, MaassenVanDenBrink A, de Vries R, Sharma HS, Saxena PR (2002) Characterization of sumatriptan-induced contractions in human isolated blood vessels using selective 5-HT1B and 5-HT1D receptor antagonists and in situ hybridization. Cephalalgia 22:83–93
van den Maagdenberg AM, Haan J, Terwindt GM, Ferrari MD (2007) Migraine: gene mutations and functional consequences. Curr Opin Neurol 20:299–305
Vargas HM, Gorman AJ (1995) Vascular α1 adrenergic receptor subtypes in the regulation of arterial pressure. Life Sci 57:2291–2308
Villalón CM, Centurión D (2007) Cardiovascular responses produced by 5-hydroxytriptamine:a pharmacological update on the receptors/mechanisms involved and therapeutic implications. Naunyn-Schmiedeberg’s Arch Pharmacol 376:45–63
Villalón CM, Bom AH, Heiligers JPC, Den Boer MO, Saxena PR (1990) Constriction of porcine arteriovenous anastomoses by indorenate is unrelated to 5-HT1A, 5-HT1B, 5-HT1C or 5-HT1D receptor subtypes. Eur J Pharmacol 190:167–176
Villalón CM, Centurión D, Valdivia LF, De Vries P, Saxena PR (2002) An introduction to migraine: from ancient treatment to functional pharmacology and antimigraine therapy. Proc West Pharmacol Soc 45:199–210
Villalón CM, Ramírez-San Juan E, Sanchez-Lopez A, Bravo G, Willems EW, Saxena PR, Centurión D (2003) Pharmacological profile of the vascular responses to dopamine in the canine external carotid circulation. Pharmacol Toxicol 92:165–172
Wackenfors A, Jarvius M, Ingemansson R, Edvinsson L, Malmsjo M (2005) Triptans induce vasoconstriction of human arteries and veins from the thoracic wall. J Cardiovasc Pharmacol 45:476–484
Weinshank RL, Zgombick JM, Macchi M, Adham N, Lichtblau H, Branchek TA, Hartig PR (1990) Cloning, expression, and pharmacological characterization of a human α2B-adrenergic receptor. Mol Pharmacol 38:681–688
Weiss B, Alt A, Ogden AM, Gates M, Dieckman DK, Clemens-Smith A, Ho KH, Jarvie K, Rizkalla G, Wright RA, Calligaro DO, Schoepp D, Mattiuz EL, Stratford RE, Johnson B, Salhoff C, Katofiasc M, Phebus LA, Schenck K, Cohen M, Filla SA, Ornstein PL, Johnson KW, Bleakman D (2006) Pharmacological characterization of the competitive GLUK5 receptor antagonist decahydroisoquinoline LY466195 in vitro and in vivo. J Pharmacol Exp Ther 318:772–781
Welch KMA, Chabi E, Bartosh K, Achar VS, Meyer JS (1975) Cerebrospinal fluid gamma aminobutyric acid levels in migraine. Br Med J 3:516–517
Widdop RE, Jones ES, Hannan RE, Gaspari TA (2003) Angiotensin AT2 receptors: cardiovascular hope or hype. Br J Pharmacol 140:809–824
Willems EW, Valdivia LF, Saxena PR, Villalón CM (2001a) The role of several α1- and α2-adrenoceptor subtypes mediating vasoconstriction in the canine external carotid circulation. Br J Pharmacol 132:1292–1298
Willems EW, Heiligers JPC, De Vries P, Kapoor K, Tom B, Villalón CM, Saxena PR (2001b) α1-Adrenoceptor subtypes mediating vasoconstriction in the carotid circulation of anaesthetized pigs: possible avenues for antimigraine drug development. Cephalalgia 21:110–119
Willems EW, Valdivia LF, Villalón CM, Saxena PR (2002) α-Adrenoceptors and acute migraine therapy. Drug News Perspect 15:140–146
Willems EW, Valdivia LF, Villalón CM, Saxena PR (2003) Possible role of alpha-adrenoceptor subtypes in acute migraine therapy. Cephalalgia 23:245–257
Würz R, Benmalek R, Grotemeyer KH, Foh M (1991) Bisoprolol and metoprolol in the prophylactic treatment of migraine with and without aura—a randomized double-blind cross-over multicenter study. Cephalalgia 11:152–153
Yanagisawa M, Kurihara H, Kimura S, Tomobe Y, Kobayashi M, Mitsui Y, Yazaki Y, Goto K, Masaki T (1988) A novel potent vasoconstrictor peptide produced by vascular endothelial cells. Nature 332:411–415
Yu CY, Boyd NM, Cringle SJ, Su EN, Alder VA, Yu DY (2002) Agonist-induced vasoactive responses in isolated perfused porcine dental pulpal arterioles. Arch Oral Biol 47:99–107
Zhang Y, Bhavnani BR (2005) Glutamate-induced apoptosis in primary cortical neurons is inhibited by equine estrogens via down-regulation of caspase-3 and prevention of mitochondrial cytochrome c release. BMC Neurosci 6:13
Zhang Z, Winborn CS, Marquez de Prado B, Russo AF (2007) Sensitization of calcitonin gene-related peptide receptors by receptor activity-modifying protein-1 in the trigeminal ganglion. J Neurosci 27:2693–2703
Zimmermann K, Reeh PW, Averbeck B (2002) ATP can enhance the proton-induced CGRP release through P2Y receptors and secondary PGE2 release in isolated rat dura mater. Pain 97:259–265
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Mehrotra, S., Gupta, S., Chan, K.Y. et al. Current and prospective pharmacological targets in relation to antimigraine action. Naunyn-Schmied Arch Pharmacol 378, 371–394 (2008). https://doi.org/10.1007/s00210-008-0322-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00210-008-0322-7