Abstract
Bisphenol A (BPA) is an endocrine-disrupting chemical (EDC) and one of the most produced synthetic compounds worldwide. BPA can be found in epoxy resins and polycarbonate plastics, which are frequently used in food storage and baby bottles. However, BPA can bind mainly to estrogen receptors, interfering with various neurologic functions, its use is a topic of significant concern. Nonetheless, the neurotoxicity of BPA has not been fully understood despite numerous investigations on its disruptive effects. Therefore, this review aims to highlight the most recent studies on the implications of BPA on the neurologic system. Our findings suggest that BPA exposure impairs various structural and molecular brain changes, promoting oxidative stress, changing expression levels of several crucial genes and proteins, destructive effects on neurotransmitters, excitotoxicity and neuroinflammation, damaged blood–brain barrier function, neuronal damage, apoptosis effects, disruption of intracellular Ca2+ homeostasis, increase in reactive oxygen species, promoted apoptosis and intracellular lactate dehydrogenase release, a decrease of axon length, microglial DNA damage, astrogliosis, and significantly reduced myelination. Moreover, BPA exposure increases the risk of developing neurologic diseases, including neurovascular (e.g. stroke) and neurodegenerative (e.g. Alzheimer’s and Parkinson’s) diseases. Furthermore, epidemiological studies showed that the adverse effects of BPA on neurodevelopment in children contributed to the emergence of serious neurological diseases like attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorder (ASD), depression, emotional problems, anxiety, and cognitive disorders. In summary, BPA exposure compromises human health, promoting the development and progression of neurologic disorders. More research is required to fully understand how BPA-induced neurotoxicity affects human health.
Similar content being viewed by others
Introduction
According to the World Health Organization, stroke, or brain attack, is the most common neurovascular disease, the second most prevalent cause of death, and the third leading cause of long-term disability in the world. Unfortunately, the percentage of stroke victims is expected to increase in the next decade, affecting younger and younger patients (Sarikaya et al. 2015). Most strokes are Ischemic Stroke, approximately 70%, are caused by occlusion of the major cerebral artery, usually, the middle cerebral artery, leaving Haemorrhagic stroke, affecting about 30%, which forms lesions in the brain substance or subarachnoid space, among other rarer types in very small numbers (Iadecola et al. 2020).
Neurovascular diseases are a type of neurological disease and are of extreme concern to humans, as they can be fatal or cause permanent disability. Neurovascular diseases affect the cerebral vascular system and the spinal cord. These diseases can be caused by deformations in the endothelium layer, smooth muscle layer of blood vessels, and other molecular bases of pathogenesis (Sam et al. 2015). Apart from strokes, the most common neurovascular diseases are aneurysms, arteriovenous malformations, intracranial dural arteriovenous shunts, and spinal cord arteriovenous shunts, nevertheless, there are many other rarer neurovascular diseases (Song et al. 2021; van den Berg 2003). Most neurological diseases can arise from exposure to environmental chemicals or genetic predisposition (Yirun et al. 2021). Thus, recent studies highlight the role of vascular dysfunction in several neurodegenerative diseases, like Alzheimer’s and Parkinson’s, because the nervous and vascular systems are functionally interdependent and have close anatomical apposition as well as similar molecular pathways (Ahmad et al. 2020). Moreover, neurodevelopmental diseases, another type of neurologic disease, significantly impact children. The neurodevelopmental disorders more predominant are attention-deficit/hyperactivity disorder (ADHD), autism spectrum disorder (ASD), intellectual disability, and learning and communication disorders (Hansen et al. 2021; Thapar et al. 2017). These disorders significantly influence the lives of those who are affected and are linked to decreased daily functioning, academic performance, and life quality (Escobar et al. 2005).
Endocrine disruptors (EDCs), are synthetic or natural chemicals, usually environmental pollutants, that affect the endocrine system when exposed to humans from multiple sources, like atmosphere, water and effluents, food, drinking water, and dust, predominantly through breathing and food, acting to block endogenous hormones, and therefore can disrupt normal hormonal homeostasis, reproduction, and behaviour. EDCs have been severely used for various functions in recent decades, which facilitates their exposure to animals and humans (Klenke et al. 2016; Michałowicz 2014).
Of all the endocrine disruptors, bisphenol A (BPA) is a xenoestrogen that is one of the most produced synthetic compounds worldwide, with annual production exceeding 3.8 million tons and a release to the atmosphere of 100 tons in the same period (Michałowicz 2014; Vandenberg et al. 2010). BPA is mostly used as a monomer in the production of polycarbonate plastics and epoxy resins (Hoekstra and Simoneau 2013; Michałowicz 2014; Vandenberg et al. 2010). It is designated by IUPAC as 4,4′-ispropylidenediphenol (see Fig. 1), being a ubiquitous carbon-based chemical with chemical formula C15H16O2, formed by two phenol groups, with excellent physical and chemical properties (Banerjee et al. 2022; Campanale et al. 2020). Historically, BPA was synthesized in 1891 by a Russian chemist named Alexander Dianin, but it was not until about forty years later that some estrogenic effects were discovered (Rubin 2011). Nevertheless, this EDC is still used today because of the mechanical characteristics, low moisture absorption, elasticity and thermal resistance it provides to plastics (Michałowicz 2014).
As for its physicochemical characteristics, BPA is a chemical compound with a 228.29 g/cm3 molecular mass. Visually, BPA is white, solid, and crystalline. It has a melting point of 156 °C, with a boiling point of 220 °C (at a pressure of 5 hPa). Additionally, its water-octanol coefficient expressed in logarithmic form is 3.32 (log P = 3.32), which shows good solubility capabilities in fats and low water solubility, with about 200 mg/dm3 at 25 °C. Since BPA is a phenol, which can be converted to ethers, esters and salts, it has hydroxyl residues directly linked to its aromatic ring, which designates good reactivity to this compound (Fonseca et al. 2022). BPA binds to estrogen receptors such as ERα, ERβ, ERγ, G-protein-coupled estrogen receptor (GPR30) and peroxisome proliferator-activated receptor gamma (PPAR-γ) (Acconcia et al. 2015). The mechanisms of action are not yet fully understood, but several studies seem to show that BPA can induce insulin resistance, adipogenesis, pancreatic-β-cell dysfunction, inflammation, and oxidative stress (Banerjee et al. 2022).
Several studies have already reported numerous effects of BPA on various systems in the human body and in animals, as daily exposure to BPA has proven to be a major public health concern given its ubiquity and endocrine-disrupting properties (mainly estrogenic). However, the effect of BPA on the brain system is still an understudied topic, but it has been recognized that environmental exposure to BPA may affect some brain functions, interfering with brain development and physiology after bypassing endogenous defence mechanisms and may require exogenous interventions and that it may also be related to the prevalence of stroke (Cai et al. 2020; Di Pietro et al. 2020; Santoro et al. 2019). BPA neurotoxicity occurs in the brain system by reducing synaptic plasticity, inhibiting neurogenesis, creating oxidative stress, and inducting autophagy and apoptosis (Santoro et al. 2019). As such, we aim to address the disruptive effects of BPA on the human brain system by reviewing the current literature based on experimental studies in humans and animals and epidemiological data, with a focus on the underlying molecular mechanisms.
Approach to the review
In this review, were presented and summarized experimental studies that evaluated the neurological effects caused by BPA exposure in animal, and human models, in Topic 3 and 4, respectively. In vitro and in vivo studies were the subtopics for this research looking at the effects of BPA exposure in animal models, while epidemiological studies and human cell lines were used as human models. A literature review was performed based on articles available in PubMed databases. The search strategy was carried out using Boolean operators “AND”, “OR”, and “NOT” and a combination of terms relating to Bisphenol A (“bisphenol A”, “BPA”, “neurotoxic”, “endocrine disruptor compound”) with brain system (“middle cerebral artery”, “vascular”, “vascular smooth muscle”, “smooth muscle cells”, “smooth muscle”, “brain”, “neurodevelopmental”) and neurovascular diseases (“stroke”, “cerebral infarction”, “vascular neurology”, “brain attack”, “neurodevelopmental diseases”, “neurodevelopment disorders”).
These terms were added to, along with the citations from the publications that were found through the search.
The inclusion criteria were: (1) the article was original; (2) the study was performed on in vivo animal models, in vitro models, or using epidemiological data; (3) the concentrations of exposure to BPA were well defined; (4) the studies had a control group; (5) the study analyses the neurological outcomes associated with exposure to BPA; (6) the study may also assess the effects associated with exposure to others EDCs; (7) the study evaluated the effects of BPA substitutes on other organ systems and characteristics; (8) the article was written in English. On the other hand, the exclusion criteria were: (1) the article was not original (e.g. review, editorial, and commentary); (2) studies including previous diseases or susceptible conditions without a control group; (3) the concentrations of exposure to BPA was not well established; (4) the study took place in the enteric nervous system, midgut or peripheral nervous system; (5) articles were duplicates, unrelated, inaccessible, or not written in English.
These inclusion and exclusion criteria were applied when each retrieved article's title, abstract, and materials and techniques were analysed.
Exposure to BPA
The production and use of BPA have progressively increased every year, and this EDC is used in more and more types of materials, also expanding the number of contamination pathways, both through the use and wear of the containers, and through the pollution caused when they are disposed of in the aquatic, marine, air, and soil ecosystems (Le et al. 2008; Xing et al. 2022; Zhang et al. 2022a). Its existence in nature is only associated with human production activities, i.e. anthropogenic (Xing et al. 2022).
BPA is mostly used as a monomer in the production of polycarbonate plastics and epoxy resins used in the manufacture of dental fissure sealants, water supply pipes, adhesives, water bottles, food containers, electronic equipment, children’s toys, medical equipment, thermal paper, and others (Michałowicz 2014; Vandenberg et al. 2007). The most common contact consumers have with BPA is through the reuse of polycarbonate bottles and kitchen utensils, such as containers for use in the preservation and preparation of beverages and food or baby bottles, but they can also be subjected to this EDC through atmospheric air when it is in the gas form (Hoekstra and Simoneau 2013; Xing et al. 2022). Exposure to BPA can occur, most usually, by oral exposure through the ingestion of contaminated food and beverages or by skin contact or inhalation, and later accumulates in biological tissues, with likely long-term negative effects (Chianese et al. 2018b; Nunez et al. 2001). BPA can be released from containers when residues of the monomer in the polymer move into food and beverages, usually when the container is heated together with its contents, which in turn hydrolyse the polymer, promoting the release of BPA, or by diffusion of residual BPA present in the polycarbonate after the container manufacturing process (Hoekstra and Simoneau 2013; Xing et al. 2022).
In most cases, exposure to BPA is continuous, and its metabolites are detectable in about 90% of the world's population, but the degree of exposure to BPA may depend on socioeconomic factors, lifestyles, health status, exposure pathways and diet (Calafat et al. 2008; Ramadan et al. 2020). BPA is excreted mostly in urine as glucuronide/sulphate conjugates, occurs mostly within 24 h, has an estimated biological half-life of approximately 6 h, and is often used for biomonitoring studies (Braun 2017; Ramadan et al. 2020; Thayer et al. 2015). However, the small part that is not excreted, can be found in other biological fluids in lower concentration, such as maternal blood, maternal urine, amniotic liquid, placental tissue, umbilical cord blood, breast milk and human colostrum (Lorigo and Cairrao 2022; Santoro et al. 2019; Völkel et al. 2002). Regarding the concentrations of BPA that can be found at the brain level, Geens et al. (2012) detected BPA in the brain (0.91 ng/g) in samples taken in 2002 during the autopsy of eleven patients at the University Hospital of Antwerp (Geens et al. 2012). Furthermore, in a more detailed investigation of brain tissue, Kim et al. (2004), analysed the brains of Nulliparous Fischer 344 female rats administering an oral dose of 100 mg/kg BPA (see Fig. 2), and detected BPA accumulation after 48 h in plasma (0.540 μg/g), pituitary (0.745 μg/g tissue), hypothalamus (0.180 μg/g tissue), brain stem (0.103 μg/g tissue), cerebellum (0.102 μg/g tissue), frontal cortex (0.097 μg/g tissue), hippocampus (0.181 μg/g tissue) and caudate nucleus (0.220 μg/g tissue) (Kim et al. 2004).
Accumulation of BPA in several brain regions 48 h after oral administration of 100 mg BPA/kg. The amount of BPA in each compartment is indicated as a μg BPA/g tissue. Data obtained by Kim et al. (2004). Figure created with PowerPoint version 2204 and using pictures from Servier Medical Art. Servier Medical Art by Servier, licensed under a Creative Commons Attribution 3.0 Unported License (https://creativecommons.org/licenses/by/3.0/)
Although there are several exposure pathways to BPA, most of the currently detected environmental concentrations of this compound for humans are below the current tolerable daily intake value of 0.2 ng per kilogram of body weight, established by the European Food Safety Authority (EFSA) in April 2023, a drastic reduction from the 4 μg/kg body weight/day established in 2015 (Kodila et al. 2023; Lambré et al. 2023; Silano et al. 2016). However, the tolerable daily intake rate is not completely reliable and safe, since the effects of BPA exposure are not always dose-dependent, as BPA has non-monotonic effects (Lorigo and Cairrao 2022), and BPA analogues have been developed to replace its use. However, these substitutes also appear not to be free of adverse effects, notably Bisphenol AF (BPAF) which shows higher neurotoxicity than BPA, but Bisphenol S (BPS) exhibits weaker neurotoxicity. Therefore, BPAF, BPF, and other analogues should be carefully considered as an alternative to BPA (Sam et al. 2015; Santoro et al. 2019).
The main harmful effects of BPA and its analogues are their acute and chronic effects on the brain, which is the organ responsible for controlling other organs, processing information, and supplying rapid and coordinated responses. An intricate neuronal network is formed during embryogenesis, but only in the postnatal period does the brain fully develop. Thus, the protection of neuronal cells and synaptic plasticity is crucial for healthy brain development. Conversely, neuronal damage, loss of synapses, and neurological disturbances are indicative of the development of neurological disorders and cognitive decline at the foetal level and later in the future generation (Chianese et al. 2018a; D'Angelo et al. 2019). Thus, in the prenatal phase, due to maternal exposure to BPA during the mother’s pregnancy, BPA crosses the blood–brain barrier and placenta (Balakrishnan et al. 2010) and is detected in the breast milk (Ye et al. 2006), and in the first years of a child's life, its neurodevelopment and normal behaviour can be compromised In this regard, exposure to EDCs during pregnancy is defined as “prenatal exposure” and can be subdivided into “maternal exposure” and “foetal exposure” (Lorigo and Cairrao 2022). In addition, common to the other EDCs, modulation of hormonal action by BPA occurs by specific cellular and molecular mechanisms, which may have additive, synergistic or negative biological effects. Consequently, the hormonal processes and signalling pathways that support the physiological changes that occur during pregnancy are affected, giving this EDC the possibility to increase maternal susceptibility and the risk of developing other complications in pregnancy, also affecting the foetus in the future (Lorigo and Cairrao 2022). Animal studies suggest that prenatal exposure to low doses of BPA may alter brain structure and function, and thus disrupt neurobehavioral development (Kundakovic and Champagne 2011; Kundakovic et al. 2013), whereas epidemiological studies have found the effect of maternal exposure to BPA at different times during pregnancy on neurobehavioral problems at children of different ages, especially in boys, often linking it to neurodevelopmental disorders (Evans et al. 2014; Harley et al. 2013; Jensen et al. 2019; Philippat et al. 2017).
Regarding the mode of action of this EDC, it can bind mainly to estrogen-activated receptors (ER), α and β (ERα and ERβ) and GPR30 receptors (Cimmino et al. 2020), and thanks to its chemical structure, BPA interacts as an antagonist or agonist, via a receptor-dependent signalling pathway. This EDC can also interact with other receptors, such as the androgen receptor (AR), estrogen-related receptor gamma (ERRγ), thyroid hormone receptor (THR), glucocorticoid receptor (GR) (Prasanth et al. 2010; Zhang et al. 2023), progesterone receptor (PR) (Huang et al. 2022a) and PPAR-γ (Acconcia et al. 2015; Di Pietro et al. 2020; Rubin 2011; Santoro et al. 2019). Still, the chemical structure of BPA may be an advantage, because BPA cannot adequately reach the boundaries of the hormone-binding site, only inducing a shift of α-helices forming the ligand-binding domain (LBD) (Acconcia et al. 2015). Overall, EDCs have three levels of key fragments: primary, secondary, and tertiary fragments. The secondary fragments are responsible for binding to receptors, which discriminate between active and inactive compounds, while the tertiary ones determine the type of activity, i.e., whether it is agonist, antagonist, or agonist–antagonist. This is defined by the interaction of EDCs with functional lobes, directly affecting the surface of AF-2, which handles the recruitment of coregulators. BPA holds primary fragments of oxygen-containing aromatics and secondary fragments (Bisphenol group). The activation of BPA, as an active compound, is given due to the coexistence of primary and secondary fragments. Through interactions of the secondary fragment of BPA, conformations stabilized in LBD, activation of the estrogen receptor and androgen receptor is achieved by forming hydrogen bonds with the amino acid R394 and via van der Waals interactions with the amino acid N705, respectively. Understanding the secondary fragments that form the LBD amino acid interaction network is critical to the activity of BPA. BPA ligand fragments interact with LBD causing changes in the conformation of the AF-2 surface, collecting two cofactors and identifying its tertiary fragment (agonist–antagonist activity) (Acconcia et al. 2015; Tan et al. 2020).
Similar to natural hormones, several experimental studies with BPA indicate a non-monotonic response, emphasizing the need for risk assessment with exposures from low to high dosages, given the typical U-shaped response also observed by other EDCs (Vandenberg 2014). However, this particularity may complicate the assessment of BPA toxicity risk, since this EDC can interact with hormone receptors on specific cell types and/or exhibit multiple biological endpoints with linear dose–response that cumulatively constitute a non-monotonic dose–response relationship (Cooper and Posnack 2022).
For these reasons, there has been increasing concern lately about the adverse effects of BPA exposure on human health. Accordingly, the European Food Safety Authority (EFSA) and the U.S. Food and Drug Administration (FDA) have imposed restrictions on the production and use of this EDC in infant feeding bottles and/or food plastic containers. These restrictions have also been adopted by other countries, such as Austria, Colombia, Canada, Denmark, France, and Belgium. Denmark and Sweden have also restricted the use of varnishes and coatings in food packaging for children (Boudalia and Malha 2016; Oliviero et al. 2022; Usman and Ahmad 2016).
That said, given the characteristics of BPA as an EDC and its continued exposure to humans, the endocrine-disrupting effects of BPA on the cerebral vascular system will be described in the following sections for animal models (Sect. Effects of BPA on Animal Models) and human models (Sect. Effects of BPA on Humans).
Effects of BPA on animal models
Several studies have linked exposure to BPA to adverse effects on human health, mainly on neural, immune and metabolic systems, reproductive organs, and various cancers (Xing et al. 2022). However, recent evidence has also revealed a link between BPA exposure and neurovascular diseases, such as stroke, neurodegenerative diseases, like Alzheimer’s and Parkinson’s, and neurodevelopmental disorders, such as ASD and ADHD, for example (Cai et al. 2020).
In vitro and in vivo models are currently used to classify a substance as toxic. Therefore, in this section, we will address the neurotoxic effects of BPA in animals.
In vitro studies
Exposure to BPA in animals has been reported in rodents, fish, and canines. In vitro studies are an indispensable tool for studying mechanistic pathways and can offer a faster and more flexible approach to human health effects. This type of study usually consists of exposing a certain type of cells to BPA. The in vitro studies analysed in this review have shown two major consequences caused by BPA exposure, regarding neuronal development and morphology, i.e., cell damage, and decreased cell viability, among others.
Neurodevelopmental effects
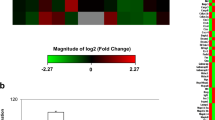
Concerning neuronal development, the first in vitro study analysed was conducted by Mathisen GH et al. The authors aimed to investigate whether prenatal exposure to BPA disrupted the neurodevelopment of the cerebellum. Thus, they exposed in vitro chicken embryos to BPA while still in the egg and prepared cerebellar granule cell cultures 24 h later. Experimentally, the authors saw that the level of Pax6 (a paired homeobox DNA binding protein) increased on day 6, and thus disrupted cerebellar development. Pax6 participates in the creation of neural circuits, neuronal migration, and brain patterning (Mathisen et al. 2013). In the same sense, Yin et al. analysed the effect of BPA exposure on mouse embryonic stem cells. These authors showed that BPA (1–10 μmol/L) affects the differentiation of germ layers during embryonic development, as well as the formation of neural ectoderm and neural progenitor cells. The authors concluded that studies in stem cells can be a powerful system for detecting the toxicity of environmental pollutants, such as BPA (Yin et al. 2015). In rat hippocampal neural stem cells (NSCs) Tiwari et al. studied the effect of BPA and concluded that exposure to 100 μM BPA significantly reduces the proliferation of NSCs, which reduces nestin, reelin, and Pax6 gene expression in the hippocampal region. Moreover, BPA also had inhibitory effects on neuronal differentiation, decreasing the number of newly born neurons and reducing long-term survival and further promoting increased phosphorylation of β-catenin, decreased levels of GSK-3β and nuclear translocation of β-catenin (Tiwari et al. 2016). Agarwal et al. in the same cells, found that chronic exposure to BPA (100 μM) impaired autophagy-mediated mitochondrial renewal, leading to increased oxidative stress, mitochondrial fragmentation, and apoptosis. Additionally, BPA also inhibited the proliferation and differentiation by decreasing the number of BrdU- and β-III tubulin-positive cells increasing levels of Drp-1 (dynamin-related protein 1) and increasing its mitochondrial translocation (which is associated with enhanced neurodegeneration and pathogenesis of neurodegenerative disorders), without difference in the hippocampus and in vitro levels for Fis-1, Mfn-1, Mfn-2, and Opa-1 (Agarwal et al. 2016). Furthermore, in the same cells from rat foetal, a comparison study of neurodevelopmental effects (cell proliferation, differentiation, and morphometric parameters) of BPA and Bisphenol F (BPF) was performed. The increase in cell proliferation and impact on differentiation rates of oligodendrocytes and neurons in a concentration-dependent manner was observed. Thus, the authors concluded that BPA and BPF induced similar changes in cell differentiation, proliferation and arborization (Gill and Kumara 2021). On the other hand, in gonadotropin-releasing hormone (GnRH) neurons, Klenke et al. investigated the effects of BPA on their activity using an explant model with a large number of primary GnRH neurons. These types of neurons are essential for reproduction, serving as an important link between the brain, pituitary, and gonads. These authors found that exposure to 50 μM of BPA significantly decreased calcium (Ca2+) activity and the GnRH neuronal activity, which occurred independently of estrogen receptors, GPER or ERRγ, via a non-canonical pathway, demonstrating a direct effect of BPA on GnRH neurons (Klenke et al. 2016). Conversely, Pang et al. investigated the transcriptional behaviour of long non-coding RNAs (lncRNAs) and mRNAs and discovered 151 lncRNAs and 794 mRNAs differentially expressed in the BPA-exposed group (2.5–200 μM). The differentially expressed mRNAs were involved mostly in basic metabolic processes as well as physiological and pathological conditions such as development, synaptic transmission, homeostasis, injury, and neuroinflammation responses (Pang et al. 2018). Besides, Cho et al. developed a method capable of effectively detecting neurotoxicity at low concentrations of BPA, in primary cultured mouse neurons. Thus, exposure to lower doses (50 µM and 100 µM) induced toxicity for developing neurons, especially impaired neuronal maturation in neural progenitor cells (Cho et al. 2018). In another in vitro study, the molecular mechanisms underlying the neurotoxicity of BPA and some analogues were investigated. The data show that 100 μM of BPA induced a 1.46-fold increase in O-GlcNAcase (OGA) protein level compared to the control. This protein performs a significant part in regulating neural activities at multiple levels, ranging from cellular processes to animal behaviours. Maintaining correct amounts of O-GlcNAcylation is necessary for embryonic development because a deficiency of OGA in mice causes mortality during embryogenesis or perinatal lethality, and therefore this OGA value is worrying. (Gu et al. 2019). Moreover, axon growth to assess the toxic effects of BPA (5 or 10 μM) on central nervous system (CNS) function and the role of protein disulfide isomerase (PDI) S-nitrosylation in BPA-induced neurotoxicity was studied. The authors concluded that BPA induced S-nitrosylation of PDI, while NG-monomethyl-l-arginine (L-NMMA), an inhibitor of nitric oxide synthases (NOS), exerted the opposite effects. However, BPA inhibited the growth of PC12 neurites, while L-NMMA reversed this inhibition (Kobayashi et al. 2020). On the other hand, in transgenic zebrafish cell lines, the neurotoxicity of 200 μg/L of BPA, BPF, BPAF and BPS was analysed, to complete the in vivo study, which will be mentioned in the next section. As a result, treatment with bisphenols led to significant reductions in green fluorescent protein (GFP) expression in the brain and spinal cord. GFP plays a key role in the development of zebrafish motor neurons. Similarly, the axon lengths of motoneurons at 36 h post-fertilization (hpf) were reduced by 40.4%, 25.2%, 33.0% and 46.2%, for BPA, BPS, BPF, and BPAF, respectively. (Gu et al. 2022). Conversely, in oligodendroglial cell lines (oli-neu), was examined how BPA affected their differentiation. BPA incubation decreased the amount of sulfatide and phosphatidylinositol in plasmalogen and changed the ratio of monounsaturated/polyunsaturated fatty acids in phospholipids, suggesting that BPA interferes with early oligodendrocyte differentiation’s lipid remodelling process (Naffaa et al. 2022). Furthermore, by treating PC12 cells, which is a cell line derived from a pheochromocytoma of the rat adrenal medulla, with BPA at 1 μM for 36 h, Bi et al. proved that exposure to this concentration of BPA impaired the neurite growth by decreasing primary and secondary branches. In addition, BPA exposure decreased the level of Ac-H3K9 by increasing the expression of HDAC2 (Bi et al. 2022).
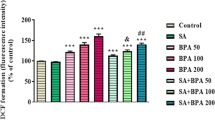
Morphological effects
Regarding the morphology effects caused by BPA, 11 studies were conducted. Khan et al. showed that, in the C8-D1A mouse astrocyte cell line, BPA-induced cell damage (30 μM), such as cell loss, shorter cellular processes, and cell shrinkage, increased SYTOX-positive astrocytes and increased cell death by approximately 77% and expression of glial fibrillary acidic protein (GFAP) (Khan et al. 2018). Moreover, in mouse hippocampal HT-22 cell lines, the toxicity of BPA and its analogues showed that BPA, BPS and Bisphenol B (BPB) exposure increased reactive oxygen species (ROS) levels and apoptosis rates, damaged the cell membrane, and inhibited the proliferation (Pang et al. 2019). In another in vitro study, mouse neural stem cells were exposed to BPA and curcumin. The data showed a significantly decreased size and number of oligospheres in the BPA-treated group (100 μM) and a significant increase in the BPA + curcumin group. Additionally, a significantly decreased number of PDGFRα/PCNA + cells in the BPA-treated group was observed, while a significant increase in the BPA + curcumin group, suggesting that cell death was more prevalent in the presence of BPA (Tandon et al. 2020). In cultured Neuro-2a cells, which are a mouse cell line derived from mouse neuroblastoma tissue, Yin et al. assessed the effects of several concentrations of BPA (50, 100, 150, or 200 μM) on synaptic development and cytoskeleton. As a result, BPA altered synapse morphology by regulating synaptophysin (SYP) expression, causing a dose-dependent toxic effect. The expression of microtubule-associated protein 2 (MAP2), Tau decreased, disrupted microtubule stability and cell proliferation was also obtained, inducing cell death (Yin et al. 2020). Furthermore, in the same cells, there was another study, which investigated the effects and mechanisms of the BPA metabolite, 4-methyl-2,4-bis(4-hydroxyphenyl)pent-1-ene (MBP), on neuronal cell growth and function. MBP, which is generated in the mammalian liver after BPA exposure, is the main active metabolite of BPA, and the data showed that MBP exerts greater toxicity than BPA. MBP exposure significantly reduced the viability of Neuro-2a cells and induced apoptotic events in which MBP (5–15 μM) showed greater neuronal cytotoxicity than BPA (50–100 μM). BPA dramatically induced annexin V-FITC binding fluorescent intensity and sub-G1 hypodiploid cell population in a dose-dependent manner and resulted in marked expression of cleaved forms of caspase 3 and 7. Thus, these results allowed us to conclude that MBP exposure exerts neuronal cytotoxicity, via the interaction of the mitochondria-dependent and ER stress-triggered apoptotic pathway, which is regulated by ERK activation and Akt inactivation, leading to neuronal cell death (Huang et al. 2021). On the other hand, in cultured N2a neurons, that have similar properties to neuro-2a cells, were also exposed to BPA, with concentrations ranging up to 100 μM. The neurotoxicity of this EDC using viability and neuronal differentiation assays was performed, and the results showed that BPA decreased cell viability and axon growth (e.g., by down-regulating MAP2 and GAP43) and that it induced neurotoxicity caused by down-regulation of Bcl-2, initiating apoptosis, causing inhibition of autophagy flux, featured by nuclear translocation of apoptosis-inducing factor (AIF), light chain 3B (LC3B) aggregation, and p62 accumulation. Therefore, the authors confirmed that BPA induces neurotoxicity of neuro2a cells characterized by the (AIF)-dependent apoptosis and p62-related autophagy defects via positive regulation of heme oxygenase-1 (HO-1) and activation of AMP kinase (AMPK) resulting in neuronal degeneration (Lee et al. 2021). Moreover, in PC12 cells, the mechanism of neuronal apoptosis induced by various BPA concentrations (1, 10, 25, 50, 75, 100, 125, 150 μM) was investigated by the group of Zhang Y. In this study, BPA exposure reduced cell viability, altered cell morphology, and aggravated intracellular lactate dehydrogenase (LDH) release, intracellular Ca2+ concentration, ROS levels, apoptosis, and reduced mitochondrial transmembrane potential (ΔΨm). Furthermore, the authors linked BPA-induced apoptosis to Nur77-mediated inhibition of the NF-κb/Bcl-2 pathway (Zhang et al. 2021b). Nevertheless, on primary rat hippocampal neurons, Meng et al. studied the oxidative damage effects of different concentrations (1, 10, 100 nM and 1, 10, 100 μM) of BPA, BPS and BPB, and additionally evaluated the effects of epigallocatechin gallate (EGCG) (5 and 6 μM for males and females, respectively) added to BPA-exposed neurons. The results of this study showed that exposure to BPA, BPS and BPB can cause increased ROS levels and malondialdehyde (MDA) contents, but significantly reduced superoxide dismutase (SOD) activity and that they can also accelerate apoptosis and reduce cellular vitality of primary neurons. In addition, also concluded that males are more sensitive to bisphenols than females, and they hypothesized that this difference was due to the greater binding of this EDC to estrogen receptors (Meng et al. 2021). On the other hand, a study was tested in wild-type or histone deacetylase (HDAC2) silenced SN56 cholinergic cells, P75NTR receptor or acetylcholinesterase (AChE) from the basal forebrain, to elucidate the mechanisms underlying the cognitive effects induced by BPA. Basal forebrain cholinergic neurons, regulate cognitive function and innervate the cortex and hippocampus, and their loss can cause cognitive disorders. Experimentally, BPA was administered, at concentrations between 0.001 μM and 100 μM, with or without recombinant nerve growth factor (NGF) and acetylcholine (ACh) for one and fourteen days. As a result, BPA induced disruption of cholinergic neurotransmission by reducing acetylcholine transferase (ChAT) activity causing decreased ACh and cell death, mediated partially by overexpression of AChE-S and dysfunction of NGF/TrkA/P75NTR signalling, through HDAC2 overexpression, independently of disruption of cholinergic neurotransmission (Moyano et al. 2021). Nevertheless, in mouse BV2 microglial cells, the research group of Sillapachaiyaporn C investigated the anti-neuroinflammatory effects of Auricularia polytricha against BPA-induced inflammation (0.01–100 µM). After exposure to the highest BPA concentration the levels of TNF-α, IL-1β and IL-6 mRNA expression were increased and a significantly decreased viability of BV2 cells after exposure for 24 and 48 h were also observed. There was still induction of inflammation, positively regulating the secretion of pro-inflammatory mediators through nuclear factor kappa B (NF-kB) signalling. These results suggest that BPA increased the secretion of pro-inflammatory cytokines in microglial cells. In addition, they used mouse hippocampal cells HT-22 to conclude that were damaged due to exposure to the same concentrations of BPA (Sillapachaiyaporn et al. 2022). Conversely, in a different study, on cortical neurons of embryonic mice, the effect of BPA exposure (0.01, 0.1, 1, 10, 100 and 1000 μM) was analysed, reporting changes in the morphology and function of synapses in the cerebral cortex. Cortical pyramidal neurons showed reduced size and number of dendrites and spines and the density of excitatory synapses decreased. Furthermore, BPA exposure impairs neurite growth and branching in cortical neurons and can disrupt normal synaptic transmission and cognitive behaviour. On the other hand, RGS4 and its downstream BDNF/NTRK2 pathway have been shown to mediate the effect of BPA on synaptic and neurological function (Hyun et al. 2022).
In summary, from this analysis, it seems clear that BPA exposure induces various brain changes at the functional level of the cortex and cellular and synaptic morphological modifications, as well as decreased cell viability and neuronal degeneration or defective development (Table 1). Moreover, it was observed that BPA promotes oxidative stress, originating from autophagy-mediated mitochondrial renewal, and originates alterations in the expression levels of several proteins, such as TNF-α, IL-1β, IL-6, nestin, reelin, SYP, MAP2, Tau, and HDAC2, of genes such as PAX-6, and lncRNAs. Thus, even while greatly remains unknown regarding the molecular effects of BPA on the brain system, it appears obvious that BPA exposure is linked to an increase in neurological pathologies.
In vivo studies
Regarding in vivo studies, the number of works currently available and included in this review is higher than in vitro studies, and these studies were mainly conducted in mammals, but there are also some studies in worms, fish, bivalves, insects, and amphibians, on the effect of this EDC on the cerebral vascular system. In this type of study, exposure to BPA is achieved in live animals and then the effects are evaluated.
Effect on worms
Neurodevelopment effects
The effect of BPA on neuroregeneration and neurodevelopment was recently analysed in worms. The asexual Schmidtea mediterranea CIW4 worms were exposed to 1.998 mg/L of BPA. BPA had severe, non-estrogenic effects on neuroregeneration in planaria, causing a severe lack of connection between nerve cords and longitudinal distribution from the brain primordia to the periphery of the head (Morris et al. 2022).
Effects on fish models
Morphological changes
Concerning the effect of BPA in relation to morphology alterations, neurodevelopment, neurobehaviour, neuroinflammation and neurovascular problems, several studies have been performed in two different species of fish. The zebrafish is a model commonly used in in vivo studies, in which animals are exposed to EDCs and the neurological effects are analysed, nevertheless, it is also possible and common to test on other fish such as goldfish. Regarding the morphologic changes caused by the BPA exposure, was seen predominantly phenotypical malformations and neuronal pyknosis. Therefore, a study in zebrafish embryos, subjected to an exposure of 100 nM and 100 μM of BPA and BPA analogues, and observed EDC-induced phenotypic malformations at 100 μM exposure, without effects at 100 nM (Björnsdotter et al. 2017). PK et al. exposed zebrafish males and females to 17.52 μM of BPA, which induced an increase of oxidative stress and neuronal pyknosis in the periventricular grey zone region of the zebrafish brain, which significantly altered the usual scototaxis behaviour (preference for darkness). Moreover, lipid peroxidation and protein carbonylation were increased, altering the antioxidant status of the brain and significantly decreasing the level of glutathione, glutathione reductase, glutathione-S-transferase and superoxide dismutase (Sahoo et al. 2020). Furthermore, adult zebrafish were exposed to 4 mg/L BPA and taurine, to evaluate the neuroprotective efficacy of taurine against BPA-induced neurotoxicity. As a result, taurine significantly ameliorated the effects of BPA exposure when exposed simultaneously, which were increased oxidative stress and neuronal pyknosis (Pradhan et al. 2021).
Neurodevelopmental effects
Thus, regarding the effects on zebrafish neurodevelopment, changes in different brain regions and even CNS homeostasis have also been observed. Moreover, in adult zebrafish, was determined the bioaccumulation potential of BPA (0.78 and 1 μg/L) in the absence and presence of plastic nanoparticles (1 mg/L), and various neurotoxic changes in the head. The results revealed that BPA can accumulate in the viscera, gills, head and muscles, and the co-exposure of nano-sized plastic particles (NPPs) and BPA resulted in a significant 2.2-fold and 2.6-fold increase in BPA uptake in the head and viscera. About the biomarkers, BPA treatment presented down-regulation of the anti-synapsin 2α (Syn2α) protein, which takes part in synaptic transmission. After the co-exposure of BPA and NPPs, the biomarkers of myelin and tubulin protein/gene expression, DA content and mesencephalic astrocyte-derived neurotrophic factor mRNA expression were significantly increased. In this regard, this study showed that BPA and NPPs can inhibit AChE activity. However, AChE activity was no longer inhibited in the co-exposure treatment. Finally, the authors also found that both BPA and NPPs can positively regulate myelin basic protein/gene in the CNS (Chen et al. 2017). Also in adult zebrafish, Guo et al. exposed them to 2 and 20 μg/L of BPA alone or together with 100 μg/L of titanium dioxide nanoparticles (n-TiO2). As a result, thyroid hormones (3,5,3′-triiodothyronine, T3 and thyroxine, T4) decreased on co-exposure, while T4 concentration in adult plasma decreased significantly because of exposure to 20 μg/L of BPA (Guo et al. 2019). On the other hand, in zebrafish during the early post-embryonic stage, a study evaluated the long-term effects of different bisphenols, with emphasis on brain development. Similar to its analogues, BPA showed accelerated embryo hatching rate effects, and in multiple brain areas, elevated levels of AroB protein expression were shown (Coumailleau et al. 2020). Conversely, in zebrafish embryos, evaluating the bioaccumulation of BPA (1, 4 and 20 μg/L) and 100 μg/L of titanium dioxide nanoparticles (n-TiO2), Fu et al. concluded that the transcript level of the neurodevelopment marker genes α1-tubulin, basic protein and Syn2α decreased in an exposure concentration-dependent manner, with significant differences in the 4 and 20 μg/L BPA groups (Fu et al. 2020). Furthermore, in the same animal and stage, in conjunction with a transgenic zebrafish model, Gyimah et al. performed BPA or BPS treatment. As a result, was caused hyperactivity, and interference with the normal expression of developmentally related genes vegfa, wnt8a and mstn1 at developmental stages. The expression of neurodevelopmental-related, ngn1, elavl3, GFAP, α1-tubulin, myelin basic protein and gap43, were also significantly increased, except for the myelin basic protein and GFAP gene that decreased considerably with exposure to 0.03 and 0.3 μM BPA, respectively (Gyimah et al. 2021). In the same sense, another study with zebrafish embryos, analysed various concentrations of Estrone or BPA. These two compounds exerted phenotypic or transcriptomic responses of about 1 nM of BPA. Exposure to estrone and BPA separately up to 5 days after fertilization caused non-monotonic transcriptomic changes, and exposure to BPA 4 to 5 days after fertilization caused hypoactivity and expression of neurological genes. Regarding short-term exposure, 100 nM BPA affected locomotive behaviour and altered the expression of 872 estrogenic and non-estrogenic genes, while at 10,000 nM there were 546 genes, with 122 genes differentially expressed at both concentrations that are linked to neurological diseases, neurodevelopmental included (Wu et al. 2021).
Neurobehavioural effects
In relation to neurobehaviour alterations, Li et al. exposed low doses of BPA (50 to 500 ng/L) for 7 weeks to adult male zebrafish, reporting physiological abnormalities and disruption of courtship behaviour (Li et al. 2017a). In the same conditions, the same authors published another study, reporting the effects of disruption of natural colour preference patterns, relief of anxiety-like behaviour, and altered ability to adapt to a different environment (Li et al. 2017b). Furthermore, in zebrafish embryos and larvae, Fraser TWK et al. showed that 10 μM BPA induced hyperactivity, hypoactivity, or had no behavioural effects (Fraser et al. 2017). However, in embryos, the research group of Zhang performed a rapid behavioural profiling assay that was designed to characterize the neurodevelopmental effects of environmental substances, such as BPA, by quantitatively assessing multiple spontaneous movement characteristics. These authors concluded that the frequency of spontaneous movement, in exposure to BPA at 1 and 10 μM, decreased significantly, but movement intensities increased by 41% for exposure with 1 μM of BPA and 19% at 10 μM, and also that intervals of spontaneous movement increased at 1 μM and 10 μM for BPA (Zhang et al. 2021a). Furthermore, the group of Sahoo PK exposed zebrafish to BPA (0.25, 0.5, 1, 2, 4.8, 16, and 32 mg/L) to discover the neurodegenerative potential of BPA in inducing Parkinson's disease-like phenotypes in zebrafish. As a result, pyknotic and Hoechst-positive neurons in the telencephalon and diencephalon were dramatically enhanced, as a measure of pyknosis and chromatin condensation. The concentration of 32 mg/L of BPA negatively affected neurobehavioural response, antioxidant status, and neuron morphology. Therefore, it was concluded that chronic exposure to BPA may induce neuropathological manifestations leading to the development of motor dysfunction and Parkinson-like neurodegenerative phenotypes in zebrafish (Sahoo et al. 2021). Besides, Gu et al. exposed the same species to 500 μg/L of BPA, which consequently had negative effects on exercise behaviour, CAT and SOD activity, larval development, gene expression in larvae, and behavioural inhibition, and also prevented the expression of CNS proteins in transgenic models (Gu et al. 2021). The same group also studied the neurotoxicity of 200 μg/L of BPA, BPF, BPAF and BPS. All bisphenols caused significant effects on embryo development at 200 μg/L, significant decreases in GABA neurotransmitters, increased concentrations of glutamate and glutamine and modification of the levels of five dopaminergic neurotransmitters (Gu et al. 2022). Moreover, the neuropharmacological effects of silibinin and naringenin were also analysed in zebrafish, against neurotoxicity and oxidative stress caused by 17.52 μM of BPA. BPA exposure induced neurobehavioural changes, such as altered scototaxis behaviour and spending more time in the upper zone compared to control groups, suggesting that the duration spent in the upper zone of the tank increased (Thayumanavan et al. 2022). In the same sense, Yang et al., in zebrafish embryos and larvae, investigated the protective effects of Cyanidin-3-O-glucoside (C3G) against BPA-induced neurodevelopment damage. The data show that C3G co-exposed with BPA had significantly attenuating BPA effects, BPA was shown to have effects on locomotor behaviour and caused aberrant changes in brain morphology in zebrafish larvae. BPA further induced the decline of GSH, SOD, GPx CAT, oxidative stress and cell apoptosis (Yang et al. 2023).
Neurovascular and neuroinflammatory issues
Additionally, the effects of BPA on neurovascular and neuroinflammatory issues were analysed in two articles. Different from other experimental studies in zebrafish, the research work of Wang Q et al. consisted of submitting goldfish to 50 μg/L of BPA to understand the impact of this EDC in the brain. The data show that BPA can disrupt dopaminergic processes and damage blood vessels and induce cerebral atherosclerosis (Wang et al. 2019c). Moreover, zebrafish embryo models were used by Haridevamuthu et al. to evaluate the neuroprotective effects of Biochanin A against BPA-induced neuroinflammation. The results show that 1 µm of BPA dramatically elevated NO and LDH levels and inflammation-related expression levels, while considerably decreasing SOD, CAT, GST, GSH, AChE and Glutathione-related enzyme activity in the head region were observed. Oxidative stress damage and cell death were still brought on by prenatal exposure. In addition, BPA considerably reduced the speed of the larvae’s swimming speed and severely impaired the zebrafish's locomotor activity (Haridevamuthu et al. 2022).
Effects in fly models
Neurobehavioural effects
Two in vivo studies examining BPA effects in flies were conducted, reporting neurobehaviour and neurodevelopmental effects. Nguyen U et al. examined the effects of BPA on neurodevelopment in two genetic strains of fruit flies (Drosophila melanogaster) and looked at the phenotypes of the neurons and behaviour. BPA (0.1 and 1 mM) promoted recurrent grooming behaviour in adults, reduced cutting behaviour in larvae, inhibited axon guidance in the mushroom body, and interfered with neural stem cell formation in the genetic strain w1118. Therefore, this data suggests that BPA's effects on neurodevelopment can vary greatly depending on genetic background (Nguyen et al. 2021).
Neurodevelopmental effects
Welch et al. investigated the effect of BPA exposure in the development of fruit flies which affects gene expression, brain function, and synapse development. BPA mostly reduced the expression of genes involved in neurodevelopment, including those involved in learning, memory, and synaptic development as well as orthologs of human genes connected to neurological and neuropsychiatric disorders. In summary, BPA impaired associative learning and significantly increased the number of axonal branches (Welch et al. 2022).
Effects in frogs, mussels, tunicates, and clams
Morphological changes
Regarding the morphological effects of BPA, studies were also found in frogs, mussels, tunicates, and clams. Different impacts were seen, particularly concerning morphology, DNA, neurodevelopment, cell differentiation, and the expression of genes encoding modulating enzymes and receptors. On embryos and larvae of the South American common frog (Rhinella arenarum), Wolkowicz et al. analysed the acute and chronic toxicity of BPA, by continuous and pulse exposure. Embryos were treated continuously during early larval stages, and by pulse exposures of BPA for 24 h at concentrations between 1.25 and 40 mg/L. As a result, several morphological changes during the early stages were described, also impairing the gill circulation stage in all exposed organisms after 3 h of treatment with 10 mg/L BPA (Wolkowicz et al. 2014). Conversely, the same authors used the same animals and exposed them to concentrations of BADGE (Bisphenol A diglycidyl ether) evaluating the adverse effects of this organic compound through standardized bioassays. BADGE is a chemical compound related to BPA but with different properties and structure. The results showed that BADGE was more toxic to embryos than to larvae at all exposure times, and the most significant sublethal effects in embryos were cell dissociation and developmental delay, while in larvae it was related to neurotoxicity, response to stimuli and narcotic effect (Hutler Wolkowicz et al. 2016).
Neurodevelopmental effects
Concerning the neurodevelopmental effects, the research group of Juhel G exposed green mussels (Perna viridis) to different concentrations of carbamazepine, BPA, and the herbicide atrazine, analysing the effects on AChE. The exposure concentrations used for BPA were divided into low, medium, and high concentrations. However, the authors showed that BPA did not alter AChE activity but induced DNA damage, with increasing chemical concentrations (Juhel et al. 2017). Therefore, Gomes IDL et al. examined how BPA affected larval brain development of the ascidian Phallusia mammillata, which is a solitary marine tunicate of the ascidian class. Experimentally BPA was median effective in 11.8 μM and lethal in 21 μM of concentrations, whereas micromolar doses of BPA impaired differentiation of the ascidian-pigmented cells. The authors concluded that BPA may affect ascidian otolith differentiation (Gomes et al. 2019). Furthermore, Tang et al. exposed invertebrate bivalve species of clam (Tegillarca granosa) to 10 or 100 ng/L of BPA alone or together with 1 mg/L of microplastics. Exposure to BPA and microplastics led to an increase in three major neurotransmitters (Gamma-aminobutyric acid (GABA), DA, and Ach), and a decrease in the expression of genes encoding modulating enzymes and receptors for these neurotransmitters. In addition, the authors highlighted that the toxic effects exerted by BPA were significantly higher compared to previous studies due to the co-presence of microplastics (Tang et al. 2020).
Effects on rodent models
Morphological changes
Most of the articles reviewed in this section were experimentally performed in rodents, a total of 61 articles, resulting in multiple outcomes. In these studies, the main complications observed were related to morphological changes, altered neurodevelopment and neurobehaviour, alterations in specific brain areas, neuroinflammation, neurodegeneration and stroke-related problems. Thus, regarding the morphological alterations, El-Missiry et al. examined the protective effect of melatonin on oxidative stress and apoptotic death receptor proteins in the brains of BPA-treated rats. The results showed that BPA exposure induced significant increases in oxidative stress, and decreased glutathione levels and superoxide dismutase activity in the brain. In addition, BPA also caused upregulation of p53 and CD95-Fas and activation of caspases 3 and 8, resulting in increased apoptosis of brain cells (El-Missiry et al. 2014). In young male mice, the group of Zhou investigated the neuron toxicities of low doses of BPA. The percentages of DNA, tail length and timing in brain cells increased with increasing concentrations of BPA exposure. The authors found that low-dose BPA exposure can lead to DNA damage in brain cells, while prolonged exposure to this compound can impair learning and memory capacity (Zhou et al. 2017). Moreover, Di Pietro et al., in conjunction with a human in vitro experiment, examined the effects of 100 μg/L of BPA in glial and microglia cells of rat offspring at postnatal day 17 from pregnant females, who received BPA soon after coupling and during lactation and weaning. A significantly increased percentage of p-H2AX positive cells within IBA1 positive microglial cells in the hippocampal dentate gyrus, DNA damage in immune cells at the peripheral and central levels, a significant increase in the number of GFAP cells and a decrease in the marked Erα expression were observed. In this sense, they concluded that BPA exposure during development can induce microglial DNA damage and astrogliosis (Di Pietro et al. 2020). Additionally, the research group of Goyal S exposed Wistar rats to 40 μg/kg of BPA and observed a significant reduction in the levels of mitochondrial biogenesis proteins (PGC1α and TFAM) and mitochondrial import protein (GFER). In this regard, the authors demonstrated that BPA induced mitochondrial damage in neurons, reduction in GFER, translocation of cytochrome c to the cytosol and increased apoptosis (Goyal et al. 2021). Furthermore, Ishtiaq et al. administered 100 μg/kg, 1 or 10 mg/kg BW of BPA in adult Sprague Dawley rats for 16 days. BPA increased oxidative stress and increased expression of p53 upregulated modulator of apoptosis (PUMA), p53 and Drp-1, resulting in apoptosis in the brain tissue of rats (Ishtiaq et al. 2021). Bi et al. studied transgenic male Thy1-Cre mice and female C57BL/6 mice and exposed them to 0.5 mg/kg/day of BPA on a postnatal day. As a result, BPA reduced the number of RV + neurons in CA3 and entorhinal cortex but not in the medial septum, decreased the percentage of CaMKIIRV + cells in CA3 hippocampus and entorhinal cortex, and the synaptic connection of upstream glutamatergic neurons and CA1 pyramidal cells was weakened. They concluded that BPA induced detrimental effects on the excitatory neural circuitry of CA3-CA1 and EC-CA1 in memory formation (Bi et al. 2021). Moreover, the same authors exposed male and female C57BL/6 mice to 1 mg/kg/day of BPA for 10 weeks and observed an aberrant induction of HDAC2 expression. Nevertheless, was concluded that repression of HDAC2 could markedly rescue the impairment of spinal density in the hippocampus and prevent cognitive impairment caused by BPA exposure (Bi et al. 2022). On the other hand, El Tabaa et al. exposed Specific-pathogen-free adult white male Wistar rats to 250 mg/kg/day of BPA alone or together with 10 mg/kg/day of epigallocatechin-3-gallate (EGCG). BPA induced apoptotic and necrotic effects in the CA3 neurons of the hippocampus and a significant decrease in hippocampal concentrations of DA, norepinephrine (NE), 5-HT and Ach, as well as in hippocampal AChE activity in rats pre-exposed with EGCG for 2 h before BPA. Abnormal pyramidal cells in the hippocampus and increased hippocampal Casp-3 activity were also demonstrated (El Tabaa et al. 2022). In another study, in male Wistar albino rats, Caglayan et al. evaluated the exposure to 250 mg/kg of BPA, which significantly increased the MDA, NF-κB and TNF-α levels, and activated the JAK1/STAT1 signalling pathway. It also led to ER stress in brain tissue, regulated the levels of ATF-6, PERK, IRE1, and GRP78, and increased the mRNA levels of Bax and caspase-3, but insignificantly reduced the levels of Bcl-2 (Caglayan et al. 2022).
Neurodevelopmental effects
Concerning the neurodevelopment impact caused by BPA exposure in rodents, 18 studies have been performed and reported effects in impaired motor, spatial learning, memory development and cognitive function. Viberg et al. postnatal exposed NMRI mice to BPA (0.32, 3.2 or 4.8 mg BPA/kg body weight), concluding that can alter adult spontaneous behaviour and cognitive function and affect the cholinergic system. These effects were dose-dependent, long-lasting and irreversible (Viberg et al. 2011). These authors, in the same conditions, realized another study, indicating that a single postnatal exposure to BPA on postnatal day 10, during the peak of the brain growth spurt, can alter adult levels of important proteins for normal brain development (CaMKII and SYP) in both hippocampus and cerebral cortex (Viberg and Lee 2012). Conversely, in the prefrontal cortex (PFC) of adult rats, Castro et al. studied the effects of exposure to BPA for 4 days at 50 µg/kg of body weight and analysed the enzymes 5α-Reductase (5α-R) and cytochrome P450 aromatase (P450arom). The authors saw an increased expression of P450arom and isoform of tryptophan hydroxylase (Tph2) in the PFC of males and females but decreased the expression of 5α-R1 (an isozyme important in protecting neurons from apoptosis induced by glucocorticoid excess) in females. In addition, they also analysed 84 genes involved in BPA neurotoxicity in the adult PFC and identified 17 genes as potential targets of BPA, related to synaptic plasticity and memory functions (Castro et al. 2013). In pregnant Institute of Cancer Research (ICR) mice, Kumamoto et al. exposed pregnant mice to 0.02 or 50 mg/kg of BPA on gestational days 6 and 15 and examined neurodevelopmental-related genes linked to the X chromosome (Fmr1, Gdi1, Nlgn3, Pak3, and Ophn1) and genes related to sexual differentiation (ERα, ERβ, and AR). BPA caused a reduction in Xist, Fmr1, Gdi1, Nlgn3, and Pak3, and an increase in Tsix in the 50 mg/kg exposed group, while in the 0.02 mg/kg group, only moderately reduced Xist, Gdi1, Nlgn3, and Pak3. ERα, ERβ, and AR expression were changed in both exposure groups, and anogenital distance and estradiol levels were reduced (Kumamoto and Oshio 2013). On the other hand, Mathisen et al. analysed two strains of mice offspring who consumed BPA-contaminated water before mating, during gestation and lactation. As a result, BPA increased the total amount of Pax6 in the cerebellum and increased the thickness of the outer layer of granules in 11-day-old rat pups. This data agrees with in vitro results, obtained in the same study, which concluded that BPA may have an impact on the granule neurons responsible for the proper development of the cerebellum (Mathisen et al. 2013). The group of Nagao T developed a method to evaluate the behaviour of newborn rats to assess the risk of neurotoxicity of environmental toxicants by analysing motor activities including crawling, turning, straightening, or tremors. The newborn rats were exposed to 2, 20, or 200 µg/kg/day of BPA between days 5 and 18 of gestation and a significant increase in tremors on postnatal day 1 was observed (Nagao et al. 2014). Moreover, Zhang et al. in postnatal Sprague–Dawley rats exposure to a greater range of concentrations, 0.5–5000 μg/kg bw/day of BPA, concluded that BPA deteriorated the learning and memory capacity of rats, impaired the dendrites and spines, and disrupted the neurotransmitters homeostasis in the hippocampus. It was also observed that the neurotoxic effects of BPA exposure were different in males and females, i.e., sex-dependent differences (Zhang et al. 2019). The same group continued the study and observed that maternal exposure impaired spatial learning and memory capacity, altered hippocampal neurotransmitter levels, decreased neuron quantities and dendritic spine density across generations, and led to variations in hippocampal neurotransmitter levels (Zhang et al. 2020).
Concerting prenatal exposition, Castro et al. analysed the effect of a low dose of BPA (10 μg/kg/day) in male rats and studied the PFC, concerning dopamine (DA) and serotonin (5-HT) related genes modulated by BPA at the juvenile stage. The authors reported effects on gene transcription in juvenile and adult male rats and a reduction in precortical DA receptor transcripts in juvenile and Tph2 rats. They also found that there was increased tyrosine hydroxylase transcription in adult rats and that permanent changes were produced in glial cell-derived neurotrophic factor (GDNF) transcript levels (Castro et al. 2015). In pregnant Wistar rats, different concentrations of BPA were analysed by Hass et al. and neurodevelopmental effects were observed, after 25 μg/kg bw/day exposition. Moreover, female offspring experienced impaired spatial learning, which suggested a masculinization of the brain (Hass et al. 2016). Furthermore, Kimura et al. studied spine density and dendritic growth in the hippocampal CA1 of aged mice and developing mice exposed in the prenatal period, in utero, to 40 or 400 μg/kg BPA. Reduced spine densities in hippocampal CA1, decreased basal dendrite length and branching number and disrupted hippocampal CA1 neuronal morphology during development were reported, suggesting that this disruption may persist into adulthood (Kimura et al. 2016). On the other hand, in NCTR Sprague–Dawley, Arambula et al. concluded the transcriptome of the neonate amygdala can be disrupted by prenatal BPA exposure, whereby foetal development may make the female amygdala more vulnerable. BPA exposure affected the signalling pathways for oxytocin, vasopressin, and estrogen, which are important for the structure and transmission of synapses in the developing brain (Arambula et al. 2018). In the same sense, in Swiss albino mice, Birla et al. evaluated the effects induced by BPA (50 μg/kg bw/day) on spatial learning and oxidative stress. It was seen that BPA increased MDA levels in the hippocampus, and subsequently increased lipid peroxidation levels, inducing oxidative stress. Thus, the authors concluded that BPA significantly impaired mice’s spatial memory and learning (Birla et al. 2019).
In another in vivo study, adult male Wistar rats were exposed to 40 μg/kg of BPA by Tandon et al. BPA exposure induced reduced proliferation of oligodendrocyte progenitor cells in the hippocampus, as well as decreased learning and memory capacity, increased apoptosis, caused a decline in oligodendrocyte differentiation, resulted in altered myelin-specific gene expression profiles and protein levels, significantly down-regulated expression of Notch pathway genes, significantly decreased axon number. In addition to these effects, occurred a significant decrease in the intensity of Olig2/myelin basic protein + and myelin basic protein/neurofilament + co-localization in the hippocampus region (Tandon et al. 2020). Also, in adult male albino rats, exposed to 50 mg/kg bw of BPA, El Morsy et al. analysed the effect of BPA on proteins involved in neurodevelopment. The data showed a significant decrease in hippocampal GSH level by 53%, along with a five-fold increase in hippocampal MDA level, a significant decrease in the expression of hippocampal proteins TrKB, MAPK, ERK1/2 and CREB by 75%, 83%, 82% and 70%, respectively, along with a significant decline in hippocampal brain BDNF level by 46%. Additionally, significantly reduced hippocampus AChE activity by 50% and caused a massive increase in the hippocampal pro-apoptotic gene Bax (fivefold), and accelerated hippocampus Caspase-3 activity (fourfold), accompanied by a significant decrease in the hippocampal antiapoptotic gene Bcl-2 (4.5-fold) (El Morsy and Ahmed 2020). Nevertheless, Mao et al. studied for the first time the effect of BPA in small RNAs and found the mRNAs and the pathways of microRNAs (miRNAs) in the rat placenta. Therefore, 43 small RNAs were differentially expressed, and target mRNAs closely matched those expressed by the brain and thymus, demonstrating their ability to control neurogenesis and related neurodevelopmental processes. Thus, the authors concluded that the placenta might influence foetal brain development via secreting miRNAs (Mao et al. 2021). In adult female Swiss albino rats, Elbakry et al. evaluated the enhancing effect of nattokinase against liver and brain damage induced by 100 mg/kg bw/day of BPA or 3 Gy/week of γ-IR. BPA caused increased levels of the misfolded proteins Aβ and p-tau, induced cognitive deficits and impaired learning memory in offspring mice, and decreased acetylcholine transferase activity (Elbakry et al. 2022). Conversely, also in the mouse hippocampus, Luo et al. investigated BPA's impact on the miRNA expression profile to learn more about the miRNA function in BPA-induced learning and memory impairment. As a result, BPA had negative effects on spatial learning and memory as well as alterations in the miRNA expression. In addition, 17 miRNAs significantly altered expression levels (Luo et al. 2023).
Specific brain area modifications
Regarding the effect of BPA exposure in rodents, some studies, have reported modifications in specific brain areas. Khadrawy et al. analysed the effect of exposure to two doses of BPA (10 and 25 mg/kg) in adult male albino rats on excitatory (of glutamate and aspartate) and inhibitory (of γ-aminobutyric acid, glycine, and taurine) amino acid neurotransmitter levels in the cortex and hippocampus. As a result, in the cortex, there was a significant increase in excitatory amino acids, lipid peroxidation and nitric oxide (NO), although a significant decrease in inhibitory amino acids and glutathione. In the hippocampus, there was a significant increase in excitatory and inhibitory amino acid neurotransmitters, such as lipid peroxidation and reduced glutathione. In addition, the authors investigated the effect of BPA on AChE activity, and it induced a significant increase in cortical and hippocampal AChE activity. Thus, the authors concluded that BPA induced a state of excitotoxicity and oxidative stress (Khadrawy et al. 2016). In the same sense, Tavakkoli et al. studied the changes of proteins in the cerebral cortex and exposed adult male Wistar rats to 0.5, 5 and 50 mg/kg of BPA. At 0.5 and 5 mg/kg, lipid peroxidation was significantly higher than in the control group and showed some pro-oxidant effects. There was an 80% increase in pyruvate kinase M2 (PKM2) levels, and PKM2 expression was also increased in some cancer cells, resulting in phosphoenolpyruvate accumulation. The authors further indicated that the expression of 10 proteins was altered, which has already been associated by other authors with neurological and psychosocial disorders, including neurodegenerative diseases, schizophrenia, depression, epilepsy, and some brain tumours (Tavakkoli et al. 2020). The group of Santoro A continued the study of Di Pietro et al. using the same animals and treatment with BPA (Di Pietro et al. 2020; Santoro et al. 2021). However, different results were obtained, reporting enlarged lateral cerebral ventricles in lactating and weaned BPA-exposed animals. BPA exposure also affected the expression of inflammatory cytokines, Sirt1, its natural antisense long non-coding RNA (Sirt1-AS LncRNA) and histone deacetylase 1 (HDAC1) (Santoro et al. 2021). Moreover, Essawy et al. investigated the effect of astragaloside IV or saponins extracted from Astragalus spinosus on DNA damage, which was induced by 125 mg/kg/day of BPA in the PFC, hippocampus, and striatal brain regions of developing male rats. On exposure to BPA, increased levels of NO and decreased levels of glutamate, glutamine, glutaminase and glutamine synthetase were seen, inducing marked DNA damage in the brain regions studied. BPA also markedly decreased BDNF concentration in the hippocampal and striatal regions, although insignificantly affected the PFC. Additionally, BPA exposure resulted in the upregulation of NR2A mRNA expression levels in the PFC and hippocampus and its downregulation in the striatum, while NR2B mRNA expression level was downregulated in PFC and hippocampus regions, but upregulated in the striatum brain region (Essawy et al. 2021).
Furthermore, the group of Yirun A exposed pregnant Sprague–Dawley rats, during pregnancy and lactation, to 50 mg/kg/day of BPA. In this study, BPA exposure led to apoptosis, histopathological changes in the hippocampus, altered GSH and MDA levels, and AchE activity. The results further showed that exposure to EDCs in early life stages caused significant changes in lipid peroxidation, total neurotransmitter levels, and activities of neurotransmitter-related enzymes (Yirun et al. 2021). In the same sense, Zheng et al. investigated the effects of BPA levels in a mouse model on the effects of maternal BPA exposure on children's brain development. Regarding the in vivo study, the authors exposed CD-1 mice to 2.25 μg/kg bw/day of BPA and concluded that provoked structural alterations in brain regions including the superior olivary complex and bed nucleus of stria terminalis with larger effect sizes (Zheng et al. 2022). Sevastre-Berghian et al. evaluated the effects of BPA with or without melatonin, in 2-month-old male Wistar rats. As a result, BPA exerted an inhibitory effect on general locomotion and was induced in the frontal lobe and the hippocampus activation of MAPK. The monocyte chemoattractant protein-1 (MCP1) expression was reduced and the expression of pNFkB was considerably enhanced. MCP1 is expressed by neurons, astrocytes, microglia, and capillary endothelium in the brain, and may alter the permeability of the blood–brain barrier and modulate various neuronal lesions (Yao and Tsirka 2014). As a result, in groups that had been exposed to BPA, there was cellular oedema, necrosis, and a polymorphic cellular inflammatory infiltration that increased the intercellular spaces (Sevastre-Berghian et al. 2022).
Neurobehavioural effects
Concerning the neurobehavioural effects in rodents, 10 articles were analysed. The first was performed in 2011 by Ishido et al. who examined the effects of BPA and two derivatives, on the behaviour of 5-day-old male Wistar rats, concluding that at 20 μg of BPA, there was an increase in hyperactivity after 4 to 5 weeks of exposure. They also reported that there was increased activity in the nocturnal phase by 1.3 times (Ishido et al. 2011). Moreover, Luo et al. exposed male mice to a 50 mg BPA/kg diet per day for 35 days, and observed an increased anxiety-like behaviour, although in the hippocampus, AChE activity was dramatically reduced (Luo et al. 2013). Furthermore, Kundakovic et al. observed the effects of long-term BPA prenatal exposure to 200 μg/kg per day on the behaviour of mice and concluded that there was an induction of long-lasting changes in DNA methylation in the transcriptionally relevant region of the derived neurotrophic factor (BDNF) gene in the hippocampus and blood (Kundakovic et al. 2015). On the other hand, in young and adult NCTR Sprague–Dawley rats, Rebuli et al. evaluated the impact of perinatal exposure to BPA (2.5, 25 or 2500 µg/kg body weight) on anxiety-related behaviours and exploratory activity. Several parameters on the behaviour were evaluated inside a 50 cm long and 10 cm wide apparatus. Differentially, two arms were placed inside 40 cm walls and two arms with a short (8 mm) overhang around the edge. No consistent effect was seen, in either sex, at either age compared to vehicle controls. However, in comparison with the exposure to ethinyl estradiol (0.5 µg/kg bw/day), which was used as the reference estrogen, significant differences were found for some parameters, such as time spent and distance walked on the apparatus, in different measurements compared to the control (Rebuli et al. 2015). The neuromodulatory effect of α-Lipoic acid against BPA neurotoxicity (10 mg/kg) in male C57BL/6 J mice was analysed by Khan et al. The data obtained showed that the activity of monoamine, the level of lipid peroxidation and the content of protein oxidation were significantly increased, while AChE, catalase (CAT), glutathione-S-transferase (GST) and glutathione (GSH) activities decreased. The combined treatment of BPA and α-Lipoic acid showed a significantly higher level of GSH (Khan et al. 2018). Furthermore, on rats, the group of Henriksen AD analysed the impact of BPA exposure, on the anterior hypothalamus, the basal nucleus of the stria terminalis, and hippocampal gene expression. 259 genes were overrepresented in categories related to mating, cell–cell signalling, behaviour, neurodevelopment, neurogenesis, synapse formation, cognition, learning behaviours, hormone activity, and signalling receptor activity, among other things, in the mice exposed to BPA (Henriksen et al. 2020). Besides, Repouskou et al. used a mixture of phthalates, pesticides, and BPA in rats and human epidemiological studies, which were used to better mimic real-life situations. This mixture was exposed to mice throughout gestation and increased active coping during swimming stress in both sexes, although just in male offspring, increased locomotion, decreased social interaction and altered the expression of all examined genes (Nr3c1, Crh, Fkbp5, Oxt, and Esr2) in the hypothalamus (Repouskou et al. 2020). In Wistar albino rats, Singha et al. exposed 5 mg/kg body weight in prenatal and postnatal periods to clarify how astrocyte shape and GABA transmission contribute to the cognitive impairments caused by BPA. BPA during and after pregnancy caused anxiety-like behaviour, decreased serum GABA levels and was observed reduced dendritic spine counts and astrocyte numbers (Singha et al. 2021). Following that, Gore et al. used a mixture called NeuroMix, that have bisphenols, phthalates, vinclozolin and perfluorinated, polybrominated and polychlorinated compounds, and exposed pregnant Sprague Dawley rats. Adult females were the only ones affected by NeuroMix's anxiety-like, social, and mate-preference behaviours, but stress had more impact on males than females. In summary, many relationships between NeuroMix and stress were discovered, particularly for brain gene expression and partner choice behaviour (Gore et al. 2022). On the other hand, the group of Hyun wanted to confirm the effect of exposure to BPA (50 µg/kg) for 2 months in Mice (C57BL/6N). In this case, BPA exposure resulted in high anxiety behaviour and disrupted memory processing, in agreement with the in vitro experiments (Hyun et al. 2022).
Stroke-related problems
Regarding the interaction of BADGE and its influence on cerebral ischemia, reperfusion injury, and ischemic stroke through a middle cerebral artery occlusion treatment (MCAo) or a middle cerebral artery occlusion and reperfusion (MCAO/R), three studies have been performed also in rodents. Therefore, the research work of Certo et al. evaluated the participation of retinoid X receptors (RXR) in the development of ischemic stroke injury. The experiments were performed in adult male mice, with 5 experimental groups, where in the last group, MCAo was performed for 30 min after administration of Bexarotene or 30 mg/kg of BADGE. The BADGE, which is a PPAR-y antagonist, was used to serve as an antagonist to improve histological outcomes and also because of the ability of bexarotene to reverse spleen atrophy induced by middle cerebral artery occlusion. Pharmacological blockade of PPAR-γ, with BADGE, significantly reversed the reduction in cerebral infarct volume (Certo et al. 2015). Subsequently, in male rats, Wang et al. induced the MCAO/R (2-h occlusion, followed by reperfusion for 48 h). The authors aimed to examine how ursolic acid acts as a neuroprotective agent to modulate the metalloprotease/anti-metalloprotease balance. They posteriorly administered ursolic acid intragastrically 0.5, 24 and 47 h after reperfusion, and BADGE intraperitoneally 1, 24.5 and 47.5 h after reperfusion. The exposure to BADGE was 30 mg/kg alone or together with 5, 10 or 20 mg/kg ursolic acid. A significant elimination of the ursolic acid-induced enhancement in PPAR-γ expression was shown. BADGE also provoked a partial and significant block of metalloproteinase-2 (MMP2) and MMP9 levels, although increased metallopeptidase inhibitor 1 (TIMP1) levels, were previously induced by ursolic acid. (Wang et al. 2016). Following that, Wu et al. investigated the alterations of the PPAR-γ-activated gamma receptor in focal cerebral ischemia–reperfusion injury. They experimentally performed the rat model of middle cerebral artery occlusion and reperfusion and exposed male Sprague–Dawley rats to 30 mg/kg BADGE, in one of the experimental groups. MCAO/R significantly increased neurological deficit scores, TNF-α, IL-1β and IL-6 levels (Wu et al. 2018).
Neuroinflammation effects
Concerning neuroinflammation effects after BPA rodent exposure, 4 studies were analysed. In hypertensive adult male Wistar rats, exposed to 100 mg/kg of BPA, Akintunde et al. observed increased motor coordination and antigen-presenting cells and CD43 T-killer cells, and also regulated pro-inflammatory mediators (Akintunde et al. 2020). On the other hand, Ni et al. exposed 8-week-old adult C57BL/6J mice to 0.05, 0.5, 5 and 50 mg/kg BPA. BPA exposure was found to induce cognitive impairment in males, but not in females, which may be caused by microbial gender differences and the role of estrogen receptors. BPA further increased neuroinflammation and damaged blood–brain barrier function, caused intestinal barrier dysfunction, altered microbiota composition, and also decreased levels of 5-HT and its metabolites in serum and hippocampus (Ni et al. 2021). Moreover, Abdou et al. exposed adult male Wister albino rats to 50 mg/kg bw/day of BPA. Exposure to BPA led to a significant increase in brain MDA and NO levels, associated with a significant reduction in GSH, total thiols, glutathione peroxidase (GPx), SOD and GST. Serum levels of total cholesterol, triglycerides, and low-density lipoprotein cholesterol (LDL) were increased, and an increase in specific AChE activity and DA and 5-HT levels occurred. The expression of inflammatory markers (tumour necrosis factor-α (TNF-α), cyclooxygenase-2 (COX-2), and tumour suppressor and pro-oxidant p53 protein (p53 genes) were also increased (Abdou et al. 2022). Furthermore, Lama et al. examined the impact of 50 μg/kg of BPA on anxiety-like behaviour in obese mice, and whether it is linked to neuroinflammation and immune activation. The data show that BPA deteriorated the anxiety-like behaviour caused by the high-fat diet (HFD) and the neuroinflammation brought on by HFD, which also increased IL-1, TNF-, and MCP1 in PFC. BPA generated monocyte recruitment and inflammation in the hypothalamus and amygdala. Nonetheless, the authors concluded that subchronic exposure to BPA increased neuroinflammation and immunological activation brought on by the HFD diet, constituting an extra risk factor for mood disorders that are solely connected to obesity (Lama et al. 2023).
Neurodegeneration effects
Regarding the neurodegeneration effects caused by BPA exposure in rodents, ten articles have been analysed. The research group of Agarwal et al. attempted to demonstrate that autophagy acts as a transient cellular protective response against BPA-induced neurotoxicity. These authors saw their effect during the early postnatal period of C57BL6 male mice and saw an increased expression and levels of genes/proteins involved in autophagy. BPA exposure further negatively regulated the rapamycin (mTOR) pathway promoting mitochondrial loss, bioenergetic deficits and increased mitochondrial translocation of PARKIN, which is a cytosolic E3 ubiquitin ligase. In the long term, decreased levels of Lamp-2 and positive regulation of p62 and cleaved caspase-3 were seen. Thus, the authors concluded that autophagy may protect against BPA-induced neurotoxicity by activating the AMPK and mTOR pathways (Agarwal et al. 2015). Moreover, in another in vivo study, the same authors concluded that chronic exposure to BPA causes mitochondrial dynamics, leading to neurodegeneration, and apoptosis in the rat brain hippocampus, in addition to autophagy. Experimentally, Wistar rats to 40 μg/kg body weight were exposed to BPA, which increased Drp-1 levels, associated with impaired autophagy, increased apoptosis, and increased the levels of Drp-1, which is a dynamin-related protein, in hippocampal tissue (Agarwal et al. 2016). On the other hand, Tiwari SK et al. exposed adult female Wistar rats to the same BPA concentration. The effects observed were a decrease of the antiapoptotic gene Bcl-2 and an upregulation of the gene Bax, thus a significant increase in neural degeneration (Tiwari et al. 2016). Furthermore, Li et al. examined the effects of 30-day exposure to 100 μg/kg/day of BPA on glucose transport and the IR/IRS/AKT/GSK3β axis in adult male mice to determine if there is an association between disruption of insulin signalling and neurotoxicity of this EDC. The authors demonstrated a decreased insulin sensitivity, decreased glucose transporter protein 1, 3 (GLUT1,3) levels, hyperactivation of the IR/AKT/GSK3β axis, and increased phosphorylated tau and β-APP. In conclusion, BPA exposure may be a potential risk factor for neurodegenerative diseases, as these results strongly indicate significant disruption of insulin signalling in the brain (Li et al. 2016). Nevertheless, Khan et al. examined whether exposure to 40 and 400 μg/kg body weight of BPA alters the expression of axial and myelin structural proteins in the cerebral cortex of C57BL/6J mice. BPA causes oxidative stress in the brain, memory loss, muscle coordination deficits, allodynia, degeneration of mature and immature oligodendrocytes, nestin, myelin basic protein, and also myelin-associated glycoprotein-1 (MAG-1). Subchronic exposure to BPA caused neuroinflammation through the downregulation of inflammatory cytokine mRNA and protein expression. In conclusion, the authors considered that long-term exposure to 40 μg/kg body weight of BPA may cause axonal degeneration and demyelination in oligodendrocytes and neurons, and may be involved in the development of neurological and neuropsychological disorders, including multiple sclerosis, neuromyelitis optics (Khan et al. 2019). In adult female Wistar albino rats, Abdel-Rafei et al. analysed the modulatory role of methylsulfonylmethane (MSM), in combating neurodegenerative disorder (Alzheimer's mimicking neurotoxicity), induced by co-exposure to BPA and gamma radiation (γ-IR). It was found that co-exposure of BPA and γ-IR induces hallmarks typical of neurodegenerative disorders, due to rather high oxidative stress, extensive neuroinflammation, elevated Alzheimer’s markers in the cortex and hippocampus, as well as up-regulation of microglial pro-inflammatory triggering receptor expressed on the myeloid cell-2/DNAX-activating protein of 12 kDa/spleen-tyrosine kinase pathway and its downstream targets (PLC-γ/DAG/p38-MAPK) in the hippocampus. In addition, neurodegenerative lesions were detected on histopathological examination of the cortex and hippocampus along with marked Aβ deposition in the hippocampus (Abdel-Rafei and Thabet 2020). Moreover, in male Sprague–Dawley rats, the research group of Kobayashi analysed the exposure effect of 100 mg/kg/day of BPA or 3 mg/kg/day of Rotenone on the cerebrovascular system. Thus, the data demonstrated that BPA and rotenone-induced S-nitrosylation of protein disulfide isomerase in brain microsomes, which can lead to Alzheimer's and Parkinson's disease, and decreased RNase oxidation activity (Kobayashi et al. 2020). Furthermore, Xue et al. exposed male and female C57BL6 mice to 2, 10, and 100 μg/kg/day of BPA from day 6 of gestation until weaning and at 3, 6 and 9 months of age, the neurotoxic effects were investigated. The authors reported that phosphorylated tau protein (p-tau), which is important in the stabilization of the internal microtubules in neurons, the characteristic protein of tauopathy, increased dramatically in the hippocampus and cortex at 3–9 months of age. In addition, it was also observed that GSK3β and CDK5, two critical kinases, were activated in most of the perinatal BPA exposure group, and protein phosphatase 2A (PP2A), one of the most important phosphatases, regulated the expression of p-Tau through its demethylation, methylation and phosphorylation (Xue et al. 2020). Zhang et al. evaluated the neurotoxic effects of the male mouse hippocampus under exposure to 0.01, 0.1 and 1 mg/L of BPA. Overall, exposure to BPA inhibited mRNA and protein expressions of oxidative phosphorylation (OXPHOs), decreased learning ability by suppressing mitochondrial OXPHOs and altered the expressions of 16 overlapping differentially expressed genes involved in Alzheimer’s disease, Parkinson’s disease, Huntington’s disease and OXPHOs in the hippocampus (Zhang et al. 2022b). In addition, the effect of vitamin E and selenium to combat the toxicity of 25 mg/kg body weight of BPA on the spinal cord and submandibular glands was evaluated in adult male 5-month-old albino rats (Rattus norvegicus). BPA caused a neurotoxic effect in the spinal cord of rats, nerve fibre degeneration with axonal disappearance of the white matter, GFAP proliferation and high level of MDA in the spinal cord and degeneration of the acinar cells of the submandibular gland and duct system. (Bashir et al. 2022).
Effects in ewe models
Specific brain area modifications
Regarding the effect of BPA on specific brain area modifications, along with neurobehavioural and cognitive disorders, one study has been performed on pregnant ewes. The authors exposed these animals to 5 µg/kg of BPA to evaluate the impact on foetal brain development in a region-specific way. The metabolic pathways excitatory and inhibitory amino-acid, cholinergic, energy, and lipid homeostasis pathways were particularly affected, which might be a factor in the neurobehavioural and cognitive disorders. The dorsal hippocampus, the cerebellar vermis, the dorsal hypothalamus, the caudate nucleus, and the lateral section of the frontal cortex were affected by BPA (Guignard et al. 2022).
In conclusion, in vivo research supports in vitro studies. These studies showed that BPA can cause changes in the neurological system, like structural and molecular alterations in cells and specific brain sections, mostly in the hippocampus and the cortex (Table 2). In the articles reviewed detrimental effects on neurotransmitters and modifications of expression and activity in important genes and proteins, excitotoxicity, oxidative stress, neuroinflammation, and damaged blood–brain barrier function have been detected. These modifications can lead to neurodevelopment and neurological implications and pathologies such as deteriorated cognitive functions and cholinergic system, impaired spatial learning, and memory capacity, neuroinflammation, stroke-related problems, neurodegenerative diseases (e.g., Alzheimer’s, Parkinson’s, and Huntington´s), and neuropsychological or neurobehavioural (social and emotional) disorders.
Effects of BPA on Humans
Some studies positively associated an increased risk of premature complications with environmental factors, such as exposure to EDCs. For this, human studies on their effect are needed and can be divided into human in vitro studies, and epidemiological studies. In these types of studies, a more detailed link to neurological diseases, such as neurovascular, neurodevelopmental, and neurodegenerative diseases and their direct effects on humans will be seen, with some focus on Alzheimer's, Parkinson's, depression, ADHD, ASD, and some other cognitive and social disorders.
In sum, this section will discuss the main effects of BPA in humans through in vitro studies and the epidemiological evidence supporting a relationship between BPA and neurological complications or diseases.
Human in vitro studies
The in vitro effects of BPA on human brain cell lines will be reviewed, namely human neural progenitor cells, SH-SY5Y, human glutamatergic neurons, human cortical neurons, human embryonic stem cells, Human peripheral blood mononuclear cells, IMR-32 from males and SK-N-SH from females.
Nervous system homeostasis effects
Huang B et al. hypothesized that maternal exposure to low doses of BPA during gestation may decrease the expression of insulin-like growth factor 1 (IGF-1), which is an essential animal multifunctional peptide that may play an important role in CNS homeostasis. The authors observed in human embryonic stem cells (hESCs)-derived embryoid bodies (hEBs), that BPA exposure-induced expression of IGF-1 insufficiency, and this IGF-1 expression can be related to inducing Parkinsonism (Huang et al. 2014). Additionally, the same authors later, in the same cells, demonstrated that this EDC can repress the expression level of IGF-1, marker genes for ectoderm, neuron progenitor cells and dopaminergic neurons. Plus, this study, has shown remarkably that BPA represses neuronal differentiation through downregulating IGF-1 expression (Huang et al. 2017).
Morphological changes
Concerning the morphologic alterations, Wu et al. analysed the BPA exposed in mitotic human neural progenitor (hNP) cells for 14 days. As a result, a decreased cell percentage by 45.2% at the highest dose assessed occurred. At 10 μM of BPA, significant reductions of 29.0%, 13.9% and 42.8% were observed for neurite length per neuron, neurites per neuron, and branch points per neuron respectively (Wu et al. 2016). Furthermore, Wang et al. investigated the chronic exposure to BPA (0.1, 1.0 and 10 μM) in human glutamatergic neurons (hGN), derived from hESC, for 14 days. BPA caused an axon growth reduction in a concentration-dependent manner, and a postsynaptic density protein-95 (PSD-95), SYP and α-amino-3-hydroxy-5-methyl-4-isoxazole-propionic acid receptors (AMPARs) expression were increased, that are linked to deteriorated dendritic spines and caused neuronal apoptosis. Moreover, the authors found that the BPA-induced adverse effects were due to increased production of reactive nitrogen species (RNS), ROS and an excessive influx of Ca2+ (Wang et al. 2019a). Further on, by the same group, human cortical neurons (hCNs) were incubated with BPA, 0.1, 1 and 10 μM for 14 days, concluding that there was a positive regulation of N-methyl-d-aspartate receptors and a disruption of intracellular calcium homeostasis. These authors also saw mitochondrial dysfunction, endoplasmic reticulum stress, neural apoptosis, and neuronal network damage (Wang et al. 2019b). On the other hand, Liang et al. incubated hESCs and NSCs to BPA and derivates. Therefore, BPA and derivates were shown to be cytotoxic at micromolar concentrations in both cell types. At nanomolar concentrations, BPA decreased axon length. Thus, the authors found that BPA substitutes may not be as neurologically safe as initially proposed (Liang et al. 2020). Furthermore, in two different cell lines, the research group of Wang C investigated the neurotoxic effects of BPA, BPS and BPB. They exposed the IMR-32 cell line of males and the SK-N-SH cell line of females, at concentrations of 1 nM, 10 nM, 100 nM, 1 μM, 10 μM and 100 μM for 24 h. The data demonstrated that bisphenols exposure can promote ROS production and increase MDA levels, SOD levels reduction, leading to oxidative stress and apoptosis in human neuroblastoma cell lines. Especially, BPA resulted in the loss of mitochondrial membrane potential (MMP) and the protein expression levels of Bak-1, Bax, cytochrome c and caspase-3 were up-regulated, but Bcl-2 was down-regulated significantly (Wang et al. 2021).
Genetic alterations
It has also been observed in several studies that exposure to BPA can alter the expression of important proteins for healthy brain function. In this regard, the group of Wang T used the SH-SY5Y cell line, which is a human neuroblastoma cell line, and incubated with BPA at 2, 20, 200, and 2000 nM/L. As a consequence, an inhibition of physiological p-IR Tyr1355 tyrosine phosphorylation, p-IRS1 tyrosine 896, p-AKT serine 473, and p-GSK3α/β serine 21/9 was observed, as well as increased phosphorylation of IRS1 Ser307, and there was a substantial increase in BACE-1, APP, β-CTF, α-CTF, Aβ 1-42 and phosphorylated tau proteins (S199, S396, T205, S214 and S404), which are pathological proteins associated with Alzheimer's disease (Wang et al. 2017). Pistollato et al. exposed human induced pluripotent stem cell (hiPSC)-derived NSCs to different chemicals, namely BPA, to evaluate the effects of acute (3 days) and repeated doses (14 days) As a result, there was a slight decrease in total PSD-95 levels and a trend toward an increase in SYP in neurites was seen after 3 days with 28.96 μM of BPA, while 14-day exposure caused a slight decrease in PSD-95 levels in neurites with 12.74 μM of BPA. There was an increase in the number of neurites after 3 days with 12.74 μM of BPA, while the number of branch points began to decrease after 14 days. Finally, the ratio between BDNF levels in neurites and cell body decreased at 12.74 μM BPA (Pistollato et al. 2020). Subsequently, the same group performed a similar experiment adding some other chemicals. Therefore, after 14 days of treatment, most chemicals induced significant positive regulation of BDNF levels, especially at the highest concentration assessed, with BPA being the main driver of positive BDNF regulation in the mixture between chlorpyrifos, lead, 2,2′4,4′-tetrabromodiphenyl ether and ethanol. Also, it was observed that the number of neurites per neuron, ethanol resulted as the chemical that contributed most to this mixture effect, while BPA and lead induced opposite effects (Pistollato et al. 2021). In the same sense, Engdahl et al. investigated whether BPA affects the function of the breast cancer resistance protein (BCRP), which is one of the major ATP-binding cassette (ABC) transporter proteins that take part in multi-drug resistance in cancer therapy. To shield the brain from a variety of chemicals, the BCRP is an important efflux transporter in the blood–brain barrier, and the authors in this study concluded that BPA significantly inhibited the transport function of BCRP (Engdahl et al. 2021). Furthermore, Chesnut et al. exposed neural progenitor cells (NPCs) derived from induced hiPSCs to BPA (50 and 100 μM) and observed a reduction in myelination (Chesnut et al. 2021).
Oxidative stress and stimulation of cytokine production
Regarding the relationship between the effects of BPA on Alzheimer’s, Parkinson’s, Dementia and neuroinflammation, the oxidative stress and stimulation of cytokine production were analysed. From in vitro incubation, human serum was incubated with 1 and 10 mg/mL of BPA. The serum was obtained from 94 random human donors aged 18 to 65 years. Kharrazian D et al. aimed to investigate associations between unconjugated BPA bound to human serum albumin antibodies (BPA-HSA) and alpha-synuclein antibodies and between IDP antibodies and alpha-synuclein antibodies, demonstrating that there were significant associations and risks between antibodies formed against BPA-bound-to-albumin antibodies and antibodies formed against alpha-synuclein, which with an abnormal deposition, plays a central role in the pathogenesis of disorders such as Parkinson's disease and Dementia (Kharrazian et al. 2019). Moreover, the group of Arita Y et al. exposed placental explant cultures to varying doses of BPA in the presence or absence of Escherichia coli colonies. As a result, it increased IL-1 and IL-6 production under basal conditions in a dose-dependent manner, 8-IsoP expression at 10 and 100 nM and BDNF synthesis at 1000 and 10,000 nM, but inhibited sgp130, a soluble receptor that reduces IL-6 bioactivity (Arita et al. 2019). Furthermore, in human peripheral blood mononuclear cells (PBMC), Di Pietro et al. saw that BPA-induced cell proliferation in the S phase of the cell cycle and caused chromosomal fragmentation affecting the DNA damage checkpoint. BPA further induced ɣH2AX activation in TCD4þ and TCD8þ lymphocytes in human proliferation and modulated the expression of ERα and ERβ. Finally, BPA exposure also caused microglial DNA damage and astrogliosis, thus it can be concluded that BPA can induce neurotoxicity in this cell type (Di Pietro et al. 2020). Wang C et al., using IMR-32 and SK-N-SH human neuroblastoma cells, aimed to investigate the BPA effect in EGCG, Z-YVAD-FMK (a caspase-1 inhibitor) and ICI182,780 (an ER inhibitor) modulators. Experimentally, BPA increased the mRNA levels of IL-18, ASC, gasdermin D (GSDMD) and the protein levels of NLRP3 (linked to inflammatory diseases), and caspase-1 in both cell lines in a non-linear manner. BPA exposure further significantly increased reactive oxygen species production, and promoted apoptosis and LDH release, with reduced cell viability and mitochondrial membrane potential, in both cell lines. Thus, the authors concluded that BPA could induce pyroptosis in neuroblastoma cells through the NLRP3/caspase-1/GSDMD pathway, mediated by ER (Wang et al. 2022a).
In summary, human in vitro studies have shown both cellular and structural human effects on the neurological system. The BPA exposome has been associated with neurodegenerative diseases such as Parkinson's, Dementia and Alzheimer's (Table 3). The human studies analysed in this review focused on studying the effects of BPA exposure on diverse types of neurons, and neuronal damage, apoptosis effects and also disruption of intracellular Ca2+ homeostasis were observed. Wang C et al. showed that exposure to BPA in IMR-32 and SK-N-SH human neuroblastoma cells increased mRNA levels of IL-18, ASC, GSDMD, protein levels of NLRP3 and caspase-1, associating them with inflammatory diseases and pyroptosis in neuroblastoma cells. Also in this study, exposure to BPA caused a significant increase in ROS and promoted apoptosis and LDH release. In addition, effects such as decreased axon length, microglial DNA damage, astrogliosis, BCRP inhibition, and significantly reduced myelination were mentioned by the other studies.
Epidemiological studies
Human exposure to BPA has been analysed mainly in the early stages of development, such as pregnancy and the prenatal period, when individuals are most susceptible to its effects, both in vitro and in vivo, but it is epidemiologically where the negative effects of both BPA and other EDCs on the human body are most accurately perceived, in this case relating to brain disorders (Abrantes-Soares et al. 2022; Thayer et al. 2015). Thus, this topic mostly relates prenatal exposure to BPA to neurological, and neurodevelopmental disorders and neurological pathologies, like ADHD, ASD, and even Stroke.
Neurodevelopmental problems
Regarding neurodevelopmental problems caused by BPA exposure, we found some epidemiological studies reporting changes in brain functions and cognitive development. The group of Myridakis A evaluated the exposure of preschool children to BPA, phthalates, and parabens. This study was part of the “RHEA” project, which is a pregnancy cohort, prospectively examining a cohort of pregnant women between February 2007 and February 2008 and their children in Heraklion, Crete, Greece. Although during the study, the link of parabens to high BPA exposure was studied since they can be found in food, they do not share the same source of exposure. Yet, a negative correlation was seen between age and high BPA exposure (Myridakis et al. 2016). Braun et al. investigated the relationship between prenatal urinary BPA metabolite and visuospatial abilities in a prospective cohort in Cincinnati, HOME study of 198 mother–child pairs. However, maternal urinary BPA concentrations during pregnancy, but no association was observed (Braun et al. 2017a). Moreover, Martinez MA et al. estimated prenatal exposure to BPA and DEHP through food consumption of pregnant women, as part of the European “HEALS” project, living in the municipality of Tarragona (Spain). As a result, plasma concentrations of free BPA were observed in women characterized by transient peaks due to meals, and foetuses showed high basal sustained BPA concentrations due to low or no metabolic activity. Thus, the authors concluded that these EDCs may have a major effect on organ development in young children or the foetus, including brain development (Martínez et al. 2017). On the other hand, Lin CC et al. investigated the association between cord blood BPA levels and neurodevelopmental outcomes at 2 and 7 years of age. In the sample of 356 mother–child pairs from the Taiwan Birth Panel Study, BPA was detected in cord blood in 55.9% of the children. In boys, there were significant associations between the full-scale intelligence quotient (IQ) and verbal comprehension index, while in girls, prenatal exposure had adverse effects on the full-scale IQ, the preceptive reasoning index, and the working memory index. Yet, the authors concluded that there was an adverse association between prenatal BPA exposure and cognitive development (Lin et al. 2017). Kim S et al. investigated the chemical exposure profile of women from the Children's Health and Environmental Chemicals in Korea (CHECK) cohort, in South Korea between 2011 and 2012, and subsequently associated it with their children's early neurodevelopmental performance at 13–24 months of age. Nonetheless, sex-dependent effects of BPA were observed, and it was found that there was an inverse association between urinary BPA levels and child mental developmental index (MDI) scores observed only among girls (Kim et al. 2018). In another epidemiological study, 506 Chinese pregnant women and their infants from the Laizhou Wan Birth Cohort (LWBC) from September 2010 to December 2013 were followed. Maternal BPA concentrations were adversely associated with children’s developmental quotient scores (DQ) at 12 months of age. Prenatal BPA concentrations were negatively associated with DQs in the adaptive domain among boys and girls, and DQs in the social domain only among girls (Pan et al. 2019). The effects of prenatal exposure to a mixture of EDCs, on neurodevelopment in school-aged children, were evaluated by the group of Tanner EM, and 718 mother–child pairs from the SELMA study were included. Among the phenols, BPA had the highest geometric means (GM) concentrations (1.53 ng/mL) and early prenatal exposure to EDCs among boys, was associated with lower intellectual functioning at age 7. Thus, it has been found that early prenatal exposure to a mixture of EDCs may be related to lower levels of cognitive functioning at age seven, particularly in boys (Tanner et al. 2020). On the other hand, from data from Wuhan Medical & Healthcare Center for Women and Children (WMHCWC), the relationships of repeated measurements of exposure to different bisphenols during pregnancy with child neurodevelopment in 456 mother–child pairs between 2014 and 2015 were evaluated. Second-trimester BPA concentrations were inversely associated with MDI scores (Jiang et al. 2020). Maternal urinary concentrations of chemical mixtures, including BPA, with IQ in children were also performed by Guo J et al. The data showed that prenatal exposure to BPA was associated with a decrease in the child's full intelligence quotient (FIQ) at age 7, thus affecting intellectual performance, especially in boys (Guo et al. 2020). Besides, Freire C et al. revealed in their study that BPA was associated in 4 to 5-year-old boys with poorer memory, verbal, and motor skills (Freire et al. 2020). Furthermore, Dualde P et al. implemented biomonitoring of biomarkers in children from Valencia, Spain, using urines from the BIOVAL program. The BIOVAL program is part of the Food Contaminants Exposure and Risk Assessment Program, which is focused on the biomonitoring of food contaminants in children from the Valencia Region. However, there are no observed negative effects after human exposure to BPA in children from this region (Dualde et al. 2021). On the other hand, Bornehag CG et al. saw the individual relationships between prenatal exposure to BPA, BPF and BPS and cognitive effects in 7-year-old children. Mothers were recruited into the SELMA study. As a result, BPA had a higher concentration of GM than BPF and BPS. However, BPA prenatal exposure had no significant association with effects on cognitive functions (Bornehag et al. 2021). Contrarily, Zheng J et al. also performed an epidemiologic study on mothers-child pairs and concluded that gestational exposure to low levels of BPA can cause damage to the developing brain at magnetic resonance imaging (MRI) resolution. Specifically, it was observed that maternal exposure to BPA can cause effects on the brain, in regions such as the postcentral gyrus, the opercular region of the inferior frontal gyrus and the superior occipital gyrus (Zheng et al. 2022). Otherwise, in the NHANES study, urinary levels of numerous phenols were assessed to see if they were related to the increased prevalence of antinuclear antibodies in adolescents and young adults. However, for BPA exposure, its levels showed no association with antinuclear antibodies (Parks et al. 2022).
Emotional neurobehavioral problems
Concerning BPA effects on neurobehaviour, several studies agreed that BPA can induce internalizing and externalizing problems, anxiety, and even depression, among other emotional problems. Yolton K et al. examined the association of prenatal exposure to BPA and phthalates, which included mother and infant pairs who were enrolled in the Health Outcomes and Measures of the Environment (HOME) study. Maternal urinary BPA metabolite concentrations at two distinct time points in pregnancy, at weeks 16 and 26 of gestation, were compared with scores on the NICU Neurobehavioral Network (NNNS), describing 13 dimensions of neurobehaviour, at 5 weeks of age in a cohort of 350 mother/infant pairs. However, prenatal BPA exposure was not associated with neurobehavioural outcomes at 5 weeks (Yolton et al. 2011). In the urine of Salinas Valley mothers during pregnancy in 1999–2000 and later in their children at age 5, the neurobehavioral effect of BPA was assessed. Higher prenatal BPA exposure is associated with depression and anxiety in boys at age 7. High urinary BPA concentration in children was also associated with internalizing problems (e.g. maladjusted emotional state), ADHD, and externalizing problems (e.g. inappropriate and uncontrolled behaviours such as aggressiveness, destruction of objects and hyperactivity) (Harley et al. 2013). In agreement, the group of Kundakovic examined DNA methylation of BDNF IV in cord blood samples from the Columbia Center for Children's Environmental Health (CCCEH) human cohort. As a result, high maternal exposure to BPA was shown to be associated with emotion regulation and increased aggressive behaviour in boys. Additionally, there was an alteration of BDNF expression and DNA methylation, which allows an association between the effects of BPA and several psychiatric disorders such as depression, schizophrenia, bipolar disorder, and ASD (Kundakovic et al. 2015). Moreover, Perez-Lobato R et al. analysed environmental BPA exposure of 300 children, belonging to the Environment and Childhood (INMA) Granada birth cohort, and assessed their child behaviour. Higher concentrations of BPA were associated with worse behavioural scores on all scales and BPA-exposed children had somatic complaints, thinking problems, and major social problems (Perez-Lobato et al. 2016). Pregnant women at 23–35 weeks of gestation between July 2002 and October 2005, from the Sapporo Toho Hospital in Hokkaido, Japan (Sapporo Cohort) were recruited by Minatoya M et al. No association between BPA level and either mental or psychomotor development at 6 and 18 months of age was found. However, it was found that at 42 months of age, the level of BPA at the umbilical cord was positively associated with increased scores of internalizing, externalizing, and developmental problems (Minatoya et al. 2017). Besides, Braun JM et al. used data from the Maternal-Infant Research on Environmental Chemicals (MIREC) study, which recruited 2,000 women in their first trimester of pregnancy from obstetric and prenatal clinics in Canada from 2008 to 2011. Prenatal urine BPA concentration was associated with some aspects of child behaviour, and some associations were stronger among boys (Braun et al. 2017b). The same group used the HOME study and followed 346 mother–child pairs (enrolled 2003–2006) from Cincinnati, OH, concluding that prenatal BPA concentrations were persistently associated with more externalizing behaviours (Braun et al. 2017c). On the other hand, Stacy SL et al. used data from the same study and showed that prenatal exposure to BPA was associated with externalizing behaviours in girls and at age 8 in boys (Stacy et al. 2017). In the Environment and Reproductive Health (EARTH) Study associations of BPA concentrations between parents and children were also analysed. Nonetheless, parental BPA concentrations were not associated with the Behavior-Assessment-System-for-Children-2 (BASC-2) index of behavioural symptoms, and internalizing or externalizing problems (Skarha et al. 2020). In contrast, the group of Li J explored the association between prenatal BPA exposure and childhood behavioural risks at ages 2 and 4 years, showing a positive association between maternal urinary concentrations of BPA during pregnancy and the risks of emotional problems, anxiety/depression problems, and internalizing problems in boys at ages 2 and 4 years. As in other studies, this association was more pronounced among boys (Li et al. 2020). Furthermore, this positive association were also observed with emotional symptoms, but not with cognitive and psychomotor development (Garí et al. 2021). Moreover, Liu J et al. investigated whether prenatal maternal exposure to BPA or BPS is associated with neurodevelopment in children at two years of age. Maternal selenium and child sex were thus found to be significant modifiers of the effect of BPA, which was negatively associated with socioemotional scores for boys but positive for girls. Still, higher exposure to bisphenols was associated with lower motor scores with lower maternal selenium levels by the Bayley Scales of Infant Development-III (Bayley-III) (Liu et al. 2021). England-Mason G et al. conducted a study in children between 2 and 4 years of age, recruited from the Alberta Pregnancy Outcomes and Nutrition (APrON) study. Child sex modified the associations between postnatal maternal BPA and changes in executive function, and thus higher concentrations of postnatal maternal BPA caused gradual problems in the domains of inhibitory self-control and emergent metacognition in girls (England-Mason et al. 2021). In another article, the same authors found an association between prenatal exposure to BPA and two of the high molecular weight phthalate-associated cytosine-phosphate-guanine sites in buccal epithelial cells, through maternal-child pairs recruited between 2009 and 2012 from the same data (England-Mason et al. 2022). The BPA exposure was also positively associated with adolescent thinking problems and somatic complaints in 130 boys from the INMA project (Mustieles et al. 2022).
Autism spectrum disorder (ASD)
Concerning the link between BPA exposure and ASD, Kondolot M et al. studied plasma levels of phthalates and BPA along with oxidant/antioxidant status in 51 autistic children admitted to Erciyes University Child Psychiatry Clinic in Kayseri between July 2011 and August 2012. 12 of these children were diagnosed with Pervasive Developmental Disorder-Not Otherwise Specified (PDD-NOS). As a result, plasma BPA levels of children with PDD-NOS were significantly higher than in autistic children and healthy children. Thus, was concluded that autistic children show increased oxidative stress due to increased exposure to BPA (Kondolot et al. 2016). From Danish participants from the Odense Child Cohort, Hansen JB et al. evaluated uterus exposure to BPA, with the aim of understanding if there is an association with ADHD and/or ASD. The data suggested an association in girls between BPA exposure and ASD score (Hansen et al. 2021). On the other hand, the group of Kim K quantified some types of phenols, such as BPA in 218 pregnant women from Markers of Autism Risk in Babies—Learning Early Signs (MARBLES). Although this study did not obtain results of cognitive effects (Kim et al. 2021). Four phenols were associated with ASD in the MARBLES study by Shin HM et al., which concluded that diet was the major source of BPA exposure, and when comparing BPA urinary concentrations between MARBLES versus NHANES, the women that had a child with ASD, had lower concentrations of BPA urinary, as they were more aware/concerned about using BPA-rich utensils (Shin et al. 2021). Besides, Santos JX et al. also performed a study to identify 77 genes with high evidence of a link to ASD and then found that BPA interacts with 35 of these genes (Santos et al. 2022).
Attention-deficit/hyperactivity disorder (ADHD)
Regarding the association of the exposure of BPA with ADHD, Adesman A et al. examined the association between infant formula feeding and preschool ADHD in 2 comparable cohorts. For this study, the National Survey of Children's Health (NSCH) data from 2007 and 2011/2012, for children with ages 3 to 5 years, was used. ADHD was more common among formula-fed infants in 2007, but not in the 2011/2012 sample, where BPA exposure was markedly reduced, indicating that the reduced prevalence of ADHD among breastfed infants may not be due to the nutritional benefits of breast milk, but rather to early BPA exposure (Adesman et al. 2017). On the other hand, with data from the prospective Odense Child Cohort, the research group of Jensen TK investigated whether the concentration of BPA in maternal urine during pregnancy was associated with ADHD and language development in children aged 18 to 36 months. BPA was detected in 85.3% of maternal urine samples, and it was concluded that boys of mothers with high BPA concentration were 3.70 more likely to have a low language score (Jensen et al. 2019). Tsai CS et al. examined some EDCs, such as BPA, to understand whether they affect the gonadal hormones and whether this was related to ADHD susceptibility. Children with or without ADHD in the study were tested and it was concluded that the level of BPA was higher in boys with ADHD than in healthy boys (Tsai et al. 2020). Furthermore, Huang Z et al. analysed serum BPA concentrations and assessed behaviour and cognitive function in 3–4-year-old children from the China-Anhui Birth Cohort (C-ABCS). As a result, boys with the highest prenatal BPA concentrations showed an increase in conduct problems, while girls had behavioural and relationship problems. Therefore, high prenatal BPA concentrations have been shown to have a relationship with increased ADHD (Huang et al. 2022b). This association was also analysed in uterus exposure but no associations between BPA exposure and ADHD were observed (Hansen et al. 2021). On the other hand, Wang LJ et al. studied the differential levels between ADHD patients and healthy controls and no significant mediating effect of IGF-1 was found between BPA and ADHD (Wang et al. 2022b). Conversely, Kim JI et al. analysed the associations between BPA, BPF and BPS with ADHD symptoms at various periods of childhood, measuring BPA levels at 4, 6 and 8 years. ADHD symptoms were assessed using the ADHD Rating Scale IV (ARS). BPA was detected in about 97% of the participants, more than double that of other bisphenols. A doubling of BPA levels was associated with increased ARS scores by 4.7% at age 6 years, and there was therefore an association of BPA with attention-deficit/hyperactivity disorder above a threshold of 3.0 μg/g creatinine. However, BPA showed non-linear relationships with ADHD symptoms, but on the other hand, exposure to BPF and BPS was associated with greater ADHD symptoms at age 6 (Kim et al. 2022).
Stroke prevalence
Regarding the linking between BPA exposure and Stroke prevalence, still very weak and recently, the research group of Cai S associated for the first time Stroke with urinary BPA. This study was conducted with participants from the United States National Health and Nutrition Examination Surveys (NHANES) between 2003 and 2014. Therefore, a relationship was observed between urinary BPA and the increased prevalence of Stroke in the US population, and this was more evident in men, in 9139 participants, 324 people suffered from stroke (Cai et al. 2020).
In summary, the set of epidemiological studies presented suggests that BPA prenatal exposure seems to be related to the development of several neurological diseases in children like ADHD, ASD, depression, emotional problems (internalizing and externalizing problems), anxiety, cognitive disorders, and others (Table 4). Thus, several studies have always tried to relate the harmful effects of BPA on neurodevelopment in children, using remarkably diverse data. As for the adult studies, this consistency was not so clear, and of the four studies, only Cai et al. (2020) positively related urinary BPA with increased prevalence of Stroke and obtained worrisome results, but the remaining studies did not associate BPA with neurological diseases. Thus, we can infer that more prospective studies are needed to find the causal inference of BPA, and therefore caution is needed in their comparative analysis.
Conclusions
In conclusion, BPA exposure is linked to an increasing prevalence of neurological disorders and diseases, based on the analysis of several BPA-induced neurological toxicity studies in animal models and humans. It’s now proved that BPA can have harmful effects on brain health, even when acting as an EDC at lower doses, especially during more vulnerable stages of development, such as pregnancy and the first years of a baby's life. In this analysis, it was seen that BPA exposure impairs various structural and molecular brain changes. In vitro, it was observed that BPA promotes oxidative stress, changing expression levels of several crucial genes and proteins. However, in vivo, was seen similar effects, adding to the destructive effects on neurotransmitters, excitotoxicity and neuroinflammation, and damaged blood–brain barrier function, leading to deteriorated cognitive functions and cholinergic system, impaired spatial learning and memory capacity, neurodegenerative diseases, and neuropsychological disorders. On the other hand, human in vitro studies showed effects such as neuronal damage, apoptosis effects, disruption of intracellular Ca2+ homeostasis, a significant increase in ROS, promoted apoptosis and LDH release, decreased axon length, microglial DNA damage, astrogliosis, BCRP inhibition, and significantly reduced myelination. Finally, epidemiological studies have demonstrated the harmful effects of BPA on neurodevelopment in children leading to the development of considerable neurological diseases like ADHD, ASD, depression, emotional problems, anxiety, and cognitive disorders. However, this type of study also reveals a positively related urinary BPA with increased prevalence of Stroke, which are worrying results.
Therefore, it becomes obvious that human daily exposure is not safe and that the issues caused by the widespread usage of this EDC are still present. The various experimental methods used, as well as adjustments to dose amounts, exposure times, or even the experimental model employed, might be used to support the contentious research. In this regard, more studies are needed to further clarify the mechanism of BPA toxicity in the neurological system. Furthermore, the fact that humans are frequently exposed to numerous endocrine disruptors, including bisphenols, highlights the necessity of researching co-exposure patterns and/or the “exposome” to best address the negative effects of this EDC on neurological health while always considering multiple exposures. A crucial stage in the progress of research on these substances is the creation of new BPA analogues as well as the examination of the safety of those analogues already created today. There should be no health concerns associated with environmental or human exposure to these substances, especially for the most susceptible populations like children and pregnant women. It's crucial to use public health strategies to determine the best ways to reduce BPA exposure. This includes promoting the use of glass containers for food storage and reducing the use of canned goods, plastic containers, water supply pipes and many more products that contain BPA. This will improve people's quality of life and reduce the risk of BPA-induced neurological toxicity.
Data availability
Data sharing not applicable to this article as no datasets were generated or analysed during the current study.
Abbreviations
- 5-HT:
-
Serotonin
- ACh:
-
Acetylcholine
- AChE:
-
Acetilcolinesterase
- ADHD:
-
Attention-deficit/hyperactivity disorder
- AR:
-
Androgen receptors
- ASD:
-
Autism spectrum disorder
- Aβ:
-
Amyloid-β
- BADGE:
-
Bisphenol A diglycidyl ether
- BCRP:
-
Breast cancer resistance protein
- BDNF:
-
Brain-derived neurotrophic factor
- BPA:
-
Bisphenol A
- BPAF:
-
Bisphenol AF
- BPB:
-
Bisphenol B
- BPF:
-
Bisphenol F
- BPS:
-
Bisphenol S
- Ca2+ :
-
Calcium
- CAT:
-
Catalase
- DA:
-
Dopamine
- DRP-1:
-
Dynamin-related protein 1
- EDC:
-
Endocrine-disrupting compound
- EGCG:
-
Epigallocatechin-3-gallate
- ER:
-
Estrogen receptors
- GABA:
-
Gamma-aminobutyric acid
- GFAP:
-
Glial fibrillary acidic protein
- GnRH:
-
Gonadotropin-releasing hormone
- GSH:
-
Glutathione
- GST:
-
Glutathione-S-transferase
- HDAC2:
-
Histone deacetylase
- hESC:
-
Human embryonic stem cells
- hiPSC:
-
Human induced pluripotent stem cell
- HOME:
-
Health Outcomes and Measures of the Environment
- IGF-1:
-
Insulin-like growth factor 1
- LDH:
-
Lactate dehydrogenase
- lncRNA:
-
Long non-coding RNAs
- MARBLES:
-
Markers of Autism Risk in Babies-Learning Early Signs
- MBP:
-
4-Metil-2,4-bis(4-hidroxifenil)pent-1-eno
- MCAo:
-
Middle cerebral artery occlusion
- MCAO/R:
-
Middle cerebral artery occlusion and reperfusion
- MCP1:
-
Monocyte chemoattractant protein-1
- MDA:
-
Malondialdehyde
- MetS:
-
Metabolic syndrome
- miRNA:
-
MicroRNAs
- MMP:
-
Mitochondrial membrane potential
- mRNA:
-
Messenger RNA
- NHANES:
-
United States National Health and Nutrition Examination Surveys
- NO:
-
Nitric oxide
- NOS:
-
Nitric oxide synthases
- NPPs:
-
Nano-sized plastic particles
- NSC:
-
Neural stem cells
- OGA:
-
O-GlcNAcase protein
- OXPHOs:
-
Oxidative phosphorylation
- PDI:
-
Protein disulfide isomerase
- PFC:
-
Prefrontal cortex
- PPAR-γ:
-
Peroxisome proliferator-activated receptor gamma
- PSD-95:
-
Postsynaptic density protein-95
- p-tau:
-
Phosphorylated tau protein
- PUMA:
-
P53 upregulated modulator of apoptosis
- ROS:
-
Reactive oxygen species
- SELMA:
-
Swedish Environmental Longitudinal, Mother and child, Asthma and allergy
- CNS:
-
Central nervous system
- SOD:
-
Superoxide dismutase
- Syn2α:
-
Anti-synapsin 2α
- SYP:
-
Synaptophysin
- γ-IR:
-
γ-Radiation
References
Abdel-Rafei MK, Thabet NM (2020) Modulatory effect of methylsulfonylmethane against BPA/γ-radiation induced neurodegenerative alterations in rats: Influence of TREM-2/DAP-12/Syk pathway. Life Sci 260:118410. https://doi.org/10.1016/j.lfs.2020.118410
Abdou HM, Abd Elkader HAE, El-Gendy AH, Eweda SM (2022) Neurotoxicity and neuroinflammatory effects of bisphenol A in male rats: the neuroprotective role of grape seed proanthocyanidins. Environ Sci Pollut Res Int 29(6):9257–9268. https://doi.org/10.1007/s11356-021-16311-1
Abrantes-Soares F, Lorigo M, Cairrao E (2022) Effects of BPA substitutes on the prenatal and cardiovascular systems. Crit Rev Toxicol 52(6):469–498. https://doi.org/10.1080/10408444.2022.2142514
Acconcia F, Pallottini V, Marino M (2015) Molecular mechanisms of action of BPA. Dose Response 13(4):1559325815610582. https://doi.org/10.1177/1559325815610582
Adesman A, Soled D, Rosen L (2017) Formula feeding as a risk factor for attention-deficit/hyperactivity disorder: is bisphenol a exposure a smoking gun? J Dev Behav Pediatr 38(7):545–551. https://doi.org/10.1097/dbp.0000000000000468
Agarwal S, Tiwari SK, Seth B et al (2015) Activation of autophagic flux against xenoestrogen bisphenol-A-induced hippocampal neurodegeneration via AMP kinase (AMPK)/Mammalian Target of Rapamycin (mTOR) Pathways. J Biol Chem 290(34):21163–21184. https://doi.org/10.1074/jbc.M115.648998
Agarwal S, Yadav A, Tiwari SK et al (2016) Dynamin-related protein 1 inhibition mitigates bisphenol A-mediated alterations in mitochondrial dynamics and neural stem cell proliferation and differentiation. J Biol Chem 291(31):15923–15939. https://doi.org/10.1074/jbc.M115.709493
Ahmad A, Patel V, Xiao J, Khan MM (2020) The role of neurovascular system in neurodegenerative diseases. Mol Neurobiol 57(11):4373–4393. https://doi.org/10.1007/s12035-020-02023-z
Akintunde JK, Akintola TE, Adenuga GO, Odugbemi ZA, Adetoye RO, Akintunde OG (2020) naringin attenuates bisphenol-A mediated neurotoxicity in hypertensive rats by abrogation of cerebral nucleotide depletion, oxidative damage and neuroinflammation. Neurotoxicology 81:18–33. https://doi.org/10.1016/j.neuro.2020.08.001
Arambula SE, Jima D, Patisaul HB (2018) Prenatal bisphenol A (BPA) exposure alters the transcriptome of the neonate rat amygdala in a sex-specific manner: a CLARITY-BPA consortium study. Neurotoxicology 65:207–220. https://doi.org/10.1016/j.neuro.2017.10.005
Arita Y, Park HJ, Cantillon A, Getahun D, Menon R, Peltier MR (2019) Effect of bisphenol-A (BPA) on placental biomarkers for inflammation, neurodevelopment and oxidative stress. J Perinat Med 47(7):741–749. https://doi.org/10.1515/jpm-2019-0045
Balakrishnan B, Henare K, Thorstensen EB, Ponnampalam AP, Mitchell MD (2010) Transfer of bisphenol A across the human placenta. Am J Obstet Gynecol 202(4):393.e1–7. https://doi.org/10.1016/j.ajog.2010.01.025
Banerjee O, Singh S, Saha I et al (2022) Molecular dissection of cellular response of pancreatic islet cells to Bisphenol-A (BPA): a comprehensive review. Biochem Pharmacol 201:115068. https://doi.org/10.1016/j.bcp.2022.115068
Bashir DW, Ahmed YH, El-Sakhawy MA (2022) Ameliorative effect of vitamin E and selenium against bisphenol A-induced toxicity in spinal cord and submandibular salivary glands of adult male albino rats. Int J Environ Health Res. https://doi.org/10.1080/09603123.2022.2067327
Bi N, Ding J, Zou R, Gu X, Liu ZH, Wang HL (2021) Developmental exposure of bisphenol A induces spatial memory deficits by weakening the excitatory neural circuits of CA3-CA1 and EC-CA1 in mice. Toxicol Appl Pharmacol 426:115641. https://doi.org/10.1016/j.taap.2021.115641
Bi N, Gu X, Fan A et al (2022) Bisphenol-A exposure leads to neurotoxicity through upregulating the expression of histone deacetylase 2 in vivo and in vitro. Toxicology 465:153052. https://doi.org/10.1016/j.tox.2021.153052
Birla H, Keswani C, Rai SN et al (2019) Neuroprotective effects of Withania somnifera in BPA induced-cognitive dysfunction and oxidative stress in mice. Behav Brain Funct 15(1):9. https://doi.org/10.1186/s12993-019-0160-4
Björnsdotter MK, Jonker W, Legradi J, Kool J, Ballesteros-Gómez A (2017) Bisphenol A alternatives in thermal paper from the Netherlands, Spain, Sweden and Norway. Screening and potential toxicity. Sci Total Environ 601–602:210–221. https://doi.org/10.1016/j.scitotenv.2017.05.171
Bornehag CG, Engdahl E, Unenge Hallerbäck M et al (2021) Prenatal exposure to bisphenols and cognitive function in children at 7 years of age in the Swedish SELMA study. Environ Int 150:106433. https://doi.org/10.1016/j.envint.2021.106433
Boudalia S, Malha O (2016) Bisphenol-A: legislation in Industrials Countries and in Algeria. Res J Environ Toxicol 10:189–192. https://doi.org/10.3923/rjet.2016.189.192
Braun JM (2017) Early-life exposure to EDCs: role in childhood obesity and neurodevelopment. Nat Rev Endocrinol 13(3):161–173. https://doi.org/10.1038/nrendo.2016.186
Braun JM, Bellinger DC, Hauser R et al (2017a) Prenatal phthalate, triclosan, and bisphenol A exposures and child visual-spatial abilities. Neurotoxicology 58:75–83. https://doi.org/10.1016/j.neuro.2016.11.009
Braun JM, Muckle G, Arbuckle T et al (2017b) Associations of prenatal urinary bisphenol A concentrations with child behaviors and cognitive abilities. Environ Health Perspect 125(6):067008. https://doi.org/10.1289/ehp984
Braun JM, Yolton K, Stacy SL et al (2017c) Prenatal environmental chemical exposures and longitudinal patterns of child neurobehavior. Neurotoxicology 62:192–199. https://doi.org/10.1016/j.neuro.2017.07.027
Caglayan C, Kandemir FM, Ayna A, Gür C, Küçükler S, Darendelioğlu E (2022) Neuroprotective effects of 18β-glycyrrhetinic acid against bisphenol A-induced neurotoxicity in rats: involvement of neuronal apoptosis, endoplasmic reticulum stress and JAK1/STAT1 signaling pathway. Metab Brain Dis 37(6):1931–1940. https://doi.org/10.1007/s11011-022-01027-z
Cai S, Rao X, Ye J et al (2020) Relationship between urinary bisphenol a levels and cardiovascular diseases in the U.S. adult population, 2003–2014. Ecotoxicol Environ Saf 192:110300. https://doi.org/10.1016/j.ecoenv.2020.110300
Calafat AM, Ye X, Wong LY, Reidy JA, Needham LL (2008) Exposure of the U.S. population to bisphenol A and 4-tertiary-octylphenol: 2003–2004. Environ Health Perspect 116(1):39–44. https://doi.org/10.1289/ehp.10753
Campanale C, Massarelli C, Savino I, Locaputo V, Uricchio VF (2020) A detailed review study on potential effects of microplastics and additives of concern on human health. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph17041212
Castro B, Sánchez P, Torres JM, Ortega E (2013) Effects of adult exposure to bisphenol a on genes involved in the physiopathology of rat prefrontal cortex. PLoS ONE 8(9):e73584. https://doi.org/10.1371/journal.pone.0073584
Castro B, Sánchez P, Miranda MT, Torres JM, Ortega E (2015) Identification of dopamine- and serotonin-related genes modulated by bisphenol A in the prefrontal cortex of male rats. Chemosphere 139:235–239. https://doi.org/10.1016/j.chemosphere.2015.06.061
Certo M, Endo Y, Ohta K, Sakurada S, Bagetta G, Amantea D (2015) Activation of RXR/PPARγ underlies neuroprotection by bexarotene in ischemic stroke. Pharmacol Res 102:298–307. https://doi.org/10.1016/j.phrs.2015.10.009
Chen Q, Yin D, Jia Y et al (2017) Enhanced uptake of BPA in the presence of nanoplastics can lead to neurotoxic effects in adult zebrafish. Sci Total Environ 609:1312–1321. https://doi.org/10.1016/j.scitotenv.2017.07.144
Chesnut M, Paschoud H, Repond C et al (2021) Human IPSC-derived model to study Myelin disruption. Int J Mol Sci. https://doi.org/10.3390/ijms22179473
Chianese R, Coccurello R, Viggiano A et al (2018a) Impact of dietary fats on brain functions. Curr Neuropharmacol 16(7):1059–1085. https://doi.org/10.2174/1570159x15666171017102547
Chianese R, Troisi J, Richards S et al (2018b) Bisphenol A in reproduction: epigenetic effects. Curr Med Chem 25(6):748–770. https://doi.org/10.2174/0929867324666171009121001
Cho JH, Kim AH, Lee S et al (2018) Sensitive neurotoxicity assessment of bisphenol A using double immunocytochemistry of DCX and MAP2. Arch Pharm Res 41(11):1098–1107. https://doi.org/10.1007/s12272-018-1077-4
Cimmino I, Fiory F, Perruolo G et al (2020) Potential mechanisms of bisphenol A (BPA) contributing to human disease. Int J Mol Sci 21(16):5761. https://doi.org/10.3390/ijms21165761
Cooper BL, Posnack NG (2022) Characteristics of bisphenol cardiotoxicity: impaired excitability, contractility, and relaxation. Cardiovasc Toxicol 22(3):273–280. https://doi.org/10.1007/s12012-022-09719-9
Coumailleau P, Trempont S, Pellegrini E, Charlier TD (2020) Impacts of bisphenol A analogues on zebrafish post-embryonic brain. J Neuroendocrinol 32(8):e12879. https://doi.org/10.1111/jne.12879
D’Angelo S, Scafuro M, Meccariello R (2019) BPA and nutraceuticals, simultaneous effects on endocrine functions. Endocr Metab Immune Disord Drug Targets 19(5):594–604. https://doi.org/10.2174/1871530319666190101120119
Di Pietro P, D’Auria R, Viggiano A et al (2020) Bisphenol A induces DNA damage in cells exerting immune surveillance functions at peripheral and central level. Chemosphere 254:126819. https://doi.org/10.1016/j.chemosphere.2020.126819
Dualde P, León N, Sanchis Y et al (2021) Biomonitoring of phthalates, bisphenols and parabens in children: exposure, predictors and risk assessment. Int J Environ Res Public Health 18(17):8909. https://doi.org/10.3390/ijerph18178909
El Morsy EM, Ahmed M (2020) Protective effects of lycopene on hippocampal neurotoxicity and memory impairment induced by bisphenol A in rats. Hum Exp Toxicol 39(8):1066–1078. https://doi.org/10.1177/0960327120909882
El Tabaa MM, Sokkar SS, Ramdan ES, El Salam IZA, Anis A (2022) Does (−)-epigallocatechin-3-gallate protect the neurotoxicity induced by bisphenol A in vivo? Environ Sci Pollut Res Int 29(21):32190–32203. https://doi.org/10.1007/s11356-021-18408-z
Elbakry MMM, Mansour SZ, Helal H, Ahmed ESA (2022) Nattokinase attenuates bisphenol A or gamma irradiation-mediated hepatic and neural toxicity by activation of Nrf2 and suppression of inflammatory mediators in rats. Environ Sci Pollut Res Int 29(49):75086–75100. https://doi.org/10.1007/s11356-022-21126-9
El-Missiry MA, Othman AI, Al-Abdan MA, El-Sayed AA (2014) Melatonin ameliorates oxidative stress, modulates death receptor pathway proteins, and protects the rat cerebrum against bisphenol-A-induced apoptosis. J Neurol Sci 347(1–2):251–256. https://doi.org/10.1016/j.jns.2014.10.009
Engdahl E, van Schijndel MDM, Voulgaris D et al (2021) Bisphenol A inhibits the transporter function of the blood-brain barrier by directly interacting with the ABC transporter breast cancer resistance protein (BCRP). Int J Mol Sci 22(11):5534. https://doi.org/10.3390/ijms22115534
England-Mason G, Liu J, Martin JW, Giesbrecht GF, Letourneau N, Dewey D (2021) Postnatal BPA is associated with increasing executive function difficulties in preschool children. Pediatr Res 89(3):686–693. https://doi.org/10.1038/s41390-020-0922-6
England-Mason G, Merrill SM, Gladish N et al (2022) Prenatal exposure to phthalates and peripheral blood and buccal epithelial DNA methylation in infants: an epigenome-wide association study. Environ Int 163:107183. https://doi.org/10.1016/j.envint.2022.107183
Escobar R, Soutullo CA, Hervas A, Gastaminza X, Polavieja P, Gilaberte I (2005) Worse quality of life for children with newly diagnosed attention-deficit/hyperactivity disorder, compared with asthmatic and healthy children. Pediatrics 116(3):e364–e369. https://doi.org/10.1542/peds.2005-0386
Essawy AE, Abd Elkader HAE, Khamiss OA, Eweda SM, Abdou HM (2021) Therapeutic effects of astragaloside IV and Astragalus spinosus saponins against bisphenol A-induced neurotoxicity and DNA damage in rats. PeerJ 9:e11930. https://doi.org/10.7717/peerj.11930
Evans SF, Kobrosly RW, Barrett ES et al (2014) Prenatal bisphenol A exposure and maternally reported behavior in boys and girls. Neurotoxicology 45:91–99. https://doi.org/10.1016/j.neuro.2014.10.003
Fonseca MI, Lorigo M, Cairrao E (2022) Endocrine-disrupting effects of bisphenol A on the cardiovascular system: a review. J Xenobiotics 12(3):181–213. https://doi.org/10.3390/jox12030015
Fraser TWK, Khezri A, Jusdado JGH, Lewandowska-Sabat AM, Henry T, Ropstad E (2017) Toxicant induced behavioural aberrations in larval zebrafish are dependent on minor methodological alterations. Toxicol Lett 276:62–68. https://doi.org/10.1016/j.toxlet.2017.05.021
Freire C, Vela-Soria F, Beneito A et al (2020) Association of placental concentrations of phenolic endocrine disrupting chemicals with cognitive functioning in preschool children from the Environment and Childhood (INMA) Project. Int J Hyg Environ Health 230:113597. https://doi.org/10.1016/j.ijheh.2020.113597
Fu J, Guo Y, Yang L, Han J, Zhou B (2020) Nano-TiO(2) enhanced bioaccumulation and developmental neurotoxicity of bisphenol a in zebrafish larvae. Environ Res 187:109682. https://doi.org/10.1016/j.envres.2020.109682
Garí M, Moos R, Bury D et al (2021) Human-Biomonitoring derived exposure and Daily Intakes of Bisphenol A and their associations with neurodevelopmental outcomes among children of the Polish Mother and Child Cohort Study. Environ Health 20(1):95. https://doi.org/10.1186/s12940-021-00777-0
Geens T, Neels H, Covaci A (2012) Distribution of bisphenol-A, triclosan and n-nonylphenol in human adipose tissue, liver and brain. Chemosphere 87(7):796–802. https://doi.org/10.1016/j.chemosphere.2012.01.002
Gill S, Kumara VMR (2021) Comparative Neurodevelopment effects of bisphenol A and bisphenol F on rat fetal neural stem cell models. Cells 10(4):793. https://doi.org/10.3390/cells10040793
Gomes IDL, Gazo I, Nabi D et al (2019) Bisphenols disrupt differentiation of the pigmented cells during larval brain formation in the ascidian. Aquat Toxicol 216:105314. https://doi.org/10.1016/j.aquatox.2019.105314
Gore AC, Moore T, Groom MJ, Thompson LM (2022) Prenatal exposure to an EDC mixture, neuromix: effects on brain, behavior, and stress responsiveness in rats. Toxics 10(3):122. https://doi.org/10.3390/toxics10030122
Goyal S, Tiwari S, Seth B et al (2021) Bisphenol-A inhibits mitochondrial biogenesis via impairment of GFER mediated mitochondrial protein import in the rat brain hippocampus. Neurotoxicology 85:18–32. https://doi.org/10.1016/j.neuro.2021.04.001
Gu YX, Liang XX, Yin NY et al (2019) New insights into mechanism of bisphenol analogue neurotoxicity: implications of inhibition of O-GlcNAcase activity in PC12 cells. Arch Toxicol 93(9):2661–2671. https://doi.org/10.1007/s00204-019-02525-3
Gu J, Guo M, Zheng L et al (2021) Protective effects of lignin-carbohydrate complexes from wheat stalk against bisphenol a neurotoxicity in zebrafish via oxidative stress. Antioxidants (basel) 10(10):1640. https://doi.org/10.3390/antiox10101640
Gu J, Guo M, Yin X et al (2022) A systematic comparison of neurotoxicity of bisphenol A and its derivatives in zebrafish. Sci Total Environ 805:150210. https://doi.org/10.1016/j.scitotenv.2021.150210
Guignard D, Canlet C, Tremblay-Franco M et al (2022) Gestational exposure to bisphenol A induces region-specific changes in brain metabolomic fingerprints in sheep. Environ Int 165:107336. https://doi.org/10.1016/j.envint.2022.107336
Guo Y, Chen L, Wu J et al (2019) Parental co-exposure to bisphenol A and nano-TiO(2) causes thyroid endocrine disruption and developmental neurotoxicity in zebrafish offspring. Sci Total Environ 650(Pt 1):557–565. https://doi.org/10.1016/j.scitotenv.2018.09.007
Guo J, Wu C, Zhang J et al (2020) Prenatal exposure to mixture of heavy metals, pesticides and phenols and IQ in children at 7 years of age: the SMBCS study. Environ Int 139:105692. https://doi.org/10.1016/j.envint.2020.105692
Gyimah E, Xu H, Dong X et al (2021) Developmental neurotoxicity of low concentrations of bisphenol A and S exposure in zebrafish. Chemosphere 262:128045. https://doi.org/10.1016/j.chemosphere.2020.128045
Hansen JB, Bilenberg N, Timmermann CAG et al (2021) Prenatal exposure to bisphenol A and autistic- and ADHD-related symptoms in children aged 2 and5 years from the Odense Child Cohort. Environ Health 20(1):24. https://doi.org/10.1186/s12940-021-00709-y
Haridevamuthu B, Guru A, Murugan R et al (2022) Neuroprotective effect of Biochanin a against Bisphenol A-induced prenatal neurotoxicity in zebrafish by modulating oxidative stress and locomotory defects. Neurosci Lett 790:136889. https://doi.org/10.1016/j.neulet.2022.136889
Harley KG, Gunier RB, Kogut K et al (2013) Prenatal and early childhood bisphenol A concentrations and behavior in school-aged children. Environ Res 126:43–50. https://doi.org/10.1016/j.envres.2013.06.004
Hass U, Christiansen S, Boberg J, Rasmussen MG, Mandrup K, Axelstad M (2016) Low-dose effect of developmental bisphenol A exposure on sperm count and behaviour in rats. Andrology 4(4):594–607. https://doi.org/10.1111/andr.12176
Henriksen AD, Andrade A, Harris EP, Rissman EF, Wolstenholme JT (2020) Bisphenol a exposure in utero disrupts hypothalamic gene expression particularly genes suspected in autism spectrum disorders and neuron and hormone signaling. Int J Mol Sci 21(9):3129. https://doi.org/10.3390/ijms21093129
Hoekstra EJ, Simoneau C (2013) Release of bisphenol A from polycarbonate: a review. Crit Rev Food Sci Nutr 53(4):386–402. https://doi.org/10.1080/10408398.2010.536919
Huang B, Jiang C, Luo J, Cui Y, Qin L, Liu J (2014) Maternal exposure to bisphenol A may increase the risks of Parkinson’s disease through down-regulation of fetal IGF-1 expression. Med Hypotheses 82(3):245–249. https://doi.org/10.1016/j.mehy.2013.10.023
Huang B, Ning S, Zhang Q et al (2017) Bisphenol A represses dopaminergic neuron differentiation from human embryonic stem cells through downregulating the expression of insulin-like growth factor 1. Mol Neurobiol 54(5):3798–3812. https://doi.org/10.1007/s12035-016-9898-y
Huang CF, Liu SH, Su CC et al (2021) Roles of ERK/Akt signals in mitochondria-dependent and endoplasmic reticulum stress-triggered neuronal cell apoptosis induced by 4-methyl-2,4-bis(4-hydroxyphenyl)pent-1-ene, a major active metabolite of bisphenol A. Toxicology 455:152764. https://doi.org/10.1016/j.tox.2021.152764
Huang Y, Zhang W, Zhang C et al (2022a) Rapid and reagent-free bioassay using autobioluminescent yeasts to detect agonistic and antagonistic activities of bisphenols against rat androgen receptor and progesterone receptor. J Steroid Biochem Mol Biol 222:106151. https://doi.org/10.1016/j.jsbmb.2022.106151
Huang Z, Fu W, Dou L et al (2022b) Prenatal bisphenol A exposure and early childhood behavior and cognitive function: a Chinese birth cohort study. Neuroendocrinology 112(4):311–323. https://doi.org/10.1159/000516881
Hutler Wolkowicz I, Svartz GV, Aronzon CM, Pérez Coll C (2016) Developmental toxicity of bisphenol A diglycidyl ether (epoxide resin badge) during the early life cycle of a native amphibian species. Environ Toxicol Chem 35(12):3031–3038. https://doi.org/10.1002/etc.3491
Hyun SA, Ko MY, Jang S et al (2022) Bisphenol-A impairs synaptic formation and function by RGS4-mediated regulation of BDNF signaling in the cerebral cortex. Dis Model Mech 15(7):dmm049177. https://doi.org/10.1242/dmm.049177
Iadecola C, Buckwalter MS, Anrather J (2020) Immune responses to stroke: mechanisms, modulation, and therapeutic potential. J Clin Invest 130(6):2777–2788. https://doi.org/10.1172/jci135530
Ishido M, Masuo Y, Terasaki M, Morita M (2011) Rat hyperactivity by bisphenol A, but not by its derivatives, 3-hydroxybisphenol A or bisphenol A 3,4-quinone. Toxicol Lett 206(3):300–305. https://doi.org/10.1016/j.toxlet.2011.08.011
Ishtiaq A, Ali T, Bakhtiar A et al (2021) Melatonin abated Bisphenol A-induced neurotoxicity via p53/PUMA/Drp-1 signaling. Environ Sci Pollut Res Int 28(14):17789–17801. https://doi.org/10.1007/s11356-020-12129-5
Jensen TK, Mustieles V, Bleses D et al (2019) Prenatal bisphenol A exposure is associated with language development but not with ADHD-related behavior in toddlers from the Odense Child Cohort. Environ Res 170:398–405. https://doi.org/10.1016/j.envres.2018.12.055
Jiang Y, Li J, Xu S et al (2020) Prenatal exposure to bisphenol A and its alternatives and child neurodevelopment at 2 years. J Hazard Mater 388:121774. https://doi.org/10.1016/j.jhazmat.2019.121774
Juhel G, Bayen S, Goh C, Lee WK, Kelly BC (2017) Use of a suite of biomarkers to assess the effects of carbamazepine, bisphenol A, atrazine, and their mixtures on green mussels. Perna Viridis Environ Toxicol Chem 36(2):429–441. https://doi.org/10.1002/etc.3556
Khadrawy YA, Noor NA, Mourad IM, Ezz HS (2016) Neurochemical impact of bisphenol A in the hippocampus and cortex of adult male albino rats. Toxicol Ind Health 32(9):1711–1719. https://doi.org/10.1177/0748233715579803
Khan J, Salhotra S, Ahmad S et al (2018) The protective effect of α-lipoic acid against bisphenol A-induced neurobehavioral toxicity. Neurochem Int 118:166–175. https://doi.org/10.1016/j.neuint.2018.06.005
Khan J, Salhotra S, Goswami P et al (2019) Bisphenol A triggers axonal injury and myelin degeneration with concomitant neurobehavioral toxicity in C57BL/6J male mice. Toxicology 428:152299. https://doi.org/10.1016/j.tox.2019.152299
Kharrazian D, Herbert M, Vojdani A (2019) The associations between immunological reactivity to the haptenation of unconjugated bisphenol A to albumin and protein disulfide isomerase with alpha-synuclein antibodies. Toxics 7(2):26. https://doi.org/10.3390/toxics7020026
Kim CS, Sapienza PP, Ross IA, Johnson W, Luu HM, Hutter JC (2004) Distribution of bisphenol A in the neuroendocrine organs of female rats. Toxicol Ind Health 20(1–5):41–50. https://doi.org/10.1191/0748233704th186oa
Kim S, Eom S, Kim HJ et al (2018) Association between maternal exposure to major phthalates, heavy metals, and persistent organic pollutants, and the neurodevelopmental performances of their children at 1 to 2years of age- CHECK cohort study. Sci Total Environ 624:377–384. https://doi.org/10.1016/j.scitotenv.2017.12.058
Kim K, Shin HM, Busgang SA et al (2021) Temporal trends of phenol, paraben, and triclocarban exposure in california pregnant women during 2007–2014. Environ Sci Technol 55(16):11155–11165. https://doi.org/10.1021/acs.est.1c01564
Kim JI, Lee YA, Shin CH, Hong YC, Kim BN, Lim YH (2022) Association of bisphenol A, bisphenol F, and bisphenol S with ADHD symptoms in children. Environ Int 161:107093. https://doi.org/10.1016/j.envint.2022.107093
Kimura E, Matsuyoshi C, Miyazaki W et al (2016) Prenatal exposure to bisphenol A impacts neuronal morphology in the hippocampal CA1 region in developing and aged mice. Arch Toxicol 90(3):691–700. https://doi.org/10.1007/s00204-015-1485-x
Klenke U, Constantin S, Wray S (2016) BPA directly decreases GnRH neuronal activity via noncanonical pathway. Endocrinology 157(5):1980–1990. https://doi.org/10.1210/en.2015-1924
Kobayashi Y, Oguro A, Yagi E, Mitani A, Kudoh SN, Imaoka S (2020) Bisphenol A and rotenone induce S-nitrosylation of protein disulfide isomerase (PDI) and inhibit neurite outgrowth of primary cultured cells of the rat hippocampus and PC12 cells. J Toxicol Sci 45(12):783–794. https://doi.org/10.2131/jts.45.783
Kodila A, Franko N, Sollner Dolenc M (2023) A review on immunomodulatory effects of BPA analogues. Arch Toxicol 97(7):1831–1846. https://doi.org/10.1007/s00204-023-03519-y
Kondolot M, Ozmert EN, Ascı A et al (2016) Plasma phthalate and bisphenol a levels and oxidant-antioxidant status in autistic children. Environ Toxicol Pharmacol 43:149–158. https://doi.org/10.1016/j.etap.2016.03.006
Kumamoto T, Oshio S (2013) Effect of fetal exposure to bisphenol A on brain mediated by X-chromosome inactivation. J Toxicol Sci 38(3):485–494. https://doi.org/10.2131/jts.38.485
Kundakovic M, Champagne FA (2011) Epigenetic perspective on the developmental effects of bisphenol A. Brain Behav Immun 25(6):1084–1093. https://doi.org/10.1016/j.bbi.2011.02.005
Kundakovic M, Gudsnuk K, Franks B et al (2013) Sex-specific epigenetic disruption and behavioral changes following low-dose in utero bisphenol A exposure. Proc Natl Acad Sci 110(24):9956–9961. https://doi.org/10.1073/pnas.1214056110
Kundakovic M, Gudsnuk K, Herbstman JB, Tang D, Perera FP, Champagne FA (2015) DNA methylation of BDNF as a biomarker of early-life adversity. Proc Natl Acad Sci USA 112(22):6807–6813. https://doi.org/10.1073/pnas.1408355111
Lama A, Del Piano F, Annunziata C et al (2023) Bisphenol A exacerbates anxiety-like behavior and neuroinflammation in prefrontal cortex of adult obese mice. Life Sci 313:121301. https://doi.org/10.1016/j.lfs.2022.121301
Lambré C, Barat Baviera JM, Bolognesi C et al (2023) Re-evaluation of the risks to public health related to the presence of bisphenol A (BPA) in foodstuffs. Efsa j 21(4):e06857. https://doi.org/10.2903/j.efsa.2023.6857
Le HH, Carlson EM, Chua JP, Belcher SM (2008) Bisphenol A is released from polycarbonate drinking bottles and mimics the neurotoxic actions of estrogen in developing cerebellar neurons. Toxicol Lett 176(2):149–156. https://doi.org/10.1016/j.toxlet.2007.11.001
Lee CT, Hsieh CF, Wang JY (2021) Bisphenol a induces autophagy defects and AIF-dependent apoptosis via HO-1 and AMPK to degenerate N2a neurons. Int J Mol Sci 22(20):10948. https://doi.org/10.3390/ijms222010948
Li J, Wang Y, Fang F et al (2016) Bisphenol A disrupts glucose transport and neurophysiological role of IR/IRS/AKT/GSK3β axis in the brain of male mice. Environ Toxicol Pharmacol 43:7–12. https://doi.org/10.1016/j.etap.2015.11.025
Li X, Guo J-Y, Li X et al (2017a) Behavioural effect of low-dose BPA on male zebrafish: tuning of male mating competition and female mating preference during courtship process. Chemosphere 169:40–52. https://doi.org/10.1016/j.chemosphere.2016.11.053
Li X, Sun MZ, Li X et al (2017b) Impact of low-dose chronic exposure to Bisphenol A (BPA) on adult male zebrafish adaption to the environmental complexity: disturbing the color preference patterns and reliving the anxiety behavior. Chemosphere 186:295–304. https://doi.org/10.1016/j.chemosphere.2017.07.164
Li F, Yang F, Li DK et al (2020) Prenatal bisphenol A exposure, fetal thyroid hormones and neurobehavioral development in children at 2 and 4 years: a prospective cohort study. Sci Total Environ 722:137887. https://doi.org/10.1016/j.scitotenv.2020.137887
Liang X, Yin N, Liang S et al (2020) Bisphenol A and several derivatives exert neural toxicity in human neuron-like cells by decreasing neurite length. Food Chem Toxicol 135:111015. https://doi.org/10.1016/j.fct.2019.111015
Lin CC, Chien CJ, Tsai MS, Hsieh CJ, Hsieh WS, Chen PC (2017) Prenatal phenolic compounds exposure and neurobehavioral development at 2 and 7years of age. Sci Total Environ 605–606:801–810. https://doi.org/10.1016/j.scitotenv.2017.06.160
Liu J, Martin LJ, Dinu I, Field CJ, Dewey D, Martin JW (2021) Interaction of prenatal bisphenols, maternal nutrients, and toxic metal exposures on neurodevelopment of 2-year-olds in the APrON cohort. Environ Int 155:106601. https://doi.org/10.1016/j.envint.2021.106601
Lorigo M, Cairrao E (2022) Fetoplacental vasculature as a model to study human cardiovascular endocrine disruption. Mol Aspects Med 87:101054. https://doi.org/10.1016/j.mam.2021.101054
Luo G, Wei R, Niu R, Wang C, Wang J (2013) Pubertal exposure to Bisphenol A increases anxiety-like behavior and decreases acetylcholinesterase activity of hippocampus in adult male mice. Food Chem Toxicol 60:177–180. https://doi.org/10.1016/j.fct.2013.07.037
Luo M, Li L, Ding M et al (2023) Long-term potentiation and depression regulatory microRNAs were highlighted in Bisphenol A induced learning and memory impairment by microRNA sequencing and bioinformatics analysis. PLoS ONE 18(1):e0279029. https://doi.org/10.1371/journal.pone.0279029
Mao J, Kinkade JA, Bivens NJ, Rosenfeld CS (2021) miRNA changes in the mouse placenta due to bisphenol A exposure. Epigenomics 13(24):1909–1919. https://doi.org/10.2217/epi-2021-0339
Martínez MA, Rovira J, Sharma RP, Nadal M, Schuhmacher M, Kumar V (2017) Prenatal exposure estimation of BPA and DEHP using integrated external and internal dosimetry: a case study. Environ Res 158:566–575. https://doi.org/10.1016/j.envres.2017.07.016
Mathisen GH, Yazdani M, Rakkestad KE et al (2013) Prenatal exposure to bisphenol A interferes with the development of cerebellar granule neurons in mice and chicken. Int J Dev Neurosci 31(8):762–769. https://doi.org/10.1016/j.ijdevneu.2013.09.009
Meng L, Liu J, Wang C et al (2021) Sex-specific oxidative damage effects induced by BPA and its analogs on primary hippocampal neurons attenuated by EGCG. Chemosphere 264(Pt 1):128450. https://doi.org/10.1016/j.chemosphere.2020.128450
Michałowicz J (2014) Bisphenol A–sources, toxicity and biotransformation. Environ Toxicol Pharmacol 37(2):738–758. https://doi.org/10.1016/j.etap.2014.02.003
Minatoya M, Araki A, Nakajima S et al (2017) Cord blood BPA level and child neurodevelopment and behavioral problems: the Hokkaido Study on Environment and Children’s Health. Sci Total Environ 607–608:351–356. https://doi.org/10.1016/j.scitotenv.2017.06.060
Morris J, Bealer EJ, Souza IDS et al (2022) Chemical exposure-induced developmental neurotoxicity in head-regenerating Schmidtea mediterranea. Toxicol Sci 185(2):220–231. https://doi.org/10.1093/toxsci/kfab132
Moyano P, Flores A, García J et al (2021) Bisphenol A single and repeated treatment increases HDAC2, leading to cholinergic neurotransmission dysfunction and SN56 cholinergic apoptotic cell death through AChE variants overexpression and NGF/TrkA/P75(NTR) signaling disruption. Food Chem Toxicol 157:112614. https://doi.org/10.1016/j.fct.2021.112614
Mustieles V, Rodríguez-Carrillo A, Vela-Soria F et al (2022) BDNF as a potential mediator between childhood BPA exposure and behavioral function in adolescent boys from the INMA-Granada cohort. Sci Total Environ 803:150014. https://doi.org/10.1016/j.scitotenv.2021.150014
Myridakis A, Chalkiadaki G, Fotou M, Kogevinas M, Chatzi L, Stephanou EG (2016) Exposure of Preschool-Age Greek Children (RHEA Cohort) to Bisphenol A, Parabens, Phthalates, and Organophosphates. Environ Sci Technol 50(2):932–941. https://doi.org/10.1021/acs.est.5b03736
Naffaa V, Hochar I, Lama C et al (2022) Bisphenol A Impairs lipid remodeling accompanying cell differentiation in the oligodendroglial cell line oli-neu. Molecules 27(7):2274. https://doi.org/10.3390/molecules27072274
Nagao T, Kawachi K, Kagawa N, Komada M (2014) Neurobehavioral evaluation of mouse newborns exposed prenatally to low-dose bisphenol A. J Toxicol Sci 39(2):231–235. https://doi.org/10.2131/jts.39.231
Nguyen U, Tinsley B, Sen Y et al (2021) Exposure to bisphenol A differentially impacts neurodevelopment and behavior in Drosophila melanogaster from distinct genetic backgrounds. Neurotoxicology 82:146–157. https://doi.org/10.1016/j.neuro.2020.12.007
Ni Y, Hu L, Yang S et al (2021) Bisphenol A impairs cognitive function and 5-HT metabolism in adult male mice by modulating the microbiota-gut-brain axis. Chemosphere 282:130952. https://doi.org/10.1016/j.chemosphere.2021.130952
Nunez AA, Kannan K, Giesy JP, Fang J, Clemens LG (2001) Effects of bisphenol A on energy balance and accumulation in brown adipose tissue in rats. Chemosphere 42(8):917–922. https://doi.org/10.1016/s0045-6535(00)00196-x
Oliviero F, Marmugi A, Viguié C, Gayrard V, Picard-Hagen N, Mselli-Lakhal L (2022) Are BPA substitutes as obesogenic as BPA? Int J Mol Sci 23(8):4238. https://doi.org/10.3390/ijms23084238
Pan R, Wang C, Shi R et al (2019) Prenatal Bisphenol A exposure and early childhood neurodevelopment in Shandong. China Int J Hyg Environ Health 222(5):896–902. https://doi.org/10.1016/j.ijheh.2019.03.002
Pang W, Lian FZ, Leng X et al (2018) Microarray expression profiling and co-expression network analysis of circulating LncRNAs and mRNAs associated with neurotoxicity induced by BPA. Environ Sci Pollut Res Int 25(15):15006–15018. https://doi.org/10.1007/s11356-018-1678-y
Pang Q, Li Y, Meng L, Li G, Luo Z, Fan R (2019) Neurotoxicity of BPA, BPS, and BPB for the hippocampal cell line (HT-22): an implication for the replacement of BPA in plastics. Chemosphere 226:545–552. https://doi.org/10.1016/j.chemosphere.2019.03.177
Parks CG, Meier HCS, Jusko TA, Wilkerson J, Miller FW, Sandler DP (2022) Benzophenone-3 and antinuclear antibodies in U.S. adolescents and adults ages 12–39 years. Front Immunol 13:958527. https://doi.org/10.3389/fimmu.2022.958527
Perez-Lobato R, Mustieles V, Calvente I et al (2016) Exposure to bisphenol A and behavior in school-age children. Neurotoxicology 53:12–19. https://doi.org/10.1016/j.neuro.2015.12.001
Philippat C, Nakiwala D, Calafat AM et al (2017) Prenatal exposure to nonpersistent endocrine disruptors and behavior in boys at 3 and 5 years. Environ Health Perspect 125(9):097014. https://doi.org/10.1289/ehp1314
Pistollato F, de Gyves EM, Carpi D et al (2020) Assessment of developmental neurotoxicity induced by chemical mixtures using an adverse outcome pathway concept. Environ Health 19(1):23. https://doi.org/10.1186/s12940-020-00578-x
Pistollato F, Carpi D, Mendoza-de Gyves E et al (2021) Combining in vitro assays and mathematical modelling to study developmental neurotoxicity induced by chemical mixtures. Reprod Toxicol 105:101–119. https://doi.org/10.1016/j.reprotox.2021.08.007
Pradhan LK, Sahoo PK, Aparna S et al (2021) Suppression of bisphenol A-induced oxidative stress by taurine promotes neuroprotection and restores altered neurobehavioral response in zebrafish (Danio rerio). Environ Toxicol 36(11):2342–2353. https://doi.org/10.1002/tox.23348
Prasanth GK, Divya LM, Sadasivan C (2010) Bisphenol-A can bind to human glucocorticoid receptor as an agonist: an in silico study. J Appl Toxicol 30(8):769–774. https://doi.org/10.1002/jat.1570
Ramadan M, Cooper B, Posnack NG (2020) Bisphenols and phthalates: plastic chemical exposures can contribute to adverse cardiovascular health outcomes. Birth Defects Res 112(17):1362–1385. https://doi.org/10.1002/bdr2.1752
Rebuli ME, Camacho L, Adonay ME, Reif DM, Aylor DL, Patisaul HB (2015) Impact of Low-Dose Oral Exposure to Bisphenol A (BPA) on juvenile and adult rat exploratory and anxiety behavior: a CLARITY-BPA consortium study. Toxicol Sci 148(2):341–354. https://doi.org/10.1093/toxsci/kfv163
Repouskou A, Papadopoulou AK, Panagiotidou E et al (2020) Long term transcriptional and behavioral effects in mice developmentally exposed to a mixture of endocrine disruptors associated with delayed human neurodevelopment. Sci Rep 10(1):9367. https://doi.org/10.1038/s41598-020-66379-x
Rubin BS (2011) Bisphenol A: an endocrine disruptor with widespread exposure and multiple effects. J Steroid Biochem Mol Biol 127(1–2):27–34. https://doi.org/10.1016/j.jsbmb.2011.05.002
Sahoo PK, Pradhan LK, Aparna S, Agarwal K, Banerjee A, Das SK (2020) Quercetin abrogates bisphenol A induced altered neurobehavioral response and oxidative stress in zebrafish by modulating brain antioxidant defence system. Environ Toxicol Pharmacol 80:103483. https://doi.org/10.1016/j.etap.2020.103483
Sahoo PK, Aparna S, Naik PK, Singh SB, Das SK (2021) Bisphenol A exposure induces neurobehavioral deficits and neurodegeneration through induction of oxidative stress and activated caspase-3 expression in zebrafish brain. J Biochem Mol Toxicol 35(10):e22873. https://doi.org/10.1002/jbt.22873
Sam C, Li FF, Liu SL (2015) Inherited neurovascular diseases affecting cerebral blood vessels and smooth muscle. Metab Brain Dis 30(5):1105–1116. https://doi.org/10.1007/s11011-015-9668-y
Santoro A, Chianese R, Troisi J et al (2019) Neuro-toxic and reproductive effects of BPA. Curr Neuropharmacol 17(12):1109–1132. https://doi.org/10.2174/1570159x17666190726112101
Santoro A, Scafuro M, Troisi J et al (2021) Multi-systemic alterations by chronic exposure to a low dose of bisphenol A in drinking water: effects on inflammation and NAD(+)-dependent deacetylase Sirtuin1 in lactating and weaned rats. Int J Mol Sci 22(18):9666. https://doi.org/10.3390/ijms22189666
Santos JX, Rasga C, Marques AR et al (2022) A role for gene-environment interactions in autism spectrum disorder is supported by variants in genes regulating the effects of exposure to xenobiotics. Front Neurosci 16:862315. https://doi.org/10.3389/fnins.2022.862315
Sarikaya H, Ferro J, Arnold M (2015) Stroke prevention—medical and lifestyle measures. Eur Neurol 73(3–4):150–157. https://doi.org/10.1159/000367652
Sevastre-Berghian AC, Casandra C, Gheban D et al (2022) Neurotoxicity of bisphenol A and the impact of melatonin administration on oxidative stress, ERK/NF-kB signaling pathway, and behavior in rats. Neurotox Res 40(6):1882–1894. https://doi.org/10.1007/s12640-022-00618-z
Shin HM, Oh J, Kim K et al (2021) Variability of urinary concentrations of phenols, parabens, and triclocarban during pregnancy in first morning voids and pooled samples. Environ Sci Technol 55(23):16001–16010. https://doi.org/10.1021/acs.est.1c04140
Silano V, Bolognesi C, Castle L et al (2016) A statement on the developmental immunotoxicity of bisphenol A (BPA): answer to the question from the Dutch Ministry of Health. Welfare and Sport Efsa j 14(10):e04580. https://doi.org/10.2903/j.efsa.2016.4580
Sillapachaiyaporn C, Chuchawankul S, Nilkhet S et al (2022) Ergosterol isolated from cloud ear mushroom (Auricularia polytricha) attenuates bisphenol A-induced BV2 microglial cell inflammation. Food Res Int 157:111433. https://doi.org/10.1016/j.foodres.2022.111433
Singha SP, Memon S, Kazi SAF, Nizamani GS (2021) Gamma aminobutyric acid signaling disturbances and altered astrocytic morphology associated with Bisphenol A induced cognitive impairments in rat offspring. Birth Defects Res 113(12):911–924. https://doi.org/10.1002/bdr2.1886
Skarha J, Messerlian C, Bellinger D et al (2020) Parental preconception and prenatal urinary bisphenol A and paraben concentrations and child behavior. Environ Epidemiol 4(1):e082. https://doi.org/10.1097/ee9.0000000000000082
Song Y, Kwon B, Al-Abdulwahhab AH et al (2021) Rare neurovascular diseases in Korea: classification and related genetic variants. Korean J Radiol 22(8):1379–1396. https://doi.org/10.3348/kjr.2020.1171
Stacy SL, Papandonatos GD, Calafat AM et al (2017) Early life bisphenol A exposure and neurobehavior at 8years of age: Identifying windows of heightened vulnerability. Environ Int 107:258–265. https://doi.org/10.1016/j.envint.2017.07.021
Tan H, Wang X, Hong H et al (2020) Structures of endocrine-disrupting chemicals determine binding to and activation of the estrogen receptor α and androgen receptor. Environ Sci Technol 54(18):11424–11433. https://doi.org/10.1021/acs.est.0c02639
Tandon A, Singh SJ, Gupta M et al (2020) Notch pathway up-regulation via curcumin mitigates bisphenol-A (BPA) induced alterations in hippocampal oligodendrogenesis. J Hazard Mater 392:122052. https://doi.org/10.1016/j.jhazmat.2020.122052
Tang Y, Zhou W, Sun S et al (2020) Immunotoxicity and neurotoxicity of bisphenol A and microplastics alone or in combination to a bivalve species. Tegillarca Granosa Environ Pollut 265(Pt A):115115. https://doi.org/10.1016/j.envpol.2020.115115
Tanner EM, Hallerbäck MU, Wikström S et al (2020) Early prenatal exposure to suspected endocrine disruptor mixtures is associated with lower IQ at age seven. Environ Int 134:105185. https://doi.org/10.1016/j.envint.2019.105185
Tavakkoli A, Abnous K, Vahdati Hassani F, Hosseinzadeh H, Birner-Gruenberger R, Mehri S (2020) Alteration of protein profile in cerebral cortex of rats exposed to bisphenol a: a proteomics study. Neurotoxicology 78:1–10. https://doi.org/10.1016/j.neuro.2020.01.013
Thapar A, Cooper M, Rutter M (2017) Neurodevelopmental disorders. Lancet Psychiatry 4(4):339–346. https://doi.org/10.1016/s2215-0366(16)30376-5
Thayer KA, Doerge DR, Hunt D et al (2015) Pharmacokinetics of bisphenol A in humans following a single oral administration. Environ Int 83:107–115. https://doi.org/10.1016/j.envint.2015.06.008
Thayumanavan G, Jeyabalan S, Fuloria S et al (2022) Silibinin and Naringenin against bisphenol A-induced neurotoxicity in zebrafish model-potential flavonoid molecules for new drug design, development, and therapy for neurological disorders. Molecules 27(8):2572. https://doi.org/10.3390/molecules27082572
Tiwari SK, Agarwal S, Tripathi A, Chaturvedi RK (2016) Bisphenol-A mediated inhibition of hippocampal neurogenesis attenuated by curcumin via canonical wnt pathway. Mol Neurobiol 53(5):3010–3029. https://doi.org/10.1007/s12035-015-9197-z
Tsai CS, Chou WJ, Lee SY, Lee MJ, Chou MC, Wang LJ (2020) Phthalates, para-hydroxybenzoic acids, bisphenol-A, and gonadal hormones’ effects on susceptibility to attention-deficit/hyperactivity disorder. Toxics 8(3):10. https://doi.org/10.3390/toxics8030057
Usman A, Ahmad M (2016) From BPA to its analogues: is it a safe journey? Chemosphere 158:131–142. https://doi.org/10.1016/j.chemosphere.2016.05.070
van den Berg R (2003) Neurovascular diseases: from angiography to management. Eur J Radiol 46(3):169–171. https://doi.org/10.1016/s0720-048x(03)00088-3
Vandenberg LN (2014) Non-monotonic dose responses in studies of endocrine disrupting chemicals: bisphenol a as a case study. Dose Response 12(2):259–276. https://doi.org/10.2203/dose-response.13-020.Vandenberg
Vandenberg LN, Hauser R, Marcus M, Olea N, Welshons WV (2007) Human exposure to bisphenol A (BPA). Reprod Toxicol 24(2):139–177. https://doi.org/10.1016/j.reprotox.2007.07.010
Vandenberg LN, Chahoud I, Heindel JJ, Padmanabhan V, Paumgartten FJ, Schoenfelder G (2010) Urinary, circulating, and tissue biomonitoring studies indicate widespread exposure to bisphenol A. Environ Health Perspect 118(8):1055–1070. https://doi.org/10.1289/ehp.0901716
Viberg H, Lee I (2012) A single exposure to bisphenol A alters the levels of important neuroproteins in adult male and female mice. Neurotoxicology 33(5):1390–1395. https://doi.org/10.1016/j.neuro.2012.09.002
Viberg H, Fredriksson A, Buratovic S, Eriksson P (2011) Dose-dependent behavioral disturbances after a single neonatal Bisphenol A dose. Toxicology 290(2):187–194. https://doi.org/10.1016/j.tox.2011.09.006
Völkel W, Colnot T, Csanády GA, Filser JG, Dekant W (2002) Metabolism and kinetics of bisphenol a in humans at low doses following oral administration. Chem Res Toxicol 15(10):1281–1287. https://doi.org/10.1021/tx025548t
Wang Y, He Z, Deng S (2016) Ursolic acid reduces the metalloprotease/anti-metalloprotease imbalance in cerebral ischemia and reperfusion injury. Drug Des Devel Ther 10:1663–1674. https://doi.org/10.2147/dddt.S103829
Wang T, Xie C, Yu P et al (2017) Involvement of insulin signaling disturbances in bisphenol A-induced Alzheimer’s disease-like neurotoxicity. Sci Rep 7(1):7497. https://doi.org/10.1038/s41598-017-07544-7
Wang H, Chang L, Aguilar JS, Dong S, Hong Y (2019a) Bisphenol-A exposure induced neurotoxicity in glutamatergic neurons derived from human embryonic stem cells. Environ Int 127:324–332. https://doi.org/10.1016/j.envint.2019.01.059
Wang H, Zhao P, Huang Q, Chi Y, Dong S, Fan J (2019b) Bisphenol-A induces neurodegeneration through disturbance of intracellular calcium homeostasis in human embryonic stem cells-derived cortical neurons. Chemosphere 229:618–630. https://doi.org/10.1016/j.chemosphere.2019.04.099
Wang Q, Lin F, He Q et al (2019c) Assessment of the effects of Bisphenol A on dopamine synthesis and blood vessels in the goldfish brain. Int J Mol Sci 20(24):6206. https://doi.org/10.3390/ijms20246206
Wang C, He J, Xu T et al (2021) Bisphenol A(BPA), BPS and BPB-induced oxidative stress and apoptosis mediated by mitochondria in human neuroblastoma cell lines. Ecotoxicol Environ Saf 207:111299. https://doi.org/10.1016/j.ecoenv.2020.111299
Wang C, Wang L, Huang C et al (2022a) Involvement of NLRP3/Caspase-1/GSDMD-Dependent pyroptosis in BPA-induced apoptosis of human neuroblastoma cells. Biochem Pharmacol 200:115042. https://doi.org/10.1016/j.bcp.2022.115042
Wang LJ, Huang YH, Chou WJ et al (2022b) Interrelationships among growth hormone, thyroid function, and endocrine-disrupting chemicals on the susceptibility to attention-deficit/hyperactivity disorder. Eur Child Adolesc Psychiatry 32:1391–1401. https://doi.org/10.1007/s00787-021-01886-4
Welch C, Johnson E, Tupikova A et al (2022) Bisphenol a affects neurodevelopmental gene expression, cognitive function, and neuromuscular synaptic morphology in Drosophila melanogaster. Neurotoxicology 89:67–78. https://doi.org/10.1016/j.neuro.2022.01.006
Wolkowicz IR, Herkovits J, Pérez Coll CS (2014) Stage-dependent toxicity of bisphenol a on Rhinella arenarum (anura, bufonidae) embryos and larvae. Environ Toxicol 29(2):146–154. https://doi.org/10.1002/tox.20781
Wu X, Majumder A, Webb R, Stice SL (2016) High content imaging quantification of multiple in vitro human neurogenesis events after neurotoxin exposure. BMC Pharmacol Toxicol 17(1):62. https://doi.org/10.1186/s40360-016-0107-4
Wu XJ, Sun XH, Wang SW, Chen JL, Bi YH, Jiang DX (2018) Mifepristone alleviates cerebral ischemia-reperfusion injury in rats by stimulating PPAR γ. Eur Rev Med Pharmacol Sci 22(17):5688–5696. https://doi.org/10.26355/eurrev_201809_15836
Wu CC, Shields JN, Akemann C et al (2021) The phenotypic and transcriptomic effects of developmental exposure to nanomolar levels of estrone and bisphenol A in zebrafish. Sci Total Environ 757:143736. https://doi.org/10.1016/j.scitotenv.2020.143736
Xing J, Zhang S, Zhang M, Hou J (2022) A critical review of presence, removal and potential impacts of endocrine disruptors bisphenol A. Comp Biochem Physiol C Toxicol Pharmacol 254:109275. https://doi.org/10.1016/j.cbpc.2022.109275
Xue J, Zhang L, Xie X et al (2020) Prenatal bisphenol A exposure contributes to Tau pathology: Potential roles of CDK5/GSK3β/PP2A axis in BPA-induced neurotoxicity. Toxicology 438:152442. https://doi.org/10.1016/j.tox.2020.152442
Yang G, Yang L, Liu Q et al (2023) Protective effects of cyanidin-3-O-glucoside on BPA-induced neurodevelopmental toxicity in zebrafish embryo model. Comp Biochem Physiol C Toxicol Pharmacol 264:109525. https://doi.org/10.1016/j.cbpc.2022.109525
Yao Y, Tsirka SE (2014) Monocyte chemoattractant protein-1 and the blood-brain barrier. Cell Mol Life Sci 71(4):683–697. https://doi.org/10.1007/s00018-013-1459-1
Ye X, Kuklenyik Z, Needham LL, Calafat AM (2006) Measuring environmental phenols and chlorinated organic chemicals in breast milk using automated on-line column-switching-high performance liquid chromatography-isotope dilution tandem mass spectrometry. J Chromatogr B Analyt Technol Biomed Life Sci 831(1–2):110–115. https://doi.org/10.1016/j.jchromb.2005.11.050
Yin N, Yao X, Qin Z, Wang YL, Faiola F (2015) Assessment of Bisphenol A (BPA) neurotoxicity in vitro with mouse embryonic stem cells. J Environ Sci (china) 36:181–187. https://doi.org/10.1016/j.jes.2015.06.004
Yin Z, Hua L, Chen L et al (2020) Bisphenol-A exposure induced neurotoxicity and associated with synapse and cytoskeleton in Neuro-2a cells. Toxicol in Vitro 67:104911. https://doi.org/10.1016/j.tiv.2020.104911
Yirun A, Ozkemahli G, Balci A et al (2021) Neuroendocrine disruption by bisphenol A and/or di(2-ethylhexyl) phthalate after prenatal, early postnatal and lactational exposure. Environ Sci Pollut Res Int 28(21):26961–26974. https://doi.org/10.1007/s11356-021-12408-9
Yolton K, Xu Y, Strauss D, Altaye M, Calafat AM, Khoury J (2011) Prenatal exposure to bisphenol A and phthalates and infant neurobehavior. Neurotoxicol Teratol 33(5):558–566. https://doi.org/10.1016/j.ntt.2011.08.003
Zhang H, Kuang H, Luo Y et al (2019) Low-dose bisphenol A exposure impairs learning and memory ability with alterations of neuromorphology and neurotransmitters in rats. Sci Total Environ 697:134036. https://doi.org/10.1016/j.scitotenv.2019.134036
Zhang H, Wang Z, Meng L et al (2020) Maternal exposure to environmental bisphenol A impairs the neurons in hippocampus across generations. Toxicology 432:152393. https://doi.org/10.1016/j.tox.2020.152393
Zhang K, Liang J, Brun NR, Zhao Y, Werdich AA (2021a) Rapid zebrafish behavioral profiling assay accelerates the identification of environmental neurodevelopmental toxicants. Environ Sci Technol 55(3):1919–1929. https://doi.org/10.1021/acs.est.0c06949
Zhang Y, Li S, Wu J et al (2021b) The orphan nuclear receptor Nur77 plays a vital role in BPA-induced PC12 cell apoptosis. Ecotoxicol Environ Saf 213:112026. https://doi.org/10.1016/j.ecoenv.2021.112026
Zhang Q, He Y, Cheng R, Li Q, Qian Z, Lin X (2022a) Recent advances in toxicological research and potential health impact of microplastics and nanoplastics in vivo. Environ Sci Pollut Res Int 29(27):40415–40448. https://doi.org/10.1007/s11356-022-19745-3
Zhang Z, Wang H, Lei X, Mehdi Ommati M, Tang Z, Yuan J (2022b) Bisphenol a exposure decreases learning ability through the suppression of mitochondrial oxidative phosphorylation in the hippocampus of male mice. Food Chem Toxicol 165:113167. https://doi.org/10.1016/j.fct.2022.113167
Zhang B, Wang S, Tang Y et al (2023) Direct inhibition of bisphenols on human and rat 11β-hydroxysteroid dehydrogenase 2: Structure-activity relationship and docking analysis. Ecotoxicol Environ Saf 254:114715. https://doi.org/10.1016/j.ecoenv.2023.114715
Zheng J, Reynolds JE, Long M et al (2022) The effects of prenatal bisphenol A exposure on brain volume of children and young mice. Environ Res 214(Pt 3):114040. https://doi.org/10.1016/j.envres.2022.114040
Zhou Y, Wang Z, Xia M et al (2017) Neurotoxicity of low bisphenol A (BPA) exposure for young male mice: Implications for children exposed to environmental levels of BPA. Environ Pollut 229:40–48. https://doi.org/10.1016/j.envpol.2017.05.043
Funding
Open access funding provided by FCT|FCCN (b-on). This work was supported by the Foundation for Science and Technology (FCT), through funds from the State Budget, and by the European Regional Development Fund (ERDF), under the Portugal 2020 Program, through the Regional Operational Program of the Center (Centro2020), through the Projects with the references (UIDB/00709/2020 + UIDP/00709/2020).
Author information
Authors and Affiliations
Contributions
HEC: investigation; writing—original draft; writing—review and editing. EC: conceptualization; validation; funding acquisition; project administration; supervision; writing—review and editing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Conflict of interest
The authors have no relevant financial or non-financial interests to disclose.
Ethics approval
This is a review article. There is not ethical approval applicable.
Consent to participate
Not applicated.
Consent to publish
This is a review article. There is no consent to publish applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Costa, H.E., Cairrao, E. Effect of bisphenol A on the neurological system: a review update. Arch Toxicol 98, 1–73 (2024). https://doi.org/10.1007/s00204-023-03614-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00204-023-03614-0