Abstract
Summary
We estimated the short-term impact of fragility fractures on community-dwelling women in five countries. Women with fragility fractures reported significantly more difficulties performing activities of daily living and significantly higher levels of lost productivity and caregiver support than those without fractures; results highlight the multi-country indirect burden of fragility fractures.
Introduction
To estimate the impact of fragility fractures on activities of daily living (ADL), productivity loss and caregiver support in women with a recent fragility fracture.
Methods
This multi-centre cross-sectional study enrolled community-dwelling women aged ≥ 50 years in South Korea, Spain, Germany, Australia and the United States. The fragility fracture cohort consisted of women with an index fragility fracture in the past 12 months; the fracture free cohort consisted of women with no fracture in the 18 months prior to study enrolment. Study participants completed three validated questionnaires: Lawton Instrumental ADL (IADL), Physical Self-Maintenance Scale (PSMS) and iMTA Productivity Cost Questionnaire (iPCQ).
Results
In total, 1,253 participants from 41 sites across the five countries were included. Compared with the fracture free cohorts, fragility fracture cohorts had significantly lower function and were more dependent on support (p < 0.05 in all countries for Lawton IADL, and in South Korea, Spain, Australia and the United States for PSMS), significantly higher hours of paid absenteeism (p < 0.05, Spain, Germany, Australia), significantly higher unpaid lost productivity (p < 0.05, South Korea, Spain, Germany), significantly more days of paid help received in the home (p < 0.05 South Korea, Spain and the United States), and significantly more days of unpaid help from family members or friends (p < 0.05, all countries).
Conclusion
In this multi-national study, fragility fractures in community-dwelling ≥ 50 years women were associated with several outcomes indicating higher indirect burden and lower quality of life, including more difficulties performing ADL and higher levels of lost productivity and caregiver support.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Fragility fractures are associated with a significant healthcare and financial burden in both formal and informal care settings, in addition to a lower quality of life and increased mortality [1, 2]. However, most studies assessing the burden of fragility fractures have focused on the direct costs, such as those associated with acute and rehabilitative care following a fracture. In 2019, the total direct cost of osteoporotic fractures across the 27 member states of the European Union, together with the UK and Switzerland, amounted to €56.9 billion [3].
International studies on the indirect burden of fragility fractures – for example, reduced functional ability, loss of paid working hours and increase in paid assistance – are more limited and have assessed only health-related quality of life (HRQoL) outcomes, or the burden of disability-adjusted life years [4, 5]. To date, there have been no international studies that include an assessment of physical functioning, such as activities of daily living (ADL) which evaluate fundamental skills required to independently care for oneself, such as eating, bathing and mobility [6].
In this study we aimed to assess the short-term (up to a year after index fracture) indirect burden of fragility fractures in community dwelling women aged 50 years or older, using three validated questionnaires (Lawton Instrumental ADL [IADL]; Physical Self-Maintenance Scale [PSMS]; Institute for Medical Technology Assessment Productivity Cost Questionnaire [iPCQ]) [7,8,9,10]. Responses to these questionnaires can highlight the impact of fragility fractures on a participant’s physical function, productivity, need of caregivers and use of rehabilitation services. Considering the burden of fragility fractures to both patients and society, data may inform policy makers, clinicians and patients about the multi-country indirect burden of fragility fractures in women. Results could also emphasise the importance of restoring loss of physical functional ability due to fractures.
Methods
Study design and population
We performed a multi-national, cross-sectional, observational study to assess the indirect burden of fragility fractures in women aged 50 years or older. The study population comprised a convenience sample of participants residing in Australia, Germany, South Korea, Spain and the USA who were willing and able to independently complete the one-time paper-and-pen survey and included two cohorts: those who had experienced a recent fragility fracture and those had not.
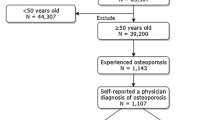
Women in the fragility fracture cohort had experienced a single fracture (i.e. a single fracture event leading to single or multiple fractures in one location) during the 12 months prior to study participation and no fracture in the 18 months prior to the index fracture; women in the fracture free cohort were free of fracture in the 18 months prior to study participation (Fig. 1). As the aim of this analysis was to assess the indirect burden of fragility fractures, rather than osteoporosis, an osteoporosis diagnosis (or use of osteoporosis medication) was not an exclusion criterion for either cohort. Participants were recruited between July 2020 and October 2021 by clinical sites. Full methods for the selection of recruitment sites and patient recruitment are described in Supplementary Appendix A. Briefly, recruitment sites were selected based on the site’s expected ability to recruit women meeting the inclusion criteria within the study timeframe and aimed to be representative of geographies, settings of care (i.e. primary versus secondary) and physician specialty. Participating clinical sites were responsible for obtaining consent from and enrolling participants on the day of a regular care visit, with eligibility criteria confirmed by the clinical staff using patient medical record data. No formal matching was performed, but recruitment for the fragility fracture cohort aimed to achieve a balanced distribution of fracture sites and number of months since index fracture (between 0 to ≤ 3 months, > 3 months to ≤ 6 months, > 6 months to ≤ 9 months, and > 9 months to ≤ 12 months).
The recruitment target for each country was 300 participants (150 in the fragility fracture cohort, 150 in the fracture free cohort), giving a total target sample size of 1,500 participants. The study design and full inclusion and exclusion criteria are described in Supplementary Appendix B and depicted in Fig. 1.
Data are presented at the country level with a focus on the comparison between the fragility fracture and fracture free cohorts; the short term (up to 12 months following the index fracture) indirect burden of fragility fractures was assessed by differences between these cohorts in each country.
Data collection
A short electronic case report form (eCRF) was completed by clinical staff for each participant, collecting data used to verify patient eligibility and describe osteoporosis diagnoses, comorbidities, menopause status, treatment history, and fracture data. Information about current physical functioning, use of rehabilitation services and informal care, and components of indirect cost including work and productivity losses were collected using a one-time patient survey, the key outcomes of which are highlighted as follows:
Physical functional ability
Physical functional ability was assessed using the self-rated versions of the Lawton Instrumental Activities of Daily Living (IADL) and the Physical Self-Maintenance Scale (PSMS). IADL are activities that are needed to live independently (e.g., doing housework, preparing meals, taking medications properly, managing finances, using a telephone). Scores were calculated as described in the Lawton IADL manual [9, 10]. Briefly, each item was rated on a trichotomous scale (1 = unable, 2 = needs assistance, 3 = independent) and all responses were summed. Total scores range from 10 to 29, with a higher score reflecting a greater level of physical functional ability; the minimal important change in IADL score has been shown to be approximately 0.5 points [11].
The PSMS consists of eight questions relating to performance of fundamental ADL (i.e. feeding, dressing, grooming, bathing, toileting, ambulating). Scores were calculated as described in the PSMS manual [7]. Briefly, each item was rated on a trichotomous scale (1 = unable, 2 = needs assistance, 3 = independent) and the eight responses summed. Total scores range from 8 to 24, with a higher score reflecting a greater level of physical functional ability.
Work and productivity
Components of indirect costs – including work (both paid and unpaid) and productivity loss – were assessed using the iMTA Productivity Cost Questionnaire (iPCQ) [8]. The questionnaire comprises 18 questions, nine of which relate to demographic information, such as age, sex and work status (e.g. number of paid working hours per week). The remaining questions quantify productivity loss across three domains: lost productivity from paid work due to absenteeism (absence from work), lost productivity from paid work due to presenteeism (reduced productivity while at work) and lost productivity from unpaid work [9]. The iPCQ has a recall period of four weeks and is structured to allow respondents to easily skip questions that are not applicable to them. Absenteeism questions are also structured in a way that allows the length of individual absenteeism periods to be specified. Productivity cost estimates were valuated using the friction cost method – productivity losses were therefore assumed to be restored after the period required to replace an absent worker (i.e. the “friction period”) [9].
Rehabilitation and informal care
Collected data included participant self-reported use of short-term care or rehabilitation facilities, durable medical equipment (e.g. wheelchair, walker or cane) and use of both paid and informal care (from family or friends) in the 30 days prior to survey completion.
Statistical analysis
Descriptive analyses were conducted to describe patient characteristics and outcomes in both the fragility fracture and fracture free cohorts. To address the potential confounding of the comparison of outcomes between these cohorts, an inverse probability of treatment weight (IPTW) was constructed within each country. Each IPTW was calculated based on the propensity score taken from a logistic regression that included at least five of the following potential confounding variables: age, ethnicity, glucocorticoid use, hormone replacement therapy use, anti-osteoporosis medication use, osteoporosis diagnosis and comorbidities (including cardiac disease, chronic obstructive pulmonary disease, asthma, diabetes and depression and anxiety). Sample sizes (within each country) did not always allow for all confounding variables to be included, with some excluded due to very low occurrences and others excluded to ensure at least 10 participants per covariate (iteratively removing variables with the highest p-value). Confounding variables were considered balanced if their weighted standardised mean differences (SMD) between the fragility fracture and fracture free cohorts were < 0.1.
Weighted means and standard deviations are reported, with comparisons made using weighted univariate regressions that only included the fracture status cohort variable from which the p-value was taken. A p-value < 0.05 was considered statistically significant.
Missing data
To increase response rates to each of the questions, the survey was designed to be completed within the physician’s office and in minimal time. The eCRF was also designed to identify skipped or missing data elements in real-time to minimise missing data. Any missing data were documented as number and percentage and presented as a separate category; methods for dealing with missing data such as multiple imputation or last observation carried forward were not applied.
Results
In total, 1,253 participants were recruited from across 41 clinical sites (nine in South Korea and Australia, eight each in Spain and the USA and seven in Germany). Clinical sites included hospitals, university hospitals, clinics (orthopaedic, or specialty such as endocrinologist, rheumatologist), solo practices and primary care centres. Baseline characteristics of participants in each country are given in Table 1. The proportion of participants with an osteoporosis diagnosis at the time of the survey varied between countries, from 26.2% (Spain) to 80.7% (Germany) in the fracture free cohort and from 51.0% (Spain) to 93.8% (Germany) in the fragility fracture cohort. Similarly, the proportions of patients prescribed anti-osteoporosis medications in the 12 months prior to completing the survey ranged from 22% (Spain) to 64% (Germany) in the fracture free cohort and from 46% (Spain) to 76% (USA) in the fragility fracture cohort; full anti-osteoporosis medication treatment history is provided in Supplementary Appendix C.
In the fragility fracture cohort, the most common index fractures in South Korea, Germany and the USA were vertebral fractures, accounting for 60%, 63% and 35% of fractures, respectively. In Spain and Australia, the most common index fractures were fractures of the upper body (including the radius, ulna, humerus, ribs, clavicle and scapula), accounting for 48% and 43% of fractures in each country. Potential confounding factors were balanced between the fracture free and fragility fracture cohorts, based on key characteristics (Supplementary Appendix D), except for the USA, where the largest weighted standardised mean difference was 0.22.
Physical functional ability
Lawton IADL scores in the fragility fracture cohort were significantly lower in all countries when compared with the fracture free cohort (South Korea: 24.3 fragility fracture cohort versus 26.6 fracture free cohort; Germany: 24.8 versus 26.6; Spain: 23.6 versus; Australia: 24.8 versus 26.4; USA: 24.6 versus 26.2, all p < 0.01; Fig. 2). When responding to questions pertaining to their ability to perform everyday activities, a numerically higher proportion of the fracture free cohort answered that they were able to perform tasks “without help” than the fragility fracture cohort for most questions. Of note were the responses to the question “Can you go shopping for groceries?” where more participants in the fracture free cohort answered “without help” compared with participants in the fragility fracture cohort (South Korea: 91% fracture free cohort versus 63% fragility fracture cohort; Germany: 86% versus 69%; Spain: 67% versus 47%; Australia: 86% versus 66%; USA: 85% versus 61%).
Physical functional ability: mean Lawton IADL and PSMS scores by country. Full study population (N = 1,253). Weighted means and standard deviations shown. Lawton IADL scores range from 10–29 and PSMS from 8–24; higher scores represent better physical functional ability. Differences between fragility fracture and fracture free cohorts were assessed using inverse probability weighted regression adjustment. *p < 0.05, †p < 0.001. IADL: instrumental activities of daily living; SD: standard deviation; PSMS: physical self-maintenance score
In the PSMS survey, scores were significantly lower in the fragility fracture cohorts in South Korea, Spain, Australia and the USA when compared with the fracture free cohort (South Korea: 22.5 fragility fracture cohort versus 23.4 fracture free cohort; Spain: 22.2 versus 22.8; Australia: 22.8 versus 23.3; USA: 22.2 versus 22.9, all p < 0.05; Fig. 2). A numerically greater proportion of the fracture free cohort indicated the ability to complete the highlighted tasks “without help” than the fragility fracture cohort; notably, more participants in the fracture free cohort reported being able to get around their house, apartment or room “without help of any kind except for a cane” compared to the fragility fracture cohort (South Korea: 96% fracture free cohort versus 78% fragility fracture cohort; Germany: 93% versus 83%; Spain: 87% versus 83%; Australia: 93% versus 84%; USA: 95% versus 80%).
Work and productivity
In all countries, a low proportion (11% to 32%) of participants in both cohorts were in paid employment (Table 2). Among those who were employed, the fragility fracture cohorts in Germany, Spain and Australia reported significantly greater paid absenteeism (absence from work) compared with the fracture free cohort; the fragility fracture cohorts in South Korea, Germany and Spain reported significantly greater unpaid productivity compared with the fracture free cohort.
Of those in paid employment, a greater proportion of the fragility fracture cohort reported missing work due to sickness in the four weeks prior to survey completion compared with the fracture free cohort (South Korea: 19% fragility fracture cohort versus 5% fracture free cohort; Germany: 41% versus 18%; Spain: 65% versus 45%; Australia: 50% versus 15%; USA: 25% versus 8%). The fragility fracture cohort also reported greater lost productivity related to unpaid work (Table 2).
Rehabilitation and informal care
The use of rehabilitation facilities in the 30 days prior to survey administration was low across all countries. In all countries, the fragility fracture cohort received a greater number of hours of unpaid help at home over the 30 days prior to survey completion compared to paid help (Table 3). Additionally, fragility fracture cohorts received a significantly greater number of days of unpaid help compared with the fracture free cohorts (South Korea: 4.8 days fragility fracture cohort versus 1.5 days fracture free cohort; Germany: 8.0 versus 2.5 days; Spain: 10.1 versus 5.2 days; Australia: 6.4 versus 3.0 days; USA: 5.1 versus 1.3 days, all p < 0.05). Furthermore, in South Korea, Spain and the USA, the fragility fracture cohort received more days of paid help at home compared with the fracture free cohort (South Korea: 1.3 days fragility fracture cohort versus 0.0 days fracture free cohort; Spain: 1.6 versus 0.4 days; USA: 2.3 versus 0.6 days).
Discussion
We have estimated the short-term (up to 12 months post-fracture) impact of fragility fractures on physical functional ability, productivity, use of rehabilitation services and informal care in community-dwelling women aged 50 years or older residing in South Korea, Germany, Spain, Australia and the USA. Participants in the fragility fracture cohort reported lower levels of physical functional ability and higher levels of absenteeism, presenteeism, lost productivity and caregiver support compared with those in the fracture free cohort.
The reduced physical functional ability of women in the fragility fracture cohort (compared with the fracture free cohort) was indicated by the significant between-cohort differences in IADL and PSMS scores. Differences in Lawton IADL scores between the fragility fracture and fracture free cohorts ranged from 1.3 to 2.3 across countries; these differences are greater than the validated minimal important change of approximately 0.5 and are similar to those previously reported six months post hip fracture in older adults [11, 12]. IADL and PSMS scores assess activities that are needed to live independently (e.g., doing housework, preparing meals, taking medications, managing finances or using a telephone); deficits in these scores can, therefore, signal the need for additional assistance.
The link between fragility fractures and workplace productivity has been documented in previous country-specific studies [13,14,15]. However, in this study, we did not perform the calculations to further quantify productivity loss in monetary terms – as our study was multi-country, the cost of lost productivity due to fragility fractures would likely differ across the included countries due to differences in wages, labour market conditions and healthcare systems. Presenting the results in monetary terms would therefore have required additional data and calculations to account for these differences, which were outside of the scope of this study. We chose to assess productivity loss using the friction cost method as it has been shown to provide a more accurate estimate of the productivity costs in the short term compared to other commonly used methods such as the human capital method [16]. This is because the friction cost method considers the expenses and time required to recruit and train a replacement worker, thereby generating a more moderate short term estimation. Using the friction cost method, significantly lower productivity (both in terms of paid and unpaid work) was reported by participants in the fragility fracture cohort compared with the fracture free cohort.
Furthermore, paid absenteeism and presenteeism were only reported by those in paid employment; in this group, participants in the fragility fracture cohort reported significantly greater paid absenteeism during the 28 days prior to survey completion compared with the fracture free cohort. It should be noted, however, that both cohorts had low levels of paid employment (< 32%) – with a mean age of around 70 years, this was not unexpected as many participants were retired. The impact of fragility fractures on unpaid productivity is therefore perhaps more relevant; indeed, in all countries except Spain, almost double the proportion of women in the fragility fracture cohort reported doing less unpaid work compared with those in the fracture free cohort (data not shown). As the impacts of a fragility fracture on productivity in unpaid employment were not captured, it is likely that the true impacts of fragility fractures were underestimated in this regard.This study also demonstrates that the burden, both in formal (e.g., paid for) and informal (e.g., care provided by family and friends) care in the community setting, was higher for the fragility fracture cohorts than the fracture free cohorts. Across all countries, participants in the fragility fracture cohorts received more hours of unpaid help than paid help over the 30 days prior to survey completion. With growing evidence documenting the economic impact of unpaid caregivers, fragility fractures could therefore present a significant informal care burden for society [17].
Both fragility fracture and fracture free cohorts reported a limited use of rehabilitation and long-term care facilities in the 30 days prior to study participation, likely due to exclusion of participants who were currently institutionalised (e.g., in hospital, nursing home, assisted living or other care facility). These participants were excluded as their incremental burden of a fragility fracture can be expected to be different to those experiencing a fragility fracture while residing in the community, as such participants are likely to have limitation of IADLs and productivity due to the support that is provided in these institutions, irrespective of fracture status. This requirement for participants not to be receiving institutional care provides a further potential underestimate of the burden of fragility fractures since it excludes those participants who are institutionalised for a period because of their fracture.
It is important to note that this study was cross-sectional in nature and intended to assess the burden during the 12 months following the index fragility fracture. Participants at varying periods post-fracture were included to allow assessment at different time points. Within the sample, some participants in the fragility fracture cohorts had therefore experienced their fracture more recently than others and were at different stages in their recovery. This study does therefore not address the cumulative burden over a 12-month period for participants who experience a single fragility fracture but instead assessed the average burden.
There are also challenges associated with assessing the burden associated with fragility fractures in terms of identifying an appropriate non-fracture population. This study included participants who had no fracture in the preceding 18 months, who were of a similar age and presented to healthcare providers at the same sites as participants with fragility fractures. The IPTW technique was employed to adjust for key confounding factors including comorbidities, and in all countries except the US it was possible to achieve a balanced sample to address this challenge.For inclusion in the fragility fracture cohort, participants needed to have experienced a single fracture within the observation window. While this approach allowed assessment of the impact of such an event with greater certainty, it is also likely to underestimate the burden associated with fragility fractures as a proportion of participants may go on to have a further fracture within a year of the index fracture [18, 19].
A further limitation of this study was the requirement for patients to be able to independently fill out the survey, which may have biased the study population towards healthier patients. Recruitment through clinical sites could have been a further source of selection bias, increasing the likelihood of patients frequently utilising healthcare services or with comorbid conditions being recruited. This, combined with the older average age (approximately 70 years) of the fragility fracture cohort, may explain the higher proportions of the fracture free cohort receiving osteoporosis medication when compared to the general population [20,21,22].
Participants were recruited during the COVID-19 pandemic, when there were limitations on social interaction and movement outside of the home. This could have had several important effects, including effects on productivity, the performance of some activities of daily living, and may have made provision of both formal and informal care challenging. However, this would have been equally true irrespective of fragility fracture status and so is unlikely to have impacted comparisons between the groups. The impacts of COVID-19 may also have biased the study population to those less healthy (i.e. those who could not wait to seek medical attention). This may have been more relevant for the non-fracture group, introducing a bias towards inclusion of non-fracture participants with more serious health conditions, with possible consequent reduced productivity and IADLs in the non-fracture group than might have been observed outside of the pandemic. This, in turn, might have led to a conservative estimate of differences between the fracture and non-fracture groups.It is difficult to draw definite conclusions from any differences in responses between countries, given the range of healthcare systems and variety of approaches to clinical care, reimbursement and policy. The key message, however, that the fragility fracture cohort represented a greater indirect healthcare burden when compared with the fracture free cohort was consistent across all countries included in the study (Australia, Germany, Spain, South Korea and the United States). Country-specific results may be used to shape policy within the individual countries included in this study; more widely, data could inform policy makers, clinicians and patients about the multi-country indirect burden of fragility fractures in women.
In conclusion, community-dwelling women aged 50 years or older in the fragility fracture cohort reported significantly more difficulties performing ADL in addition to significantly higher levels of lost productivity and caregiver support than women in the fracture free cohort.
References
Becker DJ, Kilgore ML, Morrisey MA (2010) The Societal Burden of Osteoporosis. Curr Rheumatol Rep 12(3):186–191
Kanis JA et al (2001) The burden of osteoporotic fractures: a method for setting intervention thresholds. Osteoporos Int 12(5):417–427
Kanis JA et al (2021) SCOPE 2021: a new scorecard for osteoporosis in Europe. Arch Osteoporos 16(1):82
Shen Y et al (2022) The global burden of osteoporosis, low bone mass, and its related fracture in 204 countries and territories, 1990–2019. Front Endocrinol (Lausanne) 13:882241
Svedbom A et al (2018) Quality of life after hip, vertebral, and distal forearm fragility fractures measured using the EQ-5D-3L, EQ-VAS, and time-trade-off: results from the ICUROS. Qual Life Res 27(3):707–716
Edemekong PF et al (2022) Activities of daily living. In: StatPearls. StatPearls Publishing Copyright © 2022, StatPearls Publishing LLC., Treasure Island
(1988) Physical Self-Maintenance Scale (PSMS). Self-rated version. Incorporated in the Philadelphia Geriatric Center. Multilevel Assessment Instrument (MAI). Psychopharmacol Bull 24(4):795–797
iMTA Productivity and Health Research Group (2021) iMTA productivity cost questionnaire. Available from: https://www.imta.nl/questionnaires/imcq/publications/. Accessed 5 July 2021
Bouwmans C et al (2015) The iMTA Productivity Cost Questionnaire: A Standardized Instrument for Measuring and Valuing Health-Related Productivity Losses. Value Health 18(6):753–758
Lawton MP, Brody EM (1969) Assessment of older people: self-maintaining and instrumental activities of daily living1. Gerontol 9(3_Part_1):179–186
Suijker JJ et al (2017) Minimal important change and minimal detectable change in activities of daily living in community-living older people. J Nutr Health Aging 21(2):165–172
Segev-Jacubovski O, Magen H, Maeir A (2019) Functional ability, participation, and health-related quality of life after hip fracture. OTJR (Thorofare N J) 39(1):41–47
Tran O et al (2021) Long-term direct and indirect economic burden associated with osteoporotic fracture in US postmenopausal women. Osteoporos Int 32(6):1195–1205
Fujiwara S et al (2019) Disease burden of fractures among patients with osteoporosis in Japan: health-related quality of life, work productivity and activity impairment, healthcare resource utilization, and economic costs. J Bone Miner Metab 37(2):307–318
Hansen L et al (2013) A health economic analysis of osteoporotic fractures: who carries the burden? Arch Osteoporos 8(1):126
Pike J, Grosse SD (2018) Friction cost estimates of productivity costs in cost-of-illness studies in comparison with human capital estimates: a review. Appl Health Econ Health Policy 16(6):765–778
Jacobs JC et al (2019) Economic spillover effects of intensive unpaid caregiving. Pharmacoeconomics 37(4):553–562
Johansson H et al (2017) Imminent risk of fracture after fracture. Osteoporos Int 28(3):775–780
Kanis JA et al (2018) Characteristics of recurrent fractures. Osteoporos Int 29(8):1747–1757
Choi YJ et al (2021) Temporal change in the diagnosis and treatment rates of osteoporosis: results from the Korea National Health and Nutrition Examination Survey. Osteoporos Int 32(9):1777–1784
Hadji P et al (2020) Estimated epidemiology of osteoporosis diagnoses and osteoporosis-related high fracture risk in Germany: a German claims data analysis. Arch Osteoporos 15(1):127
Practitioners RACoG (2017) Osteoporosis prevention, diagnosis and management in postmenopausal women and men over 50 years of age. [cited 2023 24 April]. https://www.racgp.org.au/clinical-resources/clinical-guidelines/key-racgp-guidelines/view-all-racgp-guidelines/osteoporosis
Acknowledgements
The authors thank the participants, the investigators and their teams who took part in this study. The authors also acknowledge Will Cherry, BSc, Costello Medical, UK for publication coordination, and Jane Spingardi, DPhil, from Costello Medical, UK for medical writing and editorial assistance based on the authors’ input and direction. This study was funded by UCB Pharma and Amgen Inc.
Funding
This study was sponsored by UCB Pharma and Amgen Inc and conducted by Adelphi Real World. Support for third-party writing assistance for this article, provided by Jane Spingardi, DPhil, Costello Medical, UK, was funded by UCB Pharma in accordance with Good Publication Practice (GPP3) guidelines (http://www.ismpp.org/gpp3).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Consent for publication
All the results presented in this article are in aggregate form, and no personally identifiable information was used for this study.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Conflicts of interest
Eric Yeh is an employee of Amgen and holds Amgen stock. Olivera Rajkovic-Hooley, Mark Silvey, Will S Ambler and Gary Milligan are employees of Adelphi Real World, which received payment from UCB Pharma and Amgen Inc as part of this research. Rafael Pinedo-Villanueva has received research funding from Amgen, Fondation privée des HUG (Geneva, Switzerland), the International Osteoporosis Foundation, Kyowa Kirin Services, the Royal Osteoporosis Society, and the UK NIHR in addition to lecture fees and/or consulting honoraria from Amgen, Astellas, the International Osteoporosis Foundation, Mereo Biopharma, and UCB Pharma. Nicholas C Harvey has received honoraria, personal, consultancy and lecture fees from Alliance for Better Bone Health, AMGEN, Consilient Healthcare, Eli Lilly, Internis Pharma, Kyowa Kirin, MSD, Servier, Shire, and UCB Pharma. Alireza Moayyeri is an employee and stockholder of UCB Pharma.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Yeh, E.J., Rajkovic-Hooley, O., Silvey, M. et al. Impact of fragility fractures on activities of daily living and productivity in community-dwelling women: a multi-national study. Osteoporos Int 34, 1751–1762 (2023). https://doi.org/10.1007/s00198-023-06822-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-023-06822-7