Abstract
Summary
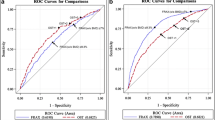
This very large dual X-ray absorptiometry (DXA) cohort confirmed a significant, inverse relationship between bone mineral density (BMD) Z-scores and the presence of secondary causes of osteoporosis but receiver operating characteristic (ROC) curves indicate that Z-score diagnostic thresholds (such as −2.0) discriminate poorly between the presence and absence of secondary causes of osteoporosis.
Introduction
BMD Z-score diagnostic thresholds have been proposed to detect secondary causes of osteoporosis. To determine the sensitivity and diagnostic utility of such thresholds, we analyzed comprehensive BMD and personal health information data from a large, multispecialty group practice.
Methods
Adult subjects were assigned their lowest axial BMD Z-score and ICD-9 diagnosis codes for secondary causes of osteoporosis when cited at least twice in their electronic medical record. Multiple logistic regression was used to model the prevalence of matching ICD-9 codes as a function of Z-score. ROC curves were used to investigate various Z-score cut points for sensitivity and specificity.
Results
Eighteen thousand six hundred seventy-four subjects were analyzed. Secondary causes of osteoporosis were identified in 31% of men and 16% of women. The frequency of secondary causes varied with age and between genders and varied inversely with Z-score. No inflection point was observed in this relationship to suggest a useful clinical decision threshold. The difference in mean Z-score of those with and without a secondary cause of osteoporosis was biologically slight (±0.3). Low Z-score diagnostic thresholds were insensitive to the presence of secondary causes of osteoporosis and provided relatively poor predictive value.
Conclusions
This DXA cohort confirmed a significant inverse relationship between Z-score and the presence of secondary causes of osteoporosis but diagnostic Z-score thresholds discriminate poorly between the presence and absence of secondary causes of osteoporosis. If only patients with very low Z-scores are evaluated for secondary causes of osteoporosis the diagnostic specificity may be high but most cases will be missed.



Similar content being viewed by others
References
NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis and Therapy (2002) J Am Med Assoc 285:785–795
US Department of Health and Human Services. Bone Health and Osteoporosis: A Report of the Surgeon General (2004) Rockville, MD: U.S. Department of Health and Human Services, Office of the Surgeon General, p. 272
World Health Organization. Assessment of fracture risk and its application to screening for postmenopausal osteoporosis (1994) WHO Technical Report Series 843. WHO, Genève
Cummings SR, Bates D, Black DM (2002) Clinical use of bone densitometry: scientific review. J Am Med Assoc 288:1889–1897
Johnson BE, Lucasey B, Robinson RG, Lukert BP (1989) Contributing diagnoses in osteoporosis. The value of complete medical evaluation. Arch Int Med 149:1069–1072
Baille SP, Davison CE, Johnson FJ, Francis RM (1992) Pathogenesis of vertebral crush fractures in men. Age Ageing 21:139–141
Caplan GA, Scane AC, Francis RM (1994) Pathogenesis of vertebral crush fracture in women. J R Soc Med 87:200–202
Peris P, Guañabens N, Monegal A, Suris X, Alvarez L, Martinez de Osaba MJ, Hernandez MV, Muñoz-Gomez J (1995) Aetiology and presenting symptoms in male osteoporosis. Br J Rheum 34:936–941
Haden ST, Fuleihan GE, Angell JE, Cotran NM, LeBoff MS (1999) Calcidiol and PTH levels in women attending an osteoporosis program. Calcif Tissue Int 64:275–279
Kelepouris N, Harper K, Gannon F, Kaplan FS, Haddad JG (1995) Severe osteoporosis in men. Ann Int Med 123:452–460
Çakir B, Odabasi E, Turan M, Güler S, Kutlu M (2002) Secondary osteoporosis in women. A retrospective analysis. Arch Gynecol Obstet 266:214–217
Cooper A, Brew S, de Lusignan S (2002) The effectiveness of blood tests in detecting secondary osteoporosis or mimicking conditions in postmenopausal women. Br J Gen Pract 52:311–315
Deutschmann HA, Weger M, Weger W, Kotanko P, Deutschmann MJ, Skrabal F (2002) Search for occult secondary osteoporosis: impact of identified possible risk factors on bone mineral density. J Int Med 252:389–397
Tannenbaum C, Clark J, Schwartzman K, Wallenstein S, Lapinski R, Meier D, Luckey M (2002) Yield of laboratory testing to identify secondary contributors to osteoporosis in otherwise healthy women. J Clin Endo Met 87:4431–4437
Crandall C (2003) Laboratory for osteoporosis. Postgrad Med 114(3):35–8, 41-4
Sikon AL, Thacker HL, Carey J, Deal C, Licata AA (2006) Secondary osteoporosis: are we recognizing it? J Women’s Health 15:1174–1183
Khan AA, Hanley DA, Bilezikian JP, Binkley N, Brown JP, Hodsman AB, Josse RG, Kendler DL, Lewiecki EM, Miller PD, Olszynski WP, Petak SM, Syed ZA, Theriault D, Watts NB (2006) Standards for performing DXA in individuals with secondary causes of osteoporosis. J Clin Densitom 9:47–57
Painter SE, Kleerekoper M, Camacho PM (2006) Secondary osteoporosis: a review of the recent evidence. Endo Pract 12:436–445
Rajeswaran C, Spencer J, Barth JH, Orme SM (2007) Utility of biochemical screening in the context of evaluating patients with a presumptive diagnosis of osteoporosis. Clin Rheumatol 26:362–365
Camacho PM, Dayal AS, Diaz JL, Nabhan FA, Agarwal M, Norton JG, Robinson PA, Albain KS (2008) Prevalence of secondary causes of bone loss among breast cancer patients with osteopenia and osteoporosis. J Clin Onc 26:5380–5385
Edwards BJ, Langman CB, Bunta AD, Vicuna M, Favus M (2008) Secondary contributors to bone loss in osteoporosis related hip fractures. Osteoporos Int 19:991–999
Cohen A, Fleischer J, Freeby MJ, McMahon DJ, Irani D, Shane E (2009) Clinical characteristics and medication use among premenopausal women with osteoporosis and low BMD: the experience of an osteoporosis referral center. J Women’s Health 18:79–84
Swaminathan K, Flynn R, Garton M, Paterson C, Leese G (2009) Search for secondary osteoporosis: are Z-scores useful predictors? Postgrad Med J 85(999):38–39
www.NOF.org, accessed 2/10/2010
www.ISCD.org accessed 2/10/2010
DeStefano F, Eaker ED, Broste SK, Nordstrom DL, Peissig PL, Vierkant RA, Konitzer KA, Gruber RL, Layde PM (1996) Epidemiologic research in an integrated regional medical care system: the Marshfield Epidemiologic Study Area. J Clin Epidemiol 49:643–652
Greenlee RT (2003) Measuring disease frequency in the Marshfield Epidemiologic Study Area (MESA). Clin Med Res 1:273–280
Wilke RA, Berg RL, Peissig P, Kitchner T, Sijercic B, McCarty CA, McCarty DJ (2007) Use of an electronic medical record for the identification of research subjects with diabetes mellitus. Clin Med Res 5:1–7
Stone CJ, Koo CY (1986) Additive splines in statistics. Proceedings of the Statistical Computing Section, American Statistical Association, pp. 45–48
Durrleman S, Simon R (1989) Flexible regression models with cubic splines. Stat Med 8:551–561
DeLong ER, DeLong DM, Clarke-Pearson DL (1988) Comparing the areas under two or more correlated receiver operating characteristic curves: a nonparametric approach. Biometrics 44:837–845
Giampietro PF, McCarty CA, Mukesh B, McKiernan F, Wilson D, Shuldiner A, Liu J, LeVasseur J, Ivacic L, Kitchner T, Ghebranious N (2010) The role of cigarette smoking and statins in the development of post menopausal osteoporosis: a pilot study utilizing the Marshfield Clinic Personalized Medicine Cohort. Osteoporos Int 21:467–477
Jamal SA, Leiter RE, Bayoumi AM, Bauer DC, Cummings SR (2005) Clinical utility of laboratory testing in women with osteoporosis. Osteoporos Int 16:534–540
Karga H, Papapetrou PD, Korakovouni A, Papandroulaki F, Polymeris A, Pampouras G (2004) Bone mineral density in hyperthyroidism. Clin Endocrinol 61:466–472
Chiodini I, Mascia ML, Muscarella S, Battista C, Minisola S, Arosio M, Santini SA, Guglielmi G, Carnevale V, Scillitani A (2007) Subclinical hypercortisolism among outpatients referred for osteoporosis. Ann Int Med 147:541–548
www.codemap.com/content.cfm?id = 7280&lcd=29510&sid=1 accessed 2/10/2010
McKiernan FE, Hocking J, Cournoyer S (2006) Antecedent 99mTc-MDP and 99mTc-sestamibi administration corrupts bone mineral density measured by DXA. J Clin Densitom 9:164–166
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Grant support
Marshfield Medical Research Foundation
Rights and permissions
About this article
Cite this article
McKiernan, F.E., Berg, R.L. & Linneman, J.G. The utility of BMD Z-score diagnostic thresholds for secondary causes of osteoporosis. Osteoporos Int 22, 1069–1077 (2011). https://doi.org/10.1007/s00198-010-1307-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-010-1307-1