Abstract
Summary
Racial/ethnic differences were observed in age at peak bone density and their correlates, with whites peaking at least 5 years earlier at the femoral neck than black and Hispanic women. Race-specific standards generated in this study could be useful when interpreting bone densitometry data in young women.
Introduction
The influence of race/ethnicity on bone measurements has not been widely examined. This study identifies age and amount of bone accumulated at peak density and their correlates by race/ethnicity.
Methods
Bone mineral content (BMC) and bone mineral density (BMD) of the spine and femoral neck were measured by dual X-ray absorptiometry in 708 white, black, and Hispanic reproductive-aged women. Race-specific nonlinear models were used to describe the relationship between age and bone measurements, after adjusting for body weight and height. Log-transformed bone measurements were used to determine predictors based on multiple linear regression.
Results
Predictors, which were race and site specific, included age, age at menarche, body weight, height, months of depot medroxyprogesterone acetate use, weight-bearing exercise, and alcohol use. Women of all races gained BMC and BMD at the spine up to 30–33 years of age. BMC and BMD of the femoral neck peaked among white women earlier (≤16 years) than among blacks (BMC 22 years; BMD 21 years) and Hispanics (BMC 29 years; BMD 20 years).
Conclusion
Age at peak bone mass and its correlates differ by race/ethnicity. Race-specific standards generated in this study could be useful when interpreting bone densitometry data in young women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a serious public health problem that is responsible for approximately 1.5 million fractures in the US each year [1]. One of the main determinants of who develops this disease is the amount of bone accumulated at peak bone density. There is poor agreement, however, on when peak bone density occurs. For women, a number of investigators have suggested that bone density peaks within a few years of menarche, while others have observed small, but significant, increases as late as the fourth decade of life [2]. Most recent studies have observed a peak in bone mineral density (BMD) among women during the teenage years [3, 4].
A significant limitation of almost all studies on peak bone density is that most have been conducted on white women only [2, 4–7]. This is a serious omission in the literature as racial differences in BMD have been demonstrated in a few studies [8–10]. Bone density data for Hispanic women are particularly sparse. A few multiracial studies have included Hispanic subjects who could not be evaluated separately because they were merged with other races into “nonwhite” or “nonblack” categories [8]. One study on 230 Asian, Hispanic, black, and white females 9–25 years of age, which did contain enough Hispanic women to analyze as a separate group, observed that total hip, spine, and whole-body BMD all reached a plateau during the teenage years (14.1, 15.7, and 16.4 years of age, respectively) [11]. Blacks and Asians reached this plateau earlier than whites and Hispanics, demonstrating that racial differences in the timing of peak BMD may occur. This well-conducted study, however, did not evaluate whether racial/ethnic differences may have resulted from differences in weight and height, even though blacks and Hispanics had a greater body mass index (BMI) than the whites and Asians in the cohort. Given the known relationship between BMD and body weight, this question warrants further investigation. Furthermore, data on correlates of bone mineral content (BMC) or BMD in minority women are sparse and need to be investigated [12, 13].
The purpose of this study was to determine if correlates of BMC/BMD and age at peak differ by race among a sample of reproductive-aged white, black, and Hispanic women.
Materials and methods
Healthy, reproductive-aged non-Hispanic black, non-Hispanic white, and Hispanic women, 16–33 years of age, who participated in a prospective study of the effect of hormonal contraception on bone mineral density between October 9, 2001 and September 14, 2004, were included in this investigation. Women were excluded from participation if they weighed >300 lb (due to safety limitations of the dual-energy X-ray absorptiometry (DXA) machine), were not eligible to receive hormonal contraceptive containing estrogen, wished to become pregnant in ≤3 years, had received depot medroxyprogesterone acetate or oral contraceptive pills in the last 3 months, had used medications or had a medical condition known to affect BMD, or had a dietary intake known or suspected to be high in isoflavones. In addition, women with abnormal serum levels of vitamin D, parathyroid or thyroid hormone, or liver function tests were excluded as these medical conditions may affect BMD. A total of 805 women out of 2,999 women who responded to advertisements agreed to participate. Of these, 708 women met all eligibility criteria and were included in the current analyses. Written informed consent was obtained from all participants and parental consent was obtained for those <18 years of age. All participants received free well-woman care during participation in the study and were compensated for their time and travel to the clinic. The study received approval from the Institutional Review Board at the University of Texas Medical Branch at Galveston.
In the present analyses, we included data collected for weight, height, current age, age at menarche, daily calcium intake, tobacco and alcohol use, and participation in weight-bearing physical activities using information collected in the clinic on the day of the study visit. Body weight was measured with women wearing light indoor clothing using a digital scale accurate to the nearest 0.1 kg. Height was measured using a wall-mounted stadiometer (Heightronic, Snoqualmie, WA, USA) accurate to the nearest 0.001 m. BMI was calculated as weight (kg) divided by the square of the height (m). Daily calcium intake (in milligram) was assessed in an interview conducted by a registered dietician who administered a 40-item calcium checklist [14]. To determine smoking status, use of tobacco was measured using questions from the MONICA Smoking Assessment [15]. Current smokers were those who reported either regular or occasional smoking, while nonsmokers were those women who currently do not smoke although they could have smoked in the past. Alcohol use was calculated from questions on the Diet History Questionnaire regarding how often subjects drank alcohol (either beer, wine or wine coolers, or liquor or mixed drinks) during the past 12 months and the amount usually consumed when drinking [16].
Weight-bearing physical activity was taken from a measure that included a list of 56 common activities, and questions on the frequency and duration of up to two physical activities performed during the past month. Kolle and colleagues have reported that the total number of minutes per week devoted to weight-bearing exercise(s) should include a medium (121–234 min) to high (235 min or more) level in order to positively impact BMD levels in reproductive-aged women [17]. Based on their findings, we categorized weight-bearing exercise into two groups including no exercise to light exercise (≤120 min/week) versus medium to high levels of exercise (≥121 min/week).
Bone densitometry was conducted using DXA (Hologic QDR 4500W Elite fan-beam densitometer). Long-term accuracy of the instrument was assessed through the use of a phantom spine calibrated daily prior to the scanning of participants. The in vitro coefficient of variation of this machine calculated on a spine phantom was 0.27%. All scanning and analyses were conducted by certified radiologic technologists using a standardized protocol recommended by the International Society for Clinical Densitometry. The same technologist scanned 78% of the subjects; two additional technologists scanned the remaining 19% and 3% of the subjects, respectively. To evaluate the reproducibility, the in vivo coefficient of variation was obtained by scanning 30 healthy women twice in the same day by the same technologist as has been recommended [18, 19]. The site-specific coefficient of variation was 0.55% for the lumbar spine, 0.78% for the hip, 1.95% for the femoral neck, 4.83% for the spine bone mineral apparent density (BMAD), and 5.63% for the femoral neck BMAD.
Densitometry measurements included BMD (g/cm2) measured at the lumbar spine (L1–L4) and total hip (Ward’s triangle, greater trochanter, intertrochanter, and femoral neck) of the left hip. Hip data are presented separately for the femoral neck, as this particular site is highly predictive of hip fracture [20]. Calculations for BMD (BMD = BMC [g] / projected area of the bone [cm2]) have been shown to be influenced by bone size as they are based on two of three dimensions of bones (length and width without depth). To address this issue, we also calculated spine BMAD (g/cm3), which is an approximation of the volumetric density of bone estimated from the BMC and the projected area of the bone (A) using the formula described by Carter et al. (spine BMAD = BMC / A 3/2) [21]. In this formula, the volume of the measured spine is approximated by A 3/2. We also calculated BMAD of the femoral neck by applying a formula developed by Katzman et al: femoral neck BMAD = BMC / A 2 [22]. Estimates of total fat mass (g), percent fat mass, and lean mass (g) were generated from DXA scans of the whole body.
Statistical analysis
One-way analysis of variance with Bonferroni corrections for continuous variables and chi-squared tests for categorical variables were used to compare the three race/ethnic groups. We used multiple linear regression techniques to explore the relationship between the dependent variable (BMC, BMD, or BMAD) and the set of independent variables (age, age at menarche, race/ethnicity, weight, height, parity, months of DMPA/pill use, smoking, alcohol use, weight-bearing exercise, and calcium intake). The skewness-kurtosis test and ladder of powers were used to determine whether the dependent variable should be transformed and to identify the transformation. First, a model with all races/ethnicities was tried with main effects and interaction terms. If the interaction term between race/ethnicity and any of the two major variables (weight or height) was significant, three race-specific models were built.
We used the same nonlinear models [β0eL / (1 + eL)] used by others [5, 23] to estimate the age at peak BMC/BMD, where L is the linear function of the explanatory variables (age, height, and weight). BMC/BMD/BMAD values adjusted by the nonlinear regression model were used to estimate the age at peak bone mineral content/density. Additional robust nonparametric smoothing techniques were used to provide the estimate as a function of age [24]. In this method, a weighted linear regression is run on the points surrounding the one of interest and the predicted value is obtained. A separate model was used for each race/ethnicity. The models were fit using the STATA’s nl module (version 9, Stata Corporation, College Station, TX, USA).
Results
A total of 708 white, black, and Hispanic women with a mean age of 24.3 years were included. Chronological age, age at menarche, percent body fat, alcohol use, and weight-bearing exercise did not differ among the three racial/ethnic groups (Table 1). However, black women were more likely to have higher values for body weight, BMI, lean mass, fat mass, months of prior DMPA use, and BMC/BMD/BMAD (except spine BMC) relative to white and Hispanic women. On the other hand, white and Hispanic women were more likely to be currently married, have a history of lactation, and have close relatives with a history of height loss and broken bones compared to black women. White women were more likely to be current smokers and had the lowest BMI, spine and femoral neck BMAD, and parity.
BMC, BMD, and BMAD were transformed to natural logarithms (ln) for analysis. Since there were significant interactions between the main explanatory variables of weight/height and BMC/BMD/BMAD, separate multiple linear regression models for each race were performed. A multiple linear regression model with logarithms of spine BMC [ln(SBMC)] as the dependent variable showed significant relationships with height and months of prior DMPA use among black women (Table 2). A similar model with logarithms of femoral neck BMC [ln(FNBMC)] as the dependent variable also identified weight as a predictor. Predictors of ln(SBMC) and ln(FNBMC) among white women were age and height, and age, weight, height, and amount of weight-bearing exercise, respectively. The predictors among Hispanic women for ln(SBMC) were age at menarche, weight, and height, and for ln(FNBMC) weight, height, and alcohol use.
There were more statistically significant predictors of BMD than for BMC, especially among black women (Table 3). Among this group, age, age at menarche, weight, height, and months of prior DMPA use were all predictors of ln(SBMD). Among white women, only weight reached significance for ln(SBMD) while age at menarche and weight were predictors for Hispanics. Two predictors (age and weight) of ln(FNBMD) were common in all races. In addition, months of prior DMPA use in black women, weight-bearing exercise in white women, and alcohol use in Hispanic women were predictive.
The predictors of ln(SBMAD) and ln(SBMD) were similar in all race/ethnic groups. However, DMPA use in blacks, age in whites, and alcohol use in Hispanics were not significant predictors of ln(FNBMAD) while they were significant for respective ln(FNBMD) models. Height was not included in any BMAD regression models as it was already adjusted in BMAD calculations.
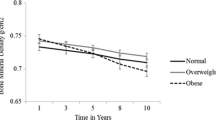
Table 4 and Figs. 1 and 2 show the relationships between age and BMC, BMD, and BMAD by race/ethnicity after adjusting for weight and height using nonlinear equation and smoothing techniques. The R 2 values for different nonlinear regressions ranged from 0.95 to 0.99, which indicates the good fit of the models. Both SBMC and SBMD did not reach an asymptote for blacks and Hispanics and continued to increase with age. Whites’ SBMD peaked at the age of 30. FNBMC peaked at the age of 22 among blacks and between 29 and 31 years among Hispanics. The respective peak for FNBMD was 21 and 20 years. However, whites did not gain BMC or BMD at the femoral neck and their values continued to decrease with age. The scenarios for SBMAD and FNBMAD are similar to those of SBMD and FNBMD (Fig. 2).
Discussion
This is the first study, of which we are aware, to examine BMC/BMD correlates based on race/ethnicity in a single setting. Based on mostly white populations, it has been reported that dietary calcium [25], physical activity [26, 27], smoking [27], alcohol use [27, 28], age at menarche [29], early pregnancy [28], and prolonged breast-feeding [30] can influence peak bone density. We observed that several of these correlates of BMD are site and race specific. For example, age at menarche was significant at the lumbar spine only for blacks and Hispanics. At the femoral neck, weight-bearing exercise was significant only for white women and alcohol use only for Hispanics. Moreover, prior DMPA use was a factor among blacks but not whites or Hispanics at both the lumbar spine and femoral neck. Future studies are needed to confirm that these factors are specific to certain populations so clinicians can provide individualized counseling to women of different racial/ethnic groups.
We also observed that there are racial differences in the timing of peak bone density at the femoral neck. White women included in this study had reached their peak BMC and BMD at this site by age 16. This very young age at peak BMD of the hip is in agreement with prior studies on white populations [4, 31, 32]. Stratification by race/ethnicity further demonstrated that black and Hispanic women exhibited higher BMC and BMD values than white women at the femoral neck for at least an additional 5 years. Similar to our findings on Hispanic women, peak BMD was noted to occur at the femoral neck between age 20 and 29 years in a sample of 131 Puerto Rican Women [33]. This earlier peak among whites as compared with minority women may contribute to racial differences in BMD and the increased risk of hip fractures noted among white women after menopause.
We observed the highest spinal BMD values in white women at 30 years of age. In contrast, Lin et al. noted that BMD reached a peak among whites by 23 years of age but that BMC continued to increase during the early thirties [5]. Several exclusion criteria of Lin’s study could be responsible for differences in findings between the two studies. For example, Lin excluded some participants who had participated in >2 h/week of exercise and others with calcium intake >1,200 mg/day. Since exercise and calcium intake may be related to BMD, exclusion of these women could have affected their findings. Moreover, women included in Lin’s study weighed less on average than those in our study (60 vs 73 kg, respectively). Our findings do mirror those of Henry et al. who observed in a sample of 68 white women that peak volumetric BMD was attained by 29 years of age [6]. We also examined peak values in black and Hispanic women and noted that these women continued to exhibit an increase in spinal BMD values until 33 years of age. However, it should be noted that we did not have data on women over age 33, so we were not able to determine if peak values occurred at 33 years or at a later point in time. If minority women continued to increase their BMD after this point, racial differences in the timing of peak values may actually be larger than we observed.
Studies on postmenopausal women have shown that Hispanic women are at lower risk of osteoporosis and fractures than whites [34, 35]. One reason suggested for this lower risk among Hispanics is that the BMD of older Hispanic women is greater that that of whites [35, 36]. We observed, however, that white women actually have greater BMD than Hispanics at both the lumbar spine and femoral neck during adolescence. In fact, the greater BMD observed in Hispanic women as compared with whites later in life is not apparent until 29 years of age at the lumbar spine and 20 years of age at the femoral neck. This change is due to an earlier peak and more rapid decline in BMD following their peak BMD among whites. It is most likely the continuation of this trend that places white women at much higher risk of fractures later in life than their Hispanic counterparts. Thus, it appears that one approach to osteoporosis prevention may be to determine why this rapid decline occurs among white women and attempt to slow the process during their reproductive years rather than waiting to intervene once osteoporosis has already occurred.
Similar to the study conducted by Lin et al. [5], we did not observe a correlation between dietary calcium intake and BMC or BMD. This may have been the result of our study design. While most interventional studies of young healthy women have shown a correlation [37–40], longitudinal and cross-sectional studies have reported inconsistent results [26, 41–43]. A meta-analysis based on mostly cross-sectional studies showed a weak correlation coefficient (0.13) [44]. The lack of correlation between bone health and calcium intake may also have resulted from measurement error if women incorrectly reported portion sizes or types of food consumed. Furthermore, the calcium intake of 625 mg/day reported in this population was far below the recommended amount of 1,300 mg/day for those 9–18 years of age and 1,000 mg for those 19–50 years of age [45], which may not be sufficient to affect bone density. Finally, we assessed current calcium intake, which has been shown to be less predictive of BMC and BMD than that consumed during the teenage years. Future studies that include women of different races/ethnicities are needed to clarify this issue.
This study has several limitations. First, we used cross-sectional data to study changes over time, rather than longitudinal data. Investigating patterns of BMD gain and loss over a 15–20-year interval, however, would have considerable limitations, including subject attrition and the probable use of multiple bone densitometry machines and radiologic technicians over time. Second, we obtained data on calcium intake, amount of exercise, and age at menarche by retrospective self-report, which is subject to recall bias. Third, errors in recall regarding age at menarche may have affected our calculations of gynecological age. Finally, use of a single site could limit the generalizability of our findings.
Most DXA manufacturers use data collected on white females during the National Health and Nutrition Examination Survey III as a reference standard for calculation of the t score. Few data are available on healthy women of reproductive age. This study addresses this gap in the literature by providing data on young women 16–33 years of age from three different racial/ethnic groups. Although standards are machine specific, measurements reported in this study may be useful in the interpretation of bone densitometry data in reproductive-aged women.
These data support the need for education regarding bone health during the early reproductive years. Initial steps may include education in the schools regarding timing of peak bone density and modifiable risk factors. In particular, young white girls and their families should be informed that peak bone density occurs at the hip by early adolescence and that weight-bearing exercise has a positive impact on bone health. By addressing this issue early in life, it may be possible to decrease the number of women affected by osteoporosis and subsequent fractures later in life.
References
National Institutes of Health (2007) Osteoporosis Overview. Osteoporosis and Related Bone Diseases National Resource Center. http://www.niams.nih.gov/Health_Info/Bone/Osteoporosis/default.asp. Accessed May 13, 2008
Sabatier JP, Guaydier-Souquieres G, Benmalek A et al (1999) Evolution of lumbar bone mineral content during adolescence and adulthood: A longitudinal study in 395 healthy females 10–24 years of age and 206 premenopausal women. Osteoporos Int 9:476–482
van der Sluis I, de Ridder MA, Boot AM et al (2002) Reference data for bone density and body composition measured with dual energy X-ray absorptiometry in white children and young adults. Arch Dis Child 87:341–347
Lloyd T, Chinchilli VM, Eggli DF et al (1998) Body composition development of adolescent white females: The Penn State Young Women’s Health Study. Arch Pediatr Adolesc Med 152:998–1002
Lin YC, Lyle RM, Weaver CM et al (2003) Peak spine and femoral neck bone mass in young women. Bone 32:546–553
Henry YM, Fatayerji D, Eastell R (2004) Attainment of peak bone mass at the lumbar spine, femoral neck and radius in men and women: relative contributions of bone size and volumetric bone mineral density. Osteoporos Int 15:263–273
Wren TA, Kim PS, Janicka A et al (2007) Timing of peak bone mass: discrepancies between CT and DXA. J Clin Endocrinol Metab 92:938–941
Kalkwarf HJ, Zemel BS, Gilsanz V et al (2007) The bone mineral density in childhood study: bone mineral content and density according to age, sex, and race. J Clin Endocrinol Metab 92:2087–2099
Cromer BA, Binkovitz L, Ziegler J et al (2004) Reference values for bone mineral density in 12- to 18-year-old girls categorized by weight, race, and age. Pediatr Radiol 34:787–792
Henry YM, Eastell R (2000) Ethnic and gender differences in bone mineral density and bone turnover in young adults: effect of bone size. Osteoporos Int 11:512–517
Bachrach LK, Hastie T, Wang MC et al (1999) Bone mineral acquisition in healthy Asian, Hispanic, black, and Caucasian youth: a longitudinal study. J Clin Endocrinol Metab 84:4702–4712
Harel Z, Gold M, Cromer B et al (2007) Bone mineral density in postmenarchal adolescent girls in the United States: associated biopsychosocial variables and bone turnover markers. J Adolesc Health 40:44–53
Wang MC, Aguirre M, Bhudhikanok GS et al (1997) Bone mass and hip axis length in healthy Asian, black, Hispanic, and white American youths. J Bone Miner Res 12:1922–1935
Hertzler AA, Frary RB (1994) A dietary calcium rapid assessment method (RAM). Top Clin Nutr 9:76–85
World Health Organization (1999) Smoking Questionnaire. MONICA Manual (1998–1999), Part III, Section 1. The WHO MONICA (Multinational Monitoring Trends in Cardiovascular Disease) Project
National Cancer Institute (2000) Diet History Questionnaire (DHQ). National Institutes of Health
Kolle E, Torstveit MK, Sundgot-Borgen J (2005) Bone mineral density in Norwegian premenopausal women. Osteoporos Int 16:914–920
Baim S, Wilson CR, Lewiecki EM et al (2005) Precision assessment and radiation safety for dual-energy X-ray absorptiometry: position paper of the International Society for Clinical Densitometry. J Clin Densitom 8:371–378
Ravaud P, Reny JL, Giraudeau B et al (1999) Individual smallest detectable difference in bone mineral density measurements. J Bone Miner Res 14:1449–1456
Marshall D, Johnell O, Wedel H (1996) Meta-analysis of how well measures of bone mineral density predict occurrence of osteoporotic fractures. BMJ 312:1254–1259
Carter DR, Bouxsein ML, Marcus R (1992) New approaches for interpreting projected bone densitometry data. J Bone Miner Res 7:137–145
Katzman DK, Bachrach LK, Carter DR et al (1991) Clinical and anthropometric correlates of bone mineral acquisition in healthy adolescent girls. J Clin Endocrinol Metab 73:1332–1339
Teegarden D, Proulx WR, Martin BR et al (1995) Peak bone mass in young women. J Bone Miner Res 10:711–715
Cleveland WS (1979) Robust locally weighted regression and smoothing scatterplots. J Amer Statist Assoc 74:829–836
Kanders B, Dempster DW, Lindsay R (1988) Interaction of calcium nutrition and physical activity on bone mass in young women. J Bone Miner Res 3:145–149
Lloyd T, Beck TJ, Lin HM et al (2002) Modifiable determinants of bone status in young women. Bone 30:416–421
Stevenson JC, Lees B, Devenport M et al (1989) Determinants of bone density in normal women: risk factors for future osteoporosis? BMJ 298:924–928
Sowers M, Wallace RB, Lemke JH (1985) Correlates of forearm bone mass among women during maximal bone mineralization. Prev Med 14:585–596
Rosenthal DI, Mayo-Smith W, Hayes CW et al (1989) Age and bone mass in premenopausal women. J Bone Miner Res 4:533–538
Sowers M, Corton G, Shapiro B et al (1993) Changes in bone density with lactation. JAMA 269:3130–3135
Theintz G, Buchs B, Rizzoli R et al (1992) Longitudinal monitoring of bone mass accumulation in healthy adolescents: evidence for a marked reduction after 16 years of age at the levels of lumbar spine and femoral neck in female subjects. J Clin Endocrinol Metab 75:1060–1065
Sabatier JP, Guaydier-Souquières G, Laroche D et al (1996) Bone mineral acquisition during adolescence and early adulthood: a study in 574 healthy females 10–24 years of age. Osteoporos Int 6:141–148
Haddock L, Ortiz V, Vazquez MD et al (1996) The lumbar and femoral bone mineral densities in a normal female Puerto Rican population. P R Health Sci J 15:5–11
Fang J, Freeman R, Jeganathan R et al (2004) Variations in hip fracture hospitalization rates among different race/ethnicity groups in New York City. Ethn Dis 14:280–284
Looker AC, Orwoll ES, Johnston CC et al (1997) Prevalence of low femoral bone density in older US adults from NHANES III. J Bone Miner Res 12:1761–1768
Castro JP, Joseph LA, Shin JJ et al (2005) Differential effect of obesity on bone mineral density in White, Hispanic and African American women: a cross sectional study. Nutr Metab (Lond) 2:9
Matkovic V, Goel PK, Badenhop-Stevens NE, Landoll JD, Li B, Ilich JZ, Skugor M, Nagode LA, Mobley SL, Ha EJ, Hangartner TN, Clairmont A (2005) Calcium supplementation and bone mineral density in females from childhood to young adulthood: a randomized controlled trial. Am J Clin Nutr 91:175–188
Merrilees MJ, Smart EJ, Gilchrist NL, Frampton C, Turner JG, Hooke E, March RL, Maguire P (2000) Effects of dairy food supplements on bone mineral density in teenage girls. Eur J Nutr 39:256–262
Rozen GS, Rennert G, Dodiuk-Gad RP, Rennert HS, Ish-Shalom N, Diab G, Raz B, Ish-Shalom S (2003) Calcium supplementation provides an extended window of opportunity for bone mass accretion after menarche. Am J Clin Nutr 78:993–998
Dodiuk-Gad RP, Rozen GS, Rennert G, Rennert HS, Ish-Shalom S (2005) Sustained effect of short-term calcium supplementation on bone mass in adolescent girls with low calcium intake. Am J Clin Nutr 81:168–174
Zhu K, Greenfield H, Zhang Q, Du X, Ma G, Foo LH, Cowell CT, Fraser DR (2008) Growth and bone mineral accretion during puberty in Chinese girls: a five year longitudinal study. J Bone Miner Res 23:167–172
Mein AL, Briffa NK, Dhaliwal SS, Price RI (2004) Lifestyle influences on 9-year changes in BMD in young women. J Bone Miner Res 19:1092–1098
Lloyd T, Petit MA, Lin HM, Beck TJ (2004) Lifestyle factors and the development of bone mass and bone strength in young women. J Pediatr 144:776–782
Welten DC, Kemper HC, Post GB, van Staveren WA (1995) A meta-analysis of the effect of calcium intake on bone mass in young and middle aged females and males. J Nutr 125:2802–2813
National Institutes of Health, Office of Dietary Supplements. Dietary Supplement Fact Sheet: Calcium. http://ods.od.nih.gov/factsheets/calcium.asp. Accessed 22 July 2008
Conflicts of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by the National Institute of Child Health and Human Development grants R01HD39883 and K24HD043659 awarded to ABB and General Clinical Research Centers (GCRC) program, National Center for Research Resources, NIH, M01RR000073.
Rights and permissions
Open Access This is an open access article distributed under the terms of the Creative Commons Attribution Noncommercial License (https://creativecommons.org/licenses/by-nc/2.0), which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
About this article
Cite this article
Berenson, A.B., Rahman, M. & Wilkinson, G. Racial difference in the correlates of bone mineral content/density and age at peak among reproductive-aged women. Osteoporos Int 20, 1439–1449 (2009). https://doi.org/10.1007/s00198-008-0817-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00198-008-0817-6