Abstract
Introduction and hypothesis
Minorly skilled gynecologists are less likely to repair obstetric anal sphincter injuries (OASIS), and this can lead to higher rate of de novo onset of pelvic floor dysfunction (PFD). The aim of this study was to understand the impact of surgeon skills in OASIS repair on de novo incidence of PFDs.
Methods
An observational prospective cohort study performed between January 2019 and December 2020. We included 116 women with OASIS. At 6-weeks from delivery, women were divided into two groups in relation to the onset of PFDs. Characteristics were compared; categorical and continuous variables were assessed with chi-squared test and the Mann–Whitney rank-sum test respectively. Factors involved in PFDs development were analysed with explorative univariate analysis; significant (p<0.05) or approaching significance (p≤0.10) variables were included in multivariable analysis.
Results
Seventy-six women (76/116; 65.5%) reported at least one PFD symptom and anal incontinence was the most prevalent (44.73%; 34/76). OASIS management by a skilled gynaecologist resulted protective for PFDs [aOR 0.33 (0.13-0.61)]. Skilled surgeon reported fewer PFDs than less skilled surgeon (4% vs 82.4%; p<0.0001). Operative delivery was more performed (32.5% vs 15.8%; p= 0.03) and severe OASIS resulted more prevalent (60% vs 17.1%; p<0.0001) among women without PDFs, even if these didn’t affect the incidence of de novo PFDs [aOR 1.03 (0.23-1.45) and 0.83 (0.13-1.45), respectively].
Conclusions
Surgeons skilled in OASIS repair resulted the only protective factor for incidence of de novo PFDs in women with OASIS at 6 weeks of follow up. Improvement of training in OASIS repair is necessary.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Obstetric anal sphincter injuries (OASIS) are one of the most dramatic, and often not predictable, consequences of the vaginal delivery, in particular in case of operative delivery. The incidence of this event reported in the available literature is variable between 1% and 18% and depends from several obstetric factors, such as the use of vacuum, the fetal weight, the use and the type of episiotomy and the duration of the second stage of labour [1, 2].
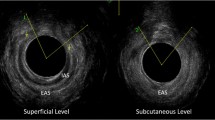
The Royal College of Obstetricians and Gynaecologists (RCOG) classified the perineal tears into four degrees. From the 3th degree the anal sphincter complex is involved. The IIIA degree is defined as the involvement of less than 50% of the external anal sphincter (EAS), the IIIB degree as the involvement of more than 50% of the EAS and the IIIC degree when both the EAS and the internal anal sphincter (IAS) are injured. The 4th degree injury involves all the anal sphincter complex (IAS and EAS) and the anal epithelium [3].
OASIS can have a significant impact on women’s quality of life, due to complications in the short and long term (perineal pain, abscess, rectovaginal fistula, wound breakdown, and anorectal symptoms). These are the most common cause of anal incontinence (AI) in otherwise healthy women. After primary repair of OASIS, the reported rates of AI range between 15 and 61%; this high prevalence underlines the need of optimal surgical techniques and post-operative management [4]. It is well demonstrated that a gynaecologist skilled in OASIS management can improve the detection of OASIS [5], and the last recommendations of RCOG highlighted that the repair of the third- and fourth-degree tears should be conducted by an appropriately trained clinician. However, very few data on the impact of a specific ability of the surgeon on the outcomes of OASIS repair exists.
The aim of this study was to evaluate the impact of the surgical skills of the surgeon involved in the OASIS repair on the de novo onset of pelvic floor dysfunctions (PFDs).
Materials and methods
This is an observational analytical prospective cohort study performed in a tertiary teaching maternity hospital, between January 2019 and December 2020. We included all consequent women who have given birth in our department and that have had anal sphincter injury according to RCOG classification. An OASIS was defined as severe when IIIC- or IV-degree perineal tears occurred. Exclusion criteria were history of PFDs related symptoms prior to delivery (anal incontinence, urinary incontinence, dyspareunia, pelvic organ prolapse and other pelvic floor disorders), preterm deliveries, twin pregnancies.
Considering the delivery room setting in our Institution, midwives attend independently about the 20% of deliveries (low risk pregnancy and low risk labor). The team of physicians available in our Hospital is constantly composed by two gynaecologists, three obstetricians, an anaesthetist and a senior gynaecologist available remotely.
When an OASIS occurs, a gynaecologist skilled on OASIS repair is contacted to repair the perineal tears. If he is not available, the anal sphincter repair is performed by the senior gynaecologist present at the delivery. We considered as skilled on OASIS repair only a gynaecologist who presents all the following characteristics: who has a large experience on vaginal surgery (at least fifty pelvic reconstructive surgeries performed), who has attended at least one theoretical-practical course based on RCOG guidelines for OASIS repair and that has already repaired at least ten OASIS.
According to RCOG guidelines for OASIS diagnosis, after each vaginal delivery a systematic recto-vaginal examination is performed. When the physician and the midwife who attended the delivery are diagnostically concordant on the OASIS detection and on the degree of the OASIS, we retain that there is no need for a third figure to verify the diagnosis. Contrary, if concordance lacks, a third health medical provider verifies the diagnosis and the degree of the OASIS.
The surgical technique, the operative theatre, the materials used were conform to the last guidelines published by the RCOG [6]. Specifically, where the torn IAS could be identified, it was separately repaired with interrupted or mattress sutures without any attempt to overlap the IAS. For the repair of a full thickness EAS tear either an overlapping or an end-to-end (approximation) method were adopted. For partial thickness (all 3A and some 3B) tears, an end-to-end technique was performed. For 3C and 4th degree tears we performed always an overlap technique. The torn anorectal mucosa was repaired with sutures using either the continuous or interrupted technique. 3-0 polyglactin was used to repair the anorectal mucosa. When repair of the EAS and/or IAS muscle is performed, either monofilament sutures such as 3-0 PDS or modern braided sutures such as 2-0 polyglactin are used. All these patients received an antibiotic prophylaxis for six days after the surgical procedure.
All patients were assessed at the follow up visit, six weeks after labour. Demographic data and medical history were collected, PFDs related symptoms as stress and urge urinary incontinence, anal incontinence (reported as faecal incontinence, gas leakage and soiling), dyspareunia and pelvic organ prolapse symptoms were assessed, physical examination and pelvic ultrasonography were performed. The terminology used to define PFD symptoms is conform to the standardization document of the International Urogynecological Association and the International Continence Society (IUGA/ICS). Each patient was asked to record the symptoms degree of bother by a visual analogue scale (VAS) with a score from 0 to 10. Women asymptomatic for PFD who had anal sphincter injury were directed to pelvic floor rehabilitation at 3-4 months after the delivery; to symptomatic patients we proposed to start the pelvic floor muscle training immediately after the screening visit.
The Institutional Review Board approval for the current study was obtained and each woman enrolled in the study signed an informed consent for treatment of personal data. The study was conducted according to the Declaration of Helsinki.
Statistical analysis
Statistical analysis was performed with IBM-SPSS v.17 for Windows (IBM Corp, Armonk, NY, USA). Student’s t test and the Mann–Whitney rank sum test were performed to compare continuous parametric and nonparametric variables, as appropriate. Categorical variables were analyzed using the Chi-squared test and the Fisher exact test as appropriate. Continuous variables were reported as median and interquartile range (IQR).
Exploratory univariate was applied to test the association between risk factors for PFD development. Variables that had a significant association with the adopted scores at univariate analysis were eventually included in the multivariate analyses. A p-value <0.05 was considered statistically significant.
Results
During the study period, 117 women with OASIS met the inclusion criteria and 116 of them (116/117; 99.14%) were enrolled in our study at six weeks from vaginal delivery (1/117; 0.86% was lost at follow up). Firstly, we divided the patients into two groups: the first group included patients with de novo PFD, while the second group included women asymptomatic for PFD. The general and obstetric characteristics of the two cohorts are described in Table 1. Seventy-six women (76/116; 65.5%) reported at least one symptom of PFD occurred after vaginal delivery. Asymptomatic women had a significantly higher rate of operative vaginal delivery and of severe OASIS than women complaining of PFD. Furthermore, asymptomatic women resulted more frequently treated by a surgeon skilled on OASIS repair. Prevalence and severity of each symptom is summarized in Table 2, with AI reported as the most prevalent condition among symptomatic women (44.73%; 34/76). Explorative univariate analysis showed that operative delivery, severity of anal sphincter tears (≥ IIIC degree) and the surgical skills of the surgeon were associated to a significantly lower risk of PFD (Table 3). However, after multivariable analysis, only the surgical skills of the surgeon resulted an independent predictive factor of significantly lower rate of PFDs [aOR 0.33; (0.13-0.61), p<0.0001]. Comparing the 25 cases of OASIS repaired by a skilled surgeon to the other 91 women with OASIS, we showed that in the first group there was a significantly higher rate of severe OASIS and a lower number of women complaining of PFD (Table 4). When the perineal tear was repaired by a trained surgeon, no reintervention was necessary while in the other cohort, we had 4 complications (4/91) that needed re-intervention; however this difference did not result statistically significant.
Discussion
This study demonstrated the presence of a strong association between the surgeon’s skill in OASIS surgical repair and the reduced incidence of de novo PFD symptoms at 6 weeks from vaginal delivery [aOR 0.33; (0.13-0.61)]. Indeed, gynecologists skilled on vaginal surgery and OASIS repair reported a fewer rate of PFDs than less skilled surgeons (4% vs 82.4%; p<0.0001).
Unexpectedly, among women not-complaining of PFDs, operative delivery was more frequently performed (32.5% vs 15.8%; p= 0.03) and severe OASIS resulted more prevalent (60% vs 17.1%; p<0.0001). Vaginal operative delivery is a well-known risk factor for OASIS, which in turn can negatively affect stool function and thus quality of life [7]. When vaginal deliveries are complicated by OASIS and/or operative intervention, prevalence of AI is reported to increase [8]. The higher prevalence of operative vaginal delivery reported in the cohort of women without PFD at 6 weeks of follow-up could be explained considering that, in case of more severe OASIS associated with operative delivery, a highly qualified gynecologist was called and involved.
In fact, at multivariate analysis operative vaginal delivery and severe OASIS did not result as risk factors for PFDs.
Additionally, our data confirmed the high prevalence of pelvic floor dysfunctions (65.5%; 76/116) in women with a post-partum diagnosis of OASIS. Among PFDs, AI (defined as gas leakage, fecal incontinence and soiling) resulted as the most frequent symptom reported by the 44.73% of symptomatic women. These data are in line with the previous literature. Evidences of long-term impact of OASIS on long-term prevalence of pelvic floor dysfunction as AI, urinary incontinence and sexual dysfunction are growing [7]. A recent meta-analysis evidenced that the half of women with a repaired OASIS will have persistent sphincter defects and that OASIS are associated with a higher risk for AI [4]. These findings have also been proved with a large prevalence at a long-term follow up [8]. Moreover, a history of OASIS delays the resumption of coital activity among women with spontaneous delivery, reflecting the long-term effects of severe perineal and pelvic trauma on postpartum sexuality [9].
At our knowledge, this is the first study aimed to evaluate the impact of the ability of the surgeon involved in the perineal repair on the outcomes of patients with OASIS. The originality of our analysis, with strict inclusion and exclusion criteria, and the high number of OASIS considered, despite the single center enrolment, are points of strength of the study. A post-hoc power analysis was performed; considering a PFDs rate in the control group (minorly skilled surgeon) of 82.4% and of 4% in the study group (skilled surgeon), with a sample size of 91 and 25 respectively, with an alpha error of 0.05, the power of the study resulted to be the 100%. Moreover, several obstetrical factors usually involved in development of PFD after vaginal delivery (use of vacuum, fetal weight, use and type of episiotomy, duration of second stage of labour, etc.) have been explored and then weight in a multivariate analysis concluding that the surgeon ability in vaginal surgery is the most important independent protective factor for the development of PFDs. Additionally, the narrow period of enrolment, in which few changes could have been in mode of repair and clinicians, gives more homogeneity to our results. However, the short time follow up can be considered a limitation of the study, as conditions like urinary incontinence, anal incontinence and dyspareunia could be underestimated and can present later as new symptoms. Furthermore, we didn’t report the incidence among groups of a non-visible pelvic floor damage in the form of partial or complete avulsions of the levator ani muscle (LAM), that can occur in up to 6-63% of vaginal delivery. LAM can cause short- and long-term PFD symptoms and its incidence is reported to be related to OASIS [10]. Lastly, due to Covid-19 pandemic, we did not assess PFD symptoms with validated questionnaires but only with a 0-10 VAS.
This study leads, in our opinion, to a medicolegal dilemma: if missed OASIS could be recognised immediately post-partum and adequately repaired by a surgeon skilled in vaginal approach, would the outcomes be better? The current study assess that it could be possible to reduce PFDs rate if perineal repair is performed by a more skilled surgeon. Therefore, it seems to be desirable and priority to implement training of obstetricians and gynaecologists in repair of complex perineal tears.
Conclusions
Skills on vaginal surgery and on OASIS repair resulted an independent protective factor for pelvic floor dysfunction in women affected by a post-partum OASIS at 6 weeks of follow up from vaginal delivery. The management of severe OASIS by a skilled gynecologist is auspicated in order to reduce post-partum PFD symptoms. Improvement of training and education in repair of perineal tears is necessary. Long-term follow up studies are needed to confirm these evidences.
References
Cattani L, Neefs L, Verbakel JY, Bosteels J, Deprest J. Obstetric risk factors for anorectal dysfunction after delivery: a systematic review and meta-analysis. Int Urogynecol J. 2021;32:2325–36.
Serati M, Salvatore S, Khullar V, Uccella S, Bertelli E, Ghezzi F, Bolis P. Prospective study to assess risk factors for pelvic floor dysfunction after delivery. Acta Obstet Gynecol Scand. 2008;87:313–8.
Obstetrical Anal Sphincter Injuries (OASIS): Prevention, Recognition, and Repair. Marie-Andrée Harvey; Marianne Pierce; et al. SOGC Clinical Practice Guideline. 2015;37(12):P1131-1148.
Sideris M, McCaughey T, Hanrahan JG, Arroyo-Manzano D, Zamora J, Jha S, Knowles CH, Thakar R, Chaliha C, Thangaratinam S. Risk of obstetric anal sphincter injuries (OASIS) and anal incontinence: A meta-analysis. Eur J Obstet Gynecol Reprod Biol. 2020;252:303–12.
Andrews V, Sultan AH, Thakar R, Jones PW. Occult anal sphincter injuries--myth or reality? BJOG. 2006;113:195–200.
RCOG. Third- and Fourth-degree Perineal Tears, Management (Green-top Guideline 29). RCOG Greentop Guidelines. London: RCOG; 2015.
Schütze S, Hohlfeld B, Friedl TWP, Otto S, Kraft K, Hancke K, Hüner B, Janni W, Deniz W. Fishing for (in)continence: long-term follow-up of women with OASIS–still a taboo. Arch Gynecol Obstet. 2020;303(4):987–97.
Johannessen HH, Mørkved S, Stordahl A, Wibe A, Falk RS. Evolution and risk factors of anal incontinence during the first 6 years after first delivery: a prospective cohort study. BJOG. 2020;127:1499–506.
Anglès-Acedo S, Ros-Cerro C, Escura-Sancho S, Elías-Santo-Domingo N, Palau-Pascual NJ, Espuña-Pons M. Coital resumption after delivery among OASIS patients: differences between instrumental and spontaneous delivery. BMC Women's Health. 2019;19:154.
Kimmich N, et al. Prediction of levator ani muscle avulsion by genital tears after vaginal birth—a prospective observational cohort study. Int Urogynecol J. 2020;31:2361–6.
Author information
Authors and Affiliations
Contributions
- M. Serati: conceptualization, formal analysis, data curation, writing original-draft, project administration
- A.F. Ruffolo: writing original-draft, visualization
- C. Scanciarello: data curation, investigation
- A. Braga: methodology, validation
- S. Salvatore: supervision
- F. Ghezzi: supervision
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Maurizio Serati, President of European Urgynaecological Association (EUGA)
Rights and permissions
About this article
Cite this article
Serati, M., Ruffolo, A.F., Scancarello, C. et al. When does oasis cause de novo pelvic floor dysfunction? role of the surgeon's skills. Int Urogynecol J 34, 493–498 (2023). https://doi.org/10.1007/s00192-022-05205-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-022-05205-6