Abstract
Introduction and hypothesis
Faecal incontinence can be a devastating outcome with social, psychological and physical repercussions, and it occurs in 10–61% following obstetric anal sphincter injury (OASIS). The aim of our study was to determine the contributing factors in the development of severity of OASIS and to correlate anal sphincter tone with the extent of anal sphincter injury.
Methods
A prospective cohort study was performed of all patients attending the postnatal perineal clinic at 4–12 months postpartum, from January 2016 until October 2017. Women were categorised into minor tears (3a and 3b) and major tears (3c and 4th degree).
Results
The mean age was 33.9 years (4.2); the mean parity was 1.6 (range 1–5). A total of 75 women (17%) were reviewed following a major tear (4th degree, n = 28, 3c, n = 47) and 362 (83%) were reviewed following a minor tear (3a n = 188, 3b, n = 174). Following analysis of numerous obstetric variables, it was shown that women who had an instrumental delivery were more likely to have a major tear compared with those who had a spontaneous vaginal delivery (p = 0.05). A significant difference was found in the distributions of symptom score between groups (p < 0.001). Women with combined defects were most likely to have reduced anal tone (p < 0.001) compared with any other group.
Conclusions
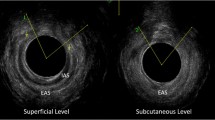
The perineal clinic provides a valuable resource for investigation and treatment of OASIS, providing a targeted pathway for management. We suggest that endoanal ultrasound and digital rectal examination are complimentary investigations which correlate well with each other.
Similar content being viewed by others
References
Harkin R, Fitzpatrick M, O'Connell PR, O'Herlihy C. Anal sphincter disruption at vaginal delivery: is recurrence predictable? Eur J Obstet Gynecol Reprod Biol. 2003;109:149–52.
Reid AJ, Beggs AD, Sultan AH, Roos A-M, Thakar R. Outcome of repair of obstetric anal sphincter injuries after three years. Int J Gynaecol Obstet. 2014;127(1):47–50.
Sultan AH, Thakar R. Third and fourth degree tears. In: Sultan AH, Thakar R, Fenner DE, editors. Perineal and anal sphincter trauma: diagnosis and clinical management. London: Springer; 2007. p. 33–51.
Jangö H, Langhoff-Roos J, Rosthøj S, Saske A. Long-term anal incontinence after obstetric anal sphincter injury-does grade of tear matter? Am J Obstet Gynecol. 2018;218(2):232.e1–232.e10.
Brubaker L, Handa VL, Bradley CS, Connolly A, Moalli P, Brown MB, et al. Sexual function 6 months after first delivery. Obstet Gynecol. 2008;111:1040–4.
Signorello LB, Harlow BL, Chekos AK, Repke JT. Postpartum sexual functioning and its relationship to perineal trauma: a retrospective cohort study of primiparous women. Am J Obstet Gynecol. 2001;184:881–8.
Fornell EU, Matthiesen L, Sjödahl R, Berg G. Obstetric anal sphincter injury ten years after: subjective and objective long term effects. BJOG. 2005;112(3):312–6.
Royal College of Obstetricians and Gynaecologists (RCOG). The management of third- and fourth-degree perineal tears. RCOG guideline 2015 (revised). RCOG Press; 2015.
Nichols CM, Lamb EH, Ramakrishnan V. Differences in outcomes after third- versus fourth-degree perineal laceration repair: a prospective study. Am J Obstet Gynecol. 2005;193(2):530–6.
Sangalli MR, Floris L, Falting D, Weil A. Anal incontinence in women with third or fourth degree perineal tears and subsequent vaginal deliveries. Aust N Z J Obstet Gynaecol. 2005;193:530–6.
De Leeuw JW, Vierhout ME, Struijk PC, Hop WC, Wallenburg HC. Anal sphincter damage after vaginal delivery: functional outcome and risk factors for fecal incontinence. Acta Obstet Gynecol Scand. 2001;80(9):830–4.
Norderval S, Nsubuga D, Bjelke C, Frasunek J, Myklebust I, Vonen B. Anal incontinence after obstetric sphincter tears: incidence in a Norwegian county. Acta Obstet Gynecol Scand. 2004;83:989–94.
Starck M, Bohe M, Valentin L. The extent of endosonographic anal sphincter defects after primary repair of obstetric sphincter tears increases over time and is related to anal incontinence. Ultrasound Obstet Gynecol. 2006;27:188–97.
Sultan AH. Obstetrical perineal injury and anal incontinence. Clin Risk. 1999;5:193–6.
Vaizey CJ, Caraped E, Cahill JA, Kamm MA. Prospective comparison of faecal incontinence grading systems. Gut. 1999;44(1):77–80.
Christianson LM, Bovbierg VE, McDavitt EC, Hullfish KL. Risk factors for perineal injury during delivery. Am J Obstet Gynecol. 2003;189(1):255–60.
Smith LA, Price N, Simonite V, Burns EE. Incidence of and risk factors for perineal trauma: a prospective observational study. BMC Pregnancy Childbirth. 2013;13:59.
Laine K, Pirhonen T, Rolland R, Pirhonene J. Decreasing the incidence of anal sphincter tears during delivery. Obstet Gynecol. 2008;111:1053–7.
Jangö H, Langhoff-Roos J, Rosthøj S, Sakse A. Modifiable risk factors of obstetric anal sphincter injury in primiparous women: a population-based cohort study. Am J Obstet Gynecol. 2014;210:59.
Hals E, Oian P, Pirhonen T, Gissler M, Hjelle S, Nilsen EB, et al. A multicenter interventional program to reduce the incidence of anal sphincter tears. Obstet Gynecol. 2010;116:901–8.
De Vogel J, van der Leeuw-van Beek A, Gietelink D, Vuijkovic M, de Leeuw JW, van Bavel J. The effect of a mediolateral episiotomy during operative vaginal delivery on the risk of developing obstetrical anal sphincter injuries. Am J Obstet Gynecol. 2012;206(5):404.
Borello-France D, Burgio KL, Richter HE, Zyczynski H, Fitzgerald MP, Whitehead W, et al. Fecal and urinary incontinence in primiparous women. Obstet Gynecol. 2006;108(4):863–72.
O’Shea MS, Lewicky-Gaupp C, Gossett DR. Long-term sexual function after obstetric anal sphincter injuries. Female Pelvic Med Reconstr Surg. 2018;24(2):82–6.
Albuquerque A. Endoanal ultrasonography in fecal incontinence: current and future perspectives. World J Gastrointest Endosc. 2015;7(6):575–81.
Wald A, Bharucha AE, Cosman BC, Whitehead WE. ACG clinical guideline: management of benign anorectal disorders. Am J Gastroenterol. 2014;109:1141–57.
Starck M, Bohe M, Valentin L. Results of endosonographic imaging of the anal sphincter 2–7 days after primary repair of third- or fourth-degree obstetric sphincter tears. Ultrasound Obstet Gynecol. 2003;22:609–15.
Norderval S, Mækskog A, Røssaak K, Vonen B. Correlation between anal sphincter defects and anal incontinence following obstetric sphincter tears assessment using scoring systems for sonographic classification of defects. Ultrasound Obstet Gynecol. 2008;31:78–84.
Dobben AC, Terra MP, Deutekom M, Gerhards MF, Bijnen AB, Felt-Bersma RJ, et al. Anal inspection and digital rectal examination compared to anorectal physiology tests and endoanal ultrasonography in evaluating fecal incontinence. Int J Color Dis. 2007;22:783–90.
Oberwalder M, Connor J, Wexner SD. Metanalysis to determine the incidence of obstetric anal sphincter damage. Br J Surg. 2003;90:1333–7.
Johnson JK, Lindow SW, Duthie GS. The prevalence of occult obstetric anal sphincter injury following childbirth—literature review. J Matern Fetal Neonatal Med. 2009:547–54.
Acknowledgements
This study describes original work and has not been submitted for consideration by any other journal. All authors have approved the manuscript and its submission. All authors have contributed substantially to obtaining and analysing data obtained for this study. All authors have had input both drafting and revision of the article and final approval of the version published.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Anglim, B., Kelly, L. & Fitzpatrick, M. Risk factors and outcome of repair of obstetric anal sphincter injuries as followed up in a dedicated perineal clinic. Int Urogynecol J 30, 1649–1655 (2019). https://doi.org/10.1007/s00192-019-03960-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-03960-7


