Abstract
Introduction and hypothesis
This segment of Chapter 1 of the International Urogynecology Consultation (IUC) on pelvic organ prolapse (POP) reviews the literature on the clinical definition of POP with the intent of creating standard terminology.
Methods
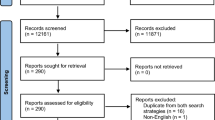
An international group containing nine urogynecologists and one university-based medical librarian performed a search of the literature using pre-specified search terms in PubMed, Embase, and Scopus. Publications were eliminated if not relevant to the clinical definition of POP, and those articles remaining were evaluated for quality using the Specialist Unit for Review Evidence (SURE). The resulting list of articles was used to inform a comprehensive review and creation of the clinical definition of POP.
Results
The original search yielded 31,931 references, of which 167 were used by the writing group. Ultimately, 78 are referenced in the manuscript.
Conclusions
The clinical definition of POP for this review of the literature is: “anatomical prolapse with descent of at least one of the vaginal walls to or beyond the vaginal hymen with maximal Valsalva effort WITH the presence either of bothersome characteristic symptoms, most commonly the sensation of vaginal bulge, or of functional or medical compromise due to prolapse without symptom bother.”



Similar content being viewed by others
Abbreviations
- AUGS:
-
American Urogynecologic Society
- ICS:
-
International Continence Society
- IUC:
-
International Urogynecological Consultation
- IUGA:
-
International Urogynecological Association
- POP:
-
Pelvic organ prolapse
- POP-Q:
-
Pelvic Organ Prolapse Quantification system
- SGS:
-
Society for Gynecologic Surgeons
References
Wu JM, Matthews CA, Conover MM, Pate V, Jonsson Funk M. Lifetime risk of stress urinary incontinence or pelvic organ prolapse surgery. Obstet Gynecol. 2014;123(6):1201–6. https://doi.org/10.1097/AOG.0000000000000286.
Wu JM, Ward RM, Allen-Brady KL, Edwards TL, Norton PA, Hartmann KE, et al. Phenotyping clinical disorders: lessons learned from pelvic organ prolapse. Am J Obstet Gynecol. 2013;208(5):360–5. https://doi.org/10.1016/j.ajog.2012.11.030.
Haylen BT, de Ridder D, Freeman RM, Swift SE, Berghmans B, Lee J, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Int Urogynecol J. 2010;21(1):5–26. https://doi.org/10.1007/s00192-009-0976-9.
Swift S, Woodman P, O’Boyle A, Kahn M, Valley M, Bland D, et al. Pelvic organ support study (POSST): the distribution, clinical definition, and epidemiologic condition of pelvic organ support defects. Am J Obstet Gynecol. 2005;192(3):795–806. https://doi.org/10.1016/j.ajog.2004.10.602.
Fitzgerald MP, Janz NK, Wren PA, Wei JT, Weber AM, Ghetti C, et al. Prolapse severity, symptoms and impact on quality of life among women planning sacrocolpopexy. Int J Gynaecol Obstet. 2007;98(1):24–8. https://doi.org/10.1016/j.ijgo.2007.03.018.
Ellerkmann RM, Cundiff GW, Melick CF, Nihira MA, Leffler K, Bent AE. Correlation of symptoms with location and severity of pelvic organ prolapse. Am J Obstet Gynecol. 2001;185(6):1332–7; discussion 1337–1338. https://doi.org/10.1067/mob.2001.119078.
Dooley YT, West K, Kenton K, Fitzgerald MP, Brubaker L. Bowel symptoms and POP-Q stage are poorly correlated. J Pelvic Med Surg. 2006;12(5):263–6. https://doi.org/10.1097/01.spv.0000243743.28791.21.
Cunkelman J, Mueller E, Brubaker L, Kenton K. Defining pelvic organ prolapse: correlation of symptoms with vaginal topography. Neurourol Urodyn. 2011;30(6):1046–8. https://doi.org/10.1002/nau.21185.
Swift SE, Tate SB, Nicholas J. Correlation of symptoms with degree of pelvic organ support in a general population of women: what is pelvic organ prolapse? Am J Obstet Gynecol. 2003;189(2):372–7; discussion 377–379. https://doi.org/10.1067/s0002-9378(03)00698-7.
Cardiff University Specialist Unit for Review Evidence. http://www.cardiff.ac.uk/specialist-unit-for-review-evidence/resources/critical-appraisal-checklists. Accessed 28 August 2020
Porges RF. A practical system of diagnosis and classification of pelvic relaxations. Surg Gynecol Obstet. 1963;117:769–73.
Baden WF, Walker TA. Physical diagnosis in the evaluation of vaginal relaxation. Clin Obstet Gynecol. 1972;15(4):1055–69. https://doi.org/10.1097/00003081-197212000-00021.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7. https://doi.org/10.1016/s0002-9378(96)70243-0.
Hall AF, Theofrastous JP, Cundiff GW, Harris RL, Hamilton LF, Swift SE, et al. Interobserver and intraobserver reliability of the proposed International Continence Society, Society of Gynecologic Surgeons, and American Urogynecologic Society pelvic organ prolapse classification system. Am J Obstet Gynecol. 1996;175(6):1467–70; discussion 1470–1461. https://doi.org/10.1016/s0002-9378(96)70091-1.
Kobak WH, Rosenberger K, Walters MD. Interobserver variation in the assessment of pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 1996;7(3):121–4. https://doi.org/10.1007/BF01894199.
Muir TW, Stepp KJ, Barber MD. Adoption of the pelvic organ prolapse quantification system in peer-reviewed literature. Am J Obstet Gynecol. 2003;189(6):1632–5; discussion 1635–1636. https://doi.org/10.1016/j.ajog.2003.09.010.
Treszezamsky AD, Rascoff L, Shahryarinejad A, Vardy MD. Use of pelvic organ prolapse staging systems in published articles of selected specialized journals. Int Urogynecol J. 2010;21(3):359–63. https://doi.org/10.1007/s00192-009-1044-1.
Committee on Practice Bulletins—Gynecology, American Urogynecologic Society. Practice bulletin no. 176: pelvic organ prolapse. Obstet Gynecol. 2017;129(4):e56–72. https://doi.org/10.1097/AOG.0000000000002016.
Auwad W, Freeman RM, Swift S. Is the pelvic organ prolapse quantification system (POPQ) being used? A survey of members of the International Continence Society (ICS) and the American Urogynecologic Society (AUGS). Int Urogynecol J Pelvic Floor Dysfunct. 2004;15(5):324–7. https://doi.org/10.1007/s00192-004-1175-3.
Patnam R, Edenfield A, Swift S. Defining normal apical vaginal support: a relook at the POSST study. Int Urogynecol J. 2019;30(1):47–51. https://doi.org/10.1007/s00192-018-3681-8.
Trutnovsky G, Robledo KP, Shek KL, Dietz HP. Definition of apical descent in women with and without previous hysterectomy: a retrospective analysis. PLoS One. 2019;14(3):e0213617. https://doi.org/10.1371/journal.pone.0213617.
Dietz HP, Mann KP. What is clinically relevant prolapse? An attempt at defining cutoffs for the clinical assessment of pelvic organ descent. Int Urogynecol J. 2014;25(4):451–5. https://doi.org/10.1007/s00192-013-2307-4.
Gutman RE, Ford DE, Quiroz LH, Shippey SH, Handa VL. Is there a pelvic organ prolapse threshold that predicts pelvic floor symptoms? Am J Obstet Gynecol 2008;199(6):683.e1–7. doi:https://doi.org/10.1016/j.ajog.2008.07.028
Ghetti C, Gregory WT, Edwards SR, Otto LN, Clark AL. Pelvic organ descent and symptoms of pelvic floor disorders. Am J Obstet Gynecol. 2005;193(1):53–7. https://doi.org/10.1016/j.ajog.2004.12.004.
Weber AM, Abrams P, Brubaker L, Cundiff G, Davis G, Dmochowski RR, et al. The standardization of terminology for researchers in female pelvic floor disorders. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12(3):178–86.
Barber MD, Brubaker L, Nygaard I, Wheeler ITL, Schaffer J, Chen Z, et al. Defining success after surgery for pelvic organ prolapse. Obstet Gynecol. 2009;114(3):600–9. https://doi.org/10.1097/AOG.0b013e3181b2b1ae.
Shek KLDH. Imaging of slings and meshes. Australas J Ultrasound Med. 2014;17(2):61–71.
Stone DEQL. Ultrasound imaging of the pelvic floor. Obstet Gynecol Clin N Am. 2016;43:141–53.
ACR, AUGS, AUA, SRU. AIUM/IUGA practice parameter for the performance of urogynecological ultrasound examinations: developed in collaboration with the ACR, the AUGS, the AUA, and the SRU. J Ultrasound Med. 2019;38:851–64.
Timor-Tritsch IE, Monteagudo A, Smilen SW, Porges RF, Avizova E. Simple ultrasound evaluation of the anal sphincter in female patients using a transvaginal transducer. Ultrasound Obstet Gynecol. 2005;25(2):177–83.
Dietz H, Kamisan Atan I, Salita A. Association between ICS POP-Q coordinates and translabial ultrasound findings: implications for definition of ‘normal pelvic organ support’. Ultrasound Obstet Gynecol. 2016;47(3):363–8.
Dietz HP. Pelvic floor ultrasound: a review. Clin Obstet Gynecol. 2017;60(1):58–81. https://doi.org/10.1097/GRF.0000000000000264.
Guzman Rojas R, Atan IK, Shek KL, Dietz HP. The prevalence of abnormal posterior compartment anatomy and its association with obstructed defecation symptoms in urogynecological patients. Int J Urogynecol. 2016;27(6):939–944. https://doi.org/10.1097/GRF.0000000000000264
Dietz HP, Steensma AB. Posterior compartment prolapse on two-dimensional and three-dimensional pelvic floor ultrasound: the distinction between true rectocele, perineal hypermobility and enterocele. Ultrasound Obstet Gynecol 2005;26(1):73–7.
De Almeida FG, Rodriguez LV, Raz S. Magnetic resonance imaging in the diagnosis of pelvic floor disorders. Int Braz J Urol. 2002;28(6):553–9.
Kobi M, Flusberg M, Paroder V, Chernyak V. Practical guide to dynamic pelvic floor MRI. J Magnetic Resonance Imaging. 2018;47(5):1155–70. https://doi.org/10.1002/jmri.25998.
Woodfield CA, Krishnamoorthy S, Hampton BS, Brody JM. Imaging pelvic floor disorders: trend toward comprehensive MRI. AJR Am J Roentgenol. 2010;194(6):1640–9. https://doi.org/10.2214/AJR.09.3670.
El Sayed RF, Alt CD, Maccioni F, Meissnitzer M, Masselli G, Manganaro L, et al. Magnetic resonance imaging of pelvic floor dysfunction—joint recommendations of the ESUR and ESGAR pelvic floor working group. Eur Radiol. 2017;27(5):2067–85. https://doi.org/10.1007/s00330-016-4471-7.
Broekhuis SR, Futterer JJ, Barentsz JO, Vierhout ME, Kluivers KB. A systematic review of clinical studies on dynamic magnetic resonance imaging of pelvic organ prolapse: the use of reference lines and anatomical landmarks. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(6):721–9. https://doi.org/10.1007/s00192-009-0848-3.
Singh K, Reid WM, Berger LA. Assessment and grading of pelvic organ prolapse by use of dynamic magnetic resonance imaging. Am J Obstet Gynecol. 2001;185(1):71–7. https://doi.org/10.1067/mob.2001.113876.
Broekhuis SR, Kluivers KB, Hendriks JC, Futterer JJ, Barentsz JO, Vierhout ME. POP-Q, dynamic MR imaging, and perineal ultrasonography: do they agree in the quantification of female pelvic organ prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(5):541–9. https://doi.org/10.1007/s00192-009-0821-1.
Woodfield CA, Hampton BS, Sung V, Brody JM. Magnetic resonance imaging of pelvic organ prolapse: comparing pubococcygeal and midpubic lines with clinical staging. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(6):695–701. https://doi.org/10.1007/s00192-009-0865-2.
Gupta S, Sharma JB, Hari S, Kumar S, Roy KK, Singh N. Study of dynamic magnetic resonance imaging in diagnosis of pelvic organ prolapse. Arch Gynecol Obstet. 2012;286(4):953–8. https://doi.org/10.1007/s00404-012-2381-8.
Fauconnier A, Zareski E, Abichedid J, Bader G, Falissard B, Fritel X. Dynamic magnetic resonance imaging for grading pelvic organ prolapse according to the international continence society classification: which line should be used? Neurourol Urodyn. 2008;27(3):191–7. https://doi.org/10.1002/nau.20491.
Lakeman MM, Zijta FM, Peringa J, Nederveen AJ, Stoker J, Roovers JP. Dynamic magnetic resonance imaging to quantify pelvic organ prolapse: reliability of assessment and correlation with clinical findings and pelvic floor symptoms. Int Urogynecol J. 2012;23(11):1547–54. https://doi.org/10.1007/s00192-012-1772-5.
Pannu HK, Scatarige JC, Eng J. MRI diagnosis of pelvic organ prolapse compared with clinical examination. Acad Radiol. 2011;18(10):1245–51. https://doi.org/10.1016/j.acra.2011.05.010.
Faccioli N, Comai A, Mainardi P, Perandini S, Moore F, Pozzi-Mucelli R. Defecography: a practical approach. Diagn Interv Radiol. 2010;16(3):209–16. https://doi.org/10.4261/1305-3825.DIR.2584-09.1.
Lienemann A, Anthuber C, Baron A, Reiser M. Diagnosing enteroceles using dynamic magnetic resonance imaging. Dis Colon Rectum. 2000;43(2):205–12; discussion 212–203. https://doi.org/10.1007/BF02236984.
Kelvin FM, Maglinte DD, Hale DS, Benson JT. Female pelvic organ prolapse: a comparison of triphasic dynamic MR imaging and triphasic fluoroscopic cystocolpoproctography. AJR Am J Roentgenol. 2000;174(1):81–8. https://doi.org/10.2214/ajr.174.1.1740081.
Altman D, Lopez A, Kierkegaard J, Zetterstrom J, Falconer C, Pollack J, et al. Assessment of posterior vaginal wall prolapse: comparison of physical findings to cystodefecoperitoneography. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(2):96–103; discussion 103. https://doi.org/10.1007/s00192-004-1220-2.
Groenendijk AG, van der Hulst VP, Birnie E, Bonsel GJ. Correlation between posterior vaginal wall defects assessed by clinical examination and by defecography. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(9):1291–7. https://doi.org/10.1007/s00192-008-0632-9.
Lienemann A, Anthuber C, Baron A, Kohz P, Reiser M. Dynamic MR colpocystorectography assessing pelvic-floor descent. Eur Radiol. 1997;7(8):1309–17. https://doi.org/10.1007/s003300050294.
Kelvin F, Maglinte D, Hornback J, Benson J. Pelvic prolapse: assessment with evacuation proctography (defecography). Radiology. 1992;184(2):547–51.
Kelvin FM, Hale DS, Maglinte DD, Patten BJ, Benson JT. Female pelvic organ prolapse: diagnostic contribution of dynamic cystoproctography and comparison with physical examination. AJR Am J Roentgenol. 1999;173(1):31–7. https://doi.org/10.2214/ajr.173.1.10397095.
Kenton K, Shott S, Brubaker L. Vaginal topography does not correlate well with visceral position in women with pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 1997;8(6):336–9. https://doi.org/10.1007/BF02765592.
Altman D, Mellgren A, Kierkegaard J, Zetterstrom J, Falconer C, Lopez A. Diagnosis of cystocele—the correlation between clinical and radiological evaluation. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15(1):3–9; discussion 9. https://doi.org/10.1007/s00192-003-1111-y.
Sung VW, Rogers RG, Barber MD, Clark MA. Conceptual framework for patient-important treatment outcomes for pelvic organ prolapse. Neurourol Urodyn. 2014;33(4):414–9. https://doi.org/10.1002/nau.22397.
Dubowitch E, Cahn D, Ross C, Husain A, Harkaway R, Metro M, et al. Procidentia as a cause of obstructive Uropathy and acute kidney injury. Curr Urol. 2014;7(4):207–9. https://doi.org/10.1159/000365678.
Siddique M, Ingraham C, Kudish B, Iglesia CB, Polland A. Hydronephrosis associated with pelvic organ prolapse: a systematic review. Female Pelvic Med Reconstr Surg. 2019;26(3):212–8. https://doi.org/10.1097/spv.0000000000000683.
Norton P, Brubaker L, Nager CW, Lemack GE, Zyczynski HM, Sirls L, et al. Pelvic organ prolapse in a cohort of women treated for stress urinary incontinence. Am J Obstet Gynecol. 2014;211(5):550.e1–55. doi:https://doi.org/10.1016/j.ajog.2014.07.053
Tan JS, Lukacz ES, Menefee SA, Powell CR, Nager CW, San Diego Pelvic Floor Consortium. Predictive value of prolapse symptoms: a large database study. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(3):203–9; discussion 209. https://doi.org/10.1007/s00192-004-1243-8.
Dixon AM, Fitzgerald CM, Brincat C. Severity and bother of prolapse symptoms in women with pelvic floor myofascial pain. Int Urogynecol J. 2019;30(11):1829–34. https://doi.org/10.1007/s00192-019-03916-x.
Manonai J, Wattanayingcharoenchai R. Relationship between pelvic floor symptoms and POP-Q measurements. Neurourol Urodyn. 2016;35(6):724–7. https://doi.org/10.1002/nau.22786.
Dietz H, Martin A. What is ‘significant’ pelvic organ prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2013;24:S65–6. https://doi.org/10.1007/s00192-013-2101-3.
Ghetti C, Skoczylas LC, Oliphant SS, Nikolajski C, Lowder JL. The emotional burden of pelvic organ prolapse in women seeking treatment: a qualitative study. Female Pelvic Med Reconstr Surg. 2015;21(6):332–8. https://doi.org/10.1097/spv.0000000000000190.
Schimpf MO, Sullivan DM, LaSala CA, Tulikangas PK. Anterior vaginal wall prolapse and voiding dysfunction in urogynecology patients. Int Urogynecol J. 2007;18(7):721–5. https://doi.org/10.1007/s00192-006-0227-2.
Dancz CE, Ozel B. Is there a pelvic organ prolapse threshold that predicts bladder outflow obstruction? Int Urogynecol J. 2011;22(7):863–8. https://doi.org/10.1007/s00192-011-1373-8.
Dietz HP, Shek KL, Chan S, Guzman Rojas R. Pelvic floor ultrasound: basic settings and procedures. https://www.iuga.org/files/55/Pelvic-Floor-Imaging/124/Pelvic-Floor-Ultrasound.pdf. Accessed August 2020
Dietz HP, Haylen BT, Vancaillie TG. Female pelvic organ prolapse and voiding function. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13(5):284–8. https://doi.org/10.1007/s001920200062.
Jelovsek JE, Walters MD, Paraiso MF, Barber MD. Functional bowel disorders and pelvic organ prolapse: a case-control study. Female Pelvic Med Reconstr Surg. 2010;16(4):209–14. https://doi.org/10.1097/SPV.0b013e3181e4f270.
Morgan DM, DeLancey JO, Guire KE, Fenner DE. Symptoms of anal incontinence and difficult defecation among women with prolapse and a matched control cohort. Am J Obstet Gynecol. 2007;197(5):509.e1–6. doi:https://doi.org/10.1016/j.ajog.2007.03.074
Weber AM, Walters MD, Schover LR, Mitchinson A. Sexual function in women with uterovaginal prolapse and urinary incontinence. Obstet Gynecol. 1995;85(4):483–7. https://doi.org/10.1016/0029-7844(94)00434-F.
Barber MD, Visco AG, Wyman JF, Fantl JA, Bump RC, Continence Program for Women Research Group. Sexual function in women with urinary incontinence and pelvic organ prolapse. Obstet Gynecol. 2002;99(2):281–9. https://doi.org/10.1016/s0029-7844(01)01727-6.
Moroni RM, Alves da Silva Lara L, Ferreira CHJ, de Mello Constantino M, Oliveira Brito LG. Assessment of body image, sexual function, and attractiveness in women with genital prolapse: a cross-sectional study with validation of the body image in the pelvic organ prolapse (BIPOP) questionnaire. J Sex Med. 2019;16(1):126–36. https://doi.org/10.1016/j.jsxm.2018.11.005.
Roos AM, Thakar R, Sultan AH, Burger CW, Paulus AT. Pelvic floor dysfunction: women’s sexual concerns unraveled. J Sex Med. 2014;11(3):743–52. https://doi.org/10.1111/jsm.12070.
Roos AM, Thakar R, Sultan AH, de Leeuw JW, Paulus AT. The impact of pelvic floor surgery on female sexual function: a mixed quantitative and qualitative study. BJOG. 2014;121(1):92–100; discussion 101. https://doi.org/10.1111/1471-0528.12412.
Shek KL, Dietz HP. What is abnormal uterine descent on translabial ultrasound? Int Urogynecol J. 2015;26(12):1783–7.
Author information
Authors and Affiliations
Contributions
S.A. Collins: Writing Group Committee Co-Chair, primary writer and editor of the manuscript; M. O’Shea: literature search, writing, editing; N. Dykes: literature search, writing, editing; O. Ramm: literature search, writing, editing; A.E. Edenfield: literature search, writing, editing; K.L. Shek: literature search, writing, editing; K. van Delft: literature search, writing, editing; M. Beestrum: coordinated the large-scale literature search and facilitated group review of the references; K. Kenton: Writing Group Committee Co-chair, writing, editing.
Corresponding author
Ethics declarations
Financial disclaimers/conflicts of interest
S.A. Collins, O. Ramm, and K. Kenton are expert witnesses for Ethicon/Johnson & Johnson. S.A. Collins is a paid content expert for MCG, a clearinghouse for medical care guidelines; K.L. Shek receives unrestricted educational grants from Mindray and GE. The remaining authors claim that they have no conflicts of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Collins, S.A., O’Shea, M., Dykes, N. et al. International Urogynecological Consultation: clinical definition of pelvic organ prolapse. Int Urogynecol J 32, 2011–2019 (2021). https://doi.org/10.1007/s00192-021-04875-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04875-y