Abstract
Introduction and hypothesis
The effect of incontinence pessaries for urine incontinence (UI) has previously been described in studies from high-income countries, where they have been documented to reduce urinary leakage significantly. However, there is a profound literature gap in these data in low- and middle-income countries. This study, therefore, aims to describe the acceptance, impact and complications of pessary treatment among Tanzanian women diagnosed with stress UI.
Methods
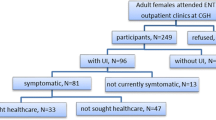
Women who reported stress UI underwent a stress test, and if positive they were offered an incontinence pessary. Swahili versions of the Urinary Distress Inventory-6 (UDI-6) and the Urinary Impact Questionnaire (UIQ) were administered at 3- and 12–18-month follow-ups in addition to questions regarding pessary acceptance and pelvic examination for complications.
Results
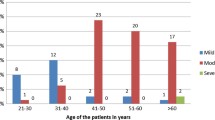
A total of 48 women were fitted with an incontinence pessary. The frequency and amount of leakage were reduced significantly at 3- and 12–18-month follow-up. Additionally, a significant reduction in the overall UDI-6 score from 29.2 to 25.0 and overall UIQ score from 52.1 to 25.0 was observed from baseline to 3-month follow-up. Thirty-seven per cent of the women reported vaginal discharge at 12–18 months while signs of infection were found in 11.5%. In all, 32/48 (67%) wanted to continue the pessary treatment at 12–18-month follow-up.
Conclusions
In the setting studied, pessaries for stress UI can be successfully fitted in most women with considerable acceptance and satisfaction rates and minimal complications.


Similar content being viewed by others
References
Walker GJ, Gunasekera P. Pelvic organ prolapse and incontinence in developing countries: review of prevalence and risk factors. Int Urogynecol J. 2011;22(2):127–35. https://doi.org/10.1007/s00192-010-1215-0.
Masenga GG, Shayo BC, Msuya S, Rasch V. Urinary incontinence and its relation to delivery circumstances: a population-based study from rural Kilimanjaro, Tanzania. PLoS One. 2019;14(1):e0208733. https://doi.org/10.1371/journal.pone.0208733.
Megabiaw B, Adefris M, Rortveit G, Degu G, Muleta M, Blystad A, et al. Pelvic floor disorders among women in Dabat district, Northwest Ethiopia: a pilot study. Int Urogynecol J. 2013;24(7):1135–43. https://doi.org/10.1007/s00192-012-1981-y.
Jokhio AH, Rizvi RM, Rizvi J, Macarthur C. Urinary incontinence in women in rural Pakistan: prevalence, severity, associated factors and impact on life. BJOG Int J Obstet Gynaecol. 2013;120(2):180–6. https://doi.org/10.1111/1471-0528.12074.
Obioha KC, Ugwu EO, Obi SN, Dim CC, Oguanuo TC. Prevalence and predictors of urinary/anal incontinence after vaginal delivery: prospective study of Nigerian women. Int Urogynecol J. 2015;26(9):1347–54. https://doi.org/10.1007/s00192-015-2690-0.
Teunissen D, Van Den Bosch W, Van Weel C, Lagro-Janssen T. “It can always happen”: the impact of urinary incontinence on elderly men and women. Scand J Prim Health Care. 2006;24(3):166–73. https://doi.org/10.1080/02813430600739371.
Gjerde JL, Rortveit G, Muleta M, Blystad A. Silently waiting to heal: experiences among women living with urinary incontinence in Northwest Ethiopia. Int Urogynecol J. 2013;24(6):953–8. https://doi.org/10.1007/s00192-012-1951-4.
Robert M, Schulz JA, Harvey MA. Technical update on pessary use. Journal of obstetrics and gynaecology Canada : JOGC = Journal d'obstetrique et gynecologie du Canada : JOGC. 2013;35(7):664–74. https://doi.org/10.1016/s1701-2163(15)30888-4.
Farrell SA, Baydock S, Amir B, Fanning C. Effectiveness of a new self-positioning pessary for the management of urinary incontinence in women. Am J Obstet Gynecol. 2007;196(5):474.e471–8. https://doi.org/10.1016/j.ajog.2006.11.038.
Jones KA, Harmanli O. Pessary use in pelvic organ prolapse and urinary incontinence. Rev Obstet Gynecol. 2010;3(1):3–9.
Komesu YM, Rogers RG, Rode MA, Craig EC, Gallegos KA, Montoya AR, et al. Pelvic floor symptom changes in pessary users. Am J Obstet Gynecol. 2007;197(6):620.e621–6. https://doi.org/10.1016/j.ajog.2007.08.013.
Donnelly MJ, Powell-Morgan S, Olsen AL, Nygaard IE. Vaginal pessaries for the management of stress and mixed urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15(5):302–7. https://doi.org/10.1007/s00192-004-1163-7.
Barber MD, Walters MD, Bump RC. Short forms of two condition-specific quality-of-life questionnaires for women with pelvic floor disorders (PFDI-20 and PFIQ-7). Am J Obstet Gynecol. 2005;193(1):103–13. https://doi.org/10.1016/j.ajog.2004.12.025.
Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. 1993;46(12):1417–32.
Robert M, Mainprize TC. Long-term assessment of the incontinence ring pessary for the treatment of stress incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2002;13(5):326–9. https://doi.org/10.1007/s001920200070.
Richter HE, Burgio KL, Brubaker L, Nygaard IE, Ye W, Weidner A, et al. Continence pessary compared with behavioral therapy or combined therapy for stress incontinence: a randomized controlled trial. Obstet Gynecol. 2010;115(3):609–17. https://doi.org/10.1097/AOG.0b013e3181d055d4.
Ko PC, Lo TS, Tseng LH, Lin YH, Liang CC, Lee SJ. Use of a pessary in treatment of pelvic organ prolapse: quality of life, compliance, and failure at 1-year follow-up. J Minim Invasive Gynecol. 2011;18(1):68–74. https://doi.org/10.1016/j.jmig.2010.09.006.
Clemons JL, Aguilar VC, Tillinghast TA, Jackson ND, Myers DL. Patient satisfaction and changes in prolapse and urinary symptoms in women who were fitted successfully with a pessary for pelvic organ prolapse. Am J Obstet Gynecol. 2004;190(4):1025–9. https://doi.org/10.1016/j.ajog.2003.10.711.
Fernando RJ, Thakar R, Sultan AH, Shah SM, Jones PW. Effect of vaginal pessaries on symptoms associated with pelvic organ prolapse. Obstet Gynecol. 2006;108(1):93–9. https://doi.org/10.1097/01.AOG.0000222903.38684.cc.
Bai SW, Yoon BS, Kwon JY, Shin JS, Kim SK, Park KH. Survey of the characteristics and satisfaction degree of the patients using a pessary. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(3):182–6; discussion 186. https://doi.org/10.1007/s00192-004-1226-9.
Hanson LA, Schulz JA, Flood CG, Cooley B, Tam F. Vaginal pessaries in managing women with pelvic organ prolapse and urinary incontinence: patient characteristics and factors contributing to success. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17(2):155–9. https://doi.org/10.1007/s00192-005-1362-x.
Alnaif B, Drutz HP. Bacterial vaginosis increases in pessary users. Int Urogynecol J Pelvic Floor Dysfunct. 2000;11(4):219–22 discussion 222-213.
Abed H, Rogers RG. Urinary incontinence and pelvic organ prolapse: diagnosis and treatment for the primary care physician. Med Clin N Am. 2008;92(5):1273–93, xii. https://doi.org/10.1016/j.mcna.2008.04.004.
Sarma S, Ying T, Moore KH. Long-term vaginal ring pessary use: discontinuation rates and adverse events. BJOG Int J Obstet Gynaecol. 2009;116(13):1715–21. https://doi.org/10.1111/j.1471-0528.2009.02380.x.
Wheeler LD, Lazarus R, Torkington J, O'Mahony MS, Woodhouse KW. Lesson of the week: perils of pessaries. Age Ageing. 2004;33(5):510–1. https://doi.org/10.1093/ageing/afh170.
Acknowledgements
We appreciate the work done by the retired nurses as field assistants in administering the questionnaires to the women.
Funding
This research was conducted under the auspices of the Building Stronger University (BSU) initiative, which is funded by DANIDA (the Danish International Development Agency). CooperSurgical, Inc., provided the Milex® Pessaries. The funders had no role in the study design, data collection and analysis, manuscript preparation or decision to publish.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Details of ethics approval
Clearance was obtained from the Kilimanjaro Christian Medical University College’s Clinical Research Ethics Review Committee in February 2015 and given research ethical clearance certificate number 811.
Conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Shayo, B.C., Mwakanyamale, D.J., Masenga, G.G. et al. Management of stress urinary incontinence using vaginal incontinence pessaries in rural Kilimanjaro, Tanzania. Int Urogynecol J 31, 1091–1097 (2020). https://doi.org/10.1007/s00192-019-03980-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-019-03980-3