Abstract
Purpose
Previous studies comparing high tibial osteotomy (HTO) with unicompartmental knee arthroplasty (UKA) have seldom accounted for differing patient characteristics between both groups. This study compared patient-reported outcomes (PROs) of HTO and UKA patients, adjusted for preoperative PROs, osteoarthritis grade and sex.
Methods
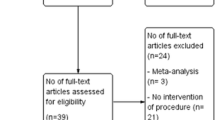
A retrospective study was performed analysing prospectively collected PROs, namely the Oxford Knee Score (OKS) and pain/satisfaction scores, collected preoperatively and at 6 months, 12 months and 24 months postoperatively. Consecutive medial opening-wedge HTOs and medial UKAs from 2016–2019, with a preoperative Kellgren–Lawrence grade ≥ 3, aged 50–60 years, were included. Linear mixed model analyses, with the OKS over time as the primary outcome, were used.
Results
We included 84 HTO patients (mean age 55.0 ± 3.0, 79% male, mean BMI 27.8 ± 3.4, 75% Kellgren–Lawrence grade 3) and 130 UKA patients (mean age 55.7 ± 2.8, 47% male, mean BMI 28.7 ± 4.0, 36% Kellgren–Lawrence grade 3). Response rates were ≥ 87% at all time points. Corrected for preoperative PROs, Kellgren–Lawrence grade and sex, the HTO group had a 2.5 (95% CI 1.0–4.0) points lower OKS over time than the UKA group (p = 0.001). The Numeric Rating Scale scores (NRS; 0–10) for pain at rest and during activity were higher (p < 0.01) in the HTO group. The EQ-5D-descriptive system (p < 0.01), NRS satisfaction (p < 0.01), anchor function and pain scores (p < 0.01) were lower over time in the HTO group.
Conclusion
UKA patients had better OKS scores, pain and satisfaction scores over time than HTO patients. However, the observed differences were below their established minimal clinically important differences. Therefore, from the patients’ perspective, HTO did not appear to be inferior to UKA under the indications outlined in this study.
Level of evidence Level IV.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
For relatively young patients (50–60 years of age) with debilitating medial unicompartmental knee osteoarthritis (OA), high tibial osteotomy (HTO) and medial unicompartmental knee arthroplasty (UKA) are suitable surgical treatment options [26]. To date, more reviews and meta-analyses than randomized, prospective studies have been published on the topic of HTO versus UKA [2, 4, 6, 11, 14, 28, 34, 37]. Overall, UKA appears to result in better outcomes regarding pain relief and satisfaction, while range-of-motion seems higher after HTO.
Interestingly, previous studies have seldom elaborated on the effect of the preoperative indication, including preoperative OA grade, on the outcome of HTO or UKA [6]. Yet, valgus-producing HTO is most often advised for patients aged 40–60 years, with an extra-articular tibial varus deformity, who are non-smokers, with a body mass index (BMI) < 30 kg/m2 and mild-to-moderate medial compartment OA. Although, among others, the UK Knee Osteotomy Consensus Group recently stated that bone-on-bone OA should not be considered a strict contraindication for HTO [5, 26, 35]. In contrast, UKA is primarily indicated in patients aged > 60 years, without BMI restrictions, for treatment of anteromedial osteoarthritis (AMOA). For AMOA, the Oxford criteria apply and medial compartment bone-on-bone OA is a strict prerequisite [13, 30]. Performing UKA in patients without bone-on-bone medial OA results in worse patient-reported outcomes (PROs), and higher rates of reoperation and revision [12, 27, 29]. These criteria show that indications, including preoperative OA grade, for HTO and UKA only partly overlap. This could be the reason that only two randomized studies of suboptimal methodological quality have reported results for HTO versus UKA [4, 37]. These studies used outdated inclusion criteria, i.e. Ahlbäck OA grade I–III for both procedures, did not perform a power analysis, and included relatively small samples.
Thus, from a patients’ perspective it remains unclear if patients in the age range 50–60 years with moderate-to-severe medial OA benefit more from one of these procedures. Several reviews noted that future prospective, preferably randomized studies, are needed to define true differences between both procedures. To allow for a true comparison between HTO and UKA, one should compare patients who could have been indicated for both procedures based on their preoperative characteristics, including the preoperative radiographic OA severity. Also, other patient and surgeon factors, e.g. the wish to participate in high-impact activities, play a role in decision-making in younger, active patients.
Therefore, the aim of the present study was to retrospectively compare HTO and UKA on prospectively collected PROs during the first two years after surgery in comparable patients, based on preoperative characteristics including OA grade and sex. The hypothesis was that HTO would result in similar PROs compared to UKA in this selected population.
Materials and methods
Study design and patient selection
A single-centre retrospective study with prospectively collected data of consecutive non-randomized HTO and UKA patients operated on by dedicated knee surgeons between January 2016 and December 2019 in a high-volume clinic was performed. Guidelines of the Dutch Health Regulatory Agency state that patients with an American Society of Anesthesiologists (ASA) score > II and a BMI > 35 kg/m2 are not allowed to be operated on in the present study’s clinic. Therefore, all patients in the present study had an ASA score of I–II and a BMI < 35 kg/m2.
Eligible patients had medial OA Kellgren–Lawrence grade (KL grade) ≥ 3, were aged between 50 and 60 years, provided a signed informed consent, and underwent HTO or UKA. Patients who were operated on both knees were included in this prospective database if their second surgery was > 6 months after the first surgery (n = 6). Exclusion criteria included OA in more than one compartment, a preoperative radiograph of insufficient quality, and double level (i.e. tibia and femur) osteotomies. The KL grade was determined by two independent researchers on regular preoperative standing AP knee radiographs and on stress radiographs if available [22]. KL grade 4 was assigned in cases with medial bone-on-bone. Discrepancies were resolved by discussion.
Surgical technique
For HTO, a medial opening-wedge technique with biplanar osteotomy was performed [15]. Plate fixation in all patients was performed with angular stable plates (TomoFix, Synthes GmbH, Switzerland). No grafts were used. Postoperatively, immediate range-of-motion exercises and muscle strengthening were started with guidance from a physical therapist. All patients were allowed full weight-bearing from 2 weeks postoperatively.
For UKA, standard surgical technique was performed as described by the manufacturer. Either a fixed bearing implant, the Physica ZUK UKA (LIMA Corporate UD, Italy) or a mobile bearing implant, the cementless Phase III Oxford UKA (ZimmerBiomet Ltd., Bridgend, UK) was used. All patients were allowed direct full weight-bearing postoperatively.
The preferred treatment option was selected based on surgeon and patient preference (Table 1; Figs. 1 and 2).
Clinical case of female, 54 years, left knee; Kellgren–Lawrence grade 3–4, tibial bone varus angle (TBVA) shows extra-articular deformity; HTO preferred by patient because of high physical demands (A preoperative X-ray + TBVA measurement [3], B preoperative stress X-ray, C postoperative X-ray)
Outcomes and measures
The primary outcome was the change in Oxford Knee Score (OKS) over time (from preoperative to 24 months postoperative).
Secondary outcomes included pain, quality of life, patient satisfaction and anchor scores for pain, function and recovery. Pain at rest and during activity were measured using a numeric rating scale (NRS; 0 no pain, 10 worst imaginable pain). Quality of life was measured by the 5-level version of EuroQol 5 Dimensions (EQ-5D-5L) [40]. A NRS to measure patient satisfaction was used (0–10, 0 dissatisfied to 10 very satisfied). The question asked was ‘How satisfied are you (in general) with the results of your knee surgery?’. Also, anchor questions were asked for pain (1–7, 1 very much deteriorated to 7 very much improved), function (1–7, 1 very much deteriorated to 7 very much improved) and recovery measured using the general perceived recovery questionnaire (GPR; 0–6, 0 worse than ever to 6 fully recovered) [20, 32].
PROs were routinely collected using an online, automated system (OnlinePROMs, Interactive Studios, The Netherlands). Patients completed questionnaires preoperatively and at 6 months, 12 months and 24 months postoperatively. A maximum of two reminders were sent to complete the questionnaires. The treating orthopaedic surgeons did not have direct access to the PROs during follow-up visits.
Patient’s age at surgery (years), BMI (kg/m2), sex (male or female), ASA score (I or II), side of surgery (left or right), patient-specific instrumentation (yes or no), date of surgery, complications and reoperations including plate removal and date of reoperation were collected from the electronic patient file.
Ethical approval
All patients provided written informed consent preoperatively, allowing the use of their anonymized data for future research. Therefore, the local ethical committee declared that they did not require formal ethical approval for studies that use these anonymized data (IRB number: 2022–02).
Statistical analysis
Statistical analysis was performed using IBM SPSS Statistics version 28.0 (IBM Corp, Armonk, New York). Results were reported as mean and standard deviation (mean ± SD), median and interquartile range (median (IQR)), and numbers with percentage (n (%)). To compare patient characteristics and preoperative PROs between the HTO group and the UKA group, continuous variables were first checked for normal distributions. Depending on normality of the data, independent t-tests or Mann–Whitney U tests were performed. For categorical variables, the Chi-square tests or Fisher’s exact tests were performed. Mixed linear models were used to analyse the overall decrease or increase for continuous outcome data. The linear models included the within-subject or group variable (HTO versus UKA) and included patient characteristics that differed between both groups as factors in the model. An alpha of 0.05 was considered statistically significant.
The primary outcome was the OKS over time. To estimate the population mean of the OKS, data from the Dutch Arthroplasty Register (LROI) were used. The mean 1-year OKS for 37,388 TKA patients was 38.6 (95% CI 38.5–38.7). The randomized controlled TOPKAT trial, comparing TKA and UKA, found no difference in OKS at five years between both procedures [1]. Therefore, this population mean for UKA patients was used in the present study. Next, Floerkemeijer et al. reported a median OKS of 43 points (range 8–48 points) after a mean follow-up of 3.6 years in 386 HTO patients [9]. The calculated sample size was based on the abovementioned mean OKS and the known minimal clinical important difference (MCID) of the OKS in knee arthroplasty patients, namely 5.0 points [7]. To demonstrate non-inferiority of HTO compared to UKA, a total of 50 patients were needed in each group. Adjusted for a 10% loss-to-follow-up, at least 55 patients needed to be included in each group.
Results
In total 84 patients were included in the HTO group and 130 patients in the UKA group. In the HTO group, more male patients were included (66 (79%)) compared to the UKA group (61 (47%); p < 0.001). Also, the majority of HTO patients had a preoperative KL grade 3 (63 (75%)) while the majority of UKA patients had a preoperative KL grade 4 (83 (64%); p < 0.001). The other patient characteristics did not significantly differ between the groups (Table 2).
Response rates for the HTO group were 100% (n = 84) preoperatively, 90% (n = 76) at 6 months, 87% (n = 73) at 12 months and 87% (n = 73) at 24 months postoperatively. Response rates for the UKA group were 100% (n = 130) preoperatively, 90% (n = 117) at 6 months, 95% (n = 123) at 12 months and 91% (n = 118) at 24 months postoperatively. No significant differences in response rates between both groups were found (p > 0.05). Three HTO patients (4%) and one UKA patient (1%) were converted to TKA during follow-up (Table 2).
The preoperative OKS was significantly higher in the HTO group (26.6 ± 8.0) than in the UKA group, (23.9 ± 6.9; p = 0.010). Also, the preoperative EQ-5D descriptive system score was significantly higher in the HTO group (0.663, IQR 0.547–0.663) than in the UKA group (0.663 IQR 0.663–0.744; p = 0.001). The other preoperative PROs did not significantly differ between both groups (Table 3).
The OKS over time was 2.5 points (95% CI 1.0–4.0) lower for the HTO group compared to the UKA group (p < 0.001), corrected for preoperative KL grade and sex (Fig. 3). The same model showed that patients with a KL grade 3 had a 1.6 (95% CI − 3.0–− 0.2) points lower OKS over time compared to KL grade 4 (p = 0.03), and males had a 2.3 points (95% CI 0.9–3.7) higher OKS over time than females (p < 0.001) (Table 4).
For the secondary outcomes, the NRS pain in rest score and NRS pain during activity score over time were higher in the THO group that the UKA group. The EQ-5D descriptive system score, NRS satisfaction score and anchor scores for pain, function and GPR were lower over time in the HTO group (Table 5). Patients with KL grade 3 had lower EQ-5D scores over time compared to KL grade 4, and males had a higher EQ-5D score over time than females (Table 5).
Discussion
Our most important findings were slightly better results over time for the UKA group compared to the HTO group in terms of function scores (OKS), scores for pain in rest and during activity, quality of life scores, patient satisfaction scores and anchor scores for pain, function and GPR during the first 24 months after surgery.
Yet, the issue of statistical significance versus clinical relevance is more difficult to address. The MCID for the OKS is 5.0 points [7]. For VAS pain and satisfaction scores, the MCID for joint arthroplasty procedures is assumed to be around 16 points on a 100 points VAS [8, 21, 24], which could be translated to 1.6 points on a 10 point NRS. For the EQ-5D, the MCID is assumed to be around 0.074 [38]. Thus, differences in PROs between HTO and UKA in the present study were below their MCIDs. Regarding the higher preoperative OKS and EQ-5D for the HTO group, this was accounted for in the analysis by analysing the improvement over time for the included PROs as the primary outcome measure.
Previous studies have seldom accounted for the effect of OA grade on PROs after HTO versus UKA. The present study only included KL grade 3 and 4, and adjusted for the difference in baseline OA grade in the linear mixed models assessing PROs. In comparison, Jacquet et al. did not statistically adjust for OA grade, but only included KL grade 2–3 for their comparison, in patients who previously participated in high-impact sports [17]. After 24 months, mean UCLA Activity Scores, Knee injury and Osteoarthritis Outcome Score (KOOS) Sports-subscale scores, and Knee Society Scores were significantly higher in the HTO group. Furthermore, 62% of HTO patients practised impact sports after 24 months, compared to 28% in the UKA group [17]. Recently, Sakai et al. compared HTO and TKA, correcting for age, OA grade and preoperative KOOS in patients > 60 years of age [33]. The authors found no difference in short-term pain relief and improvements measured by KOOS subscales. In addition, a meta-analysis found higher pre- and post-operative activity levels for HTO compared to UKA, while UKA patients showed greater pre- to post-operative improvements [2]. Pooled mean postoperative OKS was 36.7 points for the HTO group and 35.0 points for the UKA group [2], compared to a median OKS of 44 at 24 months in both groups in the present study. Unfortunately, in their meta-analysis the authors did not adjust for preoperative OA grade, limiting the applicability of their results. Thus, limited data show that HTO performs as well or better than UKA in terms of physical activity PROs when adjusting for preoperative OA grade.
Systematic reviews investigating functional outcomes consistently showed that UKA provides better postoperative pain relief and lower revision rates than HTO [6, 14, 31, 34]. Also, postoperative recovery is generally quicker after UKA than HTO [23]. For postoperative complications, several reviews report lower rates after UKA [6, 14, 34], although a 2022 South Korean registry study including 21,194 UKAs and 49,270 HTOs found higher rates of deep venous thrombosis and surgical site infection after UKA [25]. Complications found in both groups in the present study are comparable to those reported in other studies. Although the number of complications found in the present study were lower in UKA versus HTO, several complications in the HTO group occurred in a single patient. Additionally, systematic reviews also consistently show better range-of-motion after HTO than UKA [6, 10, 31, 36]. For postoperative walking velocity, no clear advantage for either procedure was found [10, 14]. Lastly, another reason why some authors prefer HTO over UKA in young, active patients, is the risk of early UKA revision. Registry studies show a significantly higher revision risk for patients < 55 years of age compared to patients > 70 years of age (9% versus 3–4%), and of > 20.000 German UKA patients, one in five patients < 55 years of age underwent revision within five years [18, 41]. Overall, return to physical activities, including sports and work, is good to excellent after both procedures, with higher participation in work and high-impact sports after HTO [2, 16, 17, 39].
Clearly, using correct indications is important to obtain satisfactory results. Modern-day HTO should be primarily offered to relatively young and non-obese patients with mild-to-moderate medial compartment OA, although no strict restrictions for BMI and OA grade exist [26]. Most importantly, an extra-articular tibial varus malalignment must be present that can be corrected while respecting joint-line obliquity [5, 26]. The tibial bone varus angle (TBVA) is one of the decisive factors in preoperative decision-making for UKA vs. HTO, with a TBVA > 5 degrees being predictive of successful HTO [3]. UKA is a proven alternative but must be reserved for patients with medial bone-on-bone OA to guarantee optimal functional outcomes and prosthesis survival [13, 26]. Finally, performing HTO for KL grade 4 may result in higher rates of dissatisfaction and failure [19, 23], although we did not find this association in the present study. On the other hand, young age and severe varus deformity were associated with dissatisfaction after UKA [23]. Therefore, the orthopaedic surgeon should carefully consider the available evidence and the limited overlap in UKA and HTO indications, and discuss this with the patient preoperatively.
Limitations
A limitation is the fact that preoperative stress radiographs were not available for all patients. Consequently, patients who were graded as KL grade 3 may have had a medial compartment KL grade 4 on stress radiographs. Also, external validity might be hampered by the fact that our clinic is a high-volume, dedicated UKA and HTO clinic. For the UKA group, two implant designs were used during the study period, although no difference in PROs was found between these two implant designs [32]. The follow-up of 24 months for both groups may represent another limitation, and follow-up data at 5 and 10 years would be interesting to compare. Next, full weight-bearing protocols differed between both groups. Lastly, selection bias was likely present in the present study, since data collection was prospective, but we did not perform a randomized study.
Conclusion
Younger (50–60 years) patients had better function (OKS), pain and satisfaction scores over time after UKA than HTO, adjusted for preoperative PROs, OA grade and sex. Yet, the observed differences were below their established minimal clinically important differences. Both HTO and UKA are suitable treatment options that will likely lead to satisfactory PROs, although overlap in indications is very limited.
Data availability
No data availability statement is available. Authors may contact the first author for questions regarding usage of data from the present study.
References
Beard DJ, Davies LJ, Cook JA, MacLennan G, Price A (2019) The clinical and cost-effectiveness of total versus partial knee replacement in patients with medial compartment osteoarthritis (TOPKAT): 5-year outcomes of a randomised controlled trial. Lancet 394:746–756
Belsey J, Yasen SK, Jobson S, Faulkner J, Wilson AJ (2021) Return to physical activity after high Tibial Osteotomy or Unicompartmental Knee arthroplasty: a systematic review and pooling data analysis. Am J Sports Med 49:1372–1380
Bonnin M, Chambat P (2004) Der stellenwert der valgisierenden, zuklappenden tikiakopfosteotomie bei der medialen gonarthrose. Orthopade 33:135–142
Borjesson M, Weidenhielm L, Mattsson E, Olsson E (2005) Gait and clinical measurements in patients with knee osteoarthritis after surgery: a prospective 5-year follow-up study. Knee 12:121–127
Brinkman J-M, Lobenhoffer P, Agneskirchner JD, Staubli AE, Wymenga AB, van Heerwaarden RJ (2008) Osteotomies around the knee. J Bone Jt Surg Br 90-B:1548–1557
Cao ZW, Mai XJ, Wang J, Feng EH, Huang YM (2018) Unicompartmental Knee arthroplasty vs high Tibial Osteotomy for Knee Osteoarthritis: a systematic review and meta-analysis. J Arthroplasty 33:952–959
Clement ND, MacDonald D, Simpson AHRWRW (2014) The minimal clinically important difference in the Oxford knee score and Short Form 12 score after total knee arthroplasty. Knee Surgery, Sport Traumatol Arthrosc 22:1933–1939
Danoff JR, Goel R, Sutton R, Maltenfort MG, Austin MS (2018) How much pain is significant? defining the minimal clinically important difference for the visual analog scale for pain after total joint arthroplasty jonathan. J Arthroplasty 7:S71–S75
Floerkemeier S, Staubli AE, Schroeter S, Goldhahn S, Lobenhoffer P (2014) Does obesity and nicotine abuse influence the outcome and complication rate after open-wedge high tibial osteotomy? A retrospective evaluation of five hundred and thirty three patients. Int Orthop 38:55–60
Fu D, Li G, Chen K, Zhao Y, Hua Y, Cai Z (2013) Comparison of high tibial osteotomy and unicompartmental knee arthroplasty in the treatment of unicompartmental osteoarthritis. A meta-analysis J Arthroplasty 28:759–765
Gandhi R, Ayeni O, Davey JR, Mahomed NN (2009) High tibial osteotomy compared with unicompartmental arthroplasty for the treatment of medial compartment osteoarthritis: a meta-analysis. Curr Orthop Pract 20:164–169
Hamilton TW, Pandit HG, Inabathula A, Ostlere SJ, Jenkins C, Mellon SJ, Dodd CAF, Murray DW (2017) Unsatisfactory outcomes following unicompartmental knee arthroplasty in patients with partial thickness cartilage loss. Bone Jt J 99B:475–482
Hamilton TW, Pandit HG, Jenkins C, Mellon SJ, Dodd CAF, Murray DW (2017) Evidence-based indications for mobile-bearing unicompartmental knee arthroplasty in a consecutive cohort of thousand knees. J Arthroplasty 32:1779–1785
Han SB, Kyung HS, Seo IW, Shin YS (2017) Better clinical outcomes after unicompartmental knee arthroplasty when comparing with high tibial osteotomy. Med (United States) 96:9–12
Hoorntje A, Kuijer PPFM, van Ginneken BT, Koenraadt KLM, van Geenen RCI, Kerkhoffs GMMJ, van Heerwaarden RJ (2019) Prognostic factors for return to sport after high tibial osteotomy: a directed acyclic graph approach. Am J Sports Med 47:1854–1862
Hoorntje A, Witjes S, Kuijer PPFM, Koenraadt KLM, van Geenen RCI, Daams JG, Getgood A, Kerkhoffs GMMJ (2017) High rates of return to sports activities and work after osteotomies around the knee: A systematic review and meta-analysis. Sport Med 47:2219–2244
Jacquet C, Gulagaci F, Schmidt A, Pendse A, Parratte S, Argenson JN, Ollivier M (2020) Opening wedge high tibial osteotomy allows better outcomes than unicompartmental knee arthroplasty in patients expecting to return to impact sports. Knee Surgery, Sport Traumatol Arthrosc 28:3849–3857
Jeschke E, Gehrke T, Günster C, Hassenpflug J, Malzahn J, Niethard FU, Schräder P, Zacher J, Halder A (2016) Five-year survival of 20,946 unicondylar knee replacements and patient risk factors for failure: an analysis of German insurance data. J Bone Jt Surg - Am 98:1691–1698
Jin C, Song EK, Santoso A, Ingale PS, Choi IS, Seon JK (2020) Survival and risk factor analysis of medial open wedge high tibial osteotomy for Unicompartment Knee Osteoarthritis. Arthrosc - J Arthrosc Relat Surg 36:535–543
Kamper SJ, Ostelo RWJG, Knol DL, Maher CG, de Vet HCW, Hancock MJ (2010) Global Perceived Effect scales provided reliable assessments of health transition in people with musculoskeletal disorders, but ratings are strongly influenced by current status. J Clin Epidemiol 63:760-766.e1
Katz NP, Paillard FC, Ekman E (2015) Determining the clinical importance of treatment benefits for interventions for painful orthopedic conditions. J Orthop Surg Res 10:1–11
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–503
Kim MS, Koh IJ, Sohn S, Jeong JH, In Y (2019) Unicompartmental knee arthroplasty is superior to high tibial osteotomy in post-operative recovery and participation in recreational and sports activities. Int Orthop 43:2493–2501
Laigaard J, Pedersen C, Thea N, Mathiesen O, Peder A (2021) Minimal clinically important differences in randomised clinical trials on pain management after total hip and knee arthroplasty: a systematic review. Br J Anaesth 126:1029–1037
Lee SH, Kim HR, Seo HY, Seon JK (2022) A comparative study of 21,194 UKAs and 49,270 HTOs for the risk of unanticipated events in mid-age patients from the national claims data in South Korea. BMC Musculoskelet Disord 23:1–9
Lobenhoffer P (2017) Indication for Unicompartmental Knee Replacement versus Osteotomy around the Knee. J Knee Surg 30:769–773
Maier MW, Kuhs F, Streit MR, Schuhmacher P, Walker T, Ewerbeck V, Gotterbarm T (2015) Unicompartmental knee arthroplasty in patients with full versus partial thickness cartilage loss (PTCL): equal in clinical outcome but with higher reoperation rate for patients with PTCL. Arch Orthop Trauma Surg 135:1169–1175
Migliorini F, Tingart M, Niewiera M, Rath B, Eschweiler J (2019) Unicompartmental versus total knee arthroplasty for knee osteoarthritis. Eur J Orthop Surg Traumatol 29:947–955
Niinimäki TT, Murray DW, Partanen J, Pajala A, Leppilahti JI (2011) Unicompartmental knee arthroplasties implanted for osteoarthritis with partial loss of joint space have high re-operation rates. Knee 18:432–435
Pandit H, Jenkins C, Gill HS, Barker K, Dodd CAF, Murray DW (2011) Minimally invasive Oxford phase 3 unicompartmental knee replacement: results of 1000 cases. J Bone Jt Surg 93:198–204
Ping H, Wen J, Liu Y, Li H, Wang X, Kong X, Chai W (2022) Unicompartmental knee arthroplasty is associated with lower pain levels but inferior range of motion, compared with high tibial osteotomy: a systematic overview of meta-analyses. J Orthop Surg Res 17:1–16
Pronk Y, Paters AAM, Brinkman JM (2021) No difference in patient satisfaction after mobile bearing or fixed bearing medial unicompartmental knee arthroplasty. Knee Surgery, Sport Traumatol Arthrosc 29:947–954
Sakai M, Akasaki Y, Akiyama T, Horikawa T, Okazaki K, Hamai S, Tsushima H, Kawahara S, Kurakazu I, Kubota K, Mizu-uchi H, Nakashima Y (2022) Similar short-term KOOS between open-wedge high Tibial Osteotomy and Total Knee Arthroplasty in patients over age 60: a propensity score-matched cohort study. Mod Rheumatol 33:623–628
Santoso MB, Wu L (2017) Unicompartmental knee arthroplasty, is it superior to high tibial osteotomy in treating unicompartmental osteoarthritis? a meta-analysis and systemic review. J Orthop Surg Res 12:50
Snow M, Jermain P, Mandalia V, Murray J, Khakha R, McNicholas M, Dawson M (2021) A 2021 consensus statement on osteotomies around the knee by the UK Knee Osteotomy consensus Group (KOG). Knee 33:73–83
Song SJ, Bae DK, Il Kim K, Park CH (2019) Long-term survival is similar between closed-wedge high tibial osteotomy and unicompartmental knee arthroplasty in patients with similar demographics. Knee Surg Sport Traumatol Arthrosc 27(4):1310–1319
Stukenborg-Colsman C, Wirth CJ, Lazovic D, Wefer A (2001) High tibial osteotomy versus unicompartmental joint replacement in unicompartmental knee joint osteoarthritis: 7–10-year follow-up prospective randomised study. Knee 8:187–194
Walters SJ, Brazier JE (2005) Comparison of the minimally important difference for two health state utility measures: EQ-5D and SF-6D. Qual Life Res 14:1523–1532
Witjes S, Gouttebarge V, Kuijer PPFM, van Geenen RCI, Poolman RW, Kerkhoffs GMMJ (2016) Return to sports and physical activity after total and unicondylar knee arthroplasty: a systematic review and meta-analysis. Sport Med 46:1–24
(1990) EuroQol--a new facility for the measurement of health-related quality of life. Health Policy 16:199–208
National joint registry for England, Wales, Northern Ireland and the Isle of Man 17th Annual Report.
Acknowledgements
None.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AH designed the study, performed the data analysis and interpretation of data, and drafted the manuscript. YP supervised the data analysis and helped draft the manuscript. JMB, RvG and RvH helped design the study and performed interpretation of data and revised the manuscript. All authors approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
RvH is a paid consultant for Newclip. The other authors declare no conflicts of interest relevant to the present study.
Ethical approval
This is a retrospective study on prospectively collected data and all patients signed the informed consent to allow further scientific analysis using their anonymised data. Thus, the institutional review board declared that formal approval was not required for this study (IRB number: 2022–02).
Informed consent
All patients signed informed consent to allow further scientific analysis using their anonymised data.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
High tibial osteotomy versus unicompartmental knee arthroplasty for Kellgren–Lawrence grade 3–4 knee osteoarthritis in younger patients: comparable improvements in patient-reported outcomes, adjusted for osteoarthritis grade and sex.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hoorntje, A., Pronk, Y., Brinkman, J.M. et al. High tibial osteotomy versus unicompartmental knee arthroplasty for Kellgren–Lawrence grade 3–4 knee osteoarthritis in younger patients: comparable improvements in patient-reported outcomes, adjusted for osteoarthritis grade and sex. Knee Surg Sports Traumatol Arthrosc 31, 4861–4870 (2023). https://doi.org/10.1007/s00167-023-07526-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-023-07526-5