Abstract
Purpose
Given the paucity of literature on the re-revision of ACL, the current study was undertaken. The purpose of this systematic review was to synthesise and qualitatively assess the currently available evidence in the literature regarding the re-revision of ACL reconstruction (rrACLR).
Methods
A systematic review was conducted based on the PRISMA guidelines. The following search terms were used in the title, abstract and keywords fields: “ACL” or “anterior cruciate ligament” AND “revision” or “multiple” or “repeat”. The outcome data extracted from the studies were the Lysholm score, Subjective IKDC, Marx Score, Tegner, Marx Score, KOOS score, radiological changes and the rate of return to sports. Complications, failures and/or revision surgery were also analysed.
Results
The cohort consisted of 295 patients [191 (64.7%) men and 104 (35.3%) women] with a mean age of 29.9 ± 2.8 years (range 14–58 years) from 10 studies. The mean postoperative follow-up (reported in all studies except one) was 66.9 ± 44.7 months (range 13–230.4 months). Associated injuries were 103 (34.9%) medial meniscus tears, 57 (19.3%) lateral meniscus tears, 14 (4.7%) combined medial plus lateral meniscus tears, 11 (3.7%) meniscal tears (not specified), 252 (85.4%) cartilage lesions, 6 (2.0%) medial collateral ligament injury and 2 (0.7%) lateral collateral ligament injuries. In 47 (15.9%) patients an extra-articular plasty was performed for the anterolateral ligament. In all studies that reported pre- and post-operative IKDC (subjective and objective) and Lysholm score, there was a significant improvement compared to the pre-operative value (p < 0.05). At the final follow-up, laxity measured with KT-1000 was found to be 2.2 ± 0.6 mm. 31 (10.5%) out of 295 patients returned to their pre-injury activity level. A total of 19 (6.4%) re-ruptures were found, while only 4 (1.4%) complications (all minors) were reported, out of which 2 (0.7%) were superficial infections, 1 (0.3%) cyclops lesion and 1 (0.3%) flexion loss.
Conclusion
Multiple revisions of anterior cruciate ligament reconstruction allow acceptable clinical results and a good degree of knee stability with a low rate of subsequent new re-ruptures but the possibility of regaining pre-injury sports activity is poor; whenever possible, it is preferred to revise the ligament in one stage. This surgery remains a challenge for orthopaedic surgeons and many doubts persist regarding the ideal grafts, additional extra-articular procedures and techniques to use.
Level of evidence
IV.
Study registration
PROSPERO-CRD42022352164 (https://www.crd.york.ac.uk/prospero/).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
ACL reconstructions are one of the most commonly performed arthroscopic reconstructive procedures and this has only been estimated to increase over the next few years until 2025 by some computer-based predictive models [20]. Understandably, such increasing ACL surgeries will lead to a greater number of failures, which will in turn cause the revision surgery rates to rise. The rate of revision after primary ACL reconstruction has been reported to be between 4 and 13% and is now with the increasing burden of revision [21].
The revision of a failed ACL reconstruction can be particularly challenging considering that the surgeon needs to account for previous bony tunnels and their positions, the widening of previous tunnels, the presence of implants from previous surgery, post-surgical adhesions, bone loss and concurrent injuries to other structures of the knee that might impact the outcome of the current revision surgery [21]. These factors also have a bearing on whether one performs a single-staged or two-staged revision surgery. Preoperative tunnel widening has been reported as an indication of a two-staged revision ACL reconstruction [15, 16]. However, a recent cohort study has reported excellent results with a single-stage strategy for revision ACL reconstruction [26].
The superiority of one- or two-staged procedures over the other is yet to be proven, with most of the available evidence comparing two-staged and single-staged strategies being retrospective [26].
Thus, it can be stated that these challenges are only being compounded in the setting of a re-revision of a failed revision ACL reconstruction. Another important consideration facing surgeons is the choice of graft. In the setting of multiple revisions, the grafts from the ipsilateral limb might be unavailable and the patient cannot allow for any surgery on the uninjured limb the contralateral uninjured limb to be subjected to surgical procedure for graft harvesting [8, 29].
The revision of failed ACL reconstruction has been well studied in the literature. Although with time, the techniques have improved and the outcomes after a revision surgery have seen progress, the results after revision ACL surgery have still been reported to be inferior compared to primary ACL surgery in terms of patient-reported outcomes, clinical knee function scores and the incidence of degenerative changes [29]. Following revision anterior cruciate ligament reconstructions, failure rates up to 30% have been reported in the literature and the outcomes following revision anterior cruciate ligament reconstructions have been inferior to primary reconstructions, with failure rates up to 4 times higher in the former compared to primary ACL reconstruction [5].
These failed revisions require re-revision surgeries. Hence, there is an urgent need for a better understanding of re-revision surgery but there are lacunae in contemporary literature concerning outcomes following a re-revision [17, 28]. With the demonstrable rise of ACL reconstructions and more patients wanting to remain active in their pre-injury sports activities, there is going to be an inevitable rise in the number of re-revisions with the risk of repeated injuries [17, 28].
The purpose of this systematic review was to synthesise and qualitatively assess the currently available evidence in the literature regarding the re-revision of ACL reconstruction (rrACLR).
It has been hypothesised that re-revision surgery can provide good knee stability with satisfactory clinical results.
Materials and methods
The current systematic review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines and is registered in the PROSPERO Registry (CRD42022352164) [23, 25].
Eligibility criteria
The literature selected for this study was based on the following criteria:
Study design
Randomised controlled trials (RCTs), controlled (non-randomised) clinical trials (CCTs), prospective and retrospective comparative cohort studies, case–control studies and case series were included in the review. Case reports and case series that did not report data on clinical and functional results were excluded.
Participants
The studies were conducted on skeletally mature patients treated for at least two anterior cruciate ligament (ACL) reconstructions.
Interventions
Studies that reported data on clinical, functional and radiological outcomes following multiple (≥ 2) ACL reconstructions. For ACL reconstruction, the surgical technique (the type of graft used, number of bundles, fixation technique and tensioning protocol) and the rehabilitation protocol were collected.
Types of outcome measures
The outcome measures extracted from the studies were the Lysholm score, Subjective International Knee Documentation Committee (IKDC), Marx Scores, Tegner, Marx Scores, Knee Injury and Osteoarthritis Outcome (KOOS) scores, radiological changes, rate of return to sports, complications, failures and/or revision surgery.
Information sources and search
A systematic search for relevant literature was performed on the PubMed (MEDLINE), Scopus, EMBASE and Cochrane Library databases. The publication date was not considered an inclusion criterion. The search was carried out in July 2022. Two independent reviewers (RD and AM) assisted in conducting and validating the search. The following search terms were used in the title, abstract and keywords fields: “ACL” or “anterior cruciate ligament” AND “revision” or “multiple” or “repeat”.
Data collection and analysis
Study selection
The retrieved articles were first screened by title, and if found relevant, were screened further by reading the abstract. Then, the content of the articles was evaluated for eligibility.
The authors have separately reviewed to reduce the risk of bias all the selected articles, references, as well as articles excluded from the study. In case of any disagreement between the reviewers, the senior investigator made the final decision. At the end of the process, further studies that might have been missed were manually searched by going through the reference lists of the included studies and relevant systematic reviews.
Data collection process
The data were extracted from the selected articles by the first two authors using a computerized tool created with Microsoft Access (Version 2010, Microsoft Corp, Redmond Washington). Each article was validated again by the first author before analysis. For each study, data from the patients was extracted (age, gender, duration between injury and surgery and follow-up evaluation), their injuries (type, aetiology and associated injuries), the surgical technique (the type of grafts used, the number of bundles, fixation technique, extra-articular procedures and tensioning protocol), the rehabilitation protocol, post-operative outcomes, rate of complications and the rate of return to sports.
Level of evidence
The Oxford Levels of Evidence set by the Oxford Centre for Evidence-Based Medicine was used to categorise the level of evidence [24].
Evaluation of the quality of studies
The quality of the selected studies was evaluated using the Methodological Index for Nonrandomized Studies (MINORS) score [27]. The checklist includes 12 items, out of which the last four are specific to comparative studies. Each item was given a score of 0–2 points. The ideal score was set at 16 points for non-comparative studies and 24 for comparative studies.
Statistical analysis
The extracted quantitative parameters (age, follow-up time and results of the PROMs) were given as mean ± standard deviation (SD) when provided in the articles. Otherwise, alternative values like median or range were extracted. Due to the high statistical and methodological heterogeneity in the included studies, a meta-analysis comparing the results between patients with and without concomitant surgeries was not possible. Instead, a narrative description and comparison of the clinical results were performed.
Results
Search results
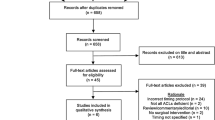
The electronic search yielded 927 studies. The 812 duplicates were removed, leaving 115 studies, out of which 88 were excluded after reviewing the abstracts, with a final number of 27. An additional 17 articles were excluded based on the aforementioned inclusion and exclusion criteria [10]. This left 10 studies for analysis [1,2,3, 7, 9, 11, 13, 14, 31, 32]. Figure 1 shows the flowchart depicting the selection process for the studies. The analysed studies had a mean MINORS score of 13 (range 12–14), which confirmed the methodological quality of the available literature (Table 1).
Patient characteristics
Table 1 shows the characteristics of the cohorts of the 10 selected studies and a summary of their data. The cohort consisted of 295 patients [191 (64.7%) men and 104 (35.3%) women] with a mean age of 29.9 ± 2.8 years (range 14–58 years). The mean postoperative follow-up (reported in all studies except one) was 66.9 ± 44.7 months (range 13–230.4 months).
Associated injuries were 103 (34.9%) medial meniscus tears, 57 (19.3%) lateral meniscus tears, 14 (4.7%) combined medial plus lateral meniscus tears, 11 (3.7%) meniscal tears (not specified), 252 (85.4%) cartilage lesion, 6 (2.0%) medial collateral ligament injury and 2 (0.7%) lateral collateral ligament injuries.
Surgical protocol and rehabilitation protocol
All procedures were performed using a single bundle technique; a double-stage surgery for the revision had been performed only in 8 (2.7%) cases, and in all other cases, a single-stage revision was performed. The graft selected for the revision was an allograft in 139 (47.1%) cases [72 (24.4%) not specified, 18 (6.1%) Achilles tendon, 15 (5.1%) tibialis posterior, 9 (3.1%) tibialis anterior, 1 (0.3%) quadriceps and 24 (8.1%) patellar tendon]; in 111 (37.6%) cases, it was an autologous homolateral graft [92 (31.2%) not specified, 16 (5.4%) patellar tendon, 2 (0.7%) hamstring and 1 (0.3%) quadriceps]; in 38 (12.9%) cases, an autologous contralateral graft [31 (10.5%) hamstring and 7 (2.4%) patellar tendon], while in 7 (2.4%) cases, it was a mixed graft. For the femoral fixation, 7 studies reported the use of a screw, while 1 study reported the use of staples of the endobutton system. For tibial fixation, the use of a titanium screw was reported in all cases except for one in which the use of a staple was mentioned.
Five different techniques were reported for the re-revision of ACL reconstruction: transtibial in 2 studies, transportal in 4 studies, outside-in in 1 study and over the top in 1 study. All studies reported a single bundle technique.
An extra-articular plasty was performed in 47 (15.9%) patients with anterolateral ligament injury, 11 (3.7%) who underwent anterolateral ligament reconstruction, and in 24 (8.1%) patients the extra-articular plasty as planned in the over-the-top technique, and 12 (4.1%) received an extra-articular tenodesis with a modified Macintosh technique). Only in 1 (0.3%) case, a high tibial valgus osteotomy was performed. Only three studies reported degrees for tibial screw fixation, which ranged from 30° to 90°. Two studies did not suggest the use of a post-surgery brace, while it was recommended in 5. Weight-bearing was allowed from day 0 in 7 studies (Table 2).
Clinical and functional outcomes
In all studies that reported pre-and post-operative IKDC (subjective and objective) and Lysholm scores, there was a significant improvement compared to the pre-operative value (p < 0.05). In detail, subjective IKDC ranged from IKDCpre 48.7 ± 7.8 to 76.2 ± 8.9 (p < 0.05).
In pre-operative IKDC, there were 6 patients with grade B, 8 with grade C, and 3 with grade D, while in post-operative, there were 8 patients with grade A, 13 with grade B, 5 with grade C and 1 with grade D.
Lysholm score ranged from Lysholmpre 54.3 ± 7.8 to Lysholmpost 80.2 ± 8.5. Tegner score ranged from Tegnerpre 5.6 ± 2.0 to Tegnerpost 4.8 ± 1.0 (p < 0.05). KOOS and Marx’s Score were reported, respectively, only in 2 studies with only final follow-up values (KOOS: Pain: 93; Symptoms: 94; ADL: 96; Sports: 75; QOL: 50; Marx Score: 6.7) (Table 3).
Laxity
In 2 studies, laxity was measured pre-and post-surgery, and there was a significant improvement in the stability of the knee (p < 0.05). At the final follow-up, laxity measured with KT-1000 resulted to be 2.2 ± 0.6 mm.
Return to sports
A total of 31 (10.5%) out of 295 patients returned to their pre-injury activity level.
Complications and failure
A total of 19 (6.4%) re-ruptures were found, while only in 4 cases (1.4%) complications (all minors) were reported, which were 2 (0.7%) superficial infections, 1 (0.3%) cyclops lesion and 1 (0.3%) flexion loss.
Discussion
The most important findings of the current systematic review are that even after a re-revision ACL reconstruction (rrACLR), knee function was improved as reflected by the significant improvements in the Lysholm knee scores and both in the objective and subjective IKDC scores and the improved Tegner activity level, there was still a considerably low rate of return to pre-injury sports level activity.
The re-revision ACL surgery offers appreciable outcomes; however, the possibility of returning to sports activity is less when compared to those after revision ACL reconstructions. In the meta-analysis by Grassi et al., the authors reported that the overall return to any sporting activity was 84% and the rate of return to pre-injury level of activity was only 52% [12]. The rate of return to sports at the pre-injury level in the current study stands lower at 10.5%. The performance of the knee after re-revision (rrACLR) could not only be affected by the quality of the reconstruction but also by other adjunctive factors. Most importantly, the presence of concomitant injuries and the management of those would also negatively influence the outcome following a rrACLR. In the current study, the most common injuries present concomitantly were meniscal injuries, followed by cartilage lesions. The influence of the concomitant injuries on the knee function, following a re-revision ACLR, is not easy to quantify and hence becomes an intangible factor while considering this outcome.
Despite this poor return to sport, the knees concerning clinical examination for laxity, performed well after the re-revision surgery, with significant improvements in laxity as measured by KT-1000; however, this was reported only in 2 studies. Given that following rrACLR, the knee stability is quite improved, it would not be incorrect to assume that other factors are at play with respect to post-rrACLR sport participation.
An overwhelming majority of cases in the current review were carried out by a single-staged re-revision procedure, with only 2.7% of cases using a two-staged procedure. The surgical techniques used were heterogenous in our review. A previous meta-analysis by Colatruglio et al. on outcomes of one versus two stages revision of ACLR showed that the outcomes of both the single and double-stage techniques were comparable, even though there were certain indications, where a one-staged procedure was considered to be better. Strong evidence of the superiority of one technique over the other is lacking [4]. A study by Mitchell et al. also found no difference in the outcome following single- and two-staged revision ACL reconstructions [22]. Literature regarding the staging of procedures in the re-revision setting is also lacking. However, the current systematic review also demonstrates good outcomes following single-staged re-revision since the review has more single-staged revisions. The results were similar to the findings of Mitchell et al. and Colatruglio et al. Thus, the surgeons may prefer a single-staged re-revision procedure unless the specific situation warrants a two-staged revision procedure [4, 22].
Regarding graft choice, allograft was the most preferred in this review, and the most commonly used allograft was the Achilles tendon. The second most commonly used was a bone-patellar tendon-bone graft from the same limb. The least utilised were autografts from the opposite limb, for which hamstring tendons were commonly used and quadriceps. The ideal graft choice in the setting of a re-revision is yet to be clarified. The high utilisation of allografts in rrACLR can be accounted for by the fact that other graft options have been exhausted when a patient undergoes multiple revisions. A Systematic review on allograft ACLR by Mariscalco et al. studied autograft versus nonirradiated allograft [19]. Similarly, graft failure rate, laxity and patient-reported outcome scores were found in both groups [19]. Similar results were also observed by Cvetanovich et al. [6]. There have been reports of greater failure rates with allograft as compared to bone-patellar-tendon-bone autograft, possibly due to the longer duration of graft incorporation predisposing to non-traumatic ACL graft failures [6, 18, 30]. The graft of choice for the re-revision of ACL reconstruction and the use of allograft are areas that need further study in the future.
Out of 295 of rrACLR, only 48 cases reported extra-articular procedures or a tibial osteotomy; in current literature, there is a growing interest in additional procedures like these to increase the knee’s stability after an ACL reconstruction, especially in re-revision settings.
Several authors confirmed that an excessive posterior tibial slope (PTS) increases tensions within the ACL and exacerbates the risk of injury [33]. The normal PTS is within the range of 5°–7°, depending on the measurement technique, and is considered pathologic if it exceeds 12° [33]. For revision ACL reconstructions, however, surgeons must consider the correction of an excessive PTS, especially after the failure of two or more consecutive procedures [33].
The potential benefit of combining ALLR with ACLR is greater rotational stability, which leads to a decrease in both the high failure rates seen particularly in young patients and progressive osteoarthritic changes seen after isolated ACLR [34].
Further study is warranted to compare directly HTO and ALL reconstruction alongside multiple-revision ACL reconstruction versus ACL reconstruction alone [34].
The overall complication rate was low and the ones observed were all minor. Hence, the re-revision of ACL reconstruction can be considered a safe and effective procedure with good outcomes, irrespective of whether it is performed single-staged or two-staged or whether it utilises both autografts and allografts (Figs. 2, 3, 4, and 5).
To the author’s best knowledge, this is one of the first systematic reviews on the re-revision of ACL reconstruction. However, the review was limited by the heterogeneous reporting of subjective and objective outcomes in the available studies. Also, it is difficult to consider the outcomes as those of re-revision ACL in isolation as they were concomitant in injuries in most of the cases with additional procedures to the knee. There were no control groups and no comparative analysis could be done.
Conclusions
Multiple revisions of anterior cruciate ligament reconstruction allow acceptable clinical results and a good degree of knee stability with a low rate of subsequent new re-ruptures but a scarce level of return to pre-injury sports activity; whenever possible, it is preferred to revise the ligament in one stage. This surgery remains a big challenge for orthopaedic surgeons and many doubts remain regarding the ideal grafts, additional extra-articular procedures and techniques to use to prevent another rupture.
References
Ahmed I, Salmon L, Roe J, Pinczewski L (2017) The long-term clinical and radiological outcomes in patients who suffer recurrent injuries to the anterior cruciate ligament after reconstruction. Bone Jt J. 99-B:337–343
Buda R, Ruffilli A, Di Caprio F, Ferruzzi A, Faldini C, Cavallo M, Vannini F, Giannini S (2013) Allograft salvage procedure in multiple-revision anterior cruciate ligament reconstruction. Am J Sports Med 41:402–410
Chen JL, Allen CR, Stephens TE, Haas AK, Huston LJ, Wright RW, Feeley BT; Multicenter ACL Revision Study (MARS) Group (2013) Differences in mechanisms of failure, intraoperative findings, and surgical characteristics between single- and multiple-revision ACL reconstructions: a MARS cohort study. Am J Sports Med 41:1571–1578
Colatruglio M, Flanigan DC, Long J, DiBartola AC, Magnussen RA (2021) Outcomes of 1- versus 2-stage revision anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Am J Sports Med 49:798–804
Cristiani R, Forssblad M, Edman G, Eriksson K, Stålman A (2021) Age, time from injury to surgery and quadriceps strength affect the risk of revision surgery after primary ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 29:4154–4162
Cvetanovich GL, Mascarenhas R, Saccomanno MF, Verma NN, Cole BJ, Bush-Joseph CA, Bach BR (2014) Hamstring autograft versus soft-tissue allograft in anterior cruciate ligament reconstruction: a systematic review and meta-analysis of randomized controlled trials. Arthroscopy 30:1616–1624
Dini F, Tecame A, Ampollini A, Adravanti P (2021) Multiple ACL revision: failure analysis and clinical outcomes. J Knee Surg 34:801–809
Ekeland A, Engebretsen L, Fenstad AM, Heir S (2020) Similar risk of ACL graft revision for alpine skiers, football and handball players: the graft revision rate is influenced by age and graft choice. Br J Sports Med 54:33–37
Engler ID, Salzler MJ, Wall AJ, Johnson WR, Makani A, Shields MV, Gill TJ (2020) Patient-reported outcomes after multiple-revision ACL reconstruction: Good but Not Great. Arthrosc Sports Med Rehabil 2:e539–e546
Glasgow RE, Huebschmann AG, Brownson RC (2018) Expanding the CONSORT figure: increasing transparency in reporting on external validity. Am J Prev Med 55:422–430
Gorodischer TD, Zicaro JP, Yacuzzi C, Costa Paz M (2021) Good short-term clinical outcomes and low rates of return to sports after repeat revision ACL reconstruction. J Knee Surg. https://doi.org/10.1055/s-0041-1723765
Grassi A, Zaffagnini S, Marcheggiani Muccioli GM, Neri MP, Della Villa S, Marcacci M (2015) After revision anterior cruciate ligament reconstruction, who returns to sport? A systematic review and meta-analysis. Br J Sports Med 49:1295–1304
Griffith TB, Allen BJ, Levy BA, Stuart MJ, Dahm DL (2013) Outcomes of repeat revision anterior cruciate ligament reconstruction. Am J Sports Med 41:1296–1301
Helito CP, da Silva AGM, Guimarães TM, Sobrado MF, Pécora JR, Camanho GL (2022) Functional results of multiple revision anterior cruciate ligament with anterolateral tibial tunnel associated with anterolateral ligament reconstruction. Knee Surg Relat Res 34:24
Järvelä T, Musahl V (2022) Revising a double-bundle anterior cruciate ligament: one- or two-stage procedure? Knee Surg Sports Traumatol Arthrosc 30:1855–1857
Kanakamedala AC, Edgar CM, Fanelli GC, Musahl V, Alaia MJ (2022) Surgical considerations in revision anterior cruciate ligament reconstruction. Instr Course Lect 71:475–487
Liukkonen RJ, Ponkilainen VT, Reito A (2022) Revision rates after primary ACL reconstruction performed between 1969 and 2018: a systematic review and metaregression analysis. Orthop J Sports Med 10:23259671221110190
Maletis GB, Chen J, Inacio MC, Funahashi TT (2016) Age-related risk factors for revision anterior cruciate ligament reconstruction: a cohort study of 21,304 patients from the kaiser permanente anterior cruciate ligament registry. Am J Sports Med 44:331–336
Mariscalco MW, Magnussen RA, Mehta D, Hewett TE, Flanigan DC, Kaeding CC (2014) Autograft versus nonirradiated allograft tissue for anterior cruciate ligament reconstruction: a systematic review. Am J Sports Med 42:492–499
Marx RG (2020) Latest trends in ACL reconstruction. Sports Med Arthrosc Rev 28:35
Miller MD, Kew ME, Quinn CA (2021) Anterior cruciate ligament revision reconstruction. J Am Acad Orthop Surg 29:723–731
Mitchell JJ, Chahla J, Dean CS, Cinque M, Matheny LM, LaPrade RF (2017) Outcomes after 1-stage versus 2-stage revision anterior cruciate ligament reconstruction. Am J Sports Med 45:1790–1798
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. J Clin Epidemiol 134:178–189
Paras T, Sabzevari S, Solomon D, Smith C, McDonough C, Lin A (2022) Trends in level of evidence of systematic reviews in sports medicine, 2010–2020: a systematic review and meta-analysis. Orthop J Sports Med 10:23259671221121330
Pieper D, Rombey T (2022) Where to prospectively register a systematic review. Syst Rev 11:8
Pioger C, Saithna A, Rayes J, Haidar IM, Fradin T, Ngbilo C, Vieira TD, Cavaignac E, Sonnery-Cottet B (2021) Influence of preoperative tunnel widening on the outcomes of a single stage-only approach to every revision anterior cruciate ligament reconstruction: an analysis of 409 consecutive patients from the SANTI study group. Am J Sports Med 49:1431–1440
Qumseya BJ (2021) Quality assessment for systematic reviews and meta-analyses of cohort studies. Gastrointest Endosc 93:486-494.e1
Rahardja R, Zhu M, Love H, Clatworthy MG, Monk AP, Young SW (2020) Rates of revision and surgeon-reported graft rupture following ACL reconstruction: early results from the New Zealand ACL Registry. Knee Surg Sports Traumatol Arthrosc 28:2194–2202
Tapasvi S, Shekhar A (2021) Revision ACL reconstruction: principles and practice. Indian J Orthop 55:263–275
Wasserstein D, Khoshbin A, Dwyer T, Chahal J, Gandhi R, Mahomed N, Ogilvie-Harris D (2013) Risk factors for recurrent anterior cruciate ligament reconstruction: a population study in Ontario, Canada, with 5-year follow-up. Am J Sports Med 41:2099–2107
Wegrzyn J, Chouteau J, Philippot R, Fessy MH, Moyen B (2009) Repeat revision of anterior cruciate ligament reconstruction: a retrospective review of management and outcome of 10 patients with an average 3-year follow-up. Am J Sports Med 37:776–785
Yoon KH, Kim JH, Kwon YB, Kim EJ, Kim SG (2020) Re-revision anterior cruciate ligament reconstruction showed more laxity than revision anterior cruciate ligament reconstruction at a minimum 2-year follow-up. Knee Surg Sports Traumatol Arthrosc 28:1909–1918
Zeng C, Yang T, Wu S, Gao SG, Li H, Deng ZH, Zhang Y, Lei GH (2016) Is posterior tibial slope associated with noncontact anterior cruciate ligament injury? Knee Surg Sports Traumatol Arthrosc 24:830–837
Ziegler CG, DePhillipo NN, Kennedy MI, Dekker TJ, Dornan GJ, LaPrade RF (2021) Beighton score, tibial slope, tibial subluxation, quadriceps circumference difference, and family history are risk factors for anterior cruciate ligament graft failure: a retrospective comparison of primary and revision anterior cruciate ligament reconstructions. Arthroscopy 37:195–205
Acknowledgements
This study was supported and funded by the Italian Ministry of Health – “Ricerca Corrente”.
Funding
Open access funding provided by Università degli Studi di Milano within the CRUI-CARE Agreement. None.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not needed.
Consent to participate
Not needed.
Consent to publish
All authors consent to the publication of the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
D’Ambrosi, R., Meena, A., Raj, A. et al. Multiple revision anterior cruciate ligament reconstruction: not the best but still good. Knee Surg Sports Traumatol Arthrosc 31, 559–571 (2023). https://doi.org/10.1007/s00167-022-07197-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07197-8