Abstract
Purpose
Cemented fixation remains the gold standard in total knee arthroplasty. With an increasing number of younger patients undergoing total knee arthroplasty and a growing patient population demanding higher physical activity, a rising interest in discussion of cementless fixation is notable. The current scientific literature does not give a clear recommendation for or against uncemented total knee arthroplasty. The purpose of this study was the investigation of the 5-year clinical and radiographic outcomes of a cementless deep-dish rotating platform implant.
Methods
A total of 91 primary cementless total knee arthroplasties were included in this single-centre prospective observational study. The primary outcome was revision rate due to aseptic component loosening. Further outcome measures were assessment of the of the radiographic outcome as well as the clinical outcome based on Range of Motion and scores such as American Knee Society Score, Oxford Knee Score, Knee Injury and Osteoarthritis Outcome Score and European Quality of Life 5 Dimension 3 Level at a follow-up of 5 years.
Results
Mean age of the study population was 67.3 ± 6.6 years with 49.5% of the participants being female. Aseptic component loosening occurred in none of the patients. Implant survival with revision for any reason as endpoint was 97.8% (95% CI 100–96%) and 95.6% (95% CI 100–94%) with reoperation of any cause as endpoint. Radiolucent lines were detected in a total of eight cases (8.8%) and disappeared within the first year after surgery in five cases. Total Range of Motion improved significantly from 106° ± 15° preoperatively to 118° ± 10° at final FU (p < 0.001). All investigated scores improved significantly after total knee arthroplasty.
Conclusion
The results of this study reveal excellent mid-term performance of a cementless deep dish rotating platform total knee implant, with no component loosening, very low overall revision rate, only temporarily present radiolucent lines in a minority of patients and excellent clinical results. Therefore, cementless total knee arthroplasty is an appropriate treatment option for patients with severe osteoarthritis of the knee.
Level of evidence
Level II (prospective cohort study).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cemented fixation remains the gold standard in TKA, demonstrating successful outcomes with low rates of aseptic loosening in long-term follow-up (FU) [13, 21].
In recent years, cementless fixation has gained more interest for several different reasons. The theoretical advantages of cementless fixation in TKA include the potential preservation of native bone stock, the avoidance of cement debris and, especially, the potential of achieving a long-lasting and biological fixation [8]. As the number of younger patients undergoing TKA is constantly increasing, there is also an increasing number of patients demanding higher physical activity resulting in mechanical stress on the implant with higher probability of possible secondary surgery [8, 15, 34]. Therefore, a rising interest in discussion of cementless fixation is notable. In studies comparing both fixation techniques, uncemented TKA shows comparable short-term and mid-term outcomes without any statistical advantage for one method over the other [9, 22, 37]. Hence, the current scientific literature does not give a clear recommendation for or against uncemented TKA.
The purpose of this study was the investigation of the 5-year clinical and radiologic outcome in patients who underwent TKA with the cementless Vanguard Deep Dish Rotating Platform Knee (Zimmer Biomet, Warsaw, Indiana, U.S.). The hypothesis of this study was that cementless rotating platform TKA is an appropriate and safe treatment option for patients with severe osteoarthritis (OA) of the knee with low revision rates and good clinical outcomes. This is the first prospective study investigating the mid-term results of the specific implant mentioned above.
Materials and methods
Study population
This is a single-arm, single-centre, prospective, observational study of performance and safety of the uncemented Vanguard Deep Dish Rotating Platform Knee (Zimmer Biomet, Warsaw, Indiana, U.S.). The performance was assessed by the rate of aseptic loosening within 5 years of FU (primary outcome measure), radiographic evaluations as well as various clinical scores (secondary outcome measure). Consecutive patients who have undergone primary TKA using the implant mentioned above between 2013 and 2016 with a FU of 5 years were included in this study. Indications for performing TKA were painful and disabled joints caused by primary OA, posttraumatic OA and rheumatoid OA that had failed conservative treatment. Further inclusion criteria were ability and willingness to follow instructions regarding the postoperative treatment and rehabilitation, returning to FU evaluations as well as full skeletal maturity (minimum age 18 years) and a signed and understood consent form. Exclusion criteria were valgus and varus deformities > 15° or insufficient collateral ligaments requiring increased constraint, infection, osteomyelitis, previous partial or total knee replacement, previous osteotomy, skeletal immaturity as well as relative contraindications including uncooperative patients, patients with neurological disorders and incapability of following therapeutical instructions, severe osteoporosis, metabolic disorders, which may impair bone formation, osteomalacia, distant foci of infections, vascular inefficiency, neuromuscular diseases and incomplete or deficit soft tissue surrounding the knee.
Implant and surgical procedure
Implant
The cementless Vanguard Deep Dish Rotating Platform Knee (Zimmer Biomet, Warsaw, Indiana, U.S.) consists of three main primary components: Femoral, tibial and a bearing component, with the option of patella resurfacing. It uses the standard Vanguard Cruciate Retaining femoral component, which is anatomically shaped and made from cobalt–chromium molybdenum alloy with a porous coated fixation surface and a highly polished articulating surface. The finned tibial component is made of cobalt–chromium molybdenum alloy with a blasted fixation surface having a porous and hydroxyapatite coating and a highly polished articulating surface. The cruciate retaining bearing component is manufactured from ArCom® Ultra High Molecular Weight Polyethylene (UHMWPE) with a compression molded tibiofemoral articulation and a machined bearing interface. Coronally, it is matched to the curved shape of the femoral component while sagittal, it has a single radius in accordance with the femoral component’s shape in extension. Inferiorly, the surface is shaped planarly with a pivot post, which latches in the tapered hole of the tibial components and allows for rotation of the bearing component.
Surgical procedure
A single shot of 1.5 g cefuroxime or 600 mg clindamycin in case of penicillin allergy was administered as perioperative prophylaxis. There were mainly three participating orthopaedic surgeons who performed surgery according to the manufacturer’s instructions. Tourniquet was used in all cases and bone surfaces were tap-dried prior to component implantation. If necessary, lateral retinacular release was performed to ensure centralized patella tracking. Full weight bearing was permitted to all patients immediately, although usage of two crutches was recommended to each patient for 6 weeks after surgery. Thromboembolic prophylaxis was prescribed to every patient postoperatively (Low molecular weight heparin in prophylactic dosage for 4 days followed by 10 mg Rivaroxaban for 10 days). Physiotherapy was provided to each patient once per day within the hospital. Further outpatient physiotherapy was prescribed after discharge from hospital.
No experimental or investigational devices were used during this study.
Follow-up
Data collection
Data collection was conducted preoperatively, intraoperatively and postoperatively at the study centre as well as within FU visits at the outpatient clinic after 3 months, 1 year, 2 years, 3 years (optionally by phone) and 5 years. Each FU visit time point was determined based on surgery date with a maximum time window of 3 months, which was also necessary due to the ongoing COVID-19 pandemic.
Implant survival and adverse events
Reoperations of any cause as well as adverse events were registered throughout the whole FU and were categorized according to the definitions according to the standardized list and definitions of the Knee Society published by Healy et al. [12].
Radiographic assessment
Radiographic assessments consisted of weight bearing anterior posterior, skyline at 30° flexion and mediolateral view to evaluate integrity, positioning and radiolucent lines (RLL) according to the evaluation system described by Meneghini et al. [19]. As for the evaluation of the implant positioning, coronal femoral (α) and tibial component angle (β) were measured as medial angle between the anatomical femoral shaft axis and a connecting line between the medial and lateral condyle of the femoral component (α) as well as medial angle between the anatomical tibial axis and the axis of the fixation surface of the tibial component (β). Sagittal femoral (γ) and tibial component angle (σ) were measured as the angle between the anatomical femoral axis and the line perpendicular to the distal fixation surface containing the pegs of the femoral component (γ) as well as the angle between the anatomical tibial axis and the axis of the fixation surface of the tibial component (σ) according to the previously published technique described by Meneghini et al. [19]. The radiographic assessment was conducted by two authors independently using IMPAX (EE R20 XVI; Agfa HealthCare, Mortsel, Belgium).
Range of motion and patient reported outcome measures
Data to determine the clinical and functional performance were collected pre- and postoperatively applying the “American Knee Society Score” (AKSS), “Oxford Knee Score” (OKS), “Knee Injury and Osteoarthritis Outcome Score” (KOOS) and “European Quality of Life 5 Dimension 3 Level” (EQ5D). Range of Motion (ROM) was measured using a long arm goniometer [10].
This study was approved prior to commencement by the ethical review committee of the Medical Faculty of the Johannes Kepler University Linz (former ethical review committee of Upper Austria) and registered as “B-53–13” and “BMETEU.CR.EU 13”.
Statistical analysis
SPSS (version 26.0, IBM, Armonk, NY) was used for the statistical analysis. Kolmogorov–Smirnov test was performed to test for normal distribution. As for metric scaled data, arithmetic mean value and the standard deviation were calculated. These two parameters were reported as mean ± standard deviation. As for non-normally distributed metric scaled parameters, Wilcoxon Signed Rank test was performed to analyze the significance of the difference between those parameters, while t test was performed if the metric scaled parameters were normally distributed. Kaplan–Meier survival analysis was performed to analyze the survival rate of the TKA. Patients lost to FU for any reason were censored at the respective FU, if no adverse events were documented. Intra-rater and inter-rater agreements were calculated using interclass correlation coefficient (ICC). Blinded repeated measurements for intra-rater reliability were conducted at a time interval of 1 week. A sample size of 90 was calculated using data regarding the incidence of aseptic loosening available at the time the study was planned to detect the primary outcome [1]. The level of significance was defined at p ≤ 0.05.
Results
Study population and surgical information
At final FU, 91 patients were available with an average FU of 5.0 ± 0.1 years (Fig. 1, Table 1). Any adverse events in patients that did not reach the 5-year FU were accounted for.
A mid-vastus approach was performed in 77 cases (84.6%) and a medial parapatellar approach in 14 cases (15.4%). Lateral retinacular release was performed in 24 cases (26.4%). Patella resurfacing was not performed.
Implant survival and adverse events
Within the FU, there were two revisions and two reoperations as mentioned below. This resulted in an implant survival rate of 97.8% (95% CI 100–96%) with revision as endpoint (2 out of 91;) and 95.6% (95% CI 100–94%) with reoperation of any cause as endpoint (4 out of 91; Fig. 2) at the 5 years FU. No aseptic loosening was observed within the FU. Accordingly, implant survival rate with aseptic loosening as endpoint was 100% (0 out of 91).
A total of six device related adverse events occurred within the FU period. There was one case of an early periprosthetic infection occurring 3 weeks after initial surgery, which was managed with a DAIR (Fucidin acid for 6 weeks for staphylococcus epidermidis). In one case, lateralization of the patella with lateral patellar compression syndrome including pain was resolved by performing a lateral release and a patella resurfacing 10 months after the initial surgery. One patient sustained a periprosthetic distal femoral fracture 5 months after the initial surgery. Intraoperatively, the femoral component was well fixed and the fracture was successfully managed with primary fixation. In one case, postoperative wound dehiscence occurred and was managed with superficial wound revision. Another patient fell on the operated knee and suffered a bony avulsion of the medial collateral ligament which was treated conservatively using a brace. There was one case of arthrofibrosis, which was successfully treated by mobilization of the knee under anaesthesia at the 10-week mark.
Radiographic assessment
Radiographic assessment of the implant revealed no significant change in implant positioning within the FU (p > 0.05; Table 2).
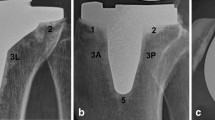
RLL surrounding the femoral or tibial component in one or more zones were detected in a total of eight cases (8.8%; Table 3, Fig. 3). All detected radiolucent lines had a width of 1 mm except for one case where the radiolucent line at zone 3 of the femoral component measured 4 mm only at the immediate postoperative radiograph.
Intra-rater ICC was 0.93, while inter-rater ICC was 0.89.
Range of motion
Compared to the values collected preoperatively, all postoperatively collected values regarding the ROM (Extension, Flexion and overall ROM) improved significantly (p < 0.05; Table 4).
Patient reported outcome measures (AKSS, OKS, KOOS, EQ5D)
The AKSS and the OKS showed a significant improvement at every FU when compared to the preoperative initial score (p < 0.05; Fig. 4). The KOOS and the EQ5D improved significantly in every subsection within the FU as well (p < 0.05; Table 5).
Discussion
The most important findings of the present study are excellent mid-term outcomes—including implant survival as well as radiographic and clinical outcomes—of the cementless Vanguard Deep Dish Rotating Platform Knee. This is the first prospective study reporting mid-term outcomes of the specific implant mentioned above.
There was a relatively low overall revision rate of 2.2% at 5 years FU with no observed case of aseptic component loosening. This is in line with other recent reports, also reporting no loosening of the uncemented tibial or femoral component after cementless TKA [30, 31]. Other reports revealed promising results regarding the revision rate due to aseptic loosening after cementless TKA with just slightly higher revision rates as well [20, 25]. Some authors, however, reported higher revision rates due to aseptic loosening after cementless TKA [3, 5]. As for possible differences regarding the rates of aseptic loosening between mobile and fixed bearing TKA previous studies revealed no significant differences between those two implant designs [11]. Nevertheless, there are hardly recent reports comparing exclusively cementless mobile bearing and fixed bearing implant designs regarding possible differences in aseptic loosening rates.
The implant survival rate within this study of 97.8% with revision as endpoint is matching results from a systematic review of the literature [18]. Comparing survival rates of cementless and cemented TKA in general, there are reports of better all-cause survivorship of cementless fixation in TKA [23], while there are also reports stating no difference in mid-term survival between cementless and cemented fixation [25, 37]. Regarding specific patient populations, cementless TKA showed a significantly lower revision rate in morbidly obese patients [2] and superior clinical outcomes with equal implant survival compared to cemented TKA in patients younger than 65 years [35].
As for the implant related complications, one case (0.9%) of periprosthetic infection occurred, which is less compared to data reported in literature [32]. Insufficient ROM leading to manipulation under anaesthesia to improve ROM was evident in one patient postoperatively (1.1%). This is also slightly less compared to other reports according to a review of literature conducted by Kornuijt et al. [14], who found rates of manipulations under anaesthesia ranging from 1.3 to 13.5% after TKA.
The radiographic evaluation revealed no significant changes in implant position within the FU (Table 3), which is in contrast to cementless unicondylar knee arthroplasty, where changes in the posterior tibial slope over time are reported [33].
Within this study, RLL, a major concern for many surgeons due to previous reports [7], occurred and disappeared within the first year after surgery. Only in one case, RLL persisted throughout the study period, but without any clinical signs of component loosening. This phenomenon has been previously described by other authors and is possibly caused by imprecise bone cuts or component positioning [36]. Regarding the difference between the occurrences of RLL in cementless vs. cemented TKA, there are various reports with different outcomes. Some authors report less RLL in cementless TKA [6], while some authors report more RLL in cementless TKA [9] and others report no difference between cementless and cemented TKA [37]. With aseptic loosening still being one of the most frequent indications for revision in TKA [28], there is a special interest in the occurrence and change over time of RLL as they also seem to be associated with dissatisfaction and pain after TKA [27]. However, the reasons for and factors leading to RLL in TKA are still subject of discussion in recent literature as they seem to be less dependent on implant design and might be triggered by implant positioning or surgical technique [4, 29]. Another reason for early RLL is bone remodeling during the ingrowth phase, during which stress shielding might occur [36].
The ROM improved at a 5-year FU (Table 4), which matches the reports of other authors in recent literature [5, 35]. This allows for managing most tasks of everyday life and is well above the minimum flexion limit of 90°, which is needed to adequately walk a set of stairs [16].
Additionally, all evaluated clinical and patient reported outcome scores including AKSS, OKS, KOOS and EQ5D showed significant improvements within the FU when compared to the preoperatively assessed values. Similar results were retrieved by other authors, who also reported a significant improvement of PROMS after cementless TKA [26].
Despite the prospective study design, there are some limitations to this study that must be considered. The patient selection for this study was conducted by the surgeons who performed TKA. Therefore, there might be a selection bias, as some patients (for example with severe osteoporosis or severe obesity) might have more likely been treated with a cemented implant alternative that was available at the centre during the study period. There were, however, no intraoperative changes of fixation due to potential bone density issue. Three surgeons performed the surgeries, which is reflected in different surgical approaches. We do not expect that the differences in approach would affect the mid-term results [17]. The surgeons were experienced in TKA. Therefore, the results of this study are not necessarily applicable on surgeons with less experience in TKA. The study was designed as a single-arm prospective study, without a comparative group. Although TKA using other implants was performed at the study centre during the study period, it was decided to solely investigate the implant mentioned above as the other implant used at the study centre was cemented with a fixed bearing inlay, which are two important and distinct variables that might have had a significant impact on the primary outcome measure. The implant can nowadays be considered of an older design, since the manufacturer now offers a more modern implant albeit not a cementless version as of writing of the manuscript. Similarly, mobile bearing is also being less used in primary arthroplasty [24]. Nevertheless, this design demonstrates encouraging results even in this version. Although component loosening was not observed, RLL were detected within the FU. However, potential component migration using radiostereometric analysis was not performed. Similarly, bone mineral density around the implant was not assessed. Lastly, the ongoing COVID-19 pandemic complicated the FU significantly. A time window of 3 months based on surgery date was allowed for FU visits, which resulted in a few patients being investigated slightly before full 5 years after surgery elapsed. Additionally, strict hygienic precautions and other pandemic related factors discouraged patients from completing the 5-year FU and, therefore, resulted in a higher number of patients lost to FU.
The present study as well as the majority of the literature demonstrate at least comparable outcomes of cementless TKA and cemented TKA. Surgeons might want to consider cementless TKA in their practice and manufacturers might want to expand their portfolio by including a cementless version of their modern implants.
Conclusion
The results of this study reveal excellent mid-term performance of a cementless deep dish rotating platform implant, with no aseptic loosening, very low revision rate, only temporarily present RLL in a minority of patients and excellent clinical results. Therefore, cementless TKA is an appropriate treatment option for patients with severe OA of the knee.
References
Ali MS, Mangaleshkar SR (2006) Uncemented rotating-platform total knee arthroplasty: a 4-year to 12-year follow-up. J Arthroplasty 21:80–84
Bagsby DT, Issa K, Smith LS, Elmallah RK, Mast LE, Harwin SF, Mont MA, Bhimani SJ, Malkani AL (2016) Cemented vs cementless total knee arthroplasty in morbidly obese patients. J Arthroplasty 31:1727–1731
Behery OA, Kearns SM, Rabinowitz JM, Levine BR (2017) Cementless vs cemented tibial fixation in primary total knee arthroplasty. J Arthroplasty 32:1510–1515
Behrend H, Hochreiter B, Potocnik P, El Baz Y, Zdravkovic V, Tomazi T (2020) No difference in radiolucent lines after TKA: a matched-pair analysis of the classic implant and its evolutional design. Knee Surg Sports Traumatol Arthrosc 28:3962–3968
Bouras T, Bitas V, Fennema P, Korovessis P (2017) Good long-term results following cementless TKA with a titanium plasma coating. Knee Surg Sports Traumatol Arthrosc 25:2801–2808
Chen C, Shi Y, Wu Z, Gao Z, Chen Y, Guo C, Bao X (2021) Long-term effects of cemented and cementless fixations of total knee arthroplasty: a meta-analysis and systematic review of randomized controlled trials. J Orthop Surg Res 16:590–590
Chockalingam S, Scott G (2000) The outcome of cemented vs. cementless fixation of a femoral component in total knee replacement (TKR) with the identification of radiological signs for the prediction of failure. Knee 7:233–238
Dalury D (2016) Cementless total knee arthroplasty: current concepts review. Bone Joint J 98-B:867–873
Fricka KB, Sritulanondha S, McAsey CJ (2015) To cement or not? two-year results of a prospective, randomized study comparing cemented vs. cementless total knee arthroplasty (TKA). J Arthroplasty 30:55–58
Hancock GE, Hepworth T, Wembridge K (2018) Accuracy and reliability of knee goniometry methods. J Exp Orthop 5:46
Hantouly AT, Ahmed AF, Alzobi O, Toubasi A, Salameh M, Elmhiregh A, Hameed S, Ahmed GO, Alvand A, Al Dosari MAA (2022) Mobile-bearing versus fixed-bearing total knee arthroplasty: a meta-analysis of randomized controlled trials. Eur J Orthop Surg Traumatol 32:481–495
Healy WL, Della Valle CJ, Iorio R, Berend KR, Cushner FD, Dalury DF, Lonner JH (2013) Complications of total knee arthroplasty: standardized list and definitions of the knee society. Clin Orthop Relat Res 471:215–220
Kane R, Saleh K, Wilt T, Bershadsky B (2005) The functional outcomes of total knee arthroplasty. J Bone Jt Surg Am 87:1719–1724
Kornuijt A, Das D, Sijbesma T, de Vries L, van der Weegen W (2018) Manipulation under anesthesia following total knee arthroplasty: a comprehensive review of literature. Musculoskelet Surg 102:223–230
Kurtz SM, Lau E, Ong K, Zhao K, Kelly M, Bozic KJ (2009) Future young patient demand for primary and revision joint replacement: National Projections from 2010 to 2030. Clin Orthop Rel Res 467:2606–2612
Laubenthal KN, Smidt GL, Kettelkamp DB (1972) A quantitative analysis of knee motion during activities of daily living. Phys Ther 52:34–43
Lechner R, Lazzeri M, Oberaigner W, Nardelli P, Roth T, Köglberger P, Krismer M, Liebensteiner MC (2021) Does the type of surgical approach affect the clinical outcome of total knee arthroplasty? Orthopade 50:674–680
van der List JP, Sheng DL, Kleeblad LJ, Chawla H, Pearle AD (2017) Outcomes of cementless unicompartmental and total knee arthroplasty: a systematic review. Knee 24:497–507
Meneghini RM, Mont MA, Backstein DB, Bourne RB, Dennis DA, Scuderi GR (2015) Development of a modern knee society radiographic evaluation system and methodology for total knee arthroplasty. J Arthroplasty 30:2311–2314
Miller AJ, Stimac JD, Smith LS, Feher AW, Yakkanti MR, Malkani AL (2018) Results of cemented vs cementless primary total knee arthroplasty using the same implant design. J Arthroplasty 33:1089–1093
Milligan DJ, O’Brien S, Doran E, Gallagher NE, Beverland DE (2019) Twenty-year survivorship of a cemented mobile bearing total knee arthroplasty. Knee 26:933–940
Nam D, Lawrie CM, Salih R, Nahhas CR, Barrack RL, Nunley RM (2019) Cemented versus cementless total knee arthroplasty of the same modern design: a prospective, randomized trial. J Bone Jt Surg Am 101:1185–1192
Newman JM, Sodhi N, Dekis JC, Khlopas A, Piuzzi NS, Sultan AA, Levin JM, Mont MA (2020) Survivorship and functional outcomes of cementless versus cemented total knee arthroplasty: a meta-analysis. J Knee Surg 33:270–278
Nguyen L-CL, Lehil MS, Bozic KJ (2015) Trends in total knee arthroplasty implant utilization. J Arthroplasty 30:739–742
Quispel CR, Duivenvoorden T, Beekhuizen SR, Verburg H, Spekenbrink-Spooren A, Van Steenbergen LN, Pasma JH, De Ridder R (2021) Comparable mid-term revision rates of primary cemented and cementless total knee arthroplasties in 201,211 cases in the Dutch Arthroplasty Register (2007–2017). Knee Surg Sports Traumatol Arthrosc 29:3400–3408
Restrepo S, Smith EB, Hozack WJ (2021) Excellent mid-term follow-up for a new 3D-printed cementless total knee arthroplasty. Bone Jt J 103-B:32–37
Sadoghi P, Leithner A, Weber P, Friesenbichler J, Gruber G, Kastner N, Pohlmann K, Jansson V, Wegener B (2011) Radiolucent lines in low-contact-stress mobile-bearing total knee arthroplasty: a blinded and matched case control study. BMC Musculoskelet Disord 12:142–142
Sharkey PF, Lichstein PM, Shen C, Tokarski AT, Parvizi J (2014) Why are total knee arthroplasties failing today—has anything changed after 10 years? J Arthroplasty 29:1774–1778
Staats K, Wannmacher T, Weihs V, Koller U, Kubista B, Windhager R (2019) Modern cemented total knee arthroplasty design shows a higher incidence of radiolucent lines compared to its predecessor. Knee Surg Sports Traumatol Arthrosc 27:1148–1155
Stempin R, Stempin K, Kaczmarek W, Dutka J (2018) Midterm results of cementless total knee arthroplasty: a retrospective case series. Open Orthop J 12:196–202
Tarazi J, Salem H, Ehiorobo J, Sodhi N, Mont M, Harwin S (2020) Cementless tritanium baseplate total knee arthroplasty: survivorship and outcomes at 5-year minimum follow-up. J Knee Surg 33:862–865
Thompson O, W-Dahl A, Lindgren V, Gordon M, Robertsson O, Stefánsdóttir A (2022) Similar periprosthetic joint infection rates after and before a national infection control program: a study of 45,438 primary total knee arthroplasties. Acta Orthop 93:3–10
Veizi E, Fırat A, Tecimel O, Çepni Ş, Subaşı İÖ, Kılıçarslan K (2021) The change in posterior tibial slope after cementless unicondylar knee arthroplasty. J Arthroplasty 36:1784–1791
Wagenmakers R, Stevens M, Groothoff JW, Zijlstra W, Bulstra SK, van Beveren J, van Raaij JJAM, van den Akker-Scheek I (2011) Physical activity behavior of patients 1 year after primary total hip arthroplasty: a prospective multicenter cohort study. Phys Ther 91:373–380
Wang K, Sun H, Zhang K, Li S, Wu G, Zhou J, Sun X (2020) Better outcomes are associated with cementless fixation in primary total knee arthroplasty in young patients: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore) 99:e18750–e18750
Wautier D, Ftaïta S, Thienpont E (2020) Radiolucent lines around knee arthroplasty components: a narrative review. Acta Orthop Belg 86:82–94
Zhou K, Yu H, Li J, Wang H, Zhou Z, Pei F (2018) No difference in implant survivorship and clinical outcomes between full-cementless and full-cemented fixation in primary total knee arthroplasty: a systematic review and meta-analysis. Int J Surg 53:312–319
Funding
Open access funding provided by Johannes Kepler University Linz. This study was sponsored from July 2013 until January 2020 by Zimmer Biomet. Zimmer Biomet prematurely terminated sponsoring of the study in January 2020. From then on, the study was funded by the Kepler University Hospital.
Author information
Authors and Affiliations
Contributions
CS: data analysis and interpretation, original draft preparation; MH: data acquisition, original draft preparation; ML: original draft preparation; MS: data acquisition; BR: data acquisition; TG: draft review and editing; AK: supervision, data interpretation, draft review and editing.
Corresponding author
Ethics declarations
Conflict of interest
Stöbich M. and Ruhs B.: Zimmer Biomet Europe: Financial compensation for conducting the follow-up and filling out the study forms of this study. Gotterbarm T.: Zimmer Biomet Europe: Grant, personal fees; Depuy Synthes Orthopedics: Grant, personal fees; Mathys AG: Grant, personal fees; Medacta: Personal fees. Klasan A.: Implancast GmbH: paid presentations; Stryker GmbH: consultant; Archives of Orthopaedic and Trauma Surgery: Editorial Board Member. The other authors have no conflicts of interests to declare.
Ethical approval
This study was approved prior to commencement by the ethical review committee of the Medical Faculty of the Johannes Kepler University Linz (former ethical review committee of Upper Austria) and registered as “B-53-13” and “BMETEU.CR.EU 13”.
Informed consent
Informed consent was obtained from all patients included in this study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Stadler, C., Hofstätter, M., Luger, M. et al. No component loosening of a cementless deep dish rotating platform knee at a 5-year follow-up. Knee Surg Sports Traumatol Arthrosc 31, 969–978 (2023). https://doi.org/10.1007/s00167-022-07113-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07113-0