Abstract
Purpose
It is unclear whether the results of arthroscopic partial meniscectomy (APM) are comparable to a structured physical therapy (PT). This systematic review investigated efficacy of APM in the management of symptomatic meniscal damages in middle aged patients. Current available randomised controlled trials (RCTs) which compared APM performed in isolation or combined with physical therapy versus sham arthroscopy or isolated physical therapy were considered in the present systematic review.
Methods
This systematic review was conducted according to the 2020 PRISMA statement. All the level I RCTs which investigated the efficacy of AMP were accessed. Studies which included elderlies with severe OA were not eligible, nor were those in which APM was combined with other surgical intervention or in patients with unstable knee or with ligaments insufficiency. The risk of bias was assessed using the software Review Manager 5.3 (The Nordic Cochrane Collaboration, Copenhagen). To rate the quality of evidence of collected outcomes, the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) was used.
Results
Data from 17 studies (2037 patients) were collected. 48.5% (988 of 2037 patients) were women. The mean age of the patients was 52.7 ± 3.9 years, the mean BMI 27.0 ± 1.3 kg/m2. The current evidence suggests no difference in functional PROMs (quality of the evidence: high), clinical PROMs (quality of the evidence: high), pain (quality of the evidence: high), quality of life (quality of the evidence: high), physical performance measures (quality of the evidence: moderate), and OA progression (quality of the evidence: moderate).
Conclusions
The benefits of APM in adults with degenerative and nonobstructive meniscal symptoms are limited. The current evidence reports similarity in the outcome between APM and PT. Further long-term RCTs are required to investigate whether APM and PT produce comparable results using validated and reliable PROMs. Moreover, future RCTs should investigate whether patients who might benefit from APM exist, clarifying proper indications and outcomes. High quality investigations are strongly required to establish the optimal PT regimes.
Level of evidence
Level I.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Degenerative meniscal damage is common in adults [14, 27]. At present, the optimal management for non-traumatic, degenerative meniscal damage remains controversial [8, 38]. Meniscal tears are defined as intrameniscal linear signal penetrating one or both surfaces of the meniscus at magnetic resonance imaging (MRI) [10]. Arthroscopic partial meniscectomy (APM) has been advocated to manage degenerative and obstructive (i.e., inducing locking of the knee joint) meniscal damage [8, 22]. However, in adults with degenerative and nonobstructive meniscal symptoms the superiority of APM over a well-structured physical therapy (PT) programme is debated [1, 9, 19, 35, 44, 47, 54]. Previous systematic reviews were inconsistent and found none to slightly better outcome in APM compared to PT [1, 9, 19, 33, 35, 44, 47, 54, 57, 59]. However, additional long-term randomised controlled trials (RCTs) [4, 6, 40, 42] and additional follow-up of previously published pivotal RCTs [31, 51], which have not yet been included in any previous systematic review, have been recently published. Therefore, an update of the clinical evidence is necessary.
This systematic review investigated the efficacy of APM in the management of symptomatic meniscal damage in middle aged patients. Current available RCTs which compared APM performed in isolation or combined with PT versus sham APM or isolated PT were considered in the present investigation. It was hypothesized that AMP is not superior compared to PT or sham APM in patient reported outcome measures (PROMs), physical performance measures, and progression of osteoarthritis (OA).
Materials and methods
Eligibility criteria
All the clinical trials which investigated the efficacy of AMP were accessed. Given the authors language capability, articles in English, German, Italian, French, and Spanish were eligible. Only RCTs with level I of evidence, according to Oxford Centre of Evidence-Based Medicine [25], were considered. Animal, biomechanics, and computational studies were not considered. Reviews, comments, editorials, and expert opinion were not eligible. Studies which included patients with severe OA (Kellgren–Lawrence IV) were not included. Studies which investigated patients with acute meniscal tears or mechanical symptoms were not eligible. Studies in patients older than 70 years were not included, nor those conducted in skeletally immature patients. Studies in which APM was combined with other surgical intervention were excluded. Studies which included patients with unstable knee or ligaments insufficiency were not eligible. Only studies which investigated patients who underwent exclusively isolated APM or APM combined with PT were included. Studies which reported data on patients who received meniscal allografts or bio-scaffolds were not considered.
Search strategy
This systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA 2020 statement) [43]. The following algorithm was preliminarily set out:
-
Population: adults aged 30–70.
-
Problem: degenerative and nonobstructive meniscal damage.
-
Intervention: APM in isolation or combined to PT.
-
Comparison: PT, sham arthroscopy.
-
Outcomes: PROMs, physical performance measures, OA progression.
-
Study design: RCT.
-
Duration: minimum 3 month follow-up.
In March 2022, the following databases were accessed: Pubmed, Web of Science, Google Scholar, Embase. No time constrains were used for the search. The following keywords were used in combination using the Boolean operators: ((knee OR meniscus OR meniscal OR meniscopathy) AND (damage OR injury OR tear OR pain) AND/OR (symptoms OR overuse OR degenerative OR nonobstructive OR mechanical OR locking)) AND ((arthroscopy OR arthroscopic) AND partial meniscectomy) AND/OR (physical AND/OR therapy OR exercises OR training OR physiotherapy OR rehabilitation)) AND (outcome OR return OR patient reported outcome measures OR proms OR vas OR visual analog scale OR womac OR Western ontario and mcmaster universities osteoarthritis index OR koos OR knee injury and osteoarthritis outcome score OR osteoarthrosis OR Kellgren–Lawrence OR performances).
Selection and data collection
Two authors (F.M and F.C.) independently performed the database search. All the resulting titles were screened, and if suitable, the abstract was accessed. The full-text of the abstracts which matched the topic were accessed. The bibliography of the full-text articles was also screened by hand for inclusion. Any disagreements were discussed and settled by a third author (**).
Data items
Two authors (F.M. and F.C.) independently performed data extraction. Study generalities were collected: author, year, level of evidence, study design, length of the follow-up, type of treatment, physical therapy or home exercise protocol, number of patients and related mean age and body mass index (BMI). At each follow-up, data concerning PROMs, physical performance measures, and progression of OA were collected.
Study risk of bias assessment
Two reviewers (F.M. and F.C.) independently evaluated the risk of bias of the extracted studies according to the Cochrane Handbook for Systematic Reviews of Interventions guidelines [11]. The risk of bias was assessed using the software Review Manager 5.3 (The Nordic Cochrane Collaboration, Copenhagen). The following endpoints were evaluated: selection, detection, performance, attrition, reporting, and other bias. The selection bias rates the method used to generate the allocation sequence. The detection and performance biases investigate the quality of blinding methods of assessor and patients, respectively. Attrition bias refers to the quality of outcome data for each study endpoint, evaluating attrition and exclusions in the study. Reporting bias explores the possibility of selective outcome reporting by the authors.
Quality of recommendations
To rate the quality of evidence of collective outcomes the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) system was used [2, 21]. The GRADE was performed by two authors (F.M. and F.C.). The GRADE is a sensitive and transparent tool to rate the quality of the recommendations which arise from the included studies, assessing the reliability of scientific evidence and formulating evidence-based clinical recommendations.
Statistical analyses
The statistical analyses were performed using the software IBM SPSS version 25. For continuous variable, the arithmetic mean and standard deviation was used.
Results
Study selection
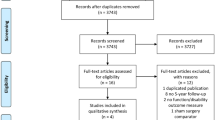
A total of 2545 studies resulted from the databases search. Of them, 1113 were excluded as they were duplicates. A further of 1415 studies were excluded with reason: not focusing on APM (N = 523), combining APM with other surgical interventions (N = 78), investigating APM in the elderlies or young population and/or in advanced OA (N = 89), not reporting the clinical or imaging outcomes of APM (N = 28), including patients with mechanical symptoms (N = 8), study design (N = 684), language limitations (N = 5). Finally, 17 RCTs were included in the present systematic review. The flow chart of the literature search is shown in Fig. 1.
Study risk of bias assessment
Given the high quality of randomisation and allocation concealment in most studies, the overall risk of selection bias was low. Performance bias was moderate, as only four RCTs (two authors), which evaluated the efficacy of sham arthroscopy versus APM, were conducted in a double blinded fashion. Detection bias was low to moderate, since few studies did not conduct assessors blinding. Detection and attrition biases were low, the risk of other biases was low to moderate. Concluding, the overall risk of publication bias was low, attesting to the present systematic review a good quality of the methodological quality assessment (Fig. 2).
Study characteristics and results of individual studies
Data from 2,037 patients were collected. 48.5% (988 of 2037 patients) were women. The mean age of the patients was 52.7 ± 3.9 years, and the mean BMI 27.0 ± 1.3 kg/m2. Table 1 shows the generalities, patient demographic, and the type of PROMs referred in the included studies.
Quality of recommendations
The GRADE found an overall high quality of recommendations. PROMs which evaluated the quality of life, pain, and the clinical and the functional outcome were clearly reported, unbiased, and with minimal inconsistencies. Heterogeneities were found in physical performance measures and OA progression. Concluding, the GRADE results in a moderate to high certainly of the evidence (Fig. 3).
Discussion
According to the main findings of the present systematic review, there is no evidence in support of APM in adults with non-traumatic and nonobstructive meniscal damages. No difference was found in PROMs (Figs. 2, 3) and progression of OA between APM and PT. Physical performance measures, as expected, were worse in APM compared to PT. Adults with non-traumatic and degenerative meniscal damage could benefit from a personalized and performance and progression-based physical therapy program, whose goals should be to increase neuromuscular control and muscles strength, to achieve compensatory functional stability of the lower limb, optimize shock-absorbing function of the lower extremity muscles, and enhancing joint stability (Figs. 4, 5).
Similar to the present study, several previous systematic reviews found no evidence in support of APM over the PT [1, 9, 19, 47, 54]. On the contrary, Van de Graaf et al. [59] in a systematic review of five RCTs found that APM yielded better functional outcomes and pain control at 3–6 months, whereas from 12 to 24 months the results were comparable. Li et al. [35] systematically reviewed six RCTs showing better results from APM up to 12 months, and no difference after 24 months. Pan et al. [44] conducted a systematic review on six RCTs comparing APM combined with PT versus PT in isolation. APM combined with PT was more effective to improve range of motion and pain control in the early postoperative period.
Two RCTs investigated APM versus sham APM [50,51,52,53]. Overall, these RCTs found that isolated APM versus sham APM provided comparable results [50,51,52,53]. Sihvonen et al. [51,52,53] compared 146 patients undergoing APM versus sham APM. At 12 and 24 month follow-up no difference was found in Lysholm and Western Ontario Meniscal Evaluation Tool (WOMET), and in VAS after training [52, 53]. At 60 month follow-up, there was a consistent, slightly greater risk for progression of OA and mechanical symptoms in the APM group, although no relevant between-group differences in PROMs were reported [51]. Similar entry criteria were used by Roos et al. [50], which randomly allocated 44 patients aged 35–55 years to receive APM or sham APM. At 24 month follow-up, the KOOS and all its subscales were similar between the two groups [50]. Similarity was also found in EQ5D, VAS, SF36, and Global Perceived Effect (GPE) [50]. Physical performance measures, such as the one-leg hop test (both legs), knee bending test (both legs), and the isometric knee extensor strength (both legs) were also similar between APM and sham APM [50].
Seven studies compared isolated APM versus isolated PT [4, 6, 34, 40, 42, 58, 60]. Overall, these RCTs found no clinical and imaging benefits of APM over isolated PT [4, 6, 34, 40, 42, 58, 60]. Previous evidence found that, in patients assigned to physical therapy who eventually needed surgery, the delay resulting from a trial of conservative management did not impair the outcomes at 12 months after the initial presentation [26]. Van de Graaf [58] compared APM versus PT in 321 patients aged 45–70 years. At 24 month follow-up PT was non inferior to APM for knee function in IKDC, VAS, RAND-36 Physical Component Score, Tegner Activity Scale, and progression of OA using the Kellgren–Lawrence scale. Noorduyn et al. [40] investigated the effectiveness of early APM versus PT in patients aged 45–70 years with a symptomatic meniscal tear. At 2 year follow-up, no relevant difference between the two cohorts in the Dutch version of the Patient-Specific Functional Scale (PSFS) were evidenced [40]. Kise et al. [34] compared PT versus APM in 140 adults aged 35–60 years. At 3, 12, and 24 months, no clinically relevant benefit of APM over PT was found in KOOS and adverse events [34]. As expected, muscle strength had greatly improved in the PT group at 3 months [34]. 19% (30 of 70 patients) allocated to PT underwent APM, with no additional benefit within the 2 year follow-up [34]. Basar et al. [4] randomly allocated 192 patients to APM versus PT. The authors also evaluated whether the addition of hyaluronic acid promoted additional benefit in WOMAC, VAS, and range of motion. At 2 and 6 month follow-up, no difference was found in PROMs; however, the PT group demonstrated greater range of motion. Finally, the use of hyaluronic acid did not produce any clinical benefit in either group. The inefficacy of intraarticular infiltrations in APM, such as hyaluronic acid and/or platelet rich plasma (PRP), is also supported by previous evidence [5, 12, 13, 15, 20, 28, 29, 32, 38, 45]. Berg et. [6] conducted a RCT on 140 patients aged 35–60, 96% of them without evidence of OA at imaging. At 5 year follow-up, both groups reported similar progression of radiographic features (joint space narrowing, medial and lateral osteophytes) and comparable incidence of OA [6]. No difference was found in KOOS at 5 year follow-up [6]. Moreover, no statistically significant or clinically relevant improvement of the subscales of the KOOS were found from baseline to last follow-up in both groups. Osteras et al. [42] randomly allocated 17 adults with meniscal symptoms lasting > 3 months and suitable for APM to receive PT or APM. At 3 months, there was no difference in VAS and KOOS [42]. The authors examined also the dynamic quadriceps muscle strength [24], which was similar between the groups. However, at 3 month follow-up, the PT group demonstrated less anxiety and depression according to the Hospital Anxiety and Depression Scale (HAD) [42]. Yim et al. [60] conducted an RCT comparing APM versus PT in patients with degenerative horizontal tear of the medial meniscus. The authors found no differences in VAS, Lysholm score, Tegner activity scale, and patient subjective knee pain and satisfaction at 2 year follow-up [60].
Six RCTs compared APM combined with PT versus PT in isolation [18, 22, 23, 30, 31, 55]. Herrlin et al. [22, 23] compared APM combined with PT versus PT in isolation in 90 patients. At 6, 24, and 60 month follow-up, KOOS, Lysholm, Tegner, and VAS were similar between APM combined with PT and PT alone [22, 23]. No difference in OA progression was found in both cohorts at 5 year follow-up [22, 23]. Katz et al. [30, 31] randomly assigned 351 patients older than 45 with Kellgren–Lawrence 0–II to undergo APM combined with PT or PT in isolation. At 6 and 12 months postoperatively, 30% of patients allocated to PT had decided to undergo surgery, and 6% of patients assigned to APM had decided not to undergo surgery [30]. The KOOS pain and subscale function of the WOMAC did not evidence difference between the two groups at 3, 6, 12, 24, 36, and 48 months [31]. At 60 month follow-up, 9.2% and 5.1% of patients allocated, respectively, to APM and PM underwent total knee replacement [31]. Gauffin et al. [18] randomly allocated 150 patients to APM combined with PT or isolated PT. At 3 and 12 month follow-up, the combined APM and PT group reported greater pain subscale of the KOOS. No other difference was found in EuroQol (EQ5D) [46] and VAS [18]. Stensrud et al. [55] compared APM in combination with PT versus PT in isolation. They included 82 patients with symptomatic unilateral, nontraumatic, meniscus tears, aged 35–60. At 3 months, the PT group evidenced greater quadriceps function, isokinetic knee extension and flexion peak torque [55]. No difference was found at 3 months in the maximum number of knee-bends in 30 s, the one-leg hop for distance, and the 6 min timed hop [55]. These functional tests have been validated in patients with meniscal symptoms [3, 7, 41, 49].
The results of the present study should be considered in the light of several limitations. Patients allocated to APM did not undergo an individualized and supervised rehabilitation program but a program of structured home exercises. This program was heterogeneous in content, intensity, and duration. Similar considerations are applicable to the PT group: though all the physiotherapy programmes aimed to increase neuromuscular control and muscle strength, some differences in methods, content, intensity, and duration were evident. Most studies included in the present investigation did not blind the patients to the treatment allocation. However, a blinded allocation is hardly possible in the comparison of APM and PT and it must be pointed out by us. The RCTs which evaluated the efficacy of sham arthroscopy versus APM were conducted in a double blinded fashion. Assessors were often not blinded to the patient treatment, increasing the detection bias. In some RCTs, many patients allocated to PT crossed over, undergoing APM before assessment of the primary outcome. Moreover, some inconsistencies in VAS score must be pointed out. Some authors did not report whether VAS referred to the pain at rest, during sports, or during daily activities. The location, type, and degree of the lesions in the meniscus were often biased; therefore, it was not possible to evaluate the efficacy of APM in these subgroups. In this respect, the reliability of the conclusion of the present systematic review are not fully generalisable. Future studies should evaluate the efficacy and safety of APM for each specific place, type, and degree of meniscal lesion. The presence of chondral defects was seldom considered for patient eligibility. Chondral defects are common, especially in middle aged adults [17, 48]. Given the limited healing potential of hyaline cartilage, these lesions are most likely unable to regenerate [16, 37]. If left untreated, patients with chondral defects may experience chronic instability, pain, and early onset osteoarthritis, along with significant reduction in the quality of life and participation to recreational activities [36, 39]. Most studies investigated PROMs and imaging findings to assess knee degeneration. However, no other imaging methodology has been used to verify whether additional modifications to the meniscus occurred at the end of the follow-up. The description of surgical technique was not adequately reported in some studies, representing a further limitation. Moreover, the included studies referred to different PROMs, which produce high variability in the endpoints. Given the lack of available pooling data, along with the heterogeneous PROMs used by the authors, further subgroup analyses were not possible. Moreover, the use of PROMs was inadequate in most studies. PROMs which focus on meniscus (i.e., Western Ontario Meniscal Evaluation Tool, WOMET) have been used only in one study. The degree of OA according to the Kellgren–Lawrence scale was slightly variable; however, no study included patients with Kellgren–Lawrence IV. Similar considerations apply for the age of the patients. The rage of patients age was wide (from 35 to 70 years), which may lead to increase the selection bias.
Further long-term RCTs are required to investigate whether APM and PT produces comparable results using validated and reliable PROMs. Moreover, future RCTs should investigate whether patients who might benefit from APM actually exist, clarifying proper indications and outcomes. In the current literature, little is published on prognosticators of the outcome of PT and on results of crossover to surgery for meniscal damage. Although rehabilitation is important for meniscus healing in meniscus ailments or following arthroscopy, the optimal rehabilitation regimen has also not been established. These issues should be addressed by future investigations.
Conclusions
The benefits of APM in adults with degenerative and nonobstructive meniscal symptoms are limited. The current evidence reports similarity in the outcome between APM and PT. Further long-term RCTs are required to investigate whether APM and PT produces comparable results using validated and reliable PROMs. Moreover, future RCTs should investigate whether patients who might benefit from APM exist, clarifying proper indications and outcomes. High quality investigations are strongly required to establish the optimal PT regimes.
Availability of data and materials
the data sets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Abram SGF, Hopewell S, Monk AP, Bayliss LE, Beard DJ, Price AJ (2020) Arthroscopic partial meniscectomy for meniscal tears of the knee: a systematic review and meta-analysis. Br J Sports Med 54:652–663
Balshem H, Helfand M, Schunemann HJ, Oxman AD, Kunz R, Brozek J et al (2011) GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol 64:401–406
Barber SD, Noyes FR, Mangine RE, McCloskey JW, Hartman W (1990) Quantitative assessment of functional limitations in normal and anterior cruciate ligament-deficient knees. Clin Orthop Relat Res 255:204–214
Basar B, Basar G, Buyukkuscu MO, Basar H (2021) Comparison of physical therapy and arthroscopic partial meniscectomy treatments in degenerative meniscus tears and the effect of combined hyaluronic acid injection with these treatments: a randomized clinical trial. J Back Musculoskelet Rehabil 34:767–774
Belk JW, Kraeutler MJ, Thon SG, Littlefield CP, Smith JH, McCarty EC (2020) Augmentation of meniscal repair with platelet-rich plasma: a systematic review of comparative studies. Orthop J Sports Med 8:2325967120926145
Berg B, Roos EM, Englund M, Kise NJ, Tiulpin A, Saarakkala S et al (2020) Development of osteoarthritis in patients with degenerative meniscal tears treated with exercise therapy or surgery: a randomized controlled trial. Osteoarthr Cartil 28:897–906
Bremander AB, Dahl LL, Roos EM (2007) Validity and reliability of functional performance tests in meniscectomized patients with or without knee osteoarthritis. Scand J Med Sci Sports 17:120–127
Castle JP, Khalil LS, Abbas MJ, DeBolle S, Tandron M, Cross AG et al (2022) Maximum subjective outcome improvement is reported by 3 months following arthroscopic partial meniscectomy: a systematic review. J Orthop 31:78–85
Choi M, Lee SJ, Park CM, Ryoo S, Kim S, Jang JY et al (2021) Arthroscopic partial meniscectomy versus physical therapy for degenerative meniscal tear: a systematic review. J Korean Med Sci 36:e292
Crues JV 3rd, Mink J, Levy TL, Lotysch M, Stoller DW (1987) Meniscal tears of the knee: accuracy of MR imaging. Radiology 164:445–448
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP et al (2019) Updated guidance for trusted systematic reviews: a new edition of the Cochrane handbook for systematic reviews of interventions. Cochrane Database Syst Rev 10:ED000142
Dai WL, Zhang H, Lin ZM, Shi ZJ, Wang J (2019) Efficacy of platelet-rich plasma in arthroscopic repair for discoid lateral meniscus tears. BMC Musculoskelet Disord 20:113
Duif C, Vogel T, Topcuoglu F, Spyrou G, von Schulze PC, Lahner M (2015) Does intraoperative application of leukocyte-poor platelet-rich plasma during arthroscopy for knee degeneration affect postoperative pain, function and quality of life? A 12-month randomized controlled double-blind trial. Arch Orthop Trauma Surg 135:971–977
Dzidzishvili L, Lopez T II, Saez D, Arguello JM, Calvo E (2021) A comparison of the transtibial pullout technique and all-inside meniscal repair in medial meniscus posterior root tear: Prognostic factors and midterm clinical outcomes. J Orthop 26:130–134
Everhart JS, Cavendish PA, Eikenberry A, Magnussen RA, Kaeding CC, Flanigan DC (2019) Platelet-rich plasma reduces failure risk for isolated meniscal repairs but provides no benefit for meniscal repairs with anterior cruciate ligament reconstruction. Am J Sports Med 47:1789–1796
Filardo G, Perdisa F, Roffi A, Marcacci M, Kon E (2016) Stem cells in articular cartilage regeneration. J Orthop Surg Res 11:42
Flanigan DC, Harris JD, Trinh TQ, Siston RA, Brophy RH (2010) Prevalence of chondral defects in athletes’ knees: a systematic review. Med Sci Sports Exerc 42:1795–1801
Gauffin H, Tagesson S, Meunier A, Magnusson H, Kvist J (2014) Knee arthroscopic surgery is beneficial to middle-aged patients with meniscal symptoms: a prospective, randomised, single-blinded study. Osteoarthr Cartil 22:1808–1816
Giuffrida A, Di Bari A, Falzone E, Iacono F, Kon E, Marcacci M et al (2020) Conservative vs. surgical approach for degenerative meniscal injuries: a systematic review of clinical evidence. Eur Rev Med Pharmacol Sci 24:2874–2885
Griffin JW, Hadeed MM, Werner BC, Diduch DR, Carson EW, Miller MD (2015) Platelet-rich plasma in meniscal repair: does augmentation improve surgical outcomes? Clin Orthop Relat Res 473:1665–1672
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J et al (2011) GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol 64:383–394
Herrlin S, Hallander M, Wange P, Weidenhielm L, Werner S (2007) Arthroscopic or conservative treatment of degenerative medial meniscal tears: a prospective randomised trial. Knee Surg Sports Traumatol Arthrosc 15:393–401
Herrlin SV, Wange PO, Lapidus G, Hallander M, Werner S, Weidenhielm L (2013) Is arthroscopic surgery beneficial in treating non-traumatic, degenerative medial meniscal tears? A five year follow-up. Knee Surg Sports Traumatol Arthrosc 21:358–364
Holm I, Hammer S, Larsen S, Nordsletten L, Steen H (1995) Can a regular leg extension bench be used in testing deficits of the quadriceps muscle during rehabilitation? Scand J Med Sci Sports 5:29–35
Howick J CI, Glasziou P, Greenhalgh T, Carl Heneghan, Liberati A, Moschetti I, Phillips B, Thornton H, Goddard O, Hodgkinson M (2011) The 2011 Oxford CEBM levels of evidence. oxford centre for evidence-based medicine. https://www.cebm.net/index.aspx?o=5653. Accessed Jan 2022
Hwang YG, Kwoh CK (2014) The METEOR trial: no rush to repair a torn meniscus. Cleve Clin J Med 81:226–232
Kaiser JT, Meeker ZD, Horner NS, Sivasundaram L, Wagner KR, Mazra AF et al (2022) Meniscal ramp lesions—skillful neglect or routine repair? J Orthop 32:31–35
Kaminski R, Kulinski K, Kozar-Kaminska K, Wielgus M, Langner M, Wasko MK et al (2018) A prospective, randomized, double-blind, parallel-group, placebo-controlled study evaluating meniscal healing, clinical outcomes, and safety in patients undergoing meniscal repair of unstable, complete vertical meniscal tears (bucket handle) augmented with platelet-rich plasma. Biomed Res Int 2018:9315815
Kaminski R, Maksymowicz-Wleklik M, Kulinski K, Kozar-Kaminska K, Dabrowska-Thing A, Pomianowski S (2019) Short-term outcomes of percutaneous trephination with a platelet rich plasma intrameniscal injection for the repair of degenerative meniscal lesions. A prospective, randomized, double-blind, parallel-group, placebo-controlled study. Int J Mol Sci 20:865
Katz JN, Brophy RH, Chaisson CE, de Chaves L, Cole BJ, Dahm DL et al (2013) Surgery versus physical therapy for a meniscal tear and osteoarthritis. N Engl J Med 368:1675–1684
Katz JN, Shrestha S, Losina E, Jones MH, Marx RG, Mandl LA et al (2020) Five-year outcome of operative and nonoperative management of meniscal tear in persons older than forty-five years. Arthritis Rheumatol 72:273–281
Kemmochi M, Sasaki S, Takahashi M, Nishimura T, Aizawa C, Kikuchi J (2018) The use of platelet-rich fibrin with platelet-rich plasma support meniscal repair surgery. J Orthop 15:711–720
Khan M, Evaniew N, Bedi A, Ayeni OR, Bhandari M (2014) Arthroscopic surgery for degenerative tears of the meniscus: a systematic review and meta-analysis. CMAJ 186:1057–1064
Kise NJ, Risberg MA, Stensrud S, Ranstam J, Engebretsen L, Roos EM (2016) Exercise therapy versus arthroscopic partial meniscectomy for degenerative meniscal tear in middle aged patients: randomised controlled trial with two year follow-up. BMJ 354:i3740
Li J, Zhu W, Gao X, Li X (2020) Comparison of arthroscopic partial meniscectomy to physical therapy following degenerative meniscus tears: a systematic review and meta-analysis. Biomed Res Int 2020:1709415
Litwic A, Edwards MH, Dennison EM, Cooper C (2013) Epidemiology and burden of osteoarthritis. Br Med Bull 105:185–199
Mei-Dan O, Carmont MR, Laver L, Mann G, Maffulli N, Nyska M (2012) Platelet-rich plasma or hyaluronate in the management of osteochondral lesions of the talus. Am J Sports Med 40:534–541
Migliorini F, Cuozzo F, Cipollaro L, Oliva F, Hildebrand F, Maffulli N (2022) Platelet-rich plasma (PRP) augmentation does not result in more favourable outcomes in arthroscopic meniscal repair: a meta-analysis. J Orthop Traumatol 23:8
Migliorini F, Eschweiler J, Maffulli N, Driessen A, Rath B, Tingart M et al (2021) Management of patellar chondral defects with autologous matrix induced chondrogenesis (AMIC) compared to microfractures: a four years follow-up clinical trial. Life (Basel) 11:141
Noorduyn JCA, Glastra van Loon T, van de Graaf VA, Willigenburg NW, Butter IK, Scholten-Peeters GGM et al (2020) Functional outcomes of arthroscopic partial meniscectomy versus physical therapy for degenerative meniscal tears using a patient-specific score: a randomized controlled trial. Orthop J Sports Med 8:2325967120954392
Noyes FR, Barber SD, Mangine RE (1991) Abnormal lower limb symmetry determined by function hop tests after anterior cruciate ligament rupture. Am J Sports Med 19:513–518
Osteras H, Osteras B, Torstensen TA (2012) Medical exercise therapy, and not arthroscopic surgery, resulted in decreased depression and anxiety in patients with degenerative meniscus injury. J Bodyw Mov Ther 16:456–463
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71
Pan H, Zhang P, Zhang Z, Yang Q (2020) Arthroscopic partial meniscectomy combined with medical exercise therapy versus isolated medical exercise therapy for degenerative meniscal tear: a meta-analysis of randomized controlled trials. Int J Surg 79:222–232
Pujol N, Salle De Chou E, Boisrenoult P, Beaufils P (2015) Platelet-rich plasma for open meniscal repair in young patients: any benefit? Knee Surg Sports Traumatol Arthrosc 23:51–58
Rabin R, de Charro F (2001) EQ-5D: a measure of health status from the EuroQol Group. Ann Med 33:337–343
Ro KH, Kim JH, Heo JW, Lee DH (2020) Clinical and radiological outcomes of meniscal repair versus partial meniscectomy for medial meniscus root tears: a systematic review and meta-analysis. Orthop J Sports Med 8:2325967120962078
Rolf CG, Barclay C, Riyami M, George J (2006) The importance of early arthroscopy in athletes with painful cartilage lesions of the ankle: a prospective study of 61 consecutive cases. J Orthop Surg Res 1:4
Roos EM, Bremander AB, Englund M, Lohmander LS (2008) Change in self-reported outcomes and objective physical function over 7 years in middle-aged subjects with or at high risk of knee osteoarthritis. Ann Rheum Dis 67:505–510
Roos EM, Hare KB, Nielsen SM, Christensen R, Lohmander LS (2018) Better outcome from arthroscopic partial meniscectomy than skin incisions only? A sham-controlled randomised trial in patients aged 35–55 years with knee pain and an MRI-verified meniscal tear. BMJ Open 8:e019461
Sihvonen R, Paavola M, Malmivaara A, Itala A, Joukainen A, Kalske J et al (2020) Arthroscopic partial meniscectomy for a degenerative meniscus tear: a 5 year follow-up of the placebo-surgery controlled FIDELITY (Finnish Degenerative Meniscus Lesion Study) trial. Br J Sports Med 54:1332–1339
Sihvonen R, Paavola M, Malmivaara A, Itala A, Joukainen A, Nurmi H et al (2018) Arthroscopic partial meniscectomy versus placebo surgery for a degenerative meniscus tear: a 2-year follow-up of the randomised controlled trial. Ann Rheum Dis 77:188–195
Sihvonen R, Paavola M, Malmivaara A, Itala A, Joukainen A, Nurmi H et al (2013) Arthroscopic partial meniscectomy versus sham surgery for a degenerative meniscal tear. N Engl J Med 369:2515–2524
Smoak JB, Matthews JR, Vinod AV, Kluczynski MA, Bisson LJ (2020) An up-to-date review of the meniscus literature: a systematic summary of systematic reviews and meta-analyses. Orthop J Sports Med 8:2325967120950306
Stensrud S, Risberg MA, Roos EM (2015) Effect of exercise therapy compared with arthroscopic surgery on knee muscle strength and functional performance in middle-aged patients with degenerative meniscus tears: a 3-mo follow-up of a randomized controlled trial. Am J Phys Med Rehabil 94:460–473
Stensrud S, Roos EM, Risberg MA (2012) A 12-week exercise therapy program in middle-aged patients with degenerative meniscus tears: a case series with 1-year follow-up. J Orthop Sports Phys Ther 42:919–931
Thorlund JB, Juhl CB, Roos EM, Lohmander LS (2015) Arthroscopic surgery for degenerative knee: systematic review and meta-analysis of benefits and harms. BMJ 350:h2747
van de Graaf VA, Noorduyn JCA, Willigenburg NW, Butter IK, de Gast A, Mol BW et al (2018) Effect of early surgery vs physical therapy on knee function among patients with nonobstructive meniscal tears: the ESCAPE randomized clinical trial. JAMA 320:1328–1337
van de Graaf VA, Wolterbeek N, Mutsaerts EL, Scholtes VA, Saris DB, de Gast A et al (2016) Arthroscopic partial meniscectomy or conservative treatment for nonobstructive meniscal tears: a systematic review and meta-analysis of randomized controlled trials. Arthroscopy 32(1855–1865):e1854
Yim JH, Seon JK, Song EK, Choi JI, Kim MC, Lee KB et al (2013) A comparative study of meniscectomy and nonoperative treatment for degenerative horizontal tears of the medial meniscus. Am J Sports Med 41:1565–1570
Funding
Open Access funding enabled and organized by Projekt DEAL. The authors received no financial or material support for the research, authorship, and/or publication of this article.
Author information
Authors and Affiliations
Contributions
FM: writing, revising, selection, data collection, data extraction, synthesis methods, study risk of bias assessment, and final approval; FC: writing, revising, study selection, data collection, data extraction, study risk of bias assessment, and final approval; FO: writing, revising, and final approval; JE: writing, revising, and final approval; FH: writing, revising, study risk of bias assessment, and final approval; NM: writing, revising, and final approval.
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have any competing interests for this article.
Ethical approval
This study complies with ethical standards.
Consent to publish
Not applicable.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Migliorini, F., Oliva, F., Eschweiler, J. et al. No evidence in support of arthroscopic partial meniscectomy in adults with degenerative and nonobstructive meniscal symptoms: a level I evidence-based systematic review. Knee Surg Sports Traumatol Arthrosc 31, 1733–1743 (2023). https://doi.org/10.1007/s00167-022-07040-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-07040-0