Abstract
Purpose
To compare the clinical outcome of arthroscopic capsulolabral repair for traumatic anterior shoulder instability with PEEK knotless and knotted biodegradable suture anchors.
Methods
Arthroscopic stabilization was performed in 78 patients with recurrent traumatic anterior shoulder instability. They were divided into 2 groups of 39 patients each, according to suture anchors used: knotless PEEK anchors in group 1, and biodegradable anchors in group 2. Exclusion criteria were: instability without dislocation, posterior or multidirectional instability, glenoid bone loss > 20%, off-track lesions, concomitant rotator cuff tears and previous surgery. The primary outcome was the Disabilities of the Arm, Shoulder and Hand (DASH) self-administered questionnaire. Secondary outcomes were: Work-DASH, Sport-DASH, Rowe score, recurrent instability and subsequent surgery. The following independent variables were considered: age, gender, dominance, generalized ligamentous hyperlaxity, duration of symptoms, age at first dislocation, number of dislocations, type of work, type of sport, sports activity level, capsule-labral injury pattern, SLAP lesion and number of anchors. Differences between groups for numerical variables were analyzed by use of the Student’s t-test or Mann–Whitney U-test. Fisher’s exact test was used for analysis of categorical variables. Significance was set at p < 0.05.
Results
Seven patients (9%) were lost at follow-up, 5 from group 1 and 2 from group 2. Follow-up ranged from 36 to 60 months (median: 44; IQR: 13). Comparison between groups did not show significant differences for each independent variable considered. No differences could be found either for DASH (n.s.) or Rowe (p = n.s.) scores between the two groups. Overall recurrence rate was 7%. Three re-dislocations were reported in group 1 and two in group 2 (n.s.). Only one patient in each group underwent re-operation.
Conclusions
The study showed no significant differences in clinical outcomes after arthroscopic treatment of traumatic anterior shoulder instability using PEEK knotless or biodegradable knotted anchors at mid-term follow-up.
Level of evidence
I.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Suture anchors represent the gold standard for arthroscopic Bankart repair. Historically, metal anchors were the first to be introduced, albeit their use for labral repair was rather discontinued and absorbable suture anchors were popularized [21]. Major strengths of using biodegradable anchors rely on their compatibility with any imaging technique and theoretically on the opportunity of easier revision surgery. Several clinical trials compared clinical outcomes of arthroscopic Bankart repair with metal and absorbable suture anchors showing no significant differences between them [19, 25]. An alternative to metal or biodegradable materials is polyether-ether-ketone (PEEK). PEEK is a stable, inert material resistant to hydrolysis and oxidation with no evidence of cytotoxicity [11].
Anchor design may be important for safety and efficacy of tissue-to-bone fixation. Nowadays, knotted or knotless anchors are available. Potential major drawback of knotted anchors depends on the presence of bulky knots protruding over the articular surface, which can cause friction and cartilage wear. Moreover, arthroscopic knot tying is time-consuming and often requires a certain learning curve. On the opposite, knotless anchors have the advantage of being easy and fast to use.
Theoretically, safe, reliable and effective fixation devices for arthroscopic Bankart repair should consist of a combination of inert material with the most suitable design. Although several ex-vivo studies compared mechanical behavior of different suture anchors available on the market [1, 14, 23], few clinical trials compared safety and efficacy of suture anchors having different composition and design [4, 18, 22].
The purpose of the present study was to compare the clinical outcome of arthroscopic capsule-labral repair for anterior shoulder instability with PEEK knotless and knotted biodegradable suture anchors. The hypothesis of the study was that there were no differences in clinical outcome between the two types of suture anchors.
Materials and methods
The protocol and informed consent process were approved by the institutional review board and by the local ethic committee (prot no. 763A1411, Catholic University, Rome). A single-blind prospective randomized controlled trial was conducted.
Population
Patients aged 18 years or older affected by recurrent traumatic anteroinferior glenohumeral instability who accepted to enter the study were considered eligible. All patients underwent a bilateral computed tomography (CT) scan preoperatively to rule out critical bone defects. Exclusion criteria were: instability without dislocation, posterior/multidirectional instability, glenoid bone defect exceeding 20% of the surface area of the inferior glenoid [26], off-track lesions [9], Bony Bankart lesions, concomitant rotator cuff tears, previous fractures and/or surgery on the same shoulder, infections, congenital or acquired inflammatory or neurologic diseases (systemic or local) involving the shoulder girdles, inability or unwillingness to sign the informed-consent form or to complete self-administered questionnaires. Enrollment was confirmed at the time of surgery.
Randomization and allocation concealment
Patients were divided into 2 groups comprising 39 cases each and were randomly allocated with a random sequence generator (www.random.org). The randomization list was kept by an independent researcher not involved in the study. Allocation concealment was performed by use of a closed-envelope procedure, and the assignment code of each patient to one of the two groups was shown to the surgeon only at the time of surgery, after confirmation of enrollment.
Intervention
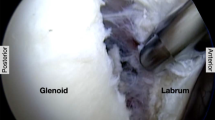
All patients underwent an arthroscopic anterior capsulolabral repair. Groups differed in the type of suture anchors used: 2.9-mm PEEK knotless anchors (Pushlock 2.9 mm; Arthrex Inc., Naples, FL, USA) in group 1; and double-loaded bioabsorbable anchors consisting of amorphous poly-l/d-lactic acid (PLDLA) (Bio-FASTak 3.0 mm; Arthrex) in group 2.
In all patients, surgery was performed in general anesthesia and in lateral decubitus position. A standard three-portals surgical approach was used. Capsule-labral status was documented according to the injury pattern of the anterior-inferior capsule-labral complex (Bankart or ALPSA lesion) and the presence and type of SLAP lesion.
Concomitant SLAP lesions were repaired. All the operations were performed by the same surgeon. After surgery, a sling was applied to the operated limb and maintained for 4 weeks; after this period, all patients underwent the same rehabilitation program for at least 2 months. In the first phase (4–8 weeks), rehabilitation was focused on regaining a full range of motion; while in the second phase (9–12 weeks), patients underwent a muscle-strengthening program. Return to work or sport activities was allowed after 4–6 months after surgery.
All patients were evaluated postoperatively as follows: 1, 3 and 6 months and then yearly.
Outcome measurements
Clinical assessment at baseline and at follow-up was performed by researchers that were blind to allocation. Baseline characteristics considered were as follows: age (years), gender, dominance, generalized ligamentous laxity (GLL) as measured with the Beighton score [2] (GLL was considered for Beighton score equal or greater than 4 [13]), duration of symptoms (months), age at first dislocation (years), number of dislocations, type of work, type of sport, sports activity level, labral injury pattern (Bankart or ALPSA lesion), and number of anchors and SLAP lesion (presence and type).
The primary outcome of the study was assessment of disability-related quality of life through the national validated version of the Disabilities of the Arm, Shoulder and Hand (DASH) questionnaire [12, 29]. This is a self-administered questionnaire that measures physical ability and symptoms of the upper extremity and explores the impact of functional impairment and pain on daily living tasks, as well as social and recreational activities, work, and sleep. The scoring system of the questionnaire is based on a metric scale, ranging from 0 points (minimum disability, best result) to 100 points (maximum disability, poorest result). Two optional modules were also administered for assessment of working capacity (Work-DASH) and ability to play sports or instruments (Sport-DASH).
Secondary outcomes included the evaluation of the shoulder function related to joint stability as measured by Rowe score [32]. It is an objective instrument composed of four items: shoulder function (score: 0–50), pain (score: 0–10), stability (score: 0–30) and range of movement (score: 0–10). Total score ranges from 0 (poor result) to 100 (excellent result).
Recurrence rate of dislocation was also considered a secondary outcome and defined as at least one episode of re-dislocation, while episodes of subluxation were recorded and scored within the Rowe scoring system [32]. Re-operation rate was also assessed; intraoperative and postoperative complications were recorded as well.
Statistical analysis
Data analysis was performed with statistical software (SPSS v.25, IBM Inc., Harmonk, NY, USA). Normality of numerical data were assessed by Shapiro–Wilk test. Descriptive statistics were reported as means and standard deviations (SD) for normally distributed numerical data, otherwise medians and interquartile ranges (IQR) were used. Categorical data were expressed as frequencies and percentages.
Comparisons between groups both at baseline and at follow-up were performed by use of Student’s t test for normally distributed data, otherwise the Mann–Whitney U-test was used. Fisher’s exact test was used for analysis of categorical variables. Significance was set at p ≤ 0.05.
Sample size was calculated according to the primary outcome measurement (DASH score) and based on a previously published study [25]. On considering 10 points as the minimal clinically important difference (MCID) detectable with the DASH score [12], estimated sample size was 31 cases per group given α equal to 0.05 and power (1 – β) equal to 0.80. This value was increased to 39 per group to compensate for an eventual 20% maximum loss of patients at follow-up.
Results
Minimum follow-up was 3 years. Follow-up ranged from 36 to 60 months (median: 44; IQR: 13). Seven patients (9%) did not return at follow-up: five from group 1 and two from group 2. All these patients were called several times but refused to return because they lived in other regions of the country or abroad; Therefore, a total of 71 patients (91%) completed the follow-up: 34 from group 1 and 37 from group 2 (Fig. 1). Overall, there were 63 males (88.7%) and 8 females (8.3%). Age ranged from 18 to 47 years (median: 26; IQR: 13).
Baseline characteristics of the two groups are shown in Table 1. The two groups did not significantly differ with respect to all the independent variables.
No significant differences between groups could be found for DASH score (Table 2), neither for working capacity and sports activity. Also, Rowe score was not significantly different in the two groups. Overall recurrence rate was 7%. Three re-dislocations were reported in group 1 and two in group 2 (n.s.). Only one patient in each group underwent re-operation (Table 2).
Discussion
The main finding of the present paper is that there are no differences in clinical outcome of arthroscopic treatment of anterior shoulder instability between PEEK knotless and biodegradable knotted suture anchors at minimum 3-year follow-up. Moreover, no complications related to anchors material and design were reported.
The main strength of the present paper is that it allowed a comparison for two combined features: biodegradable versus permanent inert material, and knotless versus knotted anchor design. Indeed, literature is lacking and quite conflicting on both topics.
Several mechanical studies compared biodegradable and metal anchors for rotator cuff repair and showed contradictory results about differences in fixation strength of the implants [6, 7, 24]. Barber et al. [1] analyzed mechanical behavior of seven absorbable glenoid anchors and found no differences in ultimate failure strength after cyclic loading. Recently, Khoo et al. [14] compared four types of anchors used in labral repair. They found that biodegradable anchors were associated with less viable cells at 48 and 72 h after incubation and higher acidic culture medium at 24, 48, and 72 h, which basically means that examined biodegradable anchors are cytotoxic and have significantly lower failure load.
On the other side, no relevant biomechanical issues have been reported for PEEK anchors [10]. In a study focused on patellar tendon repair, Lanzi et al. [17] showed that PEEK anchors are superior to the transosseous technique for minimizing gap formation and improving load-to-failure strength, thus confirming the good mechanical properties of PEEK implants.
Moving forward to comparison between knotless and knotted anchors, a recent systematic review included five cadaveric studies focusing on arthroscopic Bankart repair [22]. The authors found contradictory results: one study claimed higher mechanical properties for knotless anchors [16], another favored knotted anchors [28], and the remaining three studies showed no differences between the two implant designs [20, 31, 33].
From a clinical standpoint, few studies try to clarify the controversies. Brown et al. [4] investigated surgical factors influencing the recurrence rate after arthroscopic Bankart repair. They included 26 studies (level of evidence varying from I to IV). Due to heterogeneity of included studies, a meta-analysis was not possible, but pooled weighted means showed that recurrent instability after arthroscopic Bankart repair was not influenced by rotator interval closure, number of anchors used, and not even by anchor material and design (i.e., biodegradable versus permanent anchors, and knotless versus knotted anchors). Although methodological quality of included studies was limited overall, results were consistent with those of the present study. Conversely, Peters et al. [30] conducted a prospective cohort study on 155 patients undergoing arthroscopic Bankart repair by comparing 4 types of knotless implants: biodegradable (PGA) tack, and biodegradable (PLLA), metal and PEEK suture anchors. The authors showed higher re-dislocation rate with the use of biodegradable implants. These results differed from those of the present study, probably because of the differences among groups for duration of follow-up (permanent anchors groups had shorter follow-up than biodegradable devices groups).
Recently, Matache et al. [22] conducted a systematic review comparing knotless and knotted anchors in patients undergoing arthroscopic Bankart repair. Four level II–III of evidence were included. Three studies found no significant differences in any clinical outcome measures [3, 15, 27], while one study found a significantly higher VAS and lower recurrence and revision rate with the use of knotted anchors [5]. However, meta-analysis showed no differences in revision rate between knotless and knotted anchors.
To summarize, although some mechanical studies found a certain “time zero” difference, clinical evidence showed that biodegradable and permanent anchors as well as knotless and knotted implants provide adequate outcomes, and this is confirmed in the present study. That being said, the main clinical advantage of knotless anchors, in our opinion, relies on their ease of use, which consistently reduces surgical times [22]. Regarding materials, as no adverse reactions have been reported in the literature with PEEK anchors, they should be preferred to biodegradable devices, which are burdened by a safety issue, as reported in the previous literature [8]. Based on these assumption, knotless PEEK anchors could be considered a viable alternative to knotted bioabsorbable anchors in clinical practice.
Main limitation of the present study is the absence of a postoperative imaging assessment. Therefore, no information could be provided about anchor resorption, peri-anchor cysts formation or osteoarthritis. Moreover, since the sample size was calculated according to the primary outcome measurement (DASH score), it is not possible to state if the sample could have been underrated to study eventual reactions related to anchor properties.
Conclusions
The study showed no significant differences in clinical outcomes after arthroscopic treatment of traumatic anterior shoulder instability using PEEK knotless or biodegradable knotted anchors at minimum 3-year follow-up.
Change history
23 July 2022
“Missing Open Access funding information has been added in the Funding Note.”.
References
Barber FA, Coons DA, Ruiz-Suarez M (2008) Cyclic load testing and ultimate failure strength of biodegradable glenoid anchors. Arthroscopy 24:224–228
Beighton P, Horan F (1969) Orthopaedic aspects of the Ehlers-Danlos syndrome. J Bone Joint Surg Br 51:444–453
Bents EJ, Brady PC, Adams CR, Tokish JM, Higgins LD, Denard PJ (2017) Patient-reported outcomes of knotted and knotless glenohumeral labral repairs are equivalent. Am J Orthop Belle Mead NJ 46:279–283
Brown L, Rothermel S, Joshi R, Dhawan A (2017) Recurrent instability after arthroscopic Bankart reconstruction: a systematic review of surgical technical factors. Arthroscopy 33:2081–2092
Cho NS, Lubis AMT, Ha JH, Rhee YG (2006) Clinical results of arthroscopic Bankart repair with knot-tying and knotless suture anchors. Arthroscopy 22:1276–1282
Cummins CA, Strickland S, Appleyard RC, Szomor ZL, Marshall J, Murrell GAC (2003) Rotator cuff repair with bioabsorbable screws: an in vivo and ex vivo investigation. Arthroscopy 19:239–248
Dejong ES, DeBerardino TM, Brooks DE, Judson K (2004) In vivo comparison of a metal versus a biodegradable suture anchor. Arthroscopy 20:511–516
Dhawan A, Ghodadra N, Karas V, Salata MJ, Cole BJ (2012) Complications of bioabsorbable suture anchors in the shoulder. Am J Sports Med 40:1424–1430
Di Giacomo G, Itoi E, Burkhart SS (2014) Evolving concept of bipolar bone loss and the Hill-Sachs lesion: from “engaging/non-engaging” lesion to “on-track/off-track” lesion. Arthroscopy 30:90–98
Güleçyüz MF, Pietschmann MF, Scharpf A, Eid AS, Michalski S, Simon JM, Niethammer TR, Müller PE (2020) Revisability of polyetheretherketone suture anchors utilised in primary and revision Bankart repair. J Orthop Sci 25:830–835
He M, Huang Y, Xu H, Feng G, Liu L, Li Y, Sun D, Zhang L (2021) Modification of polyetheretherketone implants: from enhancing bone integration to enabling multi-modal therapeutics. Acta Biomater 129:18–32
Hudak PL, Amadio PC, Bombardier C (1996) Development of an upper extremity outcome measure: the DASH (disabilities of the arm, shoulder and hand) [corrected]. The Upper Extremity Collaborative Group (UECG). Am J Ind Med 29:602–608
Juul-Kristensen B, Schmedling K, Rombaut L, Lund H, Engelbert RHH (2017) Measurement properties of clinical assessment methods for classifying generalized joint hypermobility—a systematic review. Am J Med Genet C Semin Med Genet 175:116–147
Khoo JK, Lee JHT, Lam PH, Wei A-Q, Ronquillo J, Murrell GAC (2019) Cytotoxicity and biomechanics of suture anchors used in labral repairs. JSES Open Access 3:29–36
Kocaoglu B, Guven O, Nalbantoglu U, Aydin N, Haklar U (2009) No difference between knotless sutures and suture anchors in arthroscopic repair of Bankart lesions in collision athletes. Knee Surg Sports Traumatol Arthrosc 17:844–849
Lacheta L, Brady A, Rosenberg SI, Dornan GJ, Dekker TJ, Anderson N, Altintas B, Krob JJ, Millett PJ (2020) Biomechanical evaluation of knotless and knotted all-suture anchor repair constructs in 4 Bankart repair configurations. Arthroscopy 36:1523–1532
Lanzi JT, Felix J, Tucker CJ, Cameron KL, Rogers J, Owens BD, Svoboda SJ (2016) Comparison of the suture anchor and transosseous techniques for patellar tendon repair: a biomechanical study. Am J Sports Med 44:2076–2080
Lee J-H, Lee Y-B (2020) Clinical and radiologic outcomes of combined use of biocomposite and PEEK suture anchors during arthroscopic rotator cuff repair: a prospective observational study. J Clin Med 9:E2545
Lee J-H, Park I, Hyun H-S, Kim S-W, Shin S-J (2019) Comparison of clinical outcomes and computed tomography analysis for tunnel diameter after arthroscopic Bankart repair with the all-suture anchor and the biodegradable suture anchor. Arthroscopy 35:1351–1358
Leedle BP, Miller MD (2005) Pullout strength of knotless suture anchors. Arthroscopy 21:81–85
Levine WN, Sonnenfeld JJ, Shiu B (2018) Shoulder instability: common problems and solutions. Clin Sports Med 37:161–177
Matache BA, Hurley ET, Kanakamedala AC, Jazrawi LM, Virk M, Strauss EJ, Campbell KA (2020) Knotted versus knotless anchors for labral repair in the shoulder—a systematic review. Arthroscopy. https://doi.org/10.1016/j.arthro.2020.11.056
Mei XY, Sheth U, Abouali J (2021) Excellent functional outcomes and low complication rates following knotless arthroscopic Bankart repair: a systematic review of clinical and biomechanical studies. Arthrosc Sports Med Rehabil 3:e927–e938
Meyer DC, Fucentese SF, Ruffieux K, Jacob HAC, Gerber C (2003) Mechanical testing of absorbable suture anchors. Arthroscopy 19:188–193
Milano G, Grasso A, Santagada DA, Saccomanno MF, Deriu L, Fabbriciani C (2010) Comparison between metal and biodegradable suture anchors in the arthroscopic treatment of traumatic anterior shoulder instability: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc 18:1785–1791
Milano G, Saccomanno MF, Magarelli N, Bonomo L (2015) Analysis of agreement between computed tomography measurements of glenoid bone defects in anterior shoulder instability with and without comparison with the contralateral shoulder. Am J Sports Med 43:2918–2926
Ng DZ, Kumar VP (2014) Arthroscopic Bankart repair using knot-tying versus knotless suture anchors: is there a difference? Arthroscopy 30:422–427
Nho SJ, Frank RM, Van Thiel GS, Wang FC, Wang VM, Provencher MT, Verma NN (2010) A biomechanical analysis of anterior Bankart repair using suture anchors. Am J Sports Med 38:1405–1412
Padua R, Padua L, Ceccarelli E, Romanini E, Zanoli G, Amadio PC, Campi A (2003) Italian version of the Disability of the Arm, Shoulder and Hand (DASH) questionnaire. Cross-cultural adaptation and validation. J Hand Surg Edinb Scotl 28:179–186
Peters K, Pirapakaran K, Pearce A, Murrell G (2018) A comparison of permanent anchors versus biodegradable anchors and tacks for arthroscopic shoulder stabilization. Tech Shoulder Elb Surg 19:1–7
Ranawat AS, Golish SR, Miller MD, Caldwell PE, Singanamala N, Treme G, Costic R, Hart JM, Sekiya JK (2011) Modes of failure of knotted and knotless suture anchors in an arthroscopic Bankart repair model with the capsulolabral tissues intact. Am J Orthop Belle Mead NJ 40:134–138
Rowe CR, Zarins B (1981) Recurrent transient subluxation of the shoulder. J Bone Joint Surg Am 63:863–872
Slabaugh MA, Friel NA, Wang VM, Cole BJ (2010) Restoring the labral height for treatment of Bankart lesions: a comparison of suture anchor constructs. Arthroscopy 26:587–591
Funding
Open access funding provided by Università degli Studi di Brescia within the CRUI-CARE Agreement.
Author information
Authors and Affiliations
Contributions
MFS: methodology—supporting, investigation, writing. SC: investigation—equal. MA: investigation—equal. MM: investigation—equal. AM: investigation—equal. SG: Investigation—equal. AS: investigation—equal. GM: conceptualization—lead, methodology—lead, formal analysis, supervision.
Corresponding author
Ethics declarations
Conflict of interest
Giuseppe Milano is Arthrex consultant. The other authors declared no conflict of interest.
Ethical approval
The protocol and informed consent process were approved by the institutional review board and by the local ethic committee (prot no. 763A1411, Catholic University, Rome).
Informed consent
Yes.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Saccomanno, M.F., Cerciello, S., Adriani, M. et al. Knotless PEEK and double-loaded biodegradable suture anchors ensure comparable clinical outcomes in the arthroscopic treatment of traumatic anterior shoulder instability: a prospective randomized study. Knee Surg Sports Traumatol Arthrosc 30, 3835–3841 (2022). https://doi.org/10.1007/s00167-022-06969-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-06969-6