Abstract
Purpose
The purpose of this study is to describe rotator cuff muscle stiffness in patients with different degrees of rotator cuff tear (RCT) severity and to assess its predictive ability for RCT reparability.
Methods
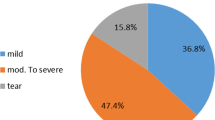
One hundred and thirty-three consecutive patients who were scheduled to undergo arthroscopic shoulder surgery were prospectively enrolled. Tendon retraction, fatty infiltration, and muscle atrophy were evaluated using magnetic resonance imaging. Shear modulus of supraspinatus (SSP) and infraspinatus (ISP) muscles were measured by ultrasound shear wave elastography (SWE). The tear size and reparability were determined intraoperatively.
Results
There were 97 patients in RCT group and 36 patients in control group. Bilateral shear modulus discrepancy (Δshear modulus) was used to represent rotator cuff stiffness. Severely fatty-infiltrated rotator cuff muscles possessed a significantly higher stiffness compared with their counterparts (SSP: CI 27.8–31.8 vs. 13.5–15.6 kPa, ISP: CI 33.2–38.1 vs. 8.8–11.2 kPa, p < 0.001). The same trend applied to muscles with distinct tendon retraction (SSP: CI 27.7–32.3 vs. 10.9–14.9 kPa, ISP: CI 33.2–38.6 vs. 6.5–11.0 kPa, p < 0.001) and obvious muscle atrophy (SSP: CI 27.9–32.1 vs. 13.6–15.8 kPa, ISP: CI 32.9–38.2 vs. 9.0–11.7 kPa, p < 0.001). Irreparable massive RCT (MRCT) patients had significantly stiffer SSP (CI 27.7–31.9 vs. 13.5–16.5 kPa, p < 0.001) and ISP (CI 33.5–37.8 vs. 10.3–14.8 kPa, p < 0.001) than reparable MRCT. The Δshear modulus of the ISP was a highly accurate predictor of RCT reparability. A cutoff value of 18.0 kPa had a sensitivity of 100% and specificity of 98.8% for irreparable MRCT.
Conclusion
Ultrasound SWE-derived rotator cuff muscle stiffness is closely correlated with RCT size and severity.
Level of evidence
I.





Similar content being viewed by others
References
Baumer TG, Davis L, Dischler J, Siegal DS, van Holsbeeck M, Moutzouros V et al (2017) Shear wave elastography of the supraspinatus muscle and tendon: repeatability and preliminary findings. J Biomech 53:201–204
Baumer TG, Dischler J, Davis L, Labyed Y, Siegal DS, van Holsbeeck M et al (2018) Effects of age and pathology on shear wave speed of the human rotator cuff. J Orthop Res 36:282–288
Chen S, He Y, Wu D, Hu N, Liang X, Jiang D et al (2021) Postoperative bone marrow edema lasts no more than 6 months after uncomplicated arthroscopic double-row rotator cuff repair with PEEK anchors. Knee Surg Sports Traumatol Arthrosc 29:162–169
Fuchs B, Weishaupt D, Zanetti M, Hodler J, Gerber C (1999) Fatty degeneration of the muscles of the rotator cuff: assessment by computed tomography versus magnetic resonance imaging. J Shoulder Elb Surg 8:599–605
Giambini H, Hatta T, Rezaei A, An KN (2018) Extensibility of the supraspinatus muscle can be predicted by combining shear wave elastography and magnetic resonance imaging-measured quantitative metrics of stiffness and volumetric fat infiltration: a cadaveric study. Clin Biomech (Bristol, Avon) 57:144–149
Guo S, Zhu Y, Song G, Jiang C (2020) Assessment of tendon retraction in large to massive rotator cuff tears: a modified Patte classification based on 2 coronal sections on preoperative magnetic resonance imaging with higher specificity on predicting reparability. Arthroscopy 36:2822–2830
Hackett L, Aveledo R, Lam PH, Murrell GA (2020) Reliability of shear wave elastography ultrasound to assess the supraspinatus tendon: an intra and inter-rater in vivo study. Shoulder Elb 12:18–23
Hatta T, Giambini H, Itoigawa Y, Hooke AW, Sperling JW, Steinmann SP et al (2017) Quantifying extensibility of rotator cuff muscle with tendon rupture using shear wave elastography: a cadaveric study. J Biomech 61:131–136
Hatta T, Giambini H, Uehara K, Okamoto S, Chen S, Sperling JW et al (2015) Quantitative assessment of rotator cuff muscle elasticity: reliability and feasibility of shear wave elastography. J Biomech 48:3853–3858
Itoigawa Y, Maruyama Y, Kawasaki T, Wada T, Yoshida K, An KN et al (2018) Shear wave elastography can predict passive stiffness of supraspinatus musculotendinous unit during arthroscopic rotator cuff repair for presurgical planning. Arthroscopy 34:2276–2284
Itoigawa Y, Sperling JW, Steinmann SP, Chen Q, Song P, Chen S et al (2015) Feasibility assessment of shear wave elastography to rotator cuff muscle. Clin Anat 28:213–218
Itoigawa Y, Wada T, Kawasaki T, Morikawa D, Maruyama Y, Kaneko K (2020) Supraspinatus muscle and tendon stiffness changes after arthroscopic rotator cuff repair: a shear wave elastography assessment. J Orthop Res 38:219–227
Jeong JY, Chung PK, Lee SM, Yoo JC (2017) Supraspinatus muscle occupation ratio predicts rotator cuff reparability. J Shoulder Elb Surg 26:960–966
Kim IB, Jung DW, Suh KT (2018) Prediction of the irreparability of rotator cuff tears. Arthroscopy 34:2076–2084
Kim JY, Park JS, Rhee YG (2017) Can preoperative magnetic resonance imaging predict the reparability of massive rotator cuff tears? Am J Sports Med 45:1654–1663
Kim K, Hwang HJ, Kim SG, Lee JH, Jeong WK (2018) Can shoulder muscle activity be evaluated with ultrasound shear wave elastography? Clin Orthop Relat Res 476:1276–1283
Kim SC, Shim SB, Kim WJ, Yoo JC (2021) Preoperative rotator cuff tendon integrity, tear size, and muscle atrophy and fatty infiltration are associated with structural outcomes of arthroscopic revision rotator cuff repair. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06732-3
Kuzel BR, Grindel S, Papandrea R, Ziegler D (2013) Fatty infiltration and rotator cuff atrophy. J Am Acad Orthop Surg 21:613–623
Lawrence RL, Ruder MC, Moutzouros V, Makhni EC, Muh SJ, Siegal D et al (2021) Ultrasound shear wave elastography and its association with rotator cuff tear characteristics. JSES Int 5:500–506
Liljequist D, Elfving B, Skavberg Roaldsen K (2019) Intraclass correlation—a discussion and demonstration of basic features. PLoS One 14:e0219854
Lin DJ, Burke CJ, Abiri B, Babb JS, Adler RS (2020) Supraspinatus muscle shear wave elastography (SWE): detection of biomechanical differences with varying tendon quality prior to gray-scale morphologic changes. Skelet Radiol 49:731–738
MacDermid JC, Bryant D, Holtby R, Razmjou H, Faber K, Canada J et al (2021) Arthroscopic versus mini-open rotator cuff repair: a randomized trial and meta-analysis. Am J Sports Med. https://doi.org/10.1177/036354652110382333635465211038233
Martinoli C (2010) Musculoskeletal ultrasound: technical guidelines. Insights Imaging 1:99–141
Nishishita S, Hasegawa S, Nakamura M, Umegaki H, Kobayashi T, Ichihashi N (2018) Effective stretching position for the supraspinatus muscle evaluated by shear wave elastography in vivo. J Shoulder Elb Surg 27:2242–2248
Patte D (1990) Classification of rotator cuff lesions. Clin Orthop Relat Res 254:81–86
Rosskopf AB, Ehrmann C, Buck FM, Gerber C, Fluck M, Pfirrmann CW (2016) Quantitative shear-wave US elastography of the supraspinatus muscle: reliability of the method and relation to tendon integrity and muscle quality. Radiology 278:465–474
Ryu J, Jeong WK (2017) Current status of musculoskeletal application of shear wave elastography. Ultrasonography 36:185–197
Schmalzl J, Fenwick A, Boehm D, Gilbert F (2017) The application of ultrasound elastography in the shoulder. J Shoulder Elb Surg 26:2236–2246
Shim SB, Jeong JY, Kim JS, Yoo JC (2018) Evaluation of risk factors for irreparable rotator cuff tear in patients older than age 70 including evaluation of radiologic factors of the shoulder. J Shoulder Elb Surg 27:1932–1938
Takeda Y, Fujii K, Suzue N, Miyatake K, Kawasaki Y, Yokoyama K (2021) Repair tension during arthroscopic rotator cuff repair is correlated with preoperative tendon retraction and postoperative rotator cuff integrity. Arthroscopy 37:2735–2742
Valencia AP, Lai JK, Iyer SR, Mistretta KL, Spangenburg EE, Davis DL et al (2018) Fatty infiltration is a prognostic marker of muscle function after rotator cuff tear. Am J Sports Med 46:2161–2169
Warner JJ, Higgins L, Parsons IM, Dowdy P (2001) Diagnosis and treatment of anterosuperior rotator cuff tears. J Shoulder Elb Surg 10:37–46
Yamamoto A, Takagishi K, Osawa T, Yanagawa T, Nakajima D, Shitara H et al (2010) Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elb Surg 19:116–120
Yuri T, Trevino JH, Hatta T, Kiyoshige Y, Jacobs PM, Giambini H (2021) Stiffness of the infraspinatus and the teres minor muscles during shoulder external rotation: an in-vitro and in-vivo shear wave elastography study. Clin Biomech (Bristol, Avon) 85:105328
Zanetti M, Gerber C, Hodler J (1998) Quantitative assessment of the muscles of the rotator cuff with magnetic resonance imaging. Investig Radiol 33:163–170
Funding
Funding was provided by Chongqing medical scientific research project (Grant no. 2021MSXM032).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Jiaxing Huang, Lan Jiang, Jiawei Wang, Dandong Wu, Wei Huang, Ning Hu, and Hong Chen declare that they have no conflict of interest.
Ethical approval
All procedures performed in this prospective study were in accordance with the ethical standards of the First Affiliated Hospital of Chongqing Medical University. This study was approved by our institutional review board (IRB, No. 2020795) and registered in the Chinese Clinical Trial Register (ChiCTR2100042462).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Huang, J., Jiang, L., Wang, J. et al. Ultrasound shear wave elastography-derived tissue stiffness is positively correlated with rotator cuff tear size and muscular degeneration. Knee Surg Sports Traumatol Arthrosc 30, 2492–2499 (2022). https://doi.org/10.1007/s00167-022-06892-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-06892-w