Abstract
Background
Rotator cuff disorders are the main causes of chronic shoulder instability and pain. Diagnostic imaging is important to guide treatment decisions with magnetic resonance imaging, which is considered the reference standard for rotator cuff evaluation. Sono-elastography is a noninvasive and reliable ultrasound technique that provides qualitative as well as quantitative assessment of tendon quality through alteration in the tissue composition before alteration in tendon echogenicity or thickness on the conventional US.
Purpose
-
1.
To assess the role of shear wave sonoelastography in the evaluation of supraspinatus tendon abnormalities.
-
2.
To assess the association between SWE and grades of tendon abnormalities on MRI (the standard imaging in the evaluation of rotator cuff abnormalities).
Results
The shear wave velocity (SWV) was notably low (reduced tendon stiffness) in patients with supraspinatus tendinopathy and tear (mean SWV for the supraspinatus tendon in cases of tendinopathy/tear was 3.91 m/s with a standard deviation of 0.67, while the mean SWV for normal supraspinatus tendons was 6.93 m/s with a standard deviation 0.57), and a significant difference was found in SWV values between cases and controls (P < 0.001).
Also, there were significant differences between the patients with different grades of tendon abnormalities (P < 0.001), with a highly significant inverse correlation observed between the measured SWV and grades of tendon abnormalities on MRI (P < 0.001).
Conclusions
Sonoelastography showed tendon softening in supraspinatus tendinopathy and tear with a good correlation to the MRI, making it a reproducible and low-cost imaging modality that can be a complementary tool to the US in the evaluation of shoulder disorders, especially when MRI is not allowed.
Similar content being viewed by others
Background
Rotator cuff abnormalities are commonly encountered in middle and old age. They are the important causes of chronic shoulder pain and lead to a lack of stability of the shoulder joint [1]. The supraspinatus tendon is the most commonly affected in rotator cuff tearing, as it anatomically traverses between two bones (the acromion process and humeral head). Rotator cuff pathologies are classified into tendinopathy, partial- and full-thickness tears [2]. The clinical differentiation between the different rotator cuff disorders is difficult, and imaging is crucial for the diagnosis and assessment of rotator cuff abnormalities to guide treatment decisions and to determine whether surgical intervention is needed [3].
US and MRI (with or without arthrography) are the most encountered imaging modalities in the diagnosis of rotator cuff diseases [4]. Ultrasonography is an inexpensive, noninvasive, and reliable modality for rotator cuff assessment with accuracy reaching 100% in the diagnosis of full-thickness tears and 91% for partial-thickness tears [5]. On ultrasound, the healthy tendon has a fascicular appearance showing multiple parallel echogenic lines on the longitudinal plane and multiple echogenic dots on the transverse plane. To avoid anisotropy during ultrasound examination, the ultrasound beam should be perpendicular to the orientation of the fascicles [6]. On ultrasound, tendinopathy appears as thickening of the tendon showing a heterogeneous hypoechoic pattern. Tendon tear appears as a hypoechoic defect within the tendon, not involving the tendon's full thickness in PTT and involving the full tendon thickness in FTT that allows communication between the subacromial/subdeltoid bursa and the glenohumeral joint cavity [7]. However, diagnosis of tendinopathy may be difficult with the conventional US as the echogenicity of the tendinopathic tendon may be similar to that of the healthy one, especially in cases of mild tendinopathy [4]. Ultrasound elastography (UE) is a new technique of US that enables qualitative as well as quantitative assessment of the tissue elastic properties, aiding in differentiation between the diseased and normal tissue [8]. Good results were reported in the use of UE in the characterization of breast, thyroid as well as focal hepatic lesions [9]. UE can be applied to different musculoskeletal tissues including the tendon, muscle, nerve, ligament, and cartilage [10]. Many recently published studies showed promising results on shear wave UE of the muscles and tendons. Most of these studies reported tendon softening in cases of tendinopathy, resulting in a reduction in the velocity of propagation of shear waves compared to the healthy tendons that are stiff [11].
Studies also showed that softening of the tendon may be a preceding sign of tendinopathy and pain. So, elastography may be helpful in the early detection of tendinopathy before the presence of symptoms, giving time for prophylactic measurements [12].
However, till now, limited research works were published on the application of SWE in rotator cuff assessment, so in this study, we aimed to assess the role of sonoelastography in the evaluation of supraspinatus tendinopathy/tear, to evaluate the relationship between shear wave velocity measured by sonoelastography and the morphological grade of tendon abnormality on MRI and to reach shear wave elastography cutoff value to determine tendinopathy and tear.
Methods
This case–control analytical observational study included 57 patients with chronic shoulder pain (> 3 months) referred to our radiology department, in the period from January 2020 to June 2021 for assessment of rotator cuff abnormality and 57 asymptomatic volunteers as control. Patients had given their informed consent.
The inclusion criteria for patients in the study were as follows: both genders, any age, history of shoulder pain for more than 3 months. The following criteria were used to exclude people: history of operative intervention for rotator cuff tendons, history of trauma, signs of calcific tendinopathy on MRI or ultrasound (as calcification causes artifact on obtaining SWE results and the measured velocities were exceeding the velocity scale on our device), and patients with contraindications to MRI as patients with pacemakers. Inclusion criteria for volunteers were both genders, any age, and no history of shoulder pain or shoulder intervention.
The sample size calculation for this comparative case–control study was done using EpiCalc 2000. Assuming 80% power, 0.05 level of significance, 50% proportion of controls exposed, to detect odds ratio OR = 3 and with the ratio of cases to controls = 1.
Included patients and volunteers were subjected to thorough history taking about age, sex, history of shoulder pain, history of the limitation of movement, duration of symptoms, history of sports activities, history of concomitant medical conditions, and history of trauma or previous operative intervention to the affected shoulder. A complete physical examination was performed for all patients by an orthopedic surgeon who referred them to the radiology department for the assessment of rotator cuff tendons by US and MRI.
Ultrasound examination was done using Toshiba ultrasound Aplio 500, Toshiba Medical, Japan, using a high frequency (14 MHz) linear probe. The examination was done by a radiologist who was an expert in MSK US for more than 10 years, and the examiner was masked to the results of the MRI.
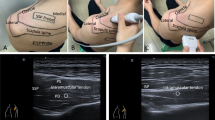
All volunteers and patients were scanned in a sitting position, the patient’s arm internally rotated and the forearm pronated and positioned on the patient’s back (standard crass position). The examiner is standing behind the patient.
The supraspinatus tendon was examined in along-axis view; this plane corresponds to the coronal oblique MRI images. The tendon was scanned from anterior to posterior with static B-mode images acquired at the areas of altered echogenicity. For acquisition of elastography images, a large amount of gel was applied on the skin surface for light contact of the probe, and to avoid compression, a color map was designated that soft tissues display a blue color while hard tissues display a red color and superimposed on the B-mode image. Then, about 3 mm ROI was organized and averaged for measurement of shear wave velocity in m/s at the area of altered echogenicity within the tendon.
Magnetic resonance imaging was done for the patients and volunteers in our radiology department using a Philips Achieva, The Netherlands (1.5 Tesla), superconducting magnet.
The MRI protocol for the shoulder joint included coronal oblique T1-weighted images (repetition time (TR) 540 ms, echo time (TE) 20 ms, section thickness 3.5 mm, intersection gap 0.3 mm, field of view 181 mm), coronal oblique T2-weighted images (TR 5020 ms, TE 100 ms, section thickness 3.5 mm, intersection gap 0.3 mm, FOV 181 mm), coronal oblique STIR images (TR 2734 ms, TE 80 ms, section thickness 3.5 mm, intersection gap 0.3 mm, FOV 181 mm), sagittal oblique T2-weighted spin-echo images (TR 5020 ms, TE 100 ms, section thickness 3.5 mm, intersection gap 0.3 mm, FOV 186 mm), and axial T2-FFE images (TR 575 ms, TE 12 ms, section thickness 4 mm, intersection gap 0.4 mm, FOV 206 mm).
MRI image evaluation was done by an experienced musculoskeletal radiologist. The abnormalities of the supraspinatus tendon on MRI were graded as grade 0 (normal): the tendon shows complete homogeneous low signal intensity on all pulse sequences, grade 1 (mild tendinopathy): normal caliber/mildly thickened tendon with mild intrasubstance increased signal on T2 and STIR sequences, grade 2 (moderate-to-severe tendinopathy): thickened tendon with moderate/marked increase in tendon signal on T2 and STIR sequences not reaching fluid signal, and grade 3 (definite tear): complete or partial disruption of tendon fibers being replaced by fluid signal.
Statistical methods
Data were coded and entered using the Statistical Package for the Social Sciences (SPSS) version 25 (IBM Corp., Armonk, NY, USA). Data were summarized using mean, standard deviation, minimum and maximum for quantitative variables and frequencies (number of cases) and relative frequencies (percentages) for categorical variables. Comparisons between groups were made using an unpaired t test [13]. For comparing categorical data, the chi-square (χ2) test was performed. The exact test was used instead when the expected frequency is less than 5 [14]. Correlations between quantitative variables were done using the Pearson correlation coefficient. The magnitude of the correlation was defined based on the value of the correlation coefficient [15]. A correlation less than 0.4 was considered weak, 0.4–0.6 was considered moderate, and more than 0.6 was considered strong. P values less than 0.05 were considered statistically significant.
Results
Characteristics of population included in the study
The study included 57 asymptomatic volunteers (34 males and 23 females with a mean age of 37.7 years) as controls and 57 patients (29 males and 28 females with a mean age of 41.8 years).
MRI grading of supraspinatus tendon abnormalities
Among the patients, 21 patients (36.8 %) had mild tendinopathy (grade I), 27 patients (47.4 %) had moderate-to-severe tendinopathy (grade II), and 9 patients (15.8 %) had supraspinatus tendon tear (grade III) (Fig. 1). The asymptomatic volunteers showed normal supraspinatus tendon on MRI.
Shear wave elastography findings
Normal supraspinatus tendons showed a homogenous stiff pattern (red color) with faster propagation of shear waves (higher SWV) (Fig. 2), while the pathological tendons showed a heterogeneous and soft pattern (green and blue color) with slower propagation of shear waves (lower SWV) (Fig. 3).
a MRI coronal oblique STIR images of supraspinatus tendon showing thickened tendon with intrasubstance increased signal (grade II), b B-mode US showing thickened tendon with heterogeneous echogenicity, c shear wave elastography showing areas of tendon softening (blue color) with average SWV equals 3.2 cm/sec
The shear wave velocities for controls were ranging from 6.00 to 8.00 m/sec with the mean SWV equaling 6.93 m/s with a standard deviation of 0.57, while the shear wave velocity for the cases was ranging from 2.70 to 5.10 m/s with mean SWV equal to 3.91 m/s with a standard deviation 0.67 with a significant difference in shear wave velocities between the two groups (P < 0.001), as illustrated in Fig. 4.
The shear wave velocity for grade I tendon abnormality was ranging from 3.8 to 5.1 m/s with a mean value of about 4.59 m/s (as shown in Fig. 5), while the shear wave velocity for grade II tendon abnormality was ranging from 2.9 to 4.6 m/s with a mean value of about 3.678 m/s (Fig. 3) and the shear wave velocity for grade III was ranging from 2.7 to 3.8 m/s with a mean value of about 3.08 (Fig. 6).
a MRI coronal oblique STIR images of supraspinatus tendon showing intrasubstance increased signal with fluid signal seen disrupting the articular surface fibers (small articular surface tear grade III). b B-mode ultrasound of supraspinatus tendon showing hypoechoic area within the tendon reaching its articular surface. c SWE images showing focal area of tendon softening (blue color reaching its articular surface). SWV equals 2.9 m/s (dashed circle)
A significant difference was found in mean shear wave velocities between the different groups (P < 0.001), as illustrated in Table 1.
Correlation between MRI grades of supraspinatus tendon abnormality and the measured SWV
A significant negative correlation was found between the grades of tendon abnormalities on MRI and the measured SWV as illustrated in Fig. 7.
Discussion
Rotator cuff abnormalities including tendinopathy and tear are the main causes of shoulder pain and limited movement [1].
Imaging is crucial for the proper evaluation of rotator cuff abnormalities to guide treatment decisions [4].
Ultrasound elastography (UE) helps in the detection of tendon abnormalities through alteration in the tissue composition and elasticity before alteration in tendon echogenicity on the conventional US [16].
In the early 1990s, UE was first introduced in vitro. After that, many techniques of sonoelastography were introduced for use in practice including strain UE, shear wave UE, transient UE as well as acoustic radiation force UE [8].
Shear wave elastography is considered more objective in comparison with strain elastography, as no compression is applied to the examined tissues, allowing direct quantitative assessment of tissue elasticity as well as an examination of deeper tissue, not reached by the application of superficial compression [17].
SWE application in the musculoskeletal system is still limited with the Achilles tendon being the most commonly examined in UE research because of its superficial location, large size, and susceptibility to injury [18].
Shear wave speed versus tissue elasticity The calculation of tissue elasticity is based upon the assumptions that the soft tissues are elastic, incompressible, homogeneous, and isotropic. The SWS measured during SWE is only a portion of the calculation of the Young's modulus, which is needed to determine tissue elasticity, as E = 3µ = 3pcT2, where E = the Young's modulus, µ = the shear modulus, p = tissue density, and cT = the speed of transversely propagated waves, or shear waves. With this relationship, unless the tissue density is 1 g/mm3, the SWS does not correspond exactly with the Young's modulus. The musculoskeletal system, with its viscoelastic, heterogeneous, anisotropic tissues, presents inherent challenges to calculating tissue elasticity using the Young's modulus. As a result, SWE measurements in the musculoskeletal system should be presented in terms of SWS (m/s), rather than tissue elasticity (kPa) [19].
In the study, we used SWE in the assessment of supraspinatus tendon abnormalities and compared its results with tendon abnormalities on MRI as the reference standard for rotator cuff evaluation.
This study included 57 asymptomatic volunteers as controls and 57 patients with chronic shoulder pain and suspected supraspinatus tendon abnormalities; MRI revealed 21 patients with grade I tendinopathy (36.8 %), 27 patients with grade II tendinopathy (47.4 %), and 9 patients (15.8 %) with supraspinatus tendon tear (grade III).
The main findings of the study were that in SWE, the normal supraspinatus tendons appeared homogenous and stiff, whereas the pathological tendons appeared heterogeneous and soft with intra-tendinous color alterations. This is explained by the fact that tendinopathy represents collagen fiber degeneration and breaking down as well as fatty infiltration, resulting in tendon softening and weakness and may lead to spontaneous rupture of the tendon [20]. This is in agreement with Abdel Razek and Ezzat [21], Galletti et al. [22], Seo et al. [4], and Frere et al. [23] studies.
De Zordo et al. [24] also found that healthy elbow extensors and healthy Achilles tendons appear hard, while the pathological tendons showed abnormal softening, and Aubry et al. [25] also detected distinct softening in cases of Achilles tendinopathy compared to the healthy ones.
Regarding SWV measurements, the study showed reduced shear wave speed of the pathological tendons due to tendon softening which led to slower propagation of shear waves with a significant difference in SWV values between the volunteers and cases and a significant difference in SWV values between cases with different grades of tendon abnormalities; this is in agreement with Dirrichs et al. [26], Lee et al. [16], Hou et al. [27], Coombes et al. [28], and Lawrence et al. [29].
However, the study done by Hou et al. [27] showed mean and median SWV values of 8–9 m/s in patients with normal or mild tendinopathy and 5–7 m/s in cases of tendinopathy and tear, while in our study the SWV for healthy supraspinatus tendons was approximately 6–8 m/s and 2.7–5.1 m/s in patients with tendinopathy and tear. This difference in values of SWV may be attributed to data acquisition using SWE technology from a different manufacturer (they used Siemens and in our study we used Toshiba).
In another study done by Baumer et al. [30], no significant difference was detected between the age-matched control subjects and RC tendinopathy patients with a range of SWV measurements being 2.0–4.5 m/s for RC tendinopathy patients and 2.5–3.9 m/s for control subjects under passive condition, but significant differences were found between the age-matched patients and control subjects under active conditions, with a range of SWV being 2.5–7.3 m/s for patients and 4.2–7.7 m/s for age-matched control subjects.
This difference in SWV values may be attributed to data acquisition using SWE technology from a different manufacturer (they used Siemens and in our study we used Toshiba); another factor that may be contributed to the differences in SWV measurements is the arm position during data acquisition, as in their study for the passive examination, the participants were examined in a sitting position with the elbow resting on a 30° abduction pillow and the forearm in pronation and resting on their thigh, while in our study the patient was examined under the passive condition with the patient in standard crass position as well as they examined the intramuscular portion of the supraspinatus tendon, while we examined the distal portion near the tendon insertion.
The study showed that SWE could detect different rotator cuff disorders with a highly significant negative correlation between the measured SWV and the morphological grades of tendon abnormalities (P < 0.001); this is in agreement with other studies that used SWE as done by Hou et al. [27] that showed a highly significant weak-to-moderate negative correlation between the measured SWS and morphologic grade in both the proximal and distal RC tendon, and other studies used strain elastography as done by Vasishta et al. [31] that showed a moderate-to-strong linear association between the MRI grade and the stiffness with a perfect negative correlation between the grade of tendinopathy and strain ratio.
Other studies that used strain elastography showed a good correlation between SE and morphological grades of tendinopathy as shown in the following studies:
-
Frere et al. [23] showed a better correlation of SE findings with MRI than the conventional US in the detection of different RC lesions.
-
Khodair and Ghieda [32] showed increased sensitivity and specificity of sonoelastography in the detection of rotator cuff disorders than conventional ultrasound with the US showing a sensitivity of 85% and specificity of 95%, while SE showed a sensitivity of 95% and specificity of 100%.
-
Seo et al. [4] reported that SE showed higher reliability in the detection and grading of supraspinatus tendinopathy than the conventional US, and they explained their result as the color-coding system of SE used in the assessment of the tendon was more objective than evaluating the proportion of heterogeneous echogenicity used on B-mode US.
-
Likewise, Klauser et al. [33] found that SE showed a good correlation when compared with conventional B-mode US in cases of Achilles tendinopathy, and De Zordo et al. [24] reported that SE has better sensitivity, specificity, and accuracy in the detection of lateral epicondylitis than the B-mode US.
However, a study done by Lawrence et al. [29] showed that estimated shear modulus was not significantly associated with tear size, tear retraction, or fatty infiltration under any testing condition and explained their result as conventional MRI imaging assesses structural and compositional abnormalities within the tendon, whereas SWE assesses tissue quality.
The introduction of SWE in musculoskeletal application and especially for rotator cuff disorders is relatively recent. In this field, SWE gives further qualitative and quantitative information about tendon quality, thus improving the diagnostic capabilities of conventional ultrasound as the first-line imaging modality; also, SWE provides a real-time and dynamic examination of RC tendons without the presence of any contraindications, so it can be used complementary to MRI in the evaluation of RC disorders, especially if there is a contraindication to MRI.
However, limitations of SWE are as follows: the region of interest must be at least 1–2 mm away from the skin surface, and it is also not applicable in very-high-frequency probes as well as the differences present in the measured SWV between the different manufacturers with the absence of standardized measurements [34].
Limitations of the study
The limitations included lack of age and sex matching between the cases and controls due to the high prevalence of tendinopathy in older participants (however the differences between the two groups were not statistically significant), a low number of participants with a limited number of patients with rotator cuff tears, and a lack of assessment of different types of rotator cuff tears.
Conclusions
The clinical utility of SWE in the musculoskeletal system is not yet well established; our study showed that SWE could differentiate between patients with RC abnormalities and asymptomatic control individuals with a good correlation to MRI and agreement with the previously published studies. So SWE can be used for the detection of tendon abnormality even before alterations in tendon echogenicity or thickness on the conventional US. Also can supplement important information to the traditional RC imaging such as tendon quality which is considered a prognostic factor for rotator cuff repair.
Future applications of SWE in clinical practice might include early diagnosis/screening, monitoring response to recent treatment regimens or rehabilitation programs, time-effective and low-cost follow-up, and prediction of surgical outcomes.
However, further research on the use of SWE US in the musculoskeletal system is needed as it is more objective and reliable with further research needed including a large population, long-term follow-up and correlation with clinical data, histological findings, conventional imaging, and surgical outcome for standardization of the examination technique and standardization of reference values of SWV at different anatomical regions of clinical interest.
Availability of data and materials
All the datasets used and analyzed in this study are available with the corresponding author upon reasonable request.
Abbreviations
- US:
-
Ultrasound
- SWV:
-
Shear wave velocity
- MRI:
-
Magnetic resonance imaging
- PTT:
-
Partial-thickness tear
- FTT:
-
Full-thickness tear
- UE:
-
Ultrasound elastography
- SWE:
-
Shear wave elastography
- MSK:
-
Musculoskeletal
- B-mode:
-
Brightness mode
- ROI:
-
Region of interest
- TR:
-
Repetition time
- TE:
-
Echo time
- FOV:
-
Field of view
- STIR:
-
Short tau inversion recovery
- FFE:
-
Fast field echo imaging
- SE:
-
Sonoelastography
- SWS:
-
Shear wave speed
- kPa:
-
Kilo Pascal
- RC:
-
Rotator cuff
References
Tawfik AM, El-Morsy A, Badran MA (2014) Rotator cuff disorders: How to write a surgically relevant magnetic resonance imaging report? World J Radiol 6(6):274
Bendale S, Vedpathak S (2019) Sonographic Evaluation of rotator cuff pathologies causing restricted movements of shoulder. Int J Contemp Med Surg Radiol 4(3):C276–C280
Boenisch U, Lembcke O, Naumann T (2000) Classification, clinical findings and operative treatment of degenerative and posttraumatic shoulder disease: what do we really need to know from an imaging report to establish a treatment strategy? Eur J Radiol 35(2):103–118
Seo JB, Yoo JS, Ryu JW (2015) Sonoelastography findings of supraspinatus tendon in rotator cuff tendinopathy without tear: comparison with magnetic resonance images and conventional ultrasonography. J Ultrasound 18(2):143–149
Vlychou M, Dailiana Z, Fotiadou A, Papanagiotou M, Fezoulidis IV, Malizos K (2009) Symptomatic partial rotator cuff tears: diagnostic performance of ultrasound and magnetic resonance imaging with surgical correlation. Acta Radiol 50(1):101–105
Hodgson RJ, O’Connor PJ, Grainger AJ (2012) Tendon and ligament imaging. Br J Radiol 85(1016):1157–1172
Venu KM, Howlett DC, Garikipati R, Anderson HJ, Bonnici AV (2002) Evaluation of the symptomatic supraspinatus tendon—a comparison of ultrasound and arthroscopy. Radiography 8(4):235–240
Manzoor I, Bacha R, Gilani SA (2018) Diagnostic accuracy of sonoelastography in different diseases. J Ultrasonogr 18(72):29
Guibal A, Boularan C, Bruce M, Vallin M, Pilleul F, Walter T, Lefort T (2013) Evaluation of shear wave elastography for the characterisation of focal liver lesions on ultrasound. Eur Radiol 23(4):1138–1149
Cosgrove D, Piscaglia F, Bamber J, Bojunga J, Correas JM, Gilja OH, Dietrich CF (2013) EFSUMB guidelines and recommendations on the clinical use of ultrasound elastography, part 2: clinical applications. Ultraschall Medizin Eur J Ultras 34(03):238–253
Winn N, Lalam R, Cassar-Pullicino V (2016) Sonoelastography in the musculoskeletal system: current role and future directions. World J Radiol 8(11):868
Balaban M, Idilman IS, Ipek A, Ikiz SS, Bektaser B, Gumus M (2016) Elastographic findings of Achilles tendons in asymptomatic professional male volleyball players. J Ultrasound Med 35(12):2623–2628
Chan YH (2003) Biostatistics102: quantitative data—parametric and non-parametric tests. Singapore Med J 44(8):391–396
Chan YH (2003) Biostatistics 103: qualitative data—tests of independence. Singapore Med J 44(10):498–503
Chan YH (2003) Biostatistics 104: Correlational analysis. Singapore Med J 44(12):614–619
Lee SU, Joo SY, Kim SK, Lee SH, Park SR, Jeong C (2016) Real-time sonoelastography in the diagnosis of rotator cuff tendinopathy. J Shoulder Elbow Surg 25(5):723–729
Li Y, Snedeker JG (2011) Elastography: modality-specific approaches, clinical applications, and research horizons. Skeletal Radiol 40(4):389–397
Rosskopf AB, Ehrmann C, Buck FM, Gerber C, Flück M, Pfirrmann CW (2016) Quantitative shear-wave US elastography of the supraspinatus muscle: reliability of the method and relation to tendon integrity and muscle quality. Radiology 278(2):465–474
Davis LC, Baumer TG, Bey MJ, Van Holsbeeck M (2019) Clinical utilization of shear wave elastography in the musculoskeletal system. Ultrasonography 38(1):2
Kainberger F, Mittermaier F, Seidl G, Parth E, Weinstabl R (1997) Imaging of tendons—adaptation, degeneration, rupture. Eur J Radiol 25(3):209–222
Abdel Razek N, Ezzat L (2008) Real-time sono-elastography in assessment of rotator cuff tendon tears: comparison of findings between elastography and MRI in healthy volunteers and patients with shoulder pain. RSNA
Galletti S, Oliva F, Masiero S, Frizziero A, Galletti R, Schiavone C, Abate M (2015) Sonoelastography in the diagnosis of tendinopathies: an added value. Muscles Ligam Tendons J 5(4):325
Frere RA, Libda I, Tantawy F, Sakr HM, El-Alfy AT (2021) Sonoelastography, conventional ultrasound and magnetic resonance imaging in detection of rotator cuff lesions in patients with chronic shoulder pain. Egyp Rheumatol 43(1):17–21
De Zordo T, Lill SR, Fink C, Feuchtner GM, Jaschke W, Bellmann-Weiler R, Klauser AS (2009) Real-time sonoelastography of lateral epicondylitis: comparison of findings between patients and healthy volunteers. Am J Roentgenol 193(1):180–185
Aubry S, Nueffer JP, Tanter M, Becce F, Vidal C, Michel F (2015) Viscoelasticity in Achilles tendinopathy: quantitative assessment by using real-time shear-wave elastography. Radiology 274(3):821–829
Dirrichs T, Quack V, Gatz M, Tingart M, Kuhl CK, Schrading S (2016) Shear wave elastography (SWE) for the evaluation of patients with tendinopathies. Acad Radiol 23(10):1204–1213
Hou SW, Merkle AN, Babb JS, McCabe R, Gyftopoulos S, Adler RS (2017) Shear wave ultrasound elastographic evaluation of the rotator cuff tendon. J Ultrasound Med 36(1):95–106
Coombes BK, Tucker K, Vicenzino B, Vuvan V, Mellor R, Heales L, Hug F (2018) Achilles and patellar tendinopathy display opposite changes in elastic properties: a shear wave elastography study. Scand J Med Sci Sports 28(3):1201–1208
Lawrence RL, Ruder MC, Moutzouros V, Makhni EC, Muh SJ, Siegal D, Bey MJ (2021) Ultrasound shear wave elastography and its association with rotator cuff tear characteristics. JSES Int 5(3):500–506
Baumer TG, Dischler J, Davis L, Labyed Y, Siegal DS, Van Holsbeeck M, Bey MJ (2018) Effects of age and pathology on shear wave speed of the human rotator cuff. J Orthop Res 36(1):282–288
Vasishta A, Kelkar A, Joshi P, Hapse R (2019) The value of sonoelastography in the diagnosis of supraspinatus tendinopathy—a comparison study. Br J Radiol 92(1096):20180951
Khodair SAZ, Ghieda U (2016) Rotator cuff tendinopathy; comparison between conventional sonography, sonoelastography, and MRI in healthy volunteers and patients with shoulder pain. In: European congress of radiology-ECR
Klauser AS, Miyamoto H, Tamegger M, Faschingbauer R, Moriggl B, Klima G, Jaschke WR (2013) Achilles tendon assessed with sonoelastography: histologic agreement. Radiology 267(3):837–842
Kocyigit F, Kuyucu E, Kocyigit A, Herek DT, Savkin R, Aslan UB (2016) Investigation of biomechanical characteristics of intact supraspinatus tendons in subacromial impingement syndrome: a cross-sectional study with real-time sonoelastography. Am J Phys Med Rehabil 95(8):588–596
Acknowledgements
Not applicable.
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
AAH and HMS put the idea of the study, are the editors of the manuscript, and participated in the study design. GRH participated in the study design and performed the statistical analysis. NEE and WRM contributed to patients collection and clinical assessment. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Written informed consent was signed by all patients before the examination. The study was approved by the research committee of Faculty of Medicine, Kasr Alainy Hospital, Cairo University, 2019. The reference number provided by the committee was MD-59-2019.
Consent for publication
All patients included in this research were fully conscious and gave written informed consent to publish the data contained within this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gadalla, A.A.E.H., Hassanein, G.R., El Azizy, H.M.S. et al. Sono-elastography findings of supraspinatus tendon in supraspinatus tendinopathy and tear: comparison study with magnetic resonance imaging. Egypt J Radiol Nucl Med 54, 37 (2023). https://doi.org/10.1186/s43055-023-00990-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43055-023-00990-6