Abstract
Purpose
In kinematically aligned total knee arthroplasty (TKA), it is necessary to infer the pre-arthritic constitutional medial proximal tibial angle (MPTA) in advanced osteoarthritis (OA) of the knee with bone loss. The aim of this study was to investigate whether MPTA at the posterior tibial plateau represents the pre-arthritic constitutional MPTA in anterior cruciate ligament (ACL)-intact, advanced OA knees. It was hypothesized that MPTA at the posterior tibial plateau represents the pre-arthritic constitutional MPTA of ACL-intact, advanced knee OA.
Methods
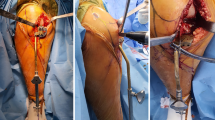
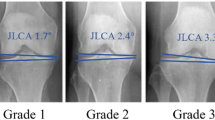
One hundred varus, anterior cruciate ligament (ACL)-intact, advanced OA knees were analysed. The hip–knee–ankle (HKA) angle and MPTA were assessed on computed radiography (CR) and MPTAs at the anterior, middle, and posterior part of the tibial plateau were assessed on computed tomography (CT) images. The association between these parameters was also analysed.
Results
CR images showed an HKA angle of 172.4 ± 4.1° and MPTA of 84.3 ± 2.5°. CT images showed different MPTAs in the three regions, ranging from 83.9 ± 2.4° to 85.9 ± 2.8°. The middle MPTA was the lowest at 83.9 ± 2.4°. HKA angle correlated with the middle MPTA (r = 0.3355, 95% confidence interval [CI] 0.1489–0.4991, p = 0.0006) and ΔMPTA (Middle-Posterior) (r = 0.5128, 95% CI 0.3518–0.6443, p < 0.0001).
Conclusion
The MPTA at the posterior tibial plateau represents the pre-arthritic constitutional MPTA in ACL-intact, advanced OA knees.
Level of evidence
III, retrospective cohort study.



Similar content being viewed by others
References
Almaawi AM, Hutt JRB, Masse V, Lavigne M, Vendittoli PA (2017) The impact of mechanical and restricted kinematic alignment on knee anatomy in total knee arthroplasty. J Arthroplast 32:2133–2140. https://doi.org/10.1016/j.arth.2017.02.028
Blakeney W, Beaulieu Y, Kiss MO, Rivière C, Vendittoli PA (2019) Less gap imbalance with restricted kinematic alignment than with mechanically aligned total knee arthroplasty: simulations on 3-D bone models created from CT-scans. Acta Orthop 90:602–609. https://doi.org/10.1080/17453674.2019.1675126
Calek AK, Hochreiter B, Hess S, Amsler F, Leclerq V, Hirschmann MT, Behrend H (2021) High inter- and intraindividual differences in medial and lateral posterior tibial slope are not reproduced accurately by conventional TKA alignment techniques. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06477-z
Calliess T, Bauer K, Stukenborg-Colsman C, Windhagen H, Budde S, Ettinger M (2017) PSI kinematic versus non-PSI mechanical alignment in total knee arthroplasty: a prospective, randomized study. Knee Surg Sports Traumatol Arthrosc 25:1743–1748. https://doi.org/10.1007/s00167-016-4136-8
Delport H, Labey L, Innocenti B, De Corte R, Vander Sloten J, Bellemans J (2015) Restoration of constitutional alignment in TKA leads to more physiological strains in the collateral ligaments. Knee Surg Sports Traumatol Arthrosc 23:2159–2169. https://doi.org/10.1007/s00167-014-2971-z
Hess S, Moser LB, Amsler F, Behrend H, Hirschmann MT (2019) Highly variable coronal tibial and femoral alignment in osteoarthritic knees: a systematic review. Knee Surg Sports Traumatol Arthrosc 27:1368–1377. https://doi.org/10.1007/s00167-019-05506-2
Hess S, Moser LB, Robertson EL, Behrend H, Amsler F, Iordache E et al (2021) Osteoarthritic and non-osteoarthritic patients show comparable coronal knee joint line orientations in a cross-sectional study based on 3D reconstructed CT images. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06740-3
Hirschmann MT, Behrend H (2018) Functional knee phenotypes: a call for a more personalised and individualised approach to total knee arthroplasty? Knee Surg Sports Traumatol Arthrosc 26:2873–2874. https://doi.org/10.1007/s00167-018-4973-8
Hirschmann MT, Hess S, Behrend H, Amsler F, Leclercq V, Moser LB (2019) Phenotyping of hip–knee–ankle angle in young non-osteoarthritic knees provides better understanding of native alignment variability. Knee Surg Sports Traumatol Arthrosc 27:1378–1384. https://doi.org/10.1007/s00167-019-05507-1
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclercq V, Hess S (2019) Phenotyping the knee in young non-osteoarthritic knees shows a wide distribution of femoral and tibial coronal alignment. Knee Surg Sports Traumatol Arthrosc 27:1385–1393. https://doi.org/10.1007/s00167-019-05508-0
Hirschmann MT, Moser LB, Amsler F, Behrend H, Leclerq V, Hess S (2019) Functional knee phenotypes: a novel classification for phenotyping the coronal lower limb alignment based on the native alignment in young non-osteoarthritic patients. Knee Surg Sports Traumatol Arthrosc 27:1394–1402. https://doi.org/10.1007/s00167-019-05509-z
Ho JPY, Merican AM, Hashim MS, Abbas AA, Chan CK, Mohamad JA (2017) Three-dimensional computed tomography analysis of the posterior tibial slope in 100 knees. J Arthroplast 32:3176–3183. https://doi.org/10.1016/j.arth.2017.04.060
Howell SM, Papadopoulos S, Kuznik KT, Hull ML (2013) Accurate alignment and high function after kinematically aligned TKA performed with generic instruments. Knee Surg Sports Traumatol Arthrosc 21:2271–2280. https://doi.org/10.1007/s00167-013-2621-x
Hunter DJ, Guermazi A, Lo GH, Grainger AJ, Conaghan PG, Boudreau RM, Roemer FW (2011) Evolution of semi-quantitative whole joint assessment of knee OA: MOAKS (MRI Osteoarthritis Knee Score). Osteoarthr Cartil 19:990–1002. https://doi.org/10.1016/j.joca.2011.05.004
Jenny JY, Baldairon F, Hirschmann MT (2021) Functional knee phenotypes of OA patients undergoing total knee arthroplasty are significantly more varus or valgus than in a non-OA control group. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-021-06687-5
Ji HM, Han J, Jin DS, Seo H, Won YY (2016) Kinematically aligned TKA can align knee joint line to horizontal. Knee Surg Sports Traumatol Arthrosc 24:2436–2441. https://doi.org/10.1007/s00167-016-3995-3
Kawahara S, Mawatari T, Matsui G, Mizu-Uchi H, Hamai S, Akasaki Y et al (2021) Malrotation of whole-leg radiograph less than 10 degrees does not influence preoperative planning in open-wedge high tibial osteotomy. J Orthop Res 39:1505–1511. https://doi.org/10.1002/jor.24845
Kawakami H, Sugano N, Yonenobu K, Yoshikawa H, Ochi T, Hattori A et al (2004) Effects of rotation on measurement of lower limb alignment for knee osteotomy. J Orthop Res 22:1248–1253. https://doi.org/10.1016/j.orthres.2004.03.016
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502. https://doi.org/10.1136/ard.16.4.494
Lankester BJ, Cottam HL, Pinskerova V, Eldridge JD, Freeman MA (2008) Variation in the anatomy of the tibial plateau: a possible factor in the development of anteromedial osteoarthritis of the knee. J Bone Jt Surg Br 90:330–333. https://doi.org/10.1302/0301-620X.90B3.19898
Lee YS, Howell SM, Won YY, Lee OS, Lee SH, Vahedi H et al (2017) Kinematic alignment is a possible alternative to mechanical alignment in total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 25:3467–3479. https://doi.org/10.1007/s00167-017-4558-y
León-Muñoz VJ, López-López M, Martínez-Martínez F, Santonja-Medina F (2020) Comparison of weight-bearing full-length radiographs and computed-tomography-scan-based three-dimensional models in the assessment of knee joint coronal alignment. Knee 27:543–551. https://doi.org/10.1016/j.knee.2019.11.017
Longstaff LM, Sloan K, Stamp N, Scaddan M, Beaver R (2009) Good alignment after total knee arthroplasty leads to faster rehabilitation and better function. J Arthroplast 24:570–578. https://doi.org/10.1016/j.arth.2008.03.002
MacDessi SJ, Griffiths-Jones W, Chen DB, Griffiths-Jones S, Wood JA, Diwan AD et al (2020) Restoring the constitutional alignment with a restrictive kinematic protocol improves quantitative soft-tissue balance in total knee arthroplasty: a randomized controlled trial. Bone Jt J 102-b:117–124. https://doi.org/10.1302/0301-620X.102B1.BJJ-2019-0674.R2
MacDessi SJ, Griffiths-Jones W, Harris IA, Bellemans J, Chen DB (2020) The arithmetic HKA (aHKA) predicts the constitutional alignment of the arthritic knee compared to the normal contralateral knee: a matched-pairs radiographic study. Bone Jt Open 1:339–345. https://doi.org/10.1302/2633-1462.17.BJO-2020-0037.R1
McEwen P, Balendra G, Doma K (2019) Medial and lateral gap laxity differential in computer-assisted kinematic total knee arthroplasty. Bone Jt J 101-b:331–339. https://doi.org/10.1302/0301-620X.101B3.BJJ-2018-0544.R1
McEwen PJ, Dlaska CE, Jovanovic IA, Doma K, Brandon BJ (2020) Computer-assisted kinematic and mechanical axis total knee arthroplasty: a prospective randomized controlled trial of bilateral simultaneous surgery. J Arthroplast 35:443–450. https://doi.org/10.1016/j.arth.2019.08.064
Meier M, Janssen D, Koeck FX, Thienpont E, Beckmann J, Best R (2021) Variations in medial and lateral slope and medial proximal tibial angle. Knee Surg Sports Traumatol Arthrosc 29:939–946. https://doi.org/10.1007/s00167-020-06052-y
Moser LB, Hess S, Amsler F, Behrend H, Hirschmann MT (2019) Native non-osteoarthritic knees have a highly variable coronal alignment: a systematic review. Knee Surg Sports Traumatol Arthrosc 27:1359–1367. https://doi.org/10.1007/s00167-019-05417-2
Nakagawa S, Arai Y, Inoue H, Fujii Y, Kaihara K, Mikami Y (2020) Relationship of alignment in the lower extremity with early degeneration of articular cartilage after resection of the medial meniscus: quantitative analysis using T2 mapping. Medicine (Baltim) 99:e22984. https://doi.org/10.1097/MD.0000000000022984
Ogawa H, Matsumoto K, Akiyama H (2018) Coronal tibiofemoral subluxation is correlated to correction angle in medial opening wedge high tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 26:3482–3490. https://doi.org/10.1007/s00167-018-4948-9
Ogawa H, Matsumoto K, Akiyama H (2019) Effect of increased posterior tibial slope on the anterior cruciate ligament status in medial open wedge high tibial osteotomy in an uninjured ACL population. Orthop Traumatol Surg Res 105:1085–1091. https://doi.org/10.1016/j.otsr.2019.05.003
Rivière C, Lazic S, Villet L, Wiart Y, Allwood SM, Cobb J (2018) Kinematic alignment technique for total hip and knee arthroplasty: the personalized implant positioning surgery. EFORT Open Rev 3:98–105. https://doi.org/10.1302/2058-5241.3.170022
Seidenstein A, Birmingham M, Foran J, Ogden S (2021) Better accuracy and reproducibility of a new robotically-assisted system for total knee arthroplasty compared to conventional instrumentation: a cadaveric study. Knee Surg Sports Traumatol Arthrosc 29:859–866. https://doi.org/10.1007/s00167-020-06038-w
Vanlommel L, Vanlommel J, Claes S, Bellemans J (2013) Slight undercorrection following total knee arthroplasty results in superior clinical outcomes in varus knees. Knee Surg Sports Traumatol Arthrosc 21:2325–2330. https://doi.org/10.1007/s00167-013-2481-4
Waterson HB, Clement ND, Eyres KS, Mandalia VI, Toms AD (2016) The early outcome of kinematic versus mechanical alignment in total knee arthroplasty: a prospective randomised control trial. Bone Jt J 98-b:1360–1368. https://doi.org/10.1302/0301-620X.98B10.36862
White SH, Ludkowski PF, Goodfellow JW (1991) Anteromedial osteoarthritis of the knee. J Bone Jt Surg Br 73:582–586. https://doi.org/10.1302/0301-620X.73B4.2071640
Yoon JR, Lee JK, Ryu J, Um R, Yang JH (2021) Increased external rotation of the osteoarthritic knee joint according to the genu varum deformity. Knee Surg Sports Traumatol Arthrosc 29:1098–1105. https://doi.org/10.1007/s00167-020-06100-7
Author information
Authors and Affiliations
Contributions
HO: study design, data collection and analysis, statistical analysis, initial draft preparation. YN, KS, MS, TS, KO: initial draft preparation and data collection. KM, HA: initial draft preparation. All authors read and approved the final version of the paper.
Corresponding author
Ethics declarations
Conflict of interest
None of the authors have any conflicts of interest to declare.
Funding
No external funding was received for this study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards. This cross-sectional study was approved by the Institutional Review Board of Ogaki Tokushukai Group (Approval number TGE01668-066).
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Ogawa, H., Nakamura, Y., Sengoku, M. et al. Medial proximal tibial angle at the posterior tibial plateau represents the pre-arthritic constitutional medial proximal tibial angle in anterior cruciate ligament-intact, advanced osteoarthritis of the knee. Knee Surg Sports Traumatol Arthrosc 30, 2941–2947 (2022). https://doi.org/10.1007/s00167-022-06890-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-022-06890-y