Abstract
Purpose
Arthroscopic lateral retinacular release (LRR) has long been considered the gold standard for the treatment for anterior knee pain caused by lateral retinacular tightness (LRT). However, one-third of patients experience continuous pain postoperatively, which is thought to be related to persistent maltracking of the patella and altered femoro-tibial kinematics. Therefore, the aim of the present study was to simultaneously assess femoro-tibial and patello-femoral kinematics and identify the influence of arthroscopic LRR.
Methods
Sixteen healthy volunteers and 12 patients with unilateral, isolated LRT were prospectively included. Open MRI scans with and without isometric quadriceps contraction were performed in 0°, 30° and 90° of knee flexion preoperatively and at 12 months after surgery. Patellar shift, tilt angle, patello-femoral contact area and magnitude of femoro-tibial rotation were calculated by digital image processing.
Results
Postoperatively, patellar shift was significantly reduced at 90° of knee flexion compared to preoperative values. The postoperative patellar tilt angle was found to be significantly smaller at 30° of knee flexion compared to that preoperatively. Isometric muscle contractions did not considerably influence patellar shift or tilt in either group. The patello-femoral contact area increased after LRR over the full range of motion (ROM), with significant changes at 0° and 90°. Regarding femoro-tibial kinematics, significantly increased femoral internal rotation at 0° was observed in the patient group preoperatively, whereas the magnitude of rotation at 90° of knee flexion was comparable to that of healthy individuals. The pathologically increased femoral internal rotation at 30° without muscular activity could be significantly decreased by LRR. With isometric quadriceps contraction no considerable improvement of femoral internal rotation could be achieved by LRR at 30° of knee flexion.
Conclusions
Patello-femoral and femoro-tibial joint kinematics could be improved, making LRR a viable surgical option in carefully selected patients with isolated LRT. However, pathologically increased femoral internal rotation during early knee flexion remained unaffected by LRR and thus potentially accounts for persistent pain.
Level of evidence
II.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Arthroscopic lateral retinacular release (LRR) has long been the treatment of choice for lateral patellar compression syndrome and patellar maltracking [30]. Nowadays, this diagnose complex is considerably differentiated and multiple factors have been identified to account for lateral patellar compression [4, 12]. Increase of patellar instability due to LRR and shortcoming of addressing all causative factors of the lateral patellar compression syndrome complex may lead to persistent maltracking [1, 12]. Accordingly, only isolated lateral retinacular tightness (LRT) is adequately addressed by LRR. However, one-third of these patients experience residual pain postoperatively indicating persistent patellar maltracking potentially influenced by pathological femoro-tibial kinematics [9].
Multiple analysis techniques for the identification of patellar kinematics have previously been applied [21, 23, 27]. Conventional radiography, however, has been proven to insufficiently assess the complex patellar motion patterns [12, 36]. 2D MRI and CT scans, on the other hand, significantly lack reproducibility regarding layer plane and orientation [4, 12]. Furthermore, 2D analysis techniques and fluoroscopy restrict the analysis to a single plane. Motion patterns perpendicular to the layer plane can rarely be assessed by these procedures, so it is not feasible to quantify 3D patellar kinematics or evaluate a potential relationship between femoro-tibial and patello-femoral motion patterns [7].
No in vivo studies have focused on the simultaneous analysis of patello-femoral and femoro-tibial kinematics in patients with LRT; yet, these data are critical for understanding the processes involved. Consequently, this knowledge may unveil if (1) patellar maltracking in patients with isolated LRT is caused by altered patello-femoral and femoro-tibial kinematics and if (2) pathological patellar tracking and femoro-tibial kinematics can be improved by arthroscopic LRR.
Materials and methods
All patients and volunteers were provided with all relevant information before the beginning of the study, and written consent was obtained. The present study was approved by the institutional ethics committee of the Goethe University Frankfurt (IRB number 118/02).
Sixteen healthy volunteers (age 22–36 years; eight females, eight males) were recruited among the institutional staff and physiological values were determined. Healthy individuals had neither a history nor diagnosis of knee or hip pathology nor patello-femoral pain.
Twelve patients (age 16–44 years; nine females, three males) with a diagnosis of unilateral, isolated LRT without patellar instability or a history of patellar dislocation were prospectively included in this study. All patients reported about pain during specific activities such as ascending and/or descending stairs, squatting, kneeling, jumping, long-sitting or running. Two independent senior orthopaedic surgeons diagnosed the cases on the basis of the patient’s medical history, clinical examination and conventional radiography as well as MRI findings. Specific in- and exclusion criteria are shown in Fig. 1. For the present study examinations and imaging scans were performed preoperatively and at 12 months after arthroscopic lateral release. In all cases, the diagnosis was confirmed intraoperatively.
Surgical technique
All surgeries were performed under general anaesthesia. Standard arthroscopic portals were established and the joint was thoroughly evaluated. Chondral lesions were documented if present. Due to the exclusion of patients with cartilage defects greater than Outerbridge I, no cartilage reconstructions techniques had to be applied (Fig. 1). Subsequently, patellar tracking was evaluated arthroscopically, and then, LRR was performed using electrocautery. The release was carried out without affecting any muscle tissue. Conclusively, final patella tracking was verified.
Postoperatively, all patients were allowed to perform full weight-bearing as tolerated without any limitations in flexion. Physiotherapy was started immediately after the operation.
Magnetic resonance imaging
Imaging scans were performed in an open MRI scanner (0.2T, MRT-open, Siemens, Erlangen) using an optimized T1-weighted 3D gradient echo sequence (TR = 16.1 ms; TE = 7.0 ms; Flipwinkel 30°) with a pixel size of 0.9 mm and a layer thickness of 1.9 mm. During the imaging scans, the patients were placed in lateral position and a positioning splint, ensuring the reproducibility of different flexion angles. Thus, the examined extremity was perfectly aligned with the longitudinal axis of the MRI scanner. Then, the patients were verified to be in the correct position with a localizer.
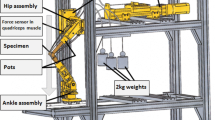
Initially, imaging of the affected knees was performed without muscular contractions in 0°, 30° and 90° of flexion. To investigate the influence of muscular activity during extension of the knee on patello-femoral kinematics, the procedure was repeated under isometric muscular activity. Therefore, an external weight was applied on the positioning splint with a torque of 10 Nm over the knee joint. Additionally, the patient had to keep contact with a specific area of the splint during the whole acquisition process to limit motion artefacts. Potential influence of muscular exhaustion was excluded by prior electromyography analysis.
Digital image processing
The digital image processing technique has been previously published by our group [34]. In brief, three-dimensional semi-automated segmentation reconstruction of the bony structures (femur, tibia, patella) was performed. For additional calculations of the patello-femoral kinematics, a patella-based coordinate system was implemented, with the patellar centre of gravity as the origin.
The relative orientation and position of the patella in relation to the femoral bearing surface were defined automatically by femoral reference points. For the medial and lateral condyles, these points were configured by determining the shortest distance to the y–z-axis (frontal plane; x = 0) in the MRI data. For the depth of the femoral bearing trochlea, the point with the farthest distance from the y–z-axis (frontal plane; x = 0) was identified in accordance with the definition of the 1st femoral eigenvector by main axis transformation. Additionally, a local tibia-based coordinate system was applied according to the magnitude of tibial rotation. Finally, the tibia-based coordinate system and the femoral reference points were projected into the coordinate system of the patella. Thus, the quantification of the patellar alignment relative to the femur and tibia allowed an accurate characterization of the patellar kinematics by well-established 2D parameters.
The femoro-patellar contact area was calculated by separately segmenting the femoral and patellar cartilage. Second, all points in each layer with a distance of zero between the femoral and patellar cartilage surfaces were identified and collectively defined as the femoro-patellar contact area.
This MRI-based image processing technique has been extensively described in previous studies and a high reproducibility with a coefficient of variation (CV) of between 0.012 and 0.083 depending on the analysed parameter has been reported [10, 34].
Primary outcome parameters were improvement of patello-femoral maltracking, in particular patellar shift, tilt and contact area, as well as femoro-tibial rotation.
Statistical analysis
All the data collected in this study were recorded and analysed using SPSS software (IBM, Armonk, NY). The normality of the data was assessed by the Shapiro–Wilk test. Pre- and postoperative results in the patient group were compared using the t test for paired samples (CI 95%). The patient and healthy control groups were compared using the t test for unpaired samples, with a 95% confidence interval. Regression analysis was performed to assess the impact of femoro-tibial rotation on the patella-femoral kinematics.
Sample sample-size power analysis of β = 0.20 and α = 0.05 was performed for a pilot study using mean differences for patellar tilt between the groups. Based on this analysis, a maximum of 11 participants per group was needed to power the study adequately.
Results
Patello-femoral kinematics
Patella shift
In the healthy knee joints a decrease in patellar shift was found from 0° to 30°, whereas a significant increase was identified at 90° of flexion (p = 0.046). Preoperatively, the knee joints of the patient group showed a continuous increase in patellar shift throughout knee flexion (Fig. 2a). Patellar shift slightly increased from pre- to postoperatively at 0° and 30° of flexion but significantly decreased at 90° of knee flexion (Table 1). The analysis of patellar shift with isometric muscle contraction revealed similar results.
Patello-femoral and femoro-tibial kinematics in healthy knees and knees with LRT preoperatively and after arthroscopic LRR during knee flexion (0°–90°) with and without isometric muscle activity; a patellar shift; b patellar tilt; c patello-femoral contact area; d femoral rotation (negative values indicate femoral internal rotation based on a tibial coordinate system). *Statistical significance (p ≤ 0.05)
Patella tilt
In healthy knee joints patella tilt angle slightly increased from 0° to 30° of flexion. A significant increase in patellar tilt was observed at 90° of flexion (Fig. 2b). The patient knee joints preoperatively showed a consistent, yet insignificant, increase throughout knee flexion (Fig. 2b). These values significantly differed from those in the control group at 0° and 30° (Table 1). The postoperative assessment revealed a decrease in patellar tilt at each measured degree of knee flexion compared to the preoperative values, with significant results at 30° of knee flexion (Table 1). Isometric quadriceps activity showed postoperatively significantly higher patellar tilt values at 0° and 30° of flexion in the patient group compared to the healthy control group (Table 1).
Patello-femoral contact area
A continuous increase of patello-femoral contact area throughout knee flexion could be observed in healthy individuals and the patient group (Fig. 2c). Preoperatively, smaller patello-femoral contact areas were found in the patient group compared to the control group. Following LRR significantly higher values were observed at 0° and 90° of flexion (Table 1). Isometric muscle contractions only had a minor effect on the patello-femoral contact area.
Femoro-tibial kinematics
Femoral rotation
Healthy knees showed a marginal increase of femoral internal rotation from 0° to 30° and a significant decrease at 90°, corresponding to dorsal translation of the lateral condyle during larger degrees of flexion (Fig. 2d). Similar kinematics were identified in the patient group. After LRR, less femoral internal rotation was observed at any degree of flexion compared to preoperative values. Additionally, postoperative values of femoral rotation were found to be almost equal to those of the healthy control group in extension and at 30° flexion (Table 1). A significant reduction of femoral internal rotation was observed with isometric muscle contraction compared to without muscle contractions in healthy knee joints at 0° and 30° of flexion, whereas the patient group only showed a minor decrease in rotation preoperatively (Fig. 2d).
Regression analysis was performed to assess the influence of femoro-tibial rotation on patellar kinematics. In the healthy individuals, femoral rotation did not significantly influence patellar shift, patellar tilt or the contact area. Femoral rotation significantly influenced patellar shift preoperatively at 90° of flexion with and without isometric muscle contractions (Table 1). Postoperatively, no significant effects were observed.
Discussion
The most important finding of the present study was that most aspects of patella-femoral and femoro-tibial joint kinematics could be improved by LRR in carefully selected patients with isolated unilateral LRT.
In the present study, an initial medialization of the patella from a more lateral position in full extension was followed by a subsequent increase in lateral patellar shift during knee flexion in the healthy control group. Similar results for healthy individuals were reported by previous studies [4, 20, 30]. The underlying mechanism is thought to be a medialization and engagement of the patella into the femoral trochlear groove, as the main static stabiliser, during early and mid-flexion. During higher degrees of flexion the passive stabilising function of the lateral retinaculum gains in importance and provokes a lateralisation of the patella [1]. Consequently, isolated LRT may only lead to an exuberant lateralisation of the patella during higher degrees of knee flexion. Confirming this hypothesis, the present study demonstrated an increased lateral patellar shift at 90° flexion in the patient group, which could be significantly reduced to values similar to those measured in the control group by LRR [24]. Furthermore, comparable values of lateral translation of the patella in full extension and at 30° knee flexion pre- and postoperatively underline the insufficiency of LRR to improve patellar shift at lower degrees of knee flexion.
Similar results were obtained for patella tilt angle with largest improvements from pre- to postoperatively at 90° of knee flexion. In contrast to other authors, however, relatively high patella tilt angles were identified in the present study [4, 14, 28]. On the other hand, in a systematic review, including only studies with CT- or MRI-based analysis techniques of patellar kinematics, Hochreiter et al. demonstrated a variation of the patella tilt angle from 0.7 ± 5.0° to 17.1 ± 4.3° in healthy individuals in full extension and 10° of flexion, respectively [12]. Besides differences in study cohorts, a lack of standardised imaging and measurement protocols was discussed as one of the main reasons for the highly variable results. In this context, several authors emphasized on the importance of 3D imaging techniques to consistently and precisely obtain landmarks, image plane location and orientation as several studies showed less accurate results for measurements on 2D images [11, 35]. Studies by Sebro et al., Mehl et al. and van Haver et al. are perfectly in line with our methods for healthy individuals [19, 31, 33]. Besides comparable measurement techniques Sebro et al. and van Haver et al. also presented good to excellent intraclass correlation coefficients (ICC) for patella tilt angle [31, 33].
Isometric muscular activity had a negligible effect on patellar shift and minor effect on patellar tilt angle in either group in the present study. Similar results were reported by Dupuy et al., who found a decrease in the lateral patella angle by 3% under load [2]. Moreover, a slight decrease in patellar tilt under muscular activity was also confirmed by Lorenz et al. [18]. Confirming these results, Lin et al. hypothesized that the relatively posterior patellar insertion of the vastus medialis oblique muscle (VMO) pulls the patella onto the femur during contraction leading to more rotational rather than translational displacement [17]. However, only flexion angles from 0° to 30° were investigated in their study. In higher degrees of knee flexion, the patella engages into the trochlea as the main static stabiliser. In individuals with a physiological anatomy of the femoral trochlea, the static stabilising function largely outweighs the impacts of the VMO [25]. This effect could be confirmed by Senavongse and Amis, as they identified a significantly larger loss of resistance to a lateral patella displacement by flattening of the lateral trochlea than by relaxation of the VMO [32]. Considering the diagnosis of isolated LRT without patellar instability or trochlea dysplasia in the present study, the aforementioned aspects could be confirmed.
Patello-femoral contact area significantly increased after arthroscopic lateral release in the present study. However, despite the improvement of patella tracking, complete restoration to physiological alignment did not occur. The present results are in line with those of a variety of other studies, even though comparism of the actual values to those in the other studies is limited due to the use of different examination techniques [22, 30, 34]. Isometric muscle contractions revealed slightly larger patellofemoral contact areas than did the absence of muscular activity, confirming trends reported in previously published studies, although Gold et al. reported considerably larger contact areas [6]. This inconsistency is probably due to Gold et al. including only male patients, who have clearly larger patello-femoral contact areas [6].
In healthy individuals, external femoral rotation during knee flexion corresponding to a posterior translation of the lateral condyle was found to occur from 30° to 90° of knee flexion in the present study. In line with these results, Hill et al. observed 15° of external femoral rotation from 60° to 110° of knee flexion whereas only 1° of external rotation occurred from 0° to 60° [8]. Similar data was presented in a recent meta-analysis by Galvin et al. [5]. Femoro-tibial rotation, in turn, has been proven to significantly influence patello-femoral kinematics [15, 16, 29]. In this context, Eckhoff et al. noted an increased external rotation of the tibia, corresponding to an internal rotation of the femur, in patients with anterior knee pain [3]. Confirming their results, larger angles of internal femoral rotation were preoperatively identified at 0° and 30° of knee flexion in the patient group compared to the control group. Besides other factors, these altered femoro-tibial kinematics may explain increased patella tilt angles and smaller patello-femoral contact areas in the patient group potentially accounting for characteristic anterior knee pain during specific activities like descending stairs, squatting, jumping, or running. Postoperatively, a significant reduction of the pathologically increased internal femoral rotation at 30° of knee flexion was observed. These results are consistent with those of previously published kinematic studies [8, 13, 26]. However, despite there being a significant reduction at 30° postoperatively in unloaded conditions, internal femoral rotation could not be completely restored to values measured in the healthy control group.
Isometric muscle contractions led to an increase in external femoral rotation in the patient and control groups. These results are in line with those of a meta-analysis regarding kinematic profiles in healthy knee joints in vivo under loaded conditions [5]. Similar results were found in an in vitro study by Li et al. with isolated quadriceps loading, specifically in extension, 30° and 60° [16]. Interestingly, in contrast to unloaded conditions, pathologically increased femoral internal rotation was not decreased by isometric quadriceps activity at 30° of knee flexion postoperatively, which is potentially attributed to a decreased lateral soft tissue tension due to the surgical release. This finding, in turn, may potentially explain persistent anterior knee pain in some patients despite improved patello-femoral kinematics.
However, several limitations of the present study have to be noted. First, LRT is not clearly defined but a diagnosis of exclusion. This can potentially lead to inclusion of patients with heterogenous patello-femoral pathologies which may influence the results. Second, patients with isolated LRT only represent a very small group within patients with anterior knee pain. Thus, the present results can only be very cautiously transferred to different patello-femoral conditions. Third, the present study was not performed as matched pair analysis. Considering the different gender ratio within the healthy individuals and the patient group, the comparison of absolute values has to be interpreted carefully. Fourth, in this study, the patients were examined only in a lying position without any axial loads, such as those incurred under physiological conditions, limiting further implications. Fifth, dynamic parameters could not be assessed by the techniques applied in this study due to insufficient quality of the data set acquired during dynamic MR techniques. Sixth, the acquisition time for a complete MR data set is approximately 4 min, and it is difficult for patients with patello-femoral pain to consistently hold isometric muscle contractions during the whole examination period. Moreover, the knee has to remain completely still for the duration of the examination to prevent artefacts.
Conclusion
Patello-femoral and femoro-tibial joint kinematics could be improved, making LRR a viable surgical option in carefully selected patients with isolated LRT. However, pathologically increased femoral internal rotation during early knee flexion remained unaffected by LRR and thus potentially accounts for persistent pain.
Abbreviations
- CT:
-
Computed tomography
- LRR:
-
Lateral retinacular release
- LRT:
-
Lateral retinacular tightness
- MRI:
-
Magnetic resonance imaging
- ROM:
-
Range of motion
- VLO:
-
Vastus lateralis oblique muscle
- VMO:
-
Vastus medialis oblique muscle
References
Cancienne JM, Christian DR, Redondo ML, Huddleston HP, Shewman EF, Farr J et al (2019) The biomechanical effects of limited lateral retinacular and capsular release on lateral patellar translation at various flexion angles in cadaveric specimens. Arthrosc Sports Med Rehabil 1:e137–e144
Dupuy DE, Hangen DH, Zachazewski JE, Boland AL, Palmer W (1997) Kinematic CT of the patellofemoral joint. AJR Am J Roentgenol 169:211–215
Eckhoff DG, Dwyer TF, Bach JM, Spitzer VM, Reinig KD (2001) Three-dimensional morphology of the distal part of the femur viewed in virtual reality. J Bone Joint Surg Am 83-A(Suppl 2):43–50
Esfandiarpour F, Lebrun CM, Dhillon S, Boulanger P (2018) In-vivo patellar tracking in individuals with patellofemoral pain and healthy individuals. J Orthop Res. https://doi.org/10.1002/jor.23887
Galvin CR, Perriman DM, Newman PM, Lynch JT, Smith PN, Scarvell JM (2018) Squatting, lunging and kneeling provided similar kinematic profiles in healthy knees-A systematic review and meta-analysis of the literature on deep knee flexion kinematics. Knee 25:514–530
Gold GE, Besier TF, Draper CE, Asakawa DS, Delp SL, Beaupre GS (2004) Weight-bearing MRI of patellofemoral joint cartilage contact area. J MagnReson Imaging 20:526–530
Heegaard JH, Leyvraz PF, Hovey CB (2001) A computer model to simulate patellar biomechanics following total knee replacement: the effects of femoral component alignment. ClinBiomech (Bristol, Avon) 16:415–423
Hill PF, Vedi V, Williams A, Iwaki H, Pinskerova V, Freeman MA (2000) Tibiofemoral movement 2: the loaded and unloaded living knee studied by MRI. J Bone Joint Surg Br 82:1196–1198
Hinckel BB, Yanke AB, Lattermann C (2019) When to add lateral soft tissue balancing? Sports Med Arthrosc Rev 27:e25–e31
Hinterwimmer S, Gotthardt M, von Eisenhart-Rothe R, Sauerland S, Siebert M, Vogl T et al (2005) In vivo contact areas of the knee in patients with patellar subluxation. J Biomech 38:2095–2101
Hirschmann MT, Konala P, Amsler F, Iranpour F, Friederich NF, Cobb JP (2011) The position and orientation of total knee replacement components: a comparison of conventional radiographs, transverse 2D-CT slices and 3D-CT reconstruction. J Bone Joint Surg Br 93:629–633
Hochreiter B, Hess S, Moser L, Hirschmann MT, Amsler F, Behrend H (2020) Healthy knees have a highly variable patellofemoral alignment: a systematic review. Knee Surg Sports TraumatolArthrosc 28:398–406
Iwaki H, Pinskerova V, Freeman MA (2000) Tibiofemoral movement 1: the shapes and relative movements of the femur and tibia in the unloaded cadaver knee. J Bone Joint Surg Br 82:1189–1195
Kim TH, Sobti A, Lee SH, Lee JS, Oh KJ (2014) The effects of weight-bearing conditions on patellofemoral indices in individuals without and with patellofemoral pain syndrome. Skeletal Radiol 43:157–164
Lee TQ, Morris G, Csintalan RP (2003) The influence of tibial and femoral rotation on patellofemoral contact area and pressure. J Orthop Sports PhysTher 33:686–693
Li G, DeFrate LE, Zayontz S, Park SE, Gill TJ (2004) The effect of tibiofemoral joint kinematics on patellofemoral contact pressures under simulated muscle loads. J Orthop Res 22:801–806
Lin YF, Lin JJ, Jan MH, Wei TC, Shih HY, Cheng CK (2008) Role of the vastus medialis obliquus in repositioning the patella: a dynamic computed tomography study. Am J Sports Med 36:741–746
Lorenz A, Bobrowitsch E, Wunschel M, Walter C, Wulker N, Leichtle UG (2015) Robot-aided in vitro measurement of patellar stability with consideration to the influence of muscle loading. Biomed Eng Online 14:70
Mehl J, Feucht MJ, Bode G, Dovi-Akue D, Sudkamp NP, Niemeyer P (2016) Association between patellar cartilage defects and patellofemoral geometry: a matched-pair MRI comparison of patients with and without isolated patellar cartilage defects. Knee Surg Sports TraumatolArthrosc 24:838–846
Mitrogiannis L, Barbouti A, Kanavaros P, Paraskevas G, Kitsouli A, Seretis A et al (2018) The contribution of the medial retinaculum as a restraining factor to the patella dislocation. ActaOrthopBelg 84:179–183
Most E, Li G, Sultan PG, Park SE, Rubash HE (2005) Kinematic analysis of conventional and high-flexion cruciate-retaining total knee arthroplasties: an in vitro investigation. J Arthroplasty 20:529–535
Osborne JD, Luczak SB, Acker WB, Bicos J (2019) Patellofemoral joint contact pressures: current concepts and use in patellar instability studies. Orthopedics 42:e172–e179
Ostermeier S, Buhrmester O, Hurschler C, Stukenborg-Colsman C (2005) Dynamic in vitro measurement of patellar movement after total knee arthroplasty: an in vitro study. BMC MusculoskeletDisord 6:30
Ostermeier S, Holst M, Hurschler C, Windhagen H, Stukenborg-Colsman C (2007) Dynamic measurement of patellofemoral kinematics and contact pressure after lateral retinacular release: an in vitro study. Knee Surg Sports TraumatolArthrosc 15:547–554
Philippot R, Boyer B, Testa R, Farizon F, Moyen B (2012) The role of the medial ligamentous structures on patellar tracking during knee flexion. Knee Surg Sports TraumatolArthrosc 20:331–336
Pinskerova V, Iwaki H, Freeman MA (2000) The shapes and relative movements of the femur and tibia at the knee. Orthopade 29(Suppl 1):S3-5
Powers CM, Chen YJ, Scher I, Lee TQ (2006) The influence of patellofemoral joint contact geometry on the modeling of three dimensional patellofemoral joint forces. J Biomech 39:2783–2791
Prakash J, Seon JK, Woo SH, Jin C, Song EK (2016) Comparison of radiological parameters between normal and patellar dislocation groups in Korean population: a rotational profile CT-based study. Knee SurgRelat Res 28:302–311
Salsich GB, Perman WH (2007) Patellofemoral joint contact area is influenced by tibiofemoral rotation alignment in individuals who have patellofemoral pain. J Orthop Sports PhysTher 37:521–528
Saper MG, Shneider DA (2014) Diagnosis and treatment of lateral patellar compression syndrome. Arthrosc Tech 3:e633-638
Sebro R, Weintraub S (2017) Knee morphometric and alignment measurements with MR imaging in young adults with central cartilage lesions of the patella and trochlea. DiagnInterv Imaging 98:429–440
Senavongse W, Amis AA (2005) The effects of articular, retinacular, or muscular deficiencies on patellofemoral joint stability: a biomechanical study in vitro. J Bone Joint Surg Br 87:577–582
Van Haver A, De Roo K, De Beule M, Van Cauter S, Audenaert E, Claessens T et al (2014) Semi-automated landmark-based 3D analysis reveals new morphometric characteristics in the trochlear dysplastic femur. Knee Surg Sports TraumatolArthrosc 22:2698–2708
von Eisenhart-Rothe R, Siebert M, Bringmann C, Vogl T, Englmeier KH, Graichen H (2004) A new in vivo technique for determination of 3D kinematics and contact areas of the patello-femoral and tibio-femoral joint. J Biomech 37:927–934
Yamada Y, Toritsuka Y, Nakamura N, Horibe S, Sugamoto K, Yoshikawa H et al (2017) Correlation of 3D shift and 3D tilt of the patella in patients with recurrent dislocation of the patella and healthy volunteers: an in vivo analysis based on 3-dimensional computer models. Am J Sports Med 45:3111–3118
Yao J, Yang B, Wang Y, Fan Y (2018) Patella tracking calculation from patellofemoral positions at finite angles of knee flexion. Med EngPhys 62:1–6
Funding
Open Access funding enabled and organized by Projekt DEAL.. No funding was received for the present study.
Author information
Authors and Affiliations
Contributions
FP: study design, data analysis, preparation of manuscript. UL: data analysis, preparation of manuscript. FWL: study design, data analysis. IL, AH: data acquisition, data analysis. SH: data acquisition, approval of manuscript. HG: study design, approval of manuscript. RE-R: study design, data acquisition, approval of manuscript.
Corresponding author
Ethics declarations
Conflict of interest
All authors declare that they have no competing interests.
Ethical approval
The present study was approved by the institutional ethics committee of the Goethe University Frankfurt (IRB number 118/02).
Informed consent
Informed consent was acquired from every subject prior to study inclusion.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pohlig, F., Lenze, U., Lenze, F.W. et al. Arthroscopic lateral retinacular release improves patello-femoral and femoro-tibial kinematics in patients with isolated lateral retinacular tightness. Knee Surg Sports Traumatol Arthrosc 30, 791–799 (2022). https://doi.org/10.1007/s00167-021-06434-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06434-w