Abstract
Purpose
The purpose of this study was to (1) report on the incidence of concurrent surgical pathology at the time of adolescent ACL reconstruction, (2) evaluate patient risk factors for concurrent pathology, and (3) measure the effect of BMI on operating room (OR) time.
Methods
A retrospective analysis of the NSQIP database for the years 2005–2017 was conducted. Nine-hundred and seventeen patients 18 years of age and younger who underwent ACL reconstruction (ACLR) were identified using CPT code 29888 and patients undergoing surgery for multi-ligamentous knee injuries were excluded. The mean patient age was 17.6 years (range 14–18, standard deviation 0.52) and consisted of 546 males (59.5%) and 371 females (40.5%). Logistic regression was used to assess the relationship between BMI and additional CPT codes for internal derangement at the time of surgery. Internal derangement was defined as any procedure for the treatment of a meniscal tear, chondral lesion, or loose body removal. Linear regression analysis was then performed to evaluate the effect of BMI on operative time.
Results
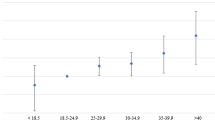
43.7% of patients undergoing ACLR required an associated procedure for internal derangement. Additionally, the risk of requiring additional procedures for internal derangement increased by 3.1% per BMI point. BMI was also predictive of operative time, independent of the number of additional procedures. Specifically, the operative time increased by nearly one minute for every point increase in BMI (58.0 s).
Conclusions
Adolescent patients with an elevated BMI were much more likely to require additional surgical procedures for internal derangement at the time of ACL reconstruction. Additionally, BMI was a significant predictor for longer operative times.
Level of Evidence
Level III.
Similar content being viewed by others
References
Agarwalla A, Gowd AK, Liu JN, Garcia GH, Bohl DD, Verma NN, Forsythe B (2019) Effect of operative time on short-term adverse events after isolated anterior cruciate ligament reconstruction. Orthop J Sports Med 7:2325967118825453
Anderson AF, Anderson CN (2015) Correlation of meniscal and articular cartilage injuries in children and adolescents with timing of anterior cruciate ligament reconstruction. Am J Sports Med 43:275–281
Beck NA, Lawrence JTR, Nordin JD, DeFor TA, Tompkins M (2017) ACL tears in school-aged children and adolescents over 20 years. Pediatrics 139:e20161877
Borchers JR, Kaeding CC, Pedroza AD, Huston LJ, Spindler KP, Wright RW, MOON Consortium and the MARS Group (2011) Intra-articular findings in primary and revision anterior cruciate ligament reconstruction surgery: a comparison of the MOON and MARS study groups. Am J Sports Med 39:1889–1893
DeFrancesco CJ, Storey EP, Shea KG, Kocher MS, Ganley TJ (2018) Challenges in the management of anterior cruciate ligament ruptures in skeletally immature patients. J Am Acad Orthop Surg 26:e50–e61
DiSilvestro KJ, Jauregui JJ, Glazier E, Cherkalin D, Bennett CH, Packer JD, Henn RF (2019) Outcomes of anterior cruciate ligament reconstruction in obese and overweight patients: a systematic review. Clin J Sport Med 29:257–261
Dodwell ER, Lamont LE, Green DW, Pan T-J, Marx RG, Lyman S (2014) 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am J Sports Med 42:675–680
Dumont GD, Hogue GD, Padalecki JR, Okoro N, Wilson PL (2012) Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears: relationship of treatment time and patient-specific factors. Am J Sports Med 40:2128–2133
Frank JS, Gambacorta PL (2013) Anterior cruciate ligament injuries in the skeletally immature athlete: diagnosis and management. J Am Acad Orthop Surg 21:78–87
Gadinsky NE, Manuel JB, Lyman S, Westrich GH (2012) Increased operating room time in patients with obesity during primary total knee arthroplasty: conflicts for scheduling. J Arthroplasty 27:1171–1176
Ghodadra N, Mall NA, Karas V, Grumet RC, Kirk S, McNickle AG, Garrido CP, Cole BJ, Bach BR (2013) Articular and meniscal pathology associated with primary anterior cruciate ligament reconstruction. J Knee Surg 26:185–193
Ichiba A, Kishimoto I (2009) Effects of articular cartilage and meniscus injuries at the time of surgery on osteoarthritic changes after anterior cruciate ligament reconstruction in patients under 40 years old. Arch Orthop Trauma Surg 129:409–415
Kadry B, Press CD, Alosh H, Opper IM, Orsini J, Popov IA, Brodsky JB, Macario A (2014) Obesity increases operating room times in patients undergoing primary hip arthroplasty: a retrospective cohort analysis. PeerJ 2:e530
Kay J, Memon M, Shah A, Yen Y-M, Samuelsson K, Peterson D, Simunovic N, Flageole H, Ayeni OR (2018) Earlier anterior cruciate ligament reconstruction is associated with a decreased risk of medial meniscal and articular cartilage damage in children and adolescents: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc 26:3738–3753
Khuri SF (2005) The NSQIP: a new frontier in surgery. Surgery 138:837–843
Kluczynski MA, Marzo JM, Bisson LJ (2013) Factors associated with meniscal tears and chondral lesions in patients undergoing anterior cruciate ligament reconstruction: a prospective study. Am J Sports Med 41:2759–2765
Larsen MW, Garrett WE, DeLee JC, Moorman CT (2006) Surgical management of anterior cruciate ligament injuries in patients with open physes. J Am Acad Orthop Surg 14:736–744
Macfarlane GJ, de Silva V, Jones GT (2011) The relationship between body mass index across the life course and knee pain in adulthood: results from the 1958 birth cohort study. Rheumatology (Oxford) 50:2251–2256
Manek NJ, Hart D, Spector TD, MacGregor AJ (2003) The association of body mass index and osteoarthritis of the knee joint: an examination of genetic and environmental influences. Arthr Rheumat 48:1024–1029
Munger AM, Gonsalves NR, Sarkisova N, Clarke E, VandenBerg CD, Pace JL (2019) Confirming the presence of unrecognized meniscal injuries on magnetic resonance imaging in pediatric and adolescent patients with anterior cruciate ligament tears. J Pediatr Orthop 39:e661–e667
Newman JT, Carry PM, Terhune EB, Spruiell MD, Heare A, Mayo M, Vidal AF (2015) Factors predictive of concomitant injuries among children and adolescents undergoing anterior cruciate ligament surgery. Am J Sports Med 43:282–288
Ogden CL, Carroll MD, Lawman HG, Fryar CD, Kruszon-Moran D, Kit BK, Flegal KM (2016) Trends in obesity prevalence among children and adolescents in the United States, 1988–1994 through 2013–2014. JAMA 315:2292–2299
Patel NM, Talathi NS, Bram JT, DeFrancesco CJ, Ganley TJ (2019) How does obesity impact pediatric anterior cruciate ligament reconstruction? Arthroscopy 35:130–135
Raphael IJ, Parmar M, Mehrganpour N, Sharkey PF, Parvizi J (2013) Obesity and operative time in primary total joint arthroplasty. J Knee Surg 26:95–99
Stanitski CL, Harvell JC, Fu F (1993) Observations on acute knee hemarthrosis in children and adolescents. J Pediatr Orthop 13:506–510
Tepolt FA, Feldman L, Kocher MS (2018) Trends in pediatric ACL reconstruction from the PHIS database. J Pediatr Orthop 38:e490–e494
Thein R, Hershkovich O, Gordon B, Burstein G, Tenenbaum S, Derazne E, Tzur D, Shamis A, Afek A, Kreiss Y (2017) The prevalence of cruciate ligament and meniscus knee injury in young adults and associations with gender, body mass index, and height a large cross-sectional study. J Knee Surg 30:565–570
Traven SA, Reeves RA, Xerogeanes JW, Slone HS (2019) Higher BMI predicts additional surgery at the time of ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 27:2552–2557
Vavken P, Tepolt FA, Kocher MS (2018) Concurrent meniscal and chondral injuries in pediatric and adolescent patients undergoing ACL reconstruction. J Pediatr Orthop 38:105–109
Wills AK, Black S, Cooper R, Coppack RJ, Hardy R, Martin KR, Cooper C, Kuh D (2012) Life course body mass index and risk of knee osteoarthritis at the age of 53 years: evidence from the 1946 British birth cohort study. Ann Rheum Dis 71:655–660
(2014, November 4) American College of Surgeons National Surgical Quality Improvement Program. User guide for the 2013 participant use data file. Retrieved from https://www.facs.org/quality-programs/acs-nsqip/participant-use
Funding
This research did not receive any funding from agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Sophia A. Traven MD, G. Jacob Wolf MD, J. Brett Goodloe MD, Russell A. Reeves MD, Shane K. Woolf, and Harris S. Slone MD declare that they have no conflict of interest.
Ethical approval
This study was a large database retrospective review, and for this type of study formal consent is not required. All aspects of this study, including the retrospective review of human surgical procedures, were in accordance with the ethical standards of the institutional and/or national research committee and the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Traven, S.A., Wolf, G.J., Goodloe, J.B. et al. Elevated BMI increases concurrent pathology and operative time in adolescent ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 29, 4182–4187 (2021). https://doi.org/10.1007/s00167-021-06432-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-021-06432-y