Abstract
Purpose
Despite public recognition, obesity is a growing epidemic affecting an estimated 34% of adults and 20% of children in the U.S. population. As such, the number of ACL reconstructions performed in this population is likely to increase. The goal of this study is to evaluate the risk that increasing BMI poses for additional surgery at the time of ACL reconstruction.
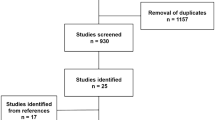
Methods
A retrospective analysis of the American College of Surgeons’ National Surgical Quality Improvement Program’s (ACS-NSQIP) database for the years 2005–2015 was conducted. Logistic regressions were used to assess the relationship between BMI and additional CPT codes for internal derangement at the time of ACL reconstruction. Internal derangement was defined as any CPT code for treatment of a meniscus tear, chondral lesion, or loose body removal. Surgeries for multi-ligamentous knee injuries were excluded.
Results
A total of 11,403 patients undergoing ACL reconstruction were identified. 41.9% of patients had an associated CPT code for internal derangement. As BMI increased, there was a corresponding increase in the odds of additional surgery. Specifically, for every 1.0 increase in BMI, the risk of additional surgery increased by 1.6% (p < 0.001). Compared to patients with a BMI of 18.5–24.9, those with a BMI 25–29.9 had an odds ratio (OR) of 1.112, BMI 30–34.9 had an OR of 1.137, BMI 35–39.9 had an OR of 1.249, and those ≥ 40 had an OR of 1.442 for additional surgery (p < 0.001).
Conclusions
This nationally-representative, population-based study demonstrates that patients with elevated BMI are much more likely to require additional surgery in the setting of primary ACL reconstruction. This risk correlates with increasing BMI. Surgeons should keep these risks in mind when evaluating and counseling patients for surgery in the setting of ACL reconstruction.
Level of evidence
Case–control study, Level III.

Similar content being viewed by others
References
Akizuki S, Shibakawa A, Takizawa T, Yamazaki I, Horiuchi H (2008) The long-term outcome of high tibial osteotomy. J Bone Jt Surg Br 90:592–596
Alvi HM, Mednick RE, Krishnan V, Kwasny MJ, Beal MD, Manning DW (2015) The effect of BMI on 30 day outcomes following total joint arthroplasty. J Arthroplasty 30:1113–1117
Amin A, Clayton R, Patton J, Gaston M, Cook R, Brenkel I (2006) Total knee replacement in morbidly obese patients. Results of a prospective, matched study. J Bone Jt Surg Br 88:1321–1326
Berend KR, Lombardi AV Jr, Mallory TH, Adams JB, Groseth KL (2005) Early failure of minimally invasive unicompartmental knee arthroplasty is associated with obesity. Clin Orthop Relat Res 440:60–66
Borchers JR, Kaeding CC, Pedroza AD, Huston LJ, Spindler KP, Wright RW, Consortium OBOTM, Group TM (2011) Intra-articular findings in primary and revision anterior cruciate ligament reconstruction surgery: a comparison of the MOON and MARS study groups. Am J Sports Med 39:1889–1893
Brambilla L, Pulici L, Carimati G, Quaglia A, Prospero E, Bait C, Morenghi E, Portinaro N, Denti M, Volpi P (2015) Prevalence of associated lesions in anterior cruciate ligament reconstruction: correlation with surgical timing and with patient age, sex, and body mass index. Am J Sports Med 43:2966–2973
Englund M, Lohmander LS (2004) Risk factors for symptomatic knee osteoarthritis fifteen to twenty-two years after meniscectomy. Arthritis Rheum 50:2811–2819
Erdil M, Bilsel K, Sungur M, Dikmen G, Tuncer N, Polat G, Elmadag NM, Tuncay I, Asik M (2013) Does obesity negatively affect the functional results of arthroscopic partial meniscectomy? A retrospective cohort study. Arthroscopy 29:232–237
Floerkemeier S, Staubli AE, Schroeter S, Goldhahn S, Lobenhoffer P (2013) Does obesity and nicotine abuse influence the outcome and complication rate after open-wedge high tibial osteotomy? A retrospective evaluation of five hundred and thirty three patients. Int Orthop 38:55–60
Ghodadra N, Mall NA, Karas V, Grumet RC, Kirk S, McNickle AG, Garrido CP, Cole BJ, Bach BR (2013) Articular and meniscal pathology associated with primary anterior cruciate ligament reconstruction. J Knee Surg 26:185–193
Haider AH, Bilimoria KY, Kibbe MR (2018) A checklist to elevate the science of surgical database research. JAMA Surg 153(6):505–507. https://doi.org/10.1001/jamasurg.2018.0628
Harrison MM, Morrell J, Hopman WM (2004) Influence of obesity on outcome after knee arthroscopy. Arthroscopy 20:691–695
Hui C, Salmon LJ, Kok A, Williams HA, Hockers N, van der Tempel WM, Chana R, Pinczewski LA (2011) Long-term survival of high tibial osteotomy for medial compartment osteoarthritis of the knee. Am J Sports Med 39:64–70
Ichiba A, Kishimoto I (2008) Effects of articular cartilage and meniscus injuries at the time of surgery on osteoarthritic changes after anterior cruciate ligament reconstruction in patients under 40 years old. Arch Orthop Trauma Surg 129:409–415
Jomha NM, Borton DC, Clingeleffer AJ, Pinczewski LA (1999) Long-term osteoarthritic changes in anterior cruciate ligament reconstructed knees. Clin Orthop Relat Res 358:188–193
Lawrence JTR, Argawal N, Ganley TJ (2011) Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: is there harm in delay of treatment? Am J Sports Med 39:2582–2587
Lementowski PW, Zelicof SB (2008) Obesity and osteoarthritis. Am J Orthop 37:148–151
Mall NA, Chalmers PN, Moric M, Tanaka MJ, Cole BJ, Bach BR Jr, Paletta GA Jr (2014) Incidence and trends of anterior cruciate ligament reconstruction in the United States. Am J Sports Med 42:2363–2370
Namba RS, Paxton L, Fithian DC, Stone ML (2005) Obesity and perioperative morbidity in total hip and total knee arthroplasty patients. J Arthroplasty 20:46–50
Noyes FR, Bassett RW, Grood ES, Butler DL (1980) Arthroscopy in acute traumatic hemarthrosis of the knee. Incidence of anterior cruciate tears and other injuries. J Bone Jt Surg Am 62:687–695
Paradowski PT, Englund M, Lohmander LS, Roos EM (2005) The effect of patient characteristics on variability in pain and function over two years in early knee osteoarthritis. Health Qual Life Outcomes 3:59
Salata MJ, Gibbs AE, Sekiya JK (2010) A systematic review of clinical outcomes in patients undergoing meniscectomy. Am J Sports Med 38:1907–1916
Sanders TL, Maradit Kremers H, Bryan AJ, Larson DR, Dahm DL, Levy BA, Stuart MJ, Krych AJ (2016) Incidence of anterior cruciate ligament tears and reconstruction. Am J Sports Med 44:1502–1507
Seon JK, Song EK, Park SJ (2006) Osteoarthritis after anterior cruciate ligament reconstruction using a patellar tendon autograft. Int Orthop 30:94–98
Sridhar MS, Jarrett CD, Xerogeanes JW, Labib SA (2012) Obesity and symptomatic osteoarthritis of the knee. J Bone Jt Surg Br 94:433–440
Thein R, Hershkovich O, Gordon B, Burstein G, Tenenbaum S, Derazne E, Tzur D, Shamis A, Afek A, Kreiss Y (2017) The prevalence of cruciate ligament and meniscus knee injury in young adults and associations with gender, body mass index, and height a large cross-sectional study. J Knee Surg 30:565–570
Vavken P, Tepolt FA, Kocher MS (2018) Concurrent meniscal and chondral injuries in pediatric and adolescent patients undergoing ACL reconstruction. J Pediatr Orthop 38:105–109
Wang Y, Beydoun MA, Liang L, Caballero B, Kumanyika SK (2008) Will all Americans become overweight or obese? Estimating the progression and cost of the US obesity epidemic. Obesity (Silver Spring) 16:2323–2330
Yoo JC, Ahn JH, Lee SH, Yoon YC (2009) Increasing incidence of medial meniscal tears in nonoperatively treated anterior cruciate ligament insufficiency patients documented by serial magnetic resonance imaging studies. Am J Sports Med 37:1478–1483
Øiestad BE, Engebretsen L, Storheim K, Risberg MA (2009) Knee osteoarthritis after anterior cruciate ligament injury: a systematic review. Am J Sports Med 37:1434–1443
Funding
No funding has been received for this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
John W. Xerogeanes MD has received royalties from Arthrex, Inc. Sophia A. Traven MD, Russell A. Reeves MD, and Harris S. Slone MD declares that they have no conflict of interest.
Ethical approval
The study was deemed “non-human subjects research” by the local medical ethical committee (Medical University of South Carolina, May 2, 2018).
Rights and permissions
About this article
Cite this article
Traven, S.A., Reeves, R.A., Xerogeanes, J.W. et al. Higher BMI predicts additional surgery at the time of ACL reconstruction. Knee Surg Sports Traumatol Arthrosc 27, 2552–2557 (2019). https://doi.org/10.1007/s00167-018-5267-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5267-x