Abstract
Purpose
It is not yet known if unicompartmental knee arthroplasty (UKA) patients are more likely to return to work sooner or have improved ability to work (i.e., workability) than total knee arthroplasty (TKA) patients. The following questions were addressed: patients were assessed to determine: (1) whether they returned to work sooner following UKA compared to TKA; (2) whether UKA patients had better WORQ function scores compared to TKA patients; and (3) if UKA patients have higher workability scores and greater satisfaction regarding workability than TKA patients.
Methods
A multicenter retrospective cohort study was performed that included patients at least 2 years after having undergone either UKA or TKA surgery and on the condition that patients had been in work in the 2 years prior to surgery. Time period between stopping work and returning to work was assessed; the WORQ scores (0 = worst–100 = best) and the Work Ability Index (WAI = 0–10) and reported satisfaction with work ability.
Results
UKA patients (n = 157, median 60 years, 51% male) were compared to TKA patients (n = 167, median 60 years, 49% male) (n.s.). Of the 157 UKA patients, 115 (73%) returned to work within 2 years compared to 121 (72%) of TKA patients (n.s.). More UKA patients return to work within 3 months (73% versus 48%) (p < 0.01). WORQ scores improved similarly in both groups. The WAI was also comparable between the groups. Dissatisfaction with workability was comparable (UKA 15% versus TKA 18% (n.s.).
Conclusion
TKA and UKA patients have similar WORQ, WAI, and satisfaction scores. However, in this study population, UKA patients to return to work after surgery significantly sooner than TKA patients, which improves their quality of life and allows them to participate actively in society. This information can help health care providers and patients weigh-up the pros and cons and choose the best treatment and timing for patients in the working population.
Level of evidence
III.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Knee arthroplasty is highly effective in treating pain caused by osteoarthritis of the knee [3]. However, recently, it was found that total knee arthroplasty (TKA) has a less positive impact on return to work than expected; in fact, one-third of patients do not return to work [14]. TKA does allow carrying out some knee-burdensome work activities, but a considerable percentage of TKA patients reported impaired ability to work and that they were dissatisfied with their level of ability to work. This is important as active work participation is an important factor in enhancing patients’ quality of life and it gives structure to day-to-day life [47].
In the 1970s, the medial unicompartmental knee arthroplasty (UKA) was introduced. The UKA is a less invasive procedure and an attractive alternative to TKA, because the natural biomechanics of the knee are largely preserved, whereas in (TKA), the anterior cruciate ligament is sacrificed and the biomechanics change substantially [20]. This might contribute to better postoperative clinical outcomes following UKA compared to TKA [29]. Recently, it was also reported that UKA yields better range of motion than TKA in patients less than 65 years of age [15]. Furthermore, less intraoperative complications such as blood transfusion, stroke, thromboembolism, and myocardial infarction have been reported for UKA [23]. UKA shows promising results in increasing speed of recovery and outpatient surgery programs with good satisfaction and high activity levels [46]. Therefore, UKA is expected to improve patients’ return to work and so reduce loss of productivity for society.
The absolute number of primary TKA currently being performed is increasing and expected to rise exponentially [3, 21, 32], largely due to the obesity epidemic. Because knee arthroplasty (KA) is being performed on younger people, while, at the same time, the age for retirement is predicted to rise in The Netherlands and other western countries, KA patients are more likely to be of working age at the time of surgery. Furthermore, the number of UKA’s being implanted is increasing at a higher rate than that of TKA [33].
If there is more detailed knowledge about the impact of UKA on work, patients and doctors can make more informed decisions about whether UKA or TKA is the most appropriate choice to increase the ability to participate at work. It is hypothesized that UKA patients return to work sooner have better WORQ scores and higher workability and satisfaction levels than TKA patients. Therefore, the questions addressed in this study are: (1) do patients return to work sooner following UKA compared to TKA; (2) do UKA patients have better WORQ function scores compared to TKA; and (3) do UKA patients have higher workability scores and satisfaction regarding workability than TKA patients?
Materials and methods
The materials and methods were the same as a previous study on TKA patients performed by the same research collaboration [13, 14]. The Medical Ethics Review Committee of the Amsterdam University Medical Center deemed that the Medical Research Involving Human Subjects Act (WMO) does not apply to the study and official approval was not required. (Part of return to work initiative, approval ID W13_019# 13.7.0037).
In short, a multicenter cross-sectional study was performed in which the survival of the Vanguard TKA (Zimmer Biomet Inc., Warsaw, Indiana, USA) was assessed, since start of use both for survival as well as return to work. This TKA study was performed in two large teaching hospitals in The Netherlands, the Amsterdam UMC—location Academic Medical Center (AMC) in Amsterdam and the Amphia Hospital in Breda. In this present cross-sectional study, in addition, data on UKA patients from the Amphia Hospital were collected. The AMC does not perform the UKA procedure. The Medical Ethics Review Committee again deemed that the Medical Research Involving Human Subjects Act (WMO) did not apply to this study and official approval was not required. All patients did provide informed consent. The newly gathered data from the UKA patients and were compared to the data from the above-mentioned study on TKA performed in the same centers in The Netherlands using the same methods [13, 14]. The goal of this study is to inform health professionals about work ability and return to work following UKA. As little is known about the topic, all TKA patients from the same centers, in the same period with the same data, are shown for the purpose of reference.
Patient population
As little is known on return to work in UKA patients, the goal was to include as many patients as possible in the study period to have a comparable group size as the TKA study (n = 167). All patients who received a primary Oxford UKA (Zimmer Biomet Inc., Warsaw, Indiana, USA), since the start of use in January 2003 until January 2012 that also had a follow-up of at least 2 years was approached. The indication for UKA was anteromedial osteoarthritis with intact cruciate and collateral ligaments. Similar as in the TKA study, they had to have work (paid or voluntary) within 2 years prior to surgery. For all patients, the following characteristics were collected: age at operation, sex, body mass index (BMI), diabetes, smoking status, admittance period, and ASA classification.
All patients who were still alive at follow-up were sent an invitation with a reply form to participate either via a web-based questionnaire or a paper-based questionnaire. Patients who were deceased were excluded. They could also respond by replying that they did not want to participate. Non-responders were contacted by phone at least twice after the first invitation. If no contact was established, the remaining non-responders were sent a paper questionnaire once more.
A link to a digital questionnaire was sent to the e-mail address supplied by the patient. Patients were given a personal code to ensure anonymity of their Internet questionnaires. The use of this code meant that no medical information could be traced back to the patient without the code file that was stored on a secure in-house server.
Paper-based questionnaires were sent to the patients’ home address. After completing the questionnaires, patients were asked to return them in the stamped addressed envelope provided.
Impact on work
First, all patients were assessed for baseline characteristics. As mentioned previously, only patients who reported that they had been in work during the 2 years prior to surgery were asked to fill out the full questionnaire. The survey contained three sections. The first section contained questions on the type of job, the time when patients stopped working pre-operatively, the time when patients returned to work post-operatively, changes in the kind of physically demanding tasks following surgery (less, the same, or more), changes in working hours (less, the same or more), the type of job performed 2 years after surgery, and if patients stopped working, what the reason was for stopping (for instance retirement, knee complaints or other health complaints).
If job descriptions were reported in enough detail, patients were categorized independently by two occupational health experts with respect to knee-burdensome activities into: light work, medium work, or heavy work. Both experts were experienced in performing systematic real-time task analyses in the workplace to assess the physical demands of work in different occupations. The classification by experts into light, medium, and heavy work was performed using the evidence-based exposure criteria for work relatedness of knee disorders of The Netherlands Center for Occupational Diseases [19]. If disagreement existed, this was resolved by discussion between experts. Examples of jobs classified as light work are a hairdresser or receptionist; examples of medium work are lorry drivers or household workers, and examples of heavy work are bricklayers or farmers.
The second part of the survey consisted of the previously validated Work, Osteoarthritis, or joint-Replacement Questionnaire (WORQ) [12]. The WORQ was tested for internal consistency by factor analysis resulting in two main factors, “Knee coordination”, and “Strenuous knee flexion” that both had high reliabilities, with Cronbach's α of, respectively, 0.90 and 0.85. Cronbach's α for the total score was 0.90. A test–retest reproducibility was performed for analyzing standard error of measurement (SEM agreement which was 3.43), reliability (ICC was 0.97), and smallest detectable change (SDC) in individuals (being 9.52) and groups (being 1.42). Finally, responsiveness was analyzed and reported by standardized response means (SRM was 0.70), and floor (less than 1%) and ceiling (8.8%) effects were deemed absent, as it was less than 15% and interpretability as minimal important change (MIC was 13) [12]. The survey contained questions to assess difficulty in performing knee-burdensome work activities at three points in time. This were: (T0) before the knee problems arose (T1) within 3 months before UKA or TKA and (T2) at 2 years after UKA or TKA. The WORQ score resulting from the sum of these difficulties ranges from 0 (worst score) to 100 (the best score, no difficulty at all) and showed the impact of UKA or TKA on knee-burdening activities in those patients who did return to work.
The third section of the questionnaire contained the single item: ‘current physical work ability’ from the Work Ability Index (WAI [41, 42]) on a scale from 0 ‘completely unable to work’ to 10 ‘work ability normal’. Patients were also presented with the statement—I am satisfied with my ability to work with respect to my TKA or UKA—and were asked to choose one of the following answers: strongly disagree, disagree, neither agree nor disagree, agree, and strongly agree. Their answer was scored, respectively, 0–4 on a Likert scale.
Statistical analysis
Standard descriptive statistics were used to describe demographic data and baseline characteristics. For normally distributed variables, unpaired t tests were used to compare the UKA and TKA groups. Mann–Whitney tests were used for continuous non-normally distributed variables and Chi-square tests for dichotomous variables to test for differences between TKA and UKA patients at baseline. The effectiveness of UKA in reducing patients’ difficulty in performing specific knee-burdensome activities was evaluated. The results are given in percentage of score improvement between 3 months before the UKA (T1) and 2 years after UKA (T2) and sorted from most improvement to least. The difference in scores between T1 and T2 was tested non-parametrically with paired testing. All analyses were done using SPSS 25.0 statistics software (IBM, Armonk, New York, USA). A P value < 0.05 was considered statistically significant.
Results
Of all, TKA patients from both hospitals resulted in 807 suitable to approach. The 764 patients who were still alive received an invitation to participate, 558 (73%) responded, 78 patients declined, and 480 filled out a questionnaire. This resulted in a group of 167 TKA patients with work within 2 years prior to surgery—median 60 years, range 40–84, 49%:51%, respectively, male:female. Of the 501 eligible UKA patients, 52 patients had since died, and 449 were approached of which 315 (70%) responded. Fifty-two patients declined and 263 filled out a questionnaire. This resulted in a group of 157 eligible patients with work within 2 years prior to surgery—median 60 years, range 40–83, 51%:49% male:female. Baseline characteristics and comparison between groups are given in Table 1.
From the 137 interpretable job types in the TKA group, 66 (48%) performed light work, 44 (32%) performed medium work, and 27 (20%) performed heavy work regarding knee-burdening work-related activities [14].
The job types performed by UKA patients before surgery that could be classified were as follows: n = 110 divided into 58 (53%) light work, 30 (27%) medium work, and 22 (20%) heavy work in the sense of knee-burdensome activities.
Stopping and returning to work
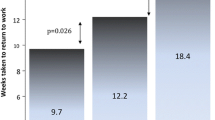
Of all 157 UKA patients, a total of 117 (75%) returned to work. Notably, of these 117 patients, 32 (27%) returned within 4 weeks and a further 85 (73%) within just 3 months (Fig. 1). Of all, 167 TKA patients 122 (72%) returned to work but only 8 (7%) returned within 4 weeks and only a further 59 (49%) within 3 months (Fig. 2). The % of patients who eventually returned to work after 2 years was almost the same for both groups. However, the UKA patients returned to work significantly sooner than TKA patients (p < 0.01).
Changes in physical burden at work
Of the 117 UKA patients who returned to work, 18 (15%) had a less, 58 (50%) an equally, and 17 (15%) a more physically demanding job after UKA. In addition, 15 (13%) of the patients worked fewer, 73 (62%) worked the same, and 3 (3%) worked more hours after UKA.
Of the 40 patients who did not return to work, six (15%) patients blamed their UKA (compared to 11% of TKA patients [14]), 21 (53%) patients had retired, 5 (13%) blamed other physical complaints, and 4 (10%) reported other reasons. Most patients returned to the same job (TKA 82% and UKA 75%).
Overall, in both groups, at 2 years after surgery, patients experienced significantly less difficulty performing activities compared to the 3 months prior to surgery (P ≤ 0.01). Median WORQ scores improved similarly between the two groups from 56 to 77 (+ 21) for UKA versus 54–71 (+ 17) for TKA patients, and post-operative scores did not differ significantly (n.s.). Improvement in scores for specific activities is given in Figs. 3 and 4, and differences were non-significant.
Patients’ opinion about their physical ability to work
The median WAI was 8 for UKA patients (IQR 5–8) and 7 for TKA (IQR 5–8) (n.s.). Of UKA patients, 12% were dissatisfied with their ability to work compared to 17% of TKA patients (n.s.).
Discussion
The most important outcome of this study is that, following surgery, UKA patients are able to return to work significantly sooner than TKA patients, even though both groups have similar WORQ, WAI, and satisfaction scores. This is important, as active work participation is an important factor in enhancing patients’ quality of life, mental well-being, and gives structure to day-to-day life [47]. A literature search was performed to find what other studies reported about ‘return to work’ after UKA. The search terms "return to work" AND ("Unicondylar Knee Replacement" OR "Unicompartmental Knee Arthroplasty" OR "Knee Arthroplasty, Unicondylar" OR "Knee Replacement, Unicompartmental" OR "Unicompartmental Knee Replacement") were used and the search produced 35 studies. Our study is the first large study to report on return to work in a large group of UKA patients in comparison with TKA patients. Furthermore, none of the studies we looked at described the impact of UKA on specific knee-burdening activities, so our results could not be compared to other studies. One recent study reported a mean return to work of 6.4 weeks (SD = 3.4) in patients following robotic-assisted UKA [10], and this seems similar to our results (27% at 1 month, 73% at 3 months). A further analysis that can be done is to compare results with previously reported outcomes of TKA and return to work. In Table 2, a summary is given of all studies reporting on patients returning to work after either UKA or TKA as well as the time of return to work, if reported. It seems that patients who return to work following surgery return sooner after UKA than after TKA.
The impact of surgery on the difficulty patients experienced performing knee-burdensome activities, was clear and we found that, also for UKA, surgery resulted in patients’ scoring a level comparable to the period before their knee complaints started. UKA can be considered to contribute to improving the ability to work. Known advantages of the UKA over the TKA are a lower risk of complications [23], better range of motion [15, 27], and better PROMs [24]. On the other hand, there is an ongoing debate about the use of UKA because of data registry that shows a lower survival rate of the implant after UKA compared to TKA [15, 17, 31]. It seems that for a definitive one-step treatment, TKA would be superior. The lower threshold for revision and the insufficient number of suitable surgeons might be an explanation for this for the difference in revision rates [24]. Apart from the physical and quality-of-life advantages of UKA over TKA, cost-effectiveness is also important in the light of an increasing financial burden on society, as the number of arthroplasties increases. Despite the poorer survival rate of a UKA device compared to a TKA, cost-effectiveness studies seem to favor UKA [37, 45]. These studies are limited to costs of the procedure and its complications and/or revisions; unfortunately, sick leave was not included. Where there is no preference to either TKA or UKA, and there is surgical expertise available to assess the indication and perform UKA, it seems that there is evidence for better outcome in the working population at least with respect to mid-term results and speedier return to work, despite the higher chance of revision surgery 10 year follow-up.
Recently, it was found that the combined loss of productivity plus medical costs for conservatively treated symptomatic knee osteoarthritis for those in paid employment in The Netherlands amounts to €871 per patient per month, with loss of productivity accounting for 83% and medical costs for 17% [8]. Returning to work sooner can potentially benefit not only patients of working age but also employers and, ultimately, society as a whole by reducing costs related to sick leave and quality of life. Thereby, the cost-effectiveness of UKA surgery could increase further from society’s perspective when compared to TKA, at least during working life and if there is a similar indication. Furthermore, patient expectation can be steered with respect to the results of this study.
TKA patients benefit least if their work requires mainly kneeling, crouching, and clambering. UKA patients benefit least if their work requires kneeling, crouching, and pushing or pulling. Kneeling and crouching improvement was similar for both TKA and UKA. The results for both procedures imply that patients whose work requires crouching or kneeling on the ground, for instance, plumbers, floor layers, and gardeners should be warned that knee replacement might relieve the pain, but will only marginally reduce difficulties y in performing these tasks. For TKA patients, it might be, because a TKA has a limited range of movement (ROM) compared to a normal knee. UKA patients tend to have better flexion, but do not score better on performing difficult tasks than TKA patients. In our previous report on the questionnaire, a clinically significant improvement was an improvement of at least 13 points on the WORQ questionnaire. Therefore, as an overall group, both TKA and UKA patients report a clinically relevant improvement of their WORQ scores. The patients who benefit most from knee replacement are those whose work involves operating a vehicle, or who have a job that involves periods of standing or walking on level ground. For these activities, the ROM is less important, whereas pain reduction is likely to play a more important role.
No difference was found with respect to WAI to describe physical work ability. One would expect UKA patients to have a better WAI, as recovery is sooner, and possibly, ROM is better. The fact that no difference was found coincides with the more reliable WORQ scores, which also did not differ significantly. There might be a trend towards overall slightly better scores, be it said not significant, for different aspects for the UKA group. As trends to superiority are found across different variables, the study might just be underpowered to find these differences. To the statement—I am satisfied with my ability to work with respect to my TKA or UKA—30 (17%) TKA patients stated that they were (strongly) dissatisfied compared to 19 (12%) UKA patients. These percentages seem higher than reported in the previous literature, where 8% of overall patients are dissatisfied with the outcome at 2–17 years [34]. It might be that with respect to the ability to work, patients are less satisfied with the result of TKA or UKA.
A limitation is the retrospective nature of reports by patients about their ‘return to work’. Hence, there is a potential for recall bias in the overall results. This is why categories were made with respect to the time interval for return to work instead of an exact amount in weeks or months. It is assumed that patients are able to assess work specific tasks at three different and distinct time points. As the same methods were used for both the TKA and UKA group, this is unlikely to influence comparability. In future research, the questionnaire should be given to patients pre-operatively and at regular follow-up moments to generate more precise results. The WORQ is validated for TKA patients, not yet specifically for UKA patients. However, as the construct is very much the same, it is assumed that the WORQ is equally valid for UKA patients, although the minimal clinical important change might differ between these two groups given their expectations pre-operatively. A validation study for the WORQ in UKA patients is currently being performed. Furthermore, there are similarities, but also differences in indication for TKA and UKA.
In the previous study, the average age of TKA patients was slightly younger than that of the general population of patients undergoing TKA [14]. This is probably due to the fact that the two involved centers are tertiary referral centers for advanced osteoarthritis in younger patients as well as severe post-traumatic deformities. Therefore, it would be good to repeat such a study in a more general primary population too.
In general, UKA patients have a more limited, anteromedial osteoarthritis and tend to be younger. Furthermore, the ACL must be intact. Surgery itself is less invasive and the wound and exposure are more limited leading to less blood loss. Rehabilitation time is generally shorter due to these differences. Therefore, it cannot be concluded based on this study that if all TKA patients would have undergone UKA surgery, they would have returned to work sooner. To answer such a question a randomised design would be needed, where patients with anteromedial osteoarthritis with an intact ACL would be allocated either to UKA or TKA surgery. The fact that UKA patients in this study return to work sooner is, therefore, multifactorial and not simply addressable to the type of prosthesis choice alone.
The patient group in The Netherlands was considered large and varied enough to give a representative picture of the impact of TKA and UKA on ‘return to work’. The exact same methods were used to collect and analyse patient data for both the TKA and UKA group to make sure collection bias was minimal. The period in which the procedures were performed were the same to reduce possible time-bias. To ensure that the results are adequate and interpretable, the validated WORQ questionnaire was used. The purpose of the WORQ was to obtain an adequate range to discover which of work-related activities remain difficult to perform and which benefit most from TKA. The WAI was introduced in 1997 [41, 42] and has been proven reliable [5] and the single item has a moderate predictive validity for return to physically demanding work [18].
It continues to be increasingly important for society that people are able to work longer. As stated before pension, funds suffer because of lower contributions from a decreasing work force, while the burden to pay out increases as a greater proportion of the population retire and pensioners live longer. As patients who undergo UKA return to work significantly sooner than TKA, in case of a working patient with a similar indication for both procedures, UKA should be chosen. This will save costs, both in loss of productivity as well as medical costs. It will be useful to find out more about differences in predictors for adequate ‘return to work’ and if there are differences between TKA and UKA in limitations that patients perceive in their work with respect to their knee function.
Conclusion
TKA and UKA patients have similar WORQ, WAI, and satisfaction scores. However, UKA patients return to work after surgery significantly sooner than TKA patients in this study population, which improves their quality of life and allows them to participate actively in society.
References
Bardgett M, Lally J, Malviya A, Deehan D (2016) Return to work after knee replacement: a qualitative study of patient experiences. BMJ Open 6:e007912
Belmont PJ Jr, Heida K, Keeney JA, Hamilton W, Burks R, Waterman BR (2015) Return to work and functional outcomes following primary total knee arthroplasty in US military servicemembers. J Arthroplasty 30:968–972
Carr AJ, Robertsson O, Graves S, Price AJ, Arden NK, Judge A et al (2012) Knee replacement. Lancet 379:1331–1340
Clyde CT, Goyal N, Matar WY, Witmer D, Restrepo C, Hozack WJ (2013) Workers' compensation patients after total joint arthroplasty: do they return to work? J Arthroplasty 28:883–887
de Zwart BCH, Frings-Dresen MHW, van Duivenbooden JC (2002) Test–retest reliability of the Work Ability Index questionnaire. Occup Med 52:177–181
Foote JA, Smith HK, Jonas SC, Greenwood R, Weale AE (2010) Return to work following knee arthroplasty. Knee 17:19–22
Glebus GP, Feather TW, Hsu JR, Gerlinger TL (2013) Return to duty and deployment after major joint arthroplasty. J Arthroplasty 28:1270–1273
Hermans J, Koopmanschap MA, Bierma-Zeinstra SM, van Linge JH, Verhaar JA, Reijman M et al (2012) Productivity costs and medical costs among working patients with knee osteoarthritis. Arthritis Care Res (Hoboken) 64:853–861
Husted H, Troelsen A, Otte KS, Kristensen BB, Holm G, Kehlet H (2011) Fast-track surgery for bilateral total knee replacement. J Bone Joint Surg Br 93:351–356
Jinnah AH, Augart MA, Lara DL, Jinnah RH, Poehling GG, Gwam CU et al (2018) Decreased time to return to work using robotic-assisted unicompartmental knee arthroplasty compared to conventional techniques. Surg Technol Int 32:279–283
Jorn LP, Johnsson R, Toksvig-Larsen S (1999) Patient satisfaction, function and return to work after knee arthroplasty. Acta Orthop Scand 70:343–347
Kievit AJ, Kuijer PPFM, Kievit RA, Sierevelt IN, Blankevoort L, Frings-Dresen MHW (2014) A reliable, valid and responsive questionnaire to score the impact of knee complaints on work following total knee arthroplasty: the WORQ. J Arthroplasty 29:1169–1175
Kievit AJ, Schafroth MU, Blankevoort L, Sierevelt IN, van Dijk CN, van Geenen RC (2014) Early experience with the vanguard complete total knee system: 2–7 years of follow-up and risk factors for revision. J Arthroplasty 29:348–354
Kievit AJ, van Geenen RCI, Kuijer PPFM, Pahlplatz TMJ, Blankevoort L, Schafroth MU (2014) Total knee arthroplasty and the unforeseen impact on return to work: a cross-sectional multicenter survey. J Arthroplasty 29:1163–1168
Kleeblad LJ, van der List JP, Zuiderbaan HA, Pearle AD (2018) Larger range of motion and increased return to activity, but higher revision rates following unicompartmental versus total knee arthroplasty in patients under 65: a systematic review. Knee Surg Sports Traumatol Arthrosc 26:1811–1822
Kleim BD, Malviya A, Rushton S, Bardgett M, Deehan DJ (2015) Understanding the patient-reported factors determining time taken to return to work after hip and knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 23:3646–3652
Koskinen E, Eskelinen A, Paavolainen P, Pulkkinen P, Remes V (2008) Comparison of survival and cost-effectiveness between unicondylar arthroplasty and total knee arthroplasty in patients with primary osteoarthritis: a follow-up study of 50,493 knee replacements from the Finnish Arthroplasty Register. Acta Orthop 79:499–507
Kuijer PP, Gouttebarge V, Wind H, van Duivenbooden C, Sluiter JK, Frings-Dresen MH (2012) Prognostic value of self-reported work ability and performance-based lifting tests for sustainable return to work among construction workers. Scand J Work Environ Health 38:600–603
Kuijer PP, Van der Molen HF, Frings-Dresen MH (2012) Evidence-based exposure criteria for work-related musculoskeletal disorders as a tool to assess physical job demands. Work 41(Suppl 1):3795–3797
Laurencin CT, Zelicof SB, Scott RD, Ewald FC (1991) Unicompartmental versus total knee arthroplasty in the same patient. A comparative study. Clin Orthop Relat Res 273:151–156
Lee K, Goodman SB (2008) Current state and future of joint replacements in the hip and knee. Expert Rev Med Dev 5:383–393
Leichtenberg CS, Tilbury C, Kuijer P, Verdegaal S, Wolterbeek R, Nelissen R et al (2016) Determinants of return to work 12 months after total hip and knee arthroplasty. Ann R Coll Surg Engl 98:387–395
Liddle AD, Judge A, Pandit H, Murray DW (2014) Adverse outcomes after total and unicompartmental knee replacement in 101,330 matched patients: a study of data from the National Joint Registry for England and Wales. Lancet 384:1437–1445
Liddle AD, Pandit H, Judge A, Murray DW (2015) Patient-reported outcomes after total and unicompartmental knee arthroplasty: a study of 14,076 matched patients from the National Joint Registry for England and Wales. Bone Joint J 97:793–801
Lombardi AV Jr, Berend KR, Walter CA, Aziz-Jacobo J, Cheney NA (2009) Is recovery faster for mobile-bearing unicompartmental than total knee arthroplasty? Clin Orthop Relat Res 467:1450–1457
Lombardi AV Jr, Nunley RM, Berend KR, Ruh EL, Clohisy JC, Hamilton WG et al (2014) Do patients return to work after total knee arthroplasty? Clin Orthop Relat Res 472:138–146
Longo UG, Loppini M, Trovato U, Rizzello G, Maffulli N, Denaro V (2015) No difference between unicompartmental versus total knee arthroplasty for the management of medial osteoarthtritis of the knee in the same patient: a systematic review and pooling data analysis. Br Med Bull 114:65–73
Lyall H, Ireland J, El-Zebdeh MY (2009) The effect of total knee replacement on employment in patients under 60 years of age. Ann R Coll Surg Engl 91:410–413
Lyons MC, MacDonald SJ, Somerville LE, Naudie DD, McCalden RW (2012) Unicompartmental versus total knee arthroplasty database analysis: is there a winner? Clin Orthop Relat Res 470:84–90
Nielsen MB, Kristensen PW, Lamm M, Schroder HM (1999) Knee alloplasty and working ability The significance of knee alloplasty for working ability of patients who were working prior to surgery. Ugeskr Laeger 161:2666–2669
Niinimaki T, Eskelinen A, Makela K, Ohtonen P, Puhto AP, Remes V (2014) Unicompartmental knee arthroplasty survivorship is lower than TKA survivorship: a 27-year Finnish registry study. Clin Orthop Relat Res 472:1496–1501
Otten R, van Roermund PM, Picavet HS (2010) Trends in the number of knee and hip arthroplasties: considerably more knee and hip prostheses due to osteoarthritis in 2030. Ned Tijdschr Geneeskd 154:A1534
Riddle DL, Jiranek WA, McGlynn FJ (2008) Yearly incidence of unicompartmental knee arthroplasty in the United States. J Arthroplasty 23:408–412
Robertsson O, Dunbar M, Pehrsson T, Knutson K, Lidgren L (2000) Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand 71:262–267
Sankar A, Davis AM, Palaganas MP, Beaton DE, Badley EM, Gignac MA (2013) Return to work and workplace activity limitations following total hip or knee replacement. Osteoarthr Cartil 21:1485–1493
Scott CEH, Turnbull GS, MacDonald D, Breusch SJ (2017) Activity levels and return to work following total knee arthroplasty in patients under 65 years of age. Bone Joint J 99:1037–1046
Shankar S, Tetreault MW, Jegier BJ, Andersson GB, Della Valle CJ (2016) A cost comparison of unicompartmental and total knee arthroplasty. Knee 23:1016–1019
Stigmar K, Dahlberg LE, Zhou C, Jacobson Lidgren H, Petersson IF, Englund M (2017) Sick leave in Sweden before and after total joint replacement in hip and knee osteoarthritis patients. Acta Orthop 88:152–157
Styron JF, Barsoum WK, Smyth KA, Singer ME (2011) Preoperative predictors of returning to work following primary total knee arthroplasty. J Bone Joint Surg Am 93:2–10
Tilbury C, Leichtenberg CS, Tordoir RL, Holtslag MJ, Verdegaal SH, Kroon HM et al (2015) Return to work after total hip and knee arthroplasty: results from a clinical study. Rheumatol Int 35:2059–2067
Tuomi K (1997) Eleven-year follow-up of aging workers. Scand J Work Environ Health 23:1–71
Tuomi K, Ilmarinen J, Jahkola A, Katajarinne L, Tulkki A (1998) Work ability index, 2nd edn. Finnish Institute of Occupational Health, Helsinki
Walton NP, Jahromi I, Lewis PL, Dobson PJ, Angel KR, Campbell DG (2006) Patient-perceived outcomes and return to sport and work: TKA versus mini-incision unicompartmental knee arthroplasty. J Knee Surg 19:112–116
Weingarten S, Riedinger MS, Sandhu M, Bowers C, Ellrodt AG, Nunn C et al (1998) Can practice guidelines safely reduce hospital length of stay? Results from a multicenter interventional study. Am J Med 105:33–40
Willis-Owen CA, Brust K, Alsop H, Miraldo M, Cobb JP (2009) Unicondylar knee arthroplasty in the UK National Health Service: an analysis of candidacy, outcome and cost efficacy. Knee 16:473–478
Witjes S, Gouttebarge V, Kuijer PP, van Geenen RC, Poolman RW, Kerkhoffs GM (2016) Return to sports and physical activity after total and unicondylar knee arthroplasty: a systematic review and meta-analysis. Sports Med 46:269–292
Witjes S, van Geenen RC, Koenraadt KL, van der Hart CP, Blankevoort L, Kerkhoffs GM et al (2017) Expectations of younger patients concerning activities after knee arthroplasty: are we asking the right questions? Qual Life Res 26:403–417
Acknowledgements
We would like to thank P.A. Kievit-Tyson for her editing work on the manuscript. Furthermore, we would like to thank Jan Ophuis for his help in collecting the data.
Funding
Zimmer Biomet (Warsaw, Indiana) supplied the department of orthopedics of the (Amsterdam University Medical Center) with an unrestricted research Grant for the employment of a PhD student.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that there is no conflict of interest apart from the unrestricted funding as mentioned above.
Ethical approval
The Medical Ethics Review Committee of the AMC deemed that the Medical Research Involving Human Subjects Act (WMO) does not apply to the study and official approval was not required.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access The article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kievit, A.J., Kuijer, P.P.F.M., de Haan, L.J. et al. Patients return to work sooner after unicompartmental knee arthroplasty than after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 28, 2905–2916 (2020). https://doi.org/10.1007/s00167-019-05667-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05667-0