Abstract
Purpose
Progression of osteoarthritis over time is poorly understood. The aim of the current study was to establish a timeline of “cartilage survival rate” per subregion of the knee in relation to mechanical alignment of the lower extremity. The study hypothesized that there are differences in progression of osteoarthritis between varus, valgus and physiologic lower extremity alignment.
Methods
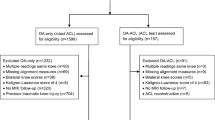
Based on hip-knee-ankle standing radiographs at baseline, 234 knees had physiologic (180° ± 3°, mean 179.7°), 158 knees had varus (< 177°; mean 174.5°) and 66 knees valgus (> 183°; mean 185.2°) alignment (consecutive knees of the OAI “Index Knee” group, n = 458; mean age 61.7; 264 females). The Osteoarthritis Initiative (OAI; a multi-center, longitudinal, prospective observational study of knee osteoarthritis [30] using MRIs) defines progressive OA as a mean decrease of cartilage thickness of 136 µm/year and a mean decrease of cartilage volume by 5% over 1 year (DESS sequences, MRI). A Kaplan–Meier curve was generated for osteoarthritis progression based on OAI criteria.
Results
Osteoarthritis progression based on volume decrease of 5% in varus knees occurred after 30.8 months (medial femoral condyle), after 37 months (medial tibia), after 42.9 months (lateral femoral condyle) and 43.4 months (lateral tibia), respectively. In a valgus alignment progression was detectable after 31.5 months (lateral tibia), after 36.2 months (lateral femoral condyle), after 40.4 months (medial femoral condyle) and 43.8 months (medial tibia), respectively. The physiological alignment shows a progression after 37.8 months (medial femoral condyle), after 41.6 months (lateral tibia), after 41.7 months (medial tibia) and after 43 months (lateral femoral condyle), respectively.
Conclusion
Based on data from the OAI, the rate and location (subregion) of osteoarthritis progression of the knee is strongly associated with lower extremity mechanical alignment.
Level of evidence
Level I (prognostic study).

Similar content being viewed by others
References
Altman RD, Brandt K, Hochberg M, Moskowitz R (1996) Design and conduct of clinical trials in patients with osteoarthritis: recommendations from a task force of the Osteoarthritis Research Society. Osteoarthr Cartil 4:217–243
Annual Report 2014. The Swedish Knee Arthroplasty Register. http://www.myknee.se/en/. Accessed 6 Jan 2019
Annual Report 2014. The Australian Orthopaedic Association National Joint Replacement Registry. https://aoanjrr.sahmri.com/annual-reports-2014. Accessed 6 Jan 2019
Beckwee D, Vaes P, Shahabpour M, Muyldermans R, Rommers N, Bautmans I (2015) The influence of joint loading on bone marrow lesions in the knee: a systematic review with meta-analysis. Am J Sports Med 43(12):3093–3107
Biswal S, Hastie T, Andriacchi TP, Bergman GA, Dillingham MF, Lang P (2002) Risk factors for progressive cartilage loss in the knee: a longitudinal magnetic resonance imaging study in forty-three patients. Arthritis Rheum 46(11):2884–2892
Cooke TD, Harrison L, Khan B, Scudamore A, Chaudhary MA (2002) Analysis of limb alignment in the pathogenesis of osteoarthritis: a comparison of Saudi Arabian and Canadian cases. Rheumatol Int 22(4):160–164
Cooke TD, Sled EA, Scudamore RA (2007) Frontal plane knee alignment: a call for standardized measurement. J Rheumatol 34(9):1796–1801
Dennis DA, Komistek RD, Mahfouz MR, Haas BD, Stiehl JB (2003) Multicenter determination of in vivo kinematics after total knee arthroplasty. Clin Orthop Relat Res (416):37–57
Dennis DA, Mahfouz MR, Komistek RD, Hoff W (2005) In vivo determination of normal and anterior cruciate ligament-deficient knee kinematics. J Biomech 38(2):241–253
Eckstein F, Ateshian G, Burgkart R, Burstein D, Cicuttini F, Dardzinski B, Gray M, Link TM, Majumdar S, Mosher T, Peterfy C, Totterman S, Waterton J, Winalski CS, Felson D (2006) Proposal for a nomenclature for magnetic resonance imaging based measures of articular cartilage in osteoarthritis. Osteoarthr Cartil 14(10):974–983
Eckstein F, Kwoh CK, Link TM, investigators OAI (2014) Imaging research results from the Osteoarthritis Initiative (OAI): a review and lessons learned 10 years after start of enrolment. Ann Rheum Dis 73(7):1289–1300
Eckstein F, Le Graverand MH (2015) Plain radiography or magnetic resonance imaging (MRI): which is better in assessing outcome in clinical trials of disease-modifying osteoarthritis drugs? Summary of a debate held at the World Congress of Osteoarthritis 2014. Semin Arthritis Rheum 45(3):251–256
Eckstein F, Maschek S, Wirt W et al (2009) One year change of knee cartilage morphology in the first release of participants from the Osteoarthritis Initiative progression subcohort—association with sex, body mass index, symptoms, and radiographic OA status. Ann Rheum Dis 68(5):674–679
Eckstein F, Nevitt M, Gimona A, Picha K, Lee JH, Davies RY, Dreher D, Benichou O, Le Graverand MP, Hudelmaier M, Maschek S, Wirth W, Osteoarthritis Initiative Investigators G (2011) Rates of change and sensitivity to change in cartilage morphology in healthy knees and in knees with mild, moderate, and end-stage radiographic osteoarthritis: results from 831 participants from the Osteoarthritis Initiative. Arthritis Care Res (Hoboken) 63(3):311–319
Eckstein F, Wirth W, Hudelmaier M, Stein V, Lengfelder V, Cahue S, Marshall M, Prasad P, Sharma L (2008) Patterns of femorotibial cartilage loss in knees with neutral, varus, and valgus alignment. Arthritis Rheum 59(11):1563–1570
Everhart JS, Abouljoud MM, Poland SG, Flanigan DC (2018) Medial compartment defects progress at a more rapid rate than lateral cartilage defects in older adults with minimal to moderate knee osteoarthritis (OA): data from the OA initiative. Knee Surg Sports Traumatol Arthrosc. https://doi.org/10.1007/s00167-018-5202-1
Felson DT, Niu J, Gross KD, Englund M, Sharma L, Cooke TD, Guermazi A, Roemer FW, Segal N, Goggins JM, Lewis CE, Eaton C, Nevitt MC (2013) Valgus malalignment is a risk factor for lateral knee osteoarthritis incidence and progression: findings from the Multicenter Osteoarthritis Study and the Osteoarthritis Initiative. Arthritis Rheum 65(2):355–362
Glyn-Jones S, Palmer AJR, Agricola R, Price AJ, Vincent TL, Weinans H, Carr AJ (2015) Osteoarthritis. Lancet 386(9991):376–387
Harman MK, Markovich GD, Banks SA, Hodge WA (1998) Wear patterns on tibial plateaus from varus and valgus osteoarthritic knees. Clin Orthop Relat Res 352:149–158
Hunter DJ, Zhang Y, Niu J, Goggins J, Amin S, LaValley MP, Guermazi A, Genant H, Gale D, Felson DT (2006) Increase in bone marrow lesions associated with cartilage loss: a longitudinal magnetic resonance imaging study of knee osteoarthritis. Arthritis Rheum 54(5):1529–1535
Khamaisy S, Nam D, Thein R, Rivkin G, Liebergall M, Pearle A (2014) Limb alignment, subluxation, and bone density relationship in the osteoarthritic varus knee. J Knee Surg 28(3):207–212
Khamaisy S, Zuiderbaan HA, Thein R, Nawabi DH, Joskowicz L, Pearle AD (2014) Coronal tibiofemoral subluxation: a new measurement method. Knee 21(6):1069–1071
LaValley MP, McAlindon TE, Chaisson CE, Levy D, Felson DT (2001) The validity of different definitions of radiographic worsening for longitudinal studies of knee osteoarthritis. J Clin Epidemiol 54(1):30–39
Lim YZ, Wang Y, Wluka AE, Davies-Tuck ML, Teichtahl A, Urquhart DM, Cicuttini FM (2013) Are biomechanical factors, meniscal pathology, and physical activity risk factors for bone marrow lesions at the knee? A systematic review. Semin Arthritis Rheum 43(2):187–194
March L, Smith EU, Hoy DG, Cross MJ, Sanchez-Riera L, Blyth F, Buchbinder R, Vos T, Woolf AD (2014) Burden of disability due to musculoskeletal (MSK) disorders. Best Pract Res Clin Rheumatol 28(3):353–366
Maschek S, Wirth W, Ladel C, Hellio Le Graverand MP, Eckstein F (2014) Rates and sensitivity of knee cartilage thickness loss in specific central reading radiographic strata from the Osteoarthritis Initiative. Osteoarthr Cartil 22(10):1550–1553
Moyer R, Wirth W, Duryea J, Eckstein F (2016) Anatomical alignment, but not goniometry, predicts femorotibial cartilage loss as well as mechanical alignment: data from the Osteoarthritis Initiative. Osteoarthr Cartil 24(2):254–261
Moyer R, Wirth W, Eckstein F (2017) Longitudinal changes in magnetic resonance imaging-based measures of femorotibial cartilage thickness as a function of alignment and obesity: data from the Osteoarthritis Initiative. Arthritis Care Res (Hoboken) 69(7):959–965
Mullaji AB, Marawar SV, Luthra M (2008) Tibial articular cartilage wear in varus osteoarthritic knees: correlation with anterior cruciate ligament integrity and severity of deformity. J Arthroplasty 23(1):128–135
Osteoarthritis-Initiative (2015) http://oai.epi-ucsf.org/datarelease/StudyOverview.asp. Accessed 12 Dec 2015
Osteoarthritis-Initiative (2015) https://oai.epi-ucsf.org/datarelease/ImageAssessments.asp. Accessed 12 Dec 2015
Rajgopal A, Noble PC, Vasdev A, Ismaily SK, Sawant A, Dahiya V (2015) Wear patterns in knee articular surfaces in varus deformity. J Arthroplasty 30(11):2012–2016
Raju PK, Kini SG, Verma A (2012) Wear patterns of tibiofemoral articulation in osteoarthritic knees: analysis and review of literature. Arch Orthop Trauma Surg 132(9):1267–1271
Sharma L, Chmiel JS, Almagor O, Felson D, Guermazi A, Roemer F, Lewis CE, Segal N, Torner J, Cooke TD, Hietpas J, Lynch J, Nevitt M (2013) The role of varus and valgus alignment in the initial development of knee cartilage damage by MRI: the MOST study. Ann Rheum Dis 72(2):235–240
Sharma L, Eckstein F, Song J, Guermazi A, Prasad P, Kapoor D, Cahue S, Marshall M, Hudelmaier M, Dunlop D (2008) Relationship of meniscal damage, meniscal extrusion, malalignment, and joint laxity to subsequent cartilage loss in osteoarthritic knees. Arthritis Rheum 58(6):1716–1726
Sharma L, Song J, Felson D, Cahue S, Shamiyeh E, Dunlop D (2001) The role of knee alignment in disease progression and functional decline in knee osteoarthritis. JAMA 286:188–195
Silverwood V, Blagojevic-Bucknall M, Jinks C, Jordan JL, Protheroe J, Jordan KP (2015) Current evidence on risk factors for knee osteoarthritis in older adults: a systematic review and meta-analysis. Osteoarthr Cartil 23(4):507–515
Weidow J, Pak J, Kärrholm J (2002) Different patterns of cartilage wear in medial and lateral gonarthrosis. Acta Orthop Scand 73:326–329
White SH, Ludkowski PF, Goodfellow JW (1991) Anteromedial osteoarthritis of the knee. J Bone Jt Surg Br 73:582–586
Wirth W, Duryea J, Hellio Le Graverand MP, John MR, Nevitt M, Buck RJ, Eckstein F, Group OAII (2013) Direct comparison of fixed flexion, radiography and MRI in knee osteoarthritis: responsiveness data from the Osteoarthritis Initiative. Osteoarthr Cartil 21(1):117–125
Wirth W, Eckstein F (2008) A technique for regional analysis of femorotibial cartilage thickness based on quantitative magnetic resonance imaging. IEEE Trans Med Imaging 27(6):737–744
Wirth W, Hellio Le Graverand MP, Wyman BT, Maschek S, Hudelmaier M, Hitzl W, Nevitt M, Eckstein F, Group OAII (2009) Regional analysis of femorotibial cartilage loss in a subsample from the Osteoarthritis Initiative progression subcohort. Osteoarthr Cartil 17(3):291–297
Wirth W, Larroque S, Davies RY, Nevitt M, Gimona A, Baribaud F, Lee JH, Benichou O, Wyman BT, Hudelmaier M, Maschek S, Eckstein F, Group OAII (2011) Comparison of 1-year vs 2-year change in regional cartilage thickness in osteoarthritis results from 346 participants from the Osteoarthritis Initiative. Osteoarthr Cartil 19(1):74–83
Wirth W, Nevitt M, Hellio Le Graverand MP, Benichou O, Dreher D, Davies RY, Lee J, Picha K, Gimona A, Maschek S, Hudelmaier M, Eckstein F, Investigators OAI (2010) Sensitivity to change of cartilage morphometry using coronal FLASH, sagittal DESS, and coronal MPR DESS protocols—comparative data from the Osteoarthritis Initiative (OAI). Osteoarthr Cartil 18(4):547–554
Wluka AE, Stuckey S, Snaddon J, Cicuttini FM (2002) The determinants of change in tibial cartilage volume in osteoarthritic knees. Arthritis Rheum 46(8):2065–2072
Funding
No funding was used to conducting this study. Outside the submitted work Dr. Boettner reports personal fees from Smith & Nephew, personal fees from Ortho Development Corporation, personal fees from Depuy and Dr. Faschingbauer reports personal fees from Deutsche Forschungsgemeinschaft (Research Fellowship, FA 1271/1-1, www.dfg.de).
Author information
Authors and Affiliations
Contributions
FM: planning/conception of the study, collection of data, analysis and interpretation, statistical analysis, writing and revising article; (orthopedic surgeon). KM: collection of data, analysis and interpretation, statistical analysis; (resident). SP, WW: collection of data, critical revision of the article; (resident, orthopedic surgeon). RH, BF: critical revision of the article, final approval of the article, overall responsibility; (surgeon in chief University of Ulm; orthopedic surgeon, attending at HSS).
Corresponding author
Ethics declarations
Conflict of interest
We certify that we have not signed any agreement with commercial interest related to this study, which would in any way limit publication of any and all data generated for the study or to delay publication for any reason. Dr. Boettner reports personal fees from Smith & Nephew, personal fees from Ortho Development Corporation, personal fees from Depuy, outside the submitted work. Dr. Faschingbauer reports personal fees from Deutsche Forschungsgemeinschaft (Research Fellowship, FA 1271/1-1, http://www.dfg.de), during the conduct of the study.
Ethical statement
The authors’ institutional review board approved this study.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Faschingbauer, M., Kasparek, M., Waldstein, W. et al. Cartilage survival of the knee strongly depends on malalignment: a survival analysis from the Osteoarthritis Initiative (OAI). Knee Surg Sports Traumatol Arthrosc 28, 1346–1355 (2020). https://doi.org/10.1007/s00167-019-05434-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-019-05434-1