Abstract
Purpose
To determine: (1) rates and risk factors for progression of lateral and medial full-thickness cartilage defect size in older adults without severe knee osteoarthritis (OA), and (2) whether risk factors for defect progression differ for knees with Kellgren–Lawrence OA grade 3 (moderate) OA versus grades 0–2 (none to mild) OA.
Methods
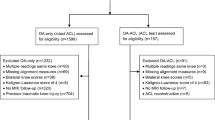
Three-hundred and eighty adults enrolled in the Osteoarthritis Initiative were included (43% male, mean age 63.0 SD 9.2 years). Ethical approval was obtained at all study sites prior to enrollment. All participants had full-thickness tibial or weight-bearing femoral condylar cartilage defects on baseline knee MRIs. Baseline OA grade was KL grade 3 in 71.3% and grades 0–2 in 21.7% of participants. Repeat MRIs were obtained at a minimum 2-year follow-up. Independent risk of progression in defect size due to demographic factors, knee alignment, OA grade, knee injury and surgery history, and baseline knee symptoms was determined by multivariate Cox proportional hazards and linear regression modeling.
Results
The average increase in defect size over 2 years for lateral defects was 0.18 cm2 (SD 0.60) and for medial defects was 0.49 cm2 (SD 1.09). Independent predictors of medical defect size progression were bipolar defects (beta 0.47 SE 0.08; p < 0.001), knee varus (per degree, beta 0.08 SE 0.03; p = 0.02) and increased weight (per kg, beta = 0.01 SE 0.004; p = 0.01). Independent predictors for lateral defect progression were larger baseline defect size (per 1.0 cm2, beta 0.14 SE 0.03; p < 0.001) and tibial sided defects (beta 0.12 SE 0.04) and degrees valgus (per degree, beta 0.04 SE 0.01; p = 0.001).
Conclusions
Medial compartment full-thickness defects progress at a more rapid rate than lateral defects in older adults with minimal to moderate OA. Medial defect progression was greatest for bipolar defects in heavier adults with varus knees. Lateral defect progression was greatest for large tibial-sided defects in adults with valgus knees.
Level of evidence
II.

Similar content being viewed by others
References
Akgun I, Unlu MC, Erdal OA, Ogut T, Erturk M, Ovali E et al (2015) Matrix-induced autologous mesenchymal stem cell implantation versus matrix-induced autologous chondrocyte implantation in the treatment of chondral defects of the knee: a 2-year randomized study. Arch Orthop Trauma Surg 135:251–263
Bae DK, Yoon KH, Song SJ (2006) Cartilage healing after microfracture in osteoarthritic knees. Arthroscopy 22:367–374
Bedson J, Croft PR (2008) The discordance between clinical and radiographic knee osteoarthritis: a systematic search and summary of the literature. BMC Musculoskelet Disord 9:116
Bekkers JE, Inklaar M, Saris DB (2009) Treatment selection in articular cartilage lesions of the knee: a systematic review. Am J Sports Med 37(Suppl 1):148S–155S
Bellamy N, Buchanan WW, Goldsmith CH, Campbell J, Stitt LW (1988) Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol 15:1833–1840
Biswal S, Hastie T, Andriacchi TP, Bergman GA, Dillingham MF, Lang P (2002) Risk factors for progressive cartilage loss in the knee: a longitudinal magnetic resonance imaging study in forty-three patients. Arthritis Rheum 46:2884–2892
Carnes J, Stannus O, Cicuttini F, Ding C, Jones G (2012) Knee cartilage defects in a sample of older adults: natural history, clinical significance and factors influencing change over 2.9 years. Osteoarthr Cartil 20:1541–1547
Cicuttini F, Ding C, Wluka A, Davis S, Ebeling PR, Jones G (2005) Association of cartilage defects with loss of knee cartilage in healthy, middle-age adults: a prospective study. Arthritis Rheum 52:2033–2039
Clavé A, Potel JF, Servien E, Neyret P, Dubrana F, Stindel E (2016) Third-generation autologous chondrocyte implantation versus mosaicplasty for knee cartilage injury: 2-year randomized trial. J Orthop Res 34:658–665
Conaghan PG, Felson DT (2004) Structural associations of osteoarthritis pain: lessons from magnetic resonance imaging. Novartis Found Symp 260:191–201 (discussion 201–195, 277–199)
Davies-Tuck ML, Wluka AE, Wang Y, Teichtahl AJ, Jones G, Ding C et al (2008) The natural history of cartilage defects in people with knee osteoarthritis. Osteoarthr Cartil 16:337–342
Ding C, Cicuttini F, Jones G (2007) Tibial subchondral bone size and knee cartilage defects: relevance to knee osteoarthritis. Osteoarthr Cartil 15:479–486
Ding C, Cicuttini F, Scott F, Cooley H, Boon C, Jones G (2006) Natural history of knee cartilage defects and factors affecting change. Arch Intern Med 166:651–658
Dong T, Chen W, Zhang F, Yin B, Tian Y, Zhang Y (2016) Radiographic measures of settlement phenomenon in patients with medial compartment knee osteoarthritis. Clin Rheumatol 35:1573–1578
Eckstein F, Kunz M, Schutzer M, Hudelmaier M, Jackson RD, Yu J et al (2007) Two year longitudinal change and test-retest-precision of knee cartilage morphology in a pilot study for the osteoarthritis initiative. Osteoarthr Cartil 15:1326–1332
Eckstein F, Maschek S, Wirth W, Hudelmaier M, Hitzl W, Wyman B et al (2009) One year change of knee cartilage morphology in the first release of participants from the osteoarthritis initiative progression subcohort: association with sex, body mass index, symptoms and radiographic osteoarthritis status. Ann Rheum Dis 68:674–679
Everhart JS, Siston RA, Flanigan DC (2014) Tibiofemoral subchondral surface ratio (SSR) is a predictor of osteoarthritis symptoms and radiographic progression: data from the Osteoarthritis Initiative (OAI). Osteoarthr Cartil 22:771–778
Gobbi A, Chaurasia S, Karnatzikos G, Nakamura N (2015) Matrix-induced autologous chondrocyte implantation versus multipotent stem cells for the treatment of large patellofemoral chondral lesions: a nonrandomized prospective trial. Cartilage 6:82–97
Hafezi-Nejad N, Zikria B, Eng J, Carrino JA, Demehri S (2015) Predictive value of semi-quantitative MRI-based scoring systems for future knee replacement: data from the osteoarthritis initiative. Skelet Radiol 44:1655–1662
Heir S, Nerhus TK, Røtterud JH, Løken S, Ekeland A, Engebretsen L et al (2010) Focal cartilage defects in the knee impair quality of life as much as severe osteoarthritis: a comparison of knee injury and osteoarthritis outcome score in 4 patient categories scheduled for knee surgery. Am J Sports Med 38:231–237
Jackson DW, Lalor PA, Aberman HM, Simon TM (2001) Spontaneous repair of full-thickness defects of articular cartilage in a goat model. A preliminary study. J Bone Jt Surg Am 83-A:53–64
Kellgren JH, Lawrence JS (1957) Radiological assessment of osteo-arthrosis. Ann Rheum Dis 16:494–502
Kon E, Mandelbaum B, Buda R, Filardo G, Delcogliano M, Timoncini A et al (2011) Platelet-rich plasma intra-articular injection versus hyaluronic acid viscosupplementation as treatments for cartilage pathology: from early degeneration to osteoarthritis. Arthroscopy 27:1490–1501
Kreuz PC, Erggelet C, Steinwachs MR, Krause SJ, Lahm A, Niemeyer P et al (2006) Is microfracture of chondral defects in the knee associated with different results in patients aged 40 years or younger? Arthroscopy 22:1180–1186
Lanyon P, O’Reilly S, Jones A, Doherty M (1998) Radiographic assessment of symptomatic knee osteoarthritis in the community: definitions and normal joint space. Ann Rheum Dis 57:595–601
Maldonado G, Greenland S (1993) Simulation study of confounder-selection strategies. Am J Epidemiol 138:923–936
Mall NA, Harris JD, Cole BJ (2015) Clinical evaluation and preoperative planning of articular cartilage lesions of the knee. J Am Acad Orthop Surg 23:633–640
Mickey RM, Greenland S (1989) The impact of confounder selection criteria on effect estimation. Am J Epidemiol 129:125–137
Moreland JR, Bassett LW, Hanker GJ (1987) Radiographic analysis of the axial alignment of the lower extremity. J Bone Jt Surg Am 69:745–749
Niemeyer P, Kostler W, Salzmann GM, Lenz P, Kreuz PC, Sudkamp NP (2010) Autologous chondrocyte implantation for treatment of focal cartilage defects in patients age 40 years and older: a matched-pair analysis with 2-year follow-up. Am J Sports Med 38:2410–2416
Patel KV, Guralnik JM, Dansie EJ, Turk DC (2013) Prevalence and impact of pain among older adults in the United States: findings from the 2011 national health and aging trends study. Pain 154:2649–2657
Pelletier JP, Raynauld JP, Berthiaume MJ, Abram F, Choquette D, Haraoui B et al (2007) Risk factors associated with the loss of cartilage volume on weight-bearing areas in knee osteoarthritis patients assessed by quantitative magnetic resonance imaging: a longitudinal study. Arthritis Res Ther 9:R74
Peterfy CG, Schneider E, Nevitt M (2008) The osteoarthritis initiative: report on the design rationale for the magnetic resonance imaging protocol for the knee. Osteoarthr Cartil 16:1433–1441
Roemer FW, Kwoh CK, Hannon MJ, Hunter DJ, Eckstein F, Wang Z et al (2015) Can structural joint damage measured with MR imaging be used to predict knee replacement in the following year? Radiology 274:810–820
Roos EM, Lohmander LS (2003) The knee injury and osteoarthritis outcome score (KOOS): from joint injury to osteoarthritis. Health Qual Life Outcomes 1:64
Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD (1998) Knee injury and osteoarthritis outcome score (KOOS)—development of a self-administered outcome measure. J Orthop Sports Phys Ther 28:88–96
Rosenberger RE, Gomoll AH, Bryant T, Minas T (2008) Repair of large chondral defects of the knee with autologous chondrocyte implantation in patients 45 years or older. Am J Sports Med 36:2336–2344
Wang Y, Ding C, Wluka AE, Davis S, Ebeling PR, Jones G et al (2006) Factors affecting progression of knee cartilage defects in normal subjects over 2 years. Rheumatology 45:79–84
Washburn RA, Smith KW, Jette AM, Janney CA (1993) The physical activity scale for the elderly (PASE): development and evaluation. J Clin Epidemiol 46:153–162
Wirth W, Hellio Le Graverand MP, Wyman BT, Maschek S, Hudelmaier M, Hitzl W et al (2009) Regional analysis of femorotibial cartilage loss in a subsample from the osteoarthritis initiative progression subcohort. Osteoarthr Cartil 17:291–297
Wluka AE, Wang Y, Davies-Tuck M, English DR, Giles GG, Cicuttini FM (2008) Bone marrow lesions predict progression of cartilage defects and loss of cartilage volume in healthy middle-aged adults without knee pain over 2 yrs. Rheumatology 47:1392–1396
Zhai G, Blizzard L, Srikanth V, Ding C, Cooley H, Cicuttini F et al (2006) Correlates of knee pain in older adults: Tasmanian older adult cohort study. Arthritis Rheum 55:264–271
Acknowledgements
The OAI is a public–private partnership comprised of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health, a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories; Novartis Pharmaceuticals Corporation; GlaxoSmithKline and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the National Institutes of Health. This manuscript was prepared using an OAI public use data set and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners.
Funding
David C. Flanigan reports consulting fees from Zimmer, DePuy Mitek, and Smith and Nephew.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
David C. Flanigan reports consulting fees from Zimmer, DePuy Mitek, and Smith and Nephew. For the remaining authors none were declared.
Ethical approval
The study protocol, amendments, and informed consent documentation were reviewed and approved by the Institutional Review Boards at all participating sites.
Rights and permissions
About this article
Cite this article
Everhart, J.S., Abouljoud, M.M., Poland, S.G. et al. Medial compartment defects progress at a more rapid rate than lateral cartilage defects in older adults with minimal to moderate knee osteoarthritis (OA): data from the OA initiative. Knee Surg Sports Traumatol Arthrosc 27, 2401–2409 (2019). https://doi.org/10.1007/s00167-018-5202-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00167-018-5202-1