Abstract
Purpose
Pulmonary vascular dysfunction is common during acute respiratory distress syndrome (ARDS), but there is controversy concerning prevalence and prognosis of cor pulmonale during protective ventilation for ARDS.
Methods
This was a prospective observational study in an academic medical intensive care unit in France. Two hundred and twenty-six consecutive patients with moderate to severe ARDS (Berlin definition) ventilated with plateau pressure limited at 30 cmH2O (mean PEEP of 8.8 ± 3.6 cmH2O) underwent transesophageal echocardiography (TEE) within the first 3 days after the diagnosis of ARDS. Cor pulmonale was defined as a dilated right ventricle associated with septal dyskinesia.
Results
Cor pulmonale was detected in 49 patients (prevalence of 22 %; 95 % confidence interval, 16–27 %). Multivariate logistic regression identified infectious causes of lung injury and higher driving pressures as independent factors associated with cor pulmonale. Patients with cor pulmonale exhibited a higher incidence of shock (need for vasoactive drug) at the time of TEE and were more often managed with prone positioning and/or nitric oxide as adjunctive therapy for severe hypoxemia during ARDS course. The 28-day mortality rate was significantly higher in the group with cor pulmonale (60 vs. 36 %, p < 0.01). Multivariate logistic regression identified McCabe and Jackson class, lung injury not related to pneumonia, aspiration, or sepsis, lactic acidosis, driving pressure, and cor pulmonale as independent risk factors for 28-day mortality.
Conclusion
Cor pulmonale occurrence is not negligible in ARDS patients ventilated with airway pressure limitation. Cor pulmonale was associated with sepsis and higher values of driving pressure and was an independent risk factor for 28-day mortality in our series.
Similar content being viewed by others
Introduction
Pulmonary vascular dysfunction in patients with acute respiratory distress syndrome (ARDS) was first described in 1977 by Zapol and Snider [1]. These authors found elevated pulmonary vascular resistance with a subsequent increase in right ventricle (RV) stroke-work index and progressive RV dysfunction resulting in cor pulmonale and refractory circulatory failure after several days on respiratory support [1]. Pulmonary vascular dysfunction during ARDS is secondary to several factors, including hypoxic or mediator-induced pulmonary vasoconstriction (by endothelins, thromboxane A2, or leucotrienes), mechanical compression by interstitial edema, and intravascular obstruction from endothelial swelling or thromboemboli (which are present in 95 % of patients with ARDS in postmortem studies [2]) [3]. Injurious mechanical ventilation with high inspiratory pressure and large tidal volumes may worsen pulmonary vascular dysfunction [4, 5]. Pulmonary hypertension and right ventricular dysfunction were frequent in ARDS patients (up to 70 %) and associated with a poorer outcome in many previous studies before the broad use of lower tidal volume ventilation [6–10]. There is controversy concerning their frequency and influence on outcome of patients in the era of protective ventilation for ARDS [11, 12].
The primary objective of this prospective study was to determine the prevalence and prognosis of cor pulmonale in ARDS patients with protective ventilation. This study has been presented in abstract form [13] and includes some patients previously described in a report focusing on patent foramen ovale during ARDS [14].
Patients and methods
Patients
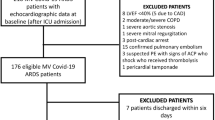
Patients who met the Berlin definition criteria for moderate to severe ARDS (respiratory failure within 1 week of a known clinical insult or new or worsening respiratory symptoms; with bilateral chest opacities not fully explained by effusions or lobar/lung collapse or nodule, and not fully explained by cardiac failure or fluid overload; and a PaO2/FiO2 ratio ≤200 mmHg with PEEP ≥5 cmH2O) [15] and who underwent transesophageal echocardiography (TEE) within the first 3 days after the diagnosis were included prospectively between June 2004 and October 2009 at the medical intensive care unit (ICU) of Henri Mondor Hospital (Creteil, France). Non-inclusion criteria were contraindications to TEE (esophageal disease or major uncontrolled bleeding), chronic pulmonary disease requiring long-term oxygen therapy or home mechanical ventilation, and chronic cor pulmonale. The study was approved by the institutional ethics committee of the French Society of Intensive Care (Société de Réanimation de Langue Française). Because we routinely use TEE to assess the circulatory status of mechanically ventilated patients with ARDS in our ICU, TEE was considered a component of standard care and patient’s consent was waived. Written and oral information about the study was given to the families. Severity of illness at admission was evaluated by the SAPS II score [16] while severity of underlying diseases was evaluated by the McCabe and Jackson score [17]. Shock was defined as the need for catecholamine infusion to maintain adequate arterial pressure [18]. Pneumonia, aspiration, and sepsis were diagnosed as previously described [18–20]. Follow-up for the study was at least 28 days and until hospital discharge.
Respiratory settings
Ventilation was in volume-assist control mode with a target tidal volume (V T) of 6 mL/kg (predicted body weight). In patients with persistent severe hypoxemia (PaO2/FiO2 <100 mmHg) despite a PEEP level as high as possible without exceeding a maximal inspiratory plateau pressure of 30 cmH2O [21], rescue interventions, namely, prone positioning and/or inhaled nitric oxide, were used at the discretion of the attending physician. If Pplat exceeded the maximal threshold, V T could be lowered until Pplat was less than 30 cmH2O; to counterbalance the effect of V T reduction on alveolar ventilation, the respiratory rate was increased to the highest rate that did not induce intrinsic PEEP [22]. Driving pressure was defined as the difference between Pplat and PEEP.
Echocardiography
Trained operators (competence in advanced critical care echocardiography) performed TEE according to a standard procedure [23] using a Sonos 5500, Envisor, or IE 33 system (Philips Ultrasound, Bothell, WA, USA) equipped with a multiplane 5-MHz transesophageal echocardiographic transducer (see Electronic Supplementary Material, ESM). Briefly, the following echocardiographic views were examined: long-axis M-mode view of the superior vena cava (SVC) to assess its collapsibility; four-chamber long-axis view to assess the end-diastolic right ventricle/left ventricle (RV/LV) area ratio and LV ejection fraction; short-axis view of the LV via the transgastric approach to evaluate the kinetics of the interventricular septum. LV systolic dysfunction was defined as LV ejection fraction less than 50 % [24]. Pulsed-wave Doppler aortic flow was obtained at the level of the aortic annulus and the velocity–time integral was automatically processed by tracing the envelope of aortic flow for cardiac index calculation. Cor pulmonale was defined as a dilated right ventricle (end-diastolic RV/LV area ratio >0.6) associated with septal dyskinesia on the short-axis view [25]. Septal dyskinesia was particularly sought during end-systole [23, 24], while analyzing images in slow motion. A longitudinal view of the fossa ovalis was obtained to evaluate patent foramen ovale shunting by injecting an aerated modified fluid gelatin solution, as previously described [14]. Echocardiographic images were recorded on videotape or compact disk, and a computer-assisted evaluation was performed off-line by two trained senior investigators (FB, AMD), with a third reading by a blinded expert (AVB) in case of disagreement or doubt (n = 28; overall agreement of 88 %). When possible, transthoracic echocardiography was also performed to assess pulmonary artery systolic pressure (PASP), using the tricuspid regurgitation continuous-wave Doppler technique. Undetectable values of tricuspid regurgitation were assigned a PASP value lower than any actually measured during the study (20 mmHg) [26–28]. In patients with cor pulmonale, respiratory and hemodynamic management or rescue therapies were not implemented with the aim of correcting or alleviating cor pulmonale. As compared to an isolated RV dilatation or pulmonary hypertension, cor pulmonale may reflect a more severe alteration of RV afterload [12, 29–31]. Patients were therefore further stratified into three groups based on the degree of pulmonary circulatory system dysfunction, as follows: no dysfunction (PASP ≤40 mmHg with normal RV size and normal interventricular septum kinetics), moderate dysfunction (PASP >40 mmHg or a dilated RV but without cor pulmonale), and severe dysfunction (cor pulmonale).
Statistical analysis
The data were analyzed using the SPSS Base 13.0 statistical software package (SPSS Inc, Chicago, IL, USA). Continuous data were expressed as mean ± standard deviation unless otherwise specified and were compared using the Student t test or Mann–Whitney test for independent samples. Categorical variables, expressed as percentages, were evaluated using the chi-square test or Fisher exact test. Survival data were analyzed with standard Kaplan–Meier techniques for estimation of survival probabilities. To evaluate independent factors associated with cor pulmonale or 28-day mortality, significant univariate risk factors were examined using backward stepwise logistic regression analysis. To avoid overfitting, we considered that we could enter a maximal number of five variables in the cor pulmonale model (in view of the 49 events observed) and nine variables in the 28-day mortality model (in view of the 91 events observed) [32]. Among related hemodynamic or respiratory significant univariate factors, only the most statistically relevant were entered into the regression models in order to minimize the effect of colinearity. The selection process was guided by maximal imbalances between groups, as estimated by absolute standardized differences, which are independent of the sample size and variable unit [33]. Coefficients were computed by the method of maximum likelihood. The calibrations of models were assessed by the Hosmer–Lemeshow goodness-of-fit statistic and discrimination was assessed by the receiver operating characteristics curves. Two-tailed p values smaller than 0.05 were considered significant.
Results
Patient characteristics
We included 226 patients (163 men and 63 women) with a mean age of 61 ± 17 years.
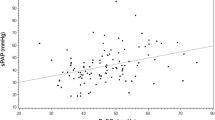
Mean delay between ARDS diagnosis and TEE was 0.85 ± 0.95 day. Cor pulmonale was detected in 49 patients (prevalence of 22 %; 95 % confidence interval, 16–27 %). The groups with and without cor pulmonale were not significantly different regarding age, SAPS II, or McCabe and Jackson class (Table 1). Lung injury was more often associated with an infectious etiology (pneumonia or non-pulmonary sepsis) in patients with cor pulmonale as compared with others [39 (79.6 %) vs. 102 (57.6 %), p < 0.01]. Respiratory settings at TEE day were different between groups, with lower values of respiratory system compliance and higher values of respiratory rate and driving pressure in the cor pulmonale group (Table 1). Although PaO2/FiO2 ratio values on the day of TEE were not different between the groups, the proportion of patients receiving nitric oxide inhalation on that day was significantly higher in the group with cor pulmonale compared to the other group [16 (33 %) vs. 25 (14 %), p < 0.01]. Multivariate logistic regression analysis identified infectious causes of lung injury and higher values of driving pressure as independent factors associated with cor pulmonale (Table 2).
Hemodynamic and echocardiographic findings
Patients with cor pulmonale exhibited a higher incidence of shock, higher heart rates, and lower systolic and mean arterial pressures at the time of TEE (Table 3). As expected, the group with cor pulmonale had larger right ventricle dimensions and higher PASP values. Patients with cor pulmonale also exhibited more atrial septal buckling towards the left atrium and more often a shunting across patent foramen ovale as compared to other patients. No significant differences were found between the two groups for SVC collapsibility, left ventricle systolic dysfunction, or cardiac index.
Outcome
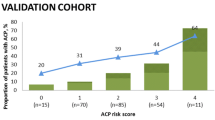
The outcome of patients with or without cor pulmonale is displayed in Table 1. The proportion of patients managed during the ICU stay with prone positioning and/or nitric oxide as adjunctive therapy for severe hypoxemia was larger in the group with cor pulmonale as compared to the other group. The pneumothorax rate during the ICU stay was not different between the groups. Mortality rates were significantly higher in the group with cor pulmonale (Table 1; Fig. 1). Among ICU survivors, mechanical ventilation duration and ICU duration were similar between the two groups (Table 1). The degree of pulmonary circulatory system dysfunction [no dysfunction (n = 69), moderate dysfunction (n = 108), and severe dysfunction (n = 49)] was associated with 28-day and hospital mortality (p = 0.006 and p = 0.018, respectively) (Fig. 2). Multivariate logistic regression analysis identified McCabe and Jackson class, lung injury not related to pneumonia, aspiration, or sepsis, driving pressure, lactic acidosis, and cor pulmonale as independent risk factors for 28-day mortality (Table E1, see ESM).
Stratification of 28-day mortality and hospital mortality in patients with acute respiratory distress syndrome by increasing degree of pulmonary circulatory system dysfunction. PCD denotes pulmonary circulatory system dysfunction, defined as absent (pulmonary artery systolic pressure ≤40 mmHg with normal right ventricle size and normal septal kinetics), moderate (pulmonary artery systolic pressure >40 mmHg or a dilated right ventricle without cor pulmonale), or severe (cor pulmonale). Asterisk indicates that three patients were lost to follow-up between day 21 and day 28
Discussion
The main finding of our study was that cor pulmonale was detected in 22 % of 226 ARDS patients ventilated with airway pressure limitation. Cor pulmonale occurrence was associated with infectious causes of lung injury and higher values of driving pressure. It was also associated with hemodynamic compromise and was an independent risk factor for 28-day mortality.
Prevalence of cor pulmonale
Increased RV afterload in ARDS patients may result from pulmonary vasoconstriction, vaso-occlusion, and/or endothelial dysfunction [2]. Pulmonary vascular dysfunction during ARDS may be enhanced by injurious mechanical ventilation [3]. The increasing use of protective ventilatory strategies for ARDS [34] in the clinical setting has been associated with a decreased prevalence of cor pulmonale [35]. Our study shows, however, the persistence of cor pulmonale in 22 % of ARDS patients in the era of protective mechanical ventilation. These findings are in accordance with another report that found a similar prevalence (25 %) of cor pulmonale in ARDS patients ventilated with a strategy aimed at limiting airway pressures, although tidal volume was slightly higher (8 ± 1 mL/kg) in that study [12].
Risk factors for cor pulmonale
We found an association between cor pulmonale and infectious causes of lung injury. Reversible myocardial depression in patients with sepsis was first reported in 1984 by Parker et al. [36], who described LV systolic dysfunction and dilatation using radionuclide cineangiography [36]. Subsequent studies using pulmonary artery catheterization or echocardiography confirmed these results and also noted the frequent association of a RV systolic dysfunction in more than 20 % of septic patients [37]. Depressed intrinsic contractility due to circulating cytokines is strongly suggested as being responsible for septic cardiomyopathy [38]. One may hypothesize that a RV with depressed intrinsic contractility due to sepsis may be more sensitive to pulmonary vascular dysfunction and increased afterload secondary to ARDS.
In our study, respiratory system compliance was more reduced in patients with cor pulmonale, probably reflecting a higher severity of lung injury in this subgroup. Because our ventilatory strategy was primarily aimed at limiting Pplat, these patients with more impaired lung mechanics were ventilated with smaller V T and PEEP values. Higher values of driving pressure were independently associated with cor pulmonale by multivariate analysis. Driving pressure may better mirror the tidal distending pressure, considered to reflect the mechanical forces operating on alveoli and capillaries during insufflation. In a previous study evaluating a ventilatory strategy with low V T and high PEEP, higher values of driving pressure were associated with increased 28-day mortality [39]. Whether a further decrease in V T in patients with very low respiratory system compliance could lessen pulmonary vascular dysfunction via a lowering of driving pressure warrants further research.
Clinical implication and prognosis of cor pulmonale
Cor pulmonale was associated with higher mortality by multivariate analysis in our study. Our finding differs from a previous report in which cor pulmonale did not influence mortality in a group of 75 ARDS patients undergoing mechanical ventilation with airway pressure limitation [12]. These investigators systematically implemented specific measures aimed at correcting cor pulmonale, a fact that may explain the lack of prognostic effect in their study [12]. Many biological (e.g., ratio of concentration of angiopoietin-2 relative to angiopoietin-1) [40], respiratory (e.g., dead-space fraction) [41], or hemodynamic (e.g., transpulmonary gradient or a central venous pressure higher than the pulmonary artery occlusion pressure) [11, 42] markers of pulmonary vascular dysfunction have been reported as independent predictors of death in ARDS patients. In our study, moderate pulmonary circulatory system dysfunction (defined as pulmonary hypertension or isolated RV dilatation, without cor pulmonale) was found in 48 % of patients and there was a progressive increase in mortality with increase in pulmonary circulatory system dysfunction severity. Whether pharmacological manipulation of pulmonary vascular tone (which is feasible in patients with ARDS, but without a proven benefit on mortality in unselected patients) [43] or prone positioning (which improves respiratory mechanics and alveolar ventilation, with reduced airway pressures and decreased RV pressure overload) [44] may alter mortality outcomes in the subgroup with cor pulmonale warrants further research.
Although the precise explanation of the increased mortality associated with cor pulmonale is not straightforward from our data, the hemodynamic compromise associated with cor pulmonale [45] could at least in part contribute to this worse outcome. In our study, patients with cor pulmonale presented more often with shock as compared to others, although left ventricle systolic function was similar between groups. Cor pulmonale was also associated with oxygenation compromise in our study. Adjunctive therapies for refractory hypoxemia were more frequently used in the group with cor pulmonale and these patients exhibited more shunting across patent foramen ovale as compared to others. An increase in right-sided pressures has been shown to favor right to left shunting via a patent foramen ovale during ARDS, a situation that could blunt the beneficial effects of increased PEEP on oxygenation in some patients if the worsening of intra-cardiac shunt overcomes the benefits on alveolar recruitment [14].
Study limitations
Our study has some limitations. First, TEE could not be performed in patients with contraindications; however, the vast majority of patients were assessed, as TEE is our first-line tool for hemodynamic management in ARDS patients. Second, we included patients during a 5-year period; however, our mechanical ventilation strategy did not vary during the study period. Third, we only report on a single TEE within 3 days of ARDS start. Data on serial TEE could be interesting inasmuch as RV afterload may progressively worsen with mechanical ventilation prolongation. Last, the monocentric nature of the study may challenge its external validity depending of the case mix of a given ICU, ventilator modalities used by intensivists, and the impact of cor pumonale diagnosis on a physician’s decisions.
In conclusion, cor pulmonale was identified in 22 % of a large series of ARDS patients ventilated with airway pressure limitation. Cor pulmonale occurred more often in case of sepsis and increased driving pressures. It was associated with higher mortality by multivariate analysis. Specific therapies and measures aimed at alleviating pulmonary vascular dysfunction and RV dysfunction should be tested in ARDS patients with cor pulmonale in the future.
References
Zapol WM, Snider MT (1977) Pulmonary hypertension in severe acute respiratory failure. N Engl J Med 296:476–480
Tomashefski JF Jr, Davies P, Boggis C, Greene R, Zapol WM, Reid LM (1983) The pulmonary vascular lesions of the adult respiratory distress syndrome. Am J Pathol 112:112–126
Moloney ED, Evans TW (2003) Pathophysiology and pharmacological treatment of pulmonary hypertension in acute respiratory distress syndrome. Eur Respir J 21:720–727
Vieillard-Baron A, Loubieres Y, Schmitt JM, Page B, Dubourg O, Jardin F (1999) Cyclic changes in right ventricular output impedance during mechanical ventilation. J Appl Physiol 87:1644–1650
Mekontso Dessap A, Voiriot G, Zhou T, Marcos E, Dudek SM, Jacobson JR, Machado R, Adnot S, Brochard L, Maitre B, Garcia JG (2012) Conflicting physiological and genomic cardiopulmonary effects of recruitment maneuvers in murine acute lung injury. Am J Respir Cell Mol Biol 46:541–550
Zapol WM, Jones R (1987) Vascular components of ARDS. Clinical pulmonary hemodynamics and morphology. Am Rev Respir Dis 136:471–474
Villar J, Blazquez MA, Lubillo S, Quintana J, Manzano JL (1989) Pulmonary hypertension in acute respiratory failure. Crit Care Med 17:523–526
Squara P, Dhainaut JF, Artigas A, Carlet J (1998) Hemodynamic profile in severe ARDS: results of the European Collaborative ARDS Study. Intensive Care Med 24:1018–1028
Sloane PJ, Gee MH, Gottlieb JE, Albertine KH, Peters SP, Burns JR, Machiedo G, Fish JE (1992) A multicenter registry of patients with acute respiratory distress syndrome. Physiology and outcome. Am Rev Respir Dis 146:419–426
Monchi M, Bellenfant F, Cariou A, Joly LM, Thebert D, Laurent I, Dhainaut JF, Brunet F (1998) Early predictive factors of survival in the acute respiratory distress syndrome. A multivariate analysis. Am J Respir Crit Care Med 158:1076–1081
Osman D, Monnet X, Castelain V, Anguel N, Warszawski J, Teboul JL, Richard C (2009) Incidence and prognostic value of right ventricular failure in acute respiratory distress syndrome. Intensive Care Med 35:69–76
Vieillard-Baron A, Schmitt JM, Augarde R, Fellahi JL, Prin S, Page B, Beauchet A, Jardin F (2001) Acute cor pulmonale in acute respiratory distress syndrome submitted to protective ventilation: incidence, clinical implications, and prognosis. Crit Care Med 29:1551–1555
Boissier F, Razazi K, Roche-Campo F, Leon R, Brun-Buisson C, Mekontso Dessap A (2012) Prévalence et pronostic du coeur pulmonaire aigu dans le SDRA. Réanimation 21:S9
Mekontso Dessap A, Boissier F, Leon R, Carreira S, Campo FR, Lemaire F, Brochard L (2010) Prevalence and prognosis of shunting across patent foramen ovale during acute respiratory distress syndrome. Crit Care Med 38:1786–1792
Ranieri VM, Rubenfeld GD, Thompson BT, Ferguson ND, Caldwell E, Fan E, Camporota L, Slutsky AS (2012) Acute respiratory distress syndrome: the Berlin definition. JAMA 307:2526–2533
Le Gall JR, Lemeshow S, Saulnier F (1993) A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA 270:2957–2963
McCabe W, Jackson GG (1962) Gram negative bacteriemia: I. Etiology and ecology. Arch Intern Med 110:847–855
ACCP/SCCM (1992) American College of Chest Physicians/Society of Critical Care Medicine Consensus Conference: definitions for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20:864–874
Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TM Jr, Musher DM, Niederman MS, Torres A, Whitney CG (2007) Infectious Diseases Society of America/American Thoracic Society consensus guidelines on the management of community-acquired pneumonia in adults. Clin Infect Dis 44(Suppl 2):S27–S72
Marik PE (2001) Aspiration pneumonitis and aspiration pneumonia. N Engl J Med 344:665–671
Mercat A, Richard JC, Vielle B, Jaber S, Osman D, Diehl JL, Lefrant JY, Prat G, Richecoeur J, Nieszkowska A, Gervais C, Baudot J, Bouadma L, Brochard L (2008) Positive end-expiratory pressure setting in adults with acute lung injury and acute respiratory distress syndrome: a randomized controlled trial. JAMA 299:646–655
Mekontso Dessap A, Charron C, Devaquet J, Aboab J, Jardin F, Brochard L, Vieillard-Baron A (2009) Impact of acute hypercapnia and augmented positive end-expiratory pressure on right ventricle function in severe acute respiratory distress syndrome. Intensive Care Med 35:1850–1858
Vieillard-Baron A, Charron C, Chergui K, Peyrouset O, Jardin F (2006) Bedside echocardiographic evaluation of hemodynamics in sepsis: is a qualitative evaluation sufficient? Intensive Care Med 32:1547–1552
Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, Gutgesell H, Reichek N, Sahn D, Schnittger I et al (1989) Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am Soc Echocardiogr 2:358–367
Jardin F, Dubourg O, Bourdarias JP (1997) Echocardiographic pattern of acute cor pulmonale. Chest 111:209–217
Berger M, Haimowitz A, Van Tosh A, Berdoff RL, Goldberg E (1985) Quantitative assessment of pulmonary hypertension in patients with tricuspid regurgitation using continuous wave Doppler ultrasound. J Am Coll Cardiol 6:359–365
Gladwin MT, Sachdev V, Jison ML, Shizukuda Y, Plehn JF, Minter K, Brown B, Coles WA, Nichols JS, Ernst I, Hunter LA, Blackwelder WC, Schechter AN, Rodgers GP, Castro O, Ognibene FP (2004) Pulmonary hypertension as a risk factor for death in patients with sickle cell disease. N Engl J Med 350:886–895
Mekontso Dessap A, Leon R, Habibi A, Nzouakou R, Roudot-Thoraval F, Adnot S, Godeau B, Galacteros F, Brun-Buisson C, Brochard L, Maitre B (2008) Pulmonary hypertension and cor pulmonale during severe acute chest syndrome in sickle cell disease. Am J Respir Crit Care Med 177:646–653
King ME, Braun H, Goldblatt A, Liberthson R, Weyman AE (1983) Interventricular septal configuration as a predictor of right ventricular systolic hypertension in children: a cross-sectional echocardiographic study. Circulation 68:68–75
Louie EK, Rich S, Brundage BH (1986) Doppler echocardiographic assessment of impaired left ventricular filling in patients with right ventricular pressure overload due to primary pulmonary hypertension. J Am Coll Cardiol 8:1298–1306
Jessup M, Sutton MS, Weber KT, Janicki JS (1987) The effect of chronic pulmonary hypertension on left ventricular size, function, and interventricular septal motion. Am Heart J 113:1114–1122
Peduzzi P, Concato J, Kemper E, Holford TR, Feinstein AR (1996) A simulation study of the number of events per variable in logistic regression analysis. J Clin Epidemiol 49:1373–1379
Austin PC (2009) Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med 28:3083–3107
The Acute Respiratory Distress Syndrome Network (2000) Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med 342:1301–1308
Jardin F, Fellahi JL, Beauchet A, Vieillard-Baron A, Loubieres Y, Page B (1999) Improved prognosis of acute respiratory distress syndrome 15 years on. Intensive Care Med 25:936–941
Parker MM, Shelhamer JH, Bacharach SL, Green MV, Natanson C, Frederick TM, Damske BA, Parrillo JE (1984) Profound but reversible myocardial depression in patients with septic shock. Ann Intern Med 100:483–490
Vieillard-Baron A, Caille V, Charron C, Belliard G, Page B, Jardin F (2008) Actual incidence of global left ventricular hypokinesia in adult septic shock. Crit Care Med 36:1701–1706
Rudiger A, Singer M (2007) Mechanisms of sepsis-induced cardiac dysfunction. Crit Care Med 35:1599–1608
Amato MB, Barbas CS, Medeiros DM, Magaldi RB, Schettino GP, Lorenzi-Filho G, Kairalla RA, Deheinzelin D, Munoz C, Oliveira R, Takagaki TY, Carvalho CR (1998) Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 338:347–354
Ong T, McClintock DE, Kallet RH, Ware LB, Matthay MA, Liu KD (2010) Ratio of angiopoietin-2 to angiopoietin-1 as a predictor of mortality in acute lung injury patients. Crit Care Med 38:1845–1851
Nuckton TJ, Alonso JA, Kallet RH, Daniel BM, Pittet JF, Eisner MD, Matthay MA (2002) Pulmonary dead-space fraction as a risk factor for death in the acute respiratory distress syndrome. N Engl J Med 346:1281–1286
Bull TM, Clark B, McFann K, Moss M (2010) Pulmonary vascular dysfunction is associated with poor outcomes in patients with acute lung injury. Am J Respir Crit Care Med 182:1123–1128
Afshari A, Brok J, Moller AM, Wetterslev J (2010) Inhaled nitric oxide for acute respiratory distress syndrome (ARDS) and acute lung injury in children and adults. Cochrane Database Syst Rev CD002787
Vieillard-Baron A, Charron C, Caille V, Belliard G, Page B, Jardin F (2007) Prone positioning unloads the right ventricle in severe ARDS. Chest 132:1440–1446
Sibbald WJ, Driedger AA (1983) Right ventricular function in acute disease states: pathophysiologic considerations. Crit Care Med 11:339–345
Acknowledgments
This study was funded by the nonprofit public organization Assistance Publique—Hôpitaux de Paris.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Boissier, F., Katsahian, S., Razazi, K. et al. Prevalence and prognosis of cor pulmonale during protective ventilation for acute respiratory distress syndrome. Intensive Care Med 39, 1725–1733 (2013). https://doi.org/10.1007/s00134-013-2941-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-013-2941-9