Abstract
Purpose
To establish the baseline prescribing error rate in a tertiary paediatric intensive care unit (PICU) and to determine the impact of a zero tolerance prescribing (ZTP) policy incorporating a dedicated prescribing area and daily feedback of prescribing errors.
Methods
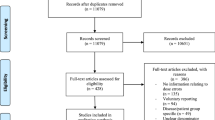
A prospective, non-blinded, observational study was undertaken in a 12-bed tertiary PICU over a period of 134 weeks. Baseline prescribing error data were collected on weekdays for all patients for a period of 32 weeks, following which the ZTP policy was introduced. Daily error feedback was introduced after a further 12 months. Errors were sub-classified as ‘clinical’, ‘non-clinical’ and ‘infusion prescription’ errors and the effects of interventions considered separately.
Results
The baseline combined prescribing error rate was 892 (95 % confidence interval (CI) 765–1,019) errors per 1,000 PICU occupied bed days (OBDs), comprising 25.6 % clinical, 44 % non-clinical and 30.4 % infusion prescription errors. The combined interventions of ZTP plus daily error feedback were associated with a reduction in the combined prescribing error rate to 447 (95 % CI 389–504) errors per 1,000 OBDs (p < 0.0001), an absolute risk reduction of 44.5 % (95 % CI 40.8–48.0 %). Introduction of the ZTP policy was associated with a significant decrease in clinical and infusion prescription errors, while the introduction of daily error feedback was associated with a significant reduction in non-clinical prescribing errors.
Conclusion
The combined interventions of ZTP and daily error feedback were associated with a significant reduction in prescribing errors in the PICU, in line with Department of Health requirements of a 40 % reduction within 5 years.


Similar content being viewed by others
Abbreviations
- ANOVA:
-
Analysis of variance
- ARR:
-
Absolute risk reduction
- CI:
-
Confidence interval
- CPOE:
-
Computerised prescriber order entry
- DoH:
-
Department of Health
- ICU:
-
Intensive care unit
- LCL:
-
Lower confidence limit
- NHS:
-
National Health Service
- NICU:
-
Neonatal intensive care unit
- OBDs:
-
Occupied bed days
- PICANet:
-
Paediatric Intensive Care Audit Network
- PICU:
-
Paediatric intensive care unit
- PIM2:
-
Paediatric index of mortality 2
- rINN:
-
Recommended international non-proprietary name
- RRR:
-
Relative risk reduction
- UCL:
-
Upper confidence limit
- UK:
-
United Kingdom
- US:
-
United States
- ZTP:
-
Zero tolerance prescribing
References
Moyen E, Camire E, Stelfox HT (2008) Clinical review: medication errors in critical care. Crit Care 12:208. doi:10.1186/cc6813
Department of Health (2004) Building a safer NHS for patients: improving medication safety. The Stationery Office, London
Camire E, Moyen E, Stelfox HT (2009) Medication errors in critical care: risk factors, prevention and disclosure. CMAJ 180:936–943
McDowell SE, Ferner HS, Ferner RE (2009) The pathophysiology of medication errors: how and where they arise. Br J Clin Pharmacol 67:605–613
Kane-Gill SL, Jacobi J, Rothschild JM (2010) Adverse drug events in intensive care units: risk factors, impact, and the role of team care. Crit Care Med 38:S83–S89
Ghaleb MA, Barber N, Franklin BD, Wong IC (2010) The incidence and nature of prescribing and medication administration errors in paediatric inpatients. Arch Dis Child 95:113–118
Mani V, Wheeler DW (2010) Drug form and expression of concentration may also lead to prescription errors. Drug Saf 33:167–168
Lesar S (2006) Medication safety in critically ill children. Clin Ped Emerg Med 7:215–225
Department of Health (2000) An organisation with a memory: report of an expert group on learning from adverse events in the NHS. The Stationery Office, London
Kaushal R, Bates DW, Abramson EL, Soukup JR, Goldmann DA (2008) Unit-based clinical pharmacists’ prevention of serious medication errors in pediatric inpatients. Am J Health Syst Pharm 65:1254–1260
Miller MR, Robinson KA, Lubomski LH, Rinke ML, Pronovost PJ (2007) Medication errors in paediatric care: a systematic review of epidemiology and an evaluation of evidence supporting reduction strategy recommendations. Qual Saf Health Care 16:116–126
Al-Jeraisy MI, Alanazi MQ, Abolfotouh MA (2011) Medication prescribing errors in a pediatric inpatient tertiary care setting in Saudi Arabia. BMC Res Notes 14:294
Alagha HZ, Badary OA, Ibrahim HM, Sabri NA (2011) Reducing prescribing errors in the paediatric intensive care unit: an experience from Egypt. Acta Paediatr 100:e169–e174
Montesi G, Lechi A (2009) Prevention of medication errors: detection and audit. Br J Clin Pharmacol 67:651–655
Leape LL (1995) Preventing adverse drug events. Am J Health Syst Pharm 52:379–382
Dean B, Barber N, Schachter M (2000) What is a prescribing error? Qual Health Care 9:232–237
Slater A, Shann F, Pearson G (2003) PIM2: a revised version of the paediatric index of mortality. Int Care Med 29:278–285
Franklin BD, Reynolds M, Shebl NA, Burnett S, Jacklin A (2011) Prescribing errors in hospital inpatients: a three-centre study of their prevalence, types and causes. Postgrad Med J 87:739–745
Nichols P, Copeland TS, Craib IA, Hopkins P, Bruce DG (2008) Learning from error: identifying contributory causes of medication errors in an Australian hospital. Med J Aust 188:276–279
Leonard MS, Cimino M, Shaha S, McDougal S, Pilliod J, Brodsky L (2006) Risk reduction for adverse drug events through sequential implementation of patient safety initiatives in a children’s hospital. Pediatrics 118:e1124–e1129
Alvarez G, Coiera E (2005) Interruptive communication patterns in the intensive care unit ward round. Int J Med Inform 74:791–796
Tang Z, Weavind L, Mazabob J, Thomas EJ, Chu-Weininger MY, Johnson TR (2007) Workflow in intensive care unit remote monitoring: a time-and-motion study. Crit Care Med 35:2057–2063
Hohenhaus SM, Powell SM (2008) Distractions and interruptions: development of a healthcare sterile cockpit. Newborn Infant Nurs Rev 8:108–110
Safe Medicine Use Expert Committee (2010) Chapter 1066: physical environments that promote safe medication use. In: USP33-NF28, The United States Pharmacopeia/National Formulary. United States Pharmacopeial Convention. Available via http://www.usp.org/sites/default/files/usp_pdf/EN/USPNF/c1066.pdf Accessed 20 May 2012
Kohn LT, Corrigan JM, Donaldson MS (1999) To err is human: building a safer health system. National Academy Press, Washington, DC
Trooskin SZ (2002) Low-technology, cost-efficient strategies for reducing medication errors. Am J Infect Control 30:351–354
Beckmann U, Bohringer C, Carless R, Gillies DM, Runciman WB, Wu AW, Pronovost P (2003) Evaluation of two methods for quality improvement in intensive care: facilitated incident monitoring and retrospective medical chart review. Crit Care Med 31:1006–1011
Ferner RE (2009) The epidemiology of medication errors: the methodological difficulties. Br J Clin Pharmacol 67:614–620
Wheeler SJ, Wheeler DW (2005) Medication errors in anaesthesia and critical care. Anaesthesia 60:257–273
Ghaleb MA, Barber N, Dean Franklin B, Wong IC (2005) What constitutes a prescribing error in paediatrics? Qual Saf Health Care 14:352–357
Potts AL, Barr FE, Gregory DF, Wright L, Patel NR (2004) Computerized physician order entry and medication errors in a pediatric critical care unit. Pediatrics 113:59–63
Kadmon G, Bron-Harlev E, Nahum E, Schiller O, Haski G, Shonfeld T (2009) Computerized order entry with limited decision support to prevent prescription errors in a PICU. Pediatrics 124:935–940
Vaidya V, Sowan AK, Mills ME, Soeken K, Gaffoor M, Hilmas E (2006) Evaluating the safety and efficiency of a CPOE system for continuous medication infusions in a pediatric ICU. AMIA Annu Symp Proc 2006:1128
Han YY, Carcillo JA, Venkataraman ST, Clark RS, Watson RS, Nguyen TC, Bayir H, Orr RA (2005) Unexpected increased mortality after implementation of a commercially sold computerized physician order entry system. Pediatrics 116:1506–1512
Koppel R, Metlay JP, Cohen A, Abaluck B, Localio AR, Kimmel SE, Strom BL (2005) Role of computerized physician order entry systems in facilitating medication errors. JAMA 293:1197–1203
Campbell EM, Sittig DF, Ash JS, Guappone KP, Dykstra RH (2006) Types of unintended consequences related to computerized provider order entry. J Am Med Inform Assoc 13:547–556
Walsh KE, Adams WG, Bauchner H, Vinci RJ, Chessare JB, Cooper MR, Hebert PM, Schainker EG, Landrigan CP (2006) Medication errors related to computerized order entry for children. Pediatrics 118:1872–1879
Redwood S, Rajakumar A, Hodson J, Coleman JJ (2011) Does the implementation of an electronic prescribing system create unintended medication errors? A study of the sociotechnical context through the analysis of reported medication incidents. BMC Med Inform Decis Mak 11:29
Barber N (2010) Electronic prescribing—safer, faster, better? J Health Serv Res Policy 15(S1):64–67
Caldwell NA, Power B (2011) The pros and cons of electronic prescribing for children. Arch Dis Child 97:124–128
Reckmann MH, Westbrook JI, Koh Y, Lo C, Day RO (2009) Does computerized provider order entry reduce prescribing errors for hospital inpatients? A systematic review. J Am Med Inform Assoc 16:613–623
Acknowledgments
Sincere thanks go to Ms Lynne Cochrane and Ms Venetia Horn for their constant support, Mr Duncan Shephard for his assistance with the statistical process control charts, Ms Gemma Ellis for her advice and encouragement and to Dr Allan Wardhaugh for the original concept of zero tolerance prescribing.
Author information
Authors and Affiliations
Corresponding author
Additional information
On behalf of the PICU/NICU Risk Action Group
Electronic supplementary material
Below is the link to the electronic supplementary material.
Appendix: Great Ormond St Hospital PICU/NICU Risk Action Group
Appendix: Great Ormond St Hospital PICU/NICU Risk Action Group
Mark Peters, MB ChB PhD MRCP FRCPCH
Rachelle Booth, BPharm MSc MRPharmS GPhC MPSNZ
Emma Sturgess, BSc RN
Alison Taberner-Stokes, RN
Andy Petros, MB BS MSc FRCP(UK) FRCPCH
Joe Brierley, MA MB ChB MRCP MRCPCH
Christine Pierce, MB BS BSc MRCP FRCPCH
Sanjiv Sharma, MBBS BSc MRCPCH
Paula Lister, MB BCh MRCPCH
Sophie Skellett, MA MB BChir MRCP FRCPCH
Quen Mok, MB BS DCH FRCP FRCPI FRCPCH
Darren Darby, RN MA
Kimberley Gray, RN Lead Nurse NICU
Ghislaine Stephenson, RN Lead Nurse PICU
Roisin Mulvaney, Patient Safety Manager
Rights and permissions
About this article
Cite this article
Booth, R., Sturgess, E., Taberner-Stokes, A. et al. Zero tolerance prescribing: a strategy to reduce prescribing errors on the paediatric intensive care unit. Intensive Care Med 38, 1858–1867 (2012). https://doi.org/10.1007/s00134-012-2660-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00134-012-2660-7