Abstract
Background
A large proportion of sickness absence (SA) in young adults is due to common mental disorders (CMDs). Still studies on CMD-related SA in young workers are lacking, especially studies for those employed in the private sector. The current study investigated the associations between sector of employment, occupational class and SA due to CMDs. In addition, associations between type of employment branch and SA due CMDs within each sector were examined.
Methods
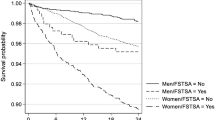
This population-based longitudinal cohort study included 663,583 employees, 19–29 years, residing in Sweden in 2009. Employment sector (i.e., private/public) and occupational class (non-manual/manual workers) were measured in 2009. Risk estimates of SA due to CMDs, between 2010 and 2016, were calculated as Hazard Ratios (HR) with 95% confidence intervals (CI), using Cox regression analysis.
Results
Sector of employment was associated with SA due to CMDs, such that public sector workers had an elevated risk when compared with private sector employees (adjusted HR: 1.31 (95% CI 1.29–1.33). Moreover, manual workers had a slightly elevated risk for SA due to CMDs compared to non-manual workers. Within the private sector, in both manual and non-manual workers, those employed in education and health and social services evidenced the highest rates and risks of SA due to CMDs.
Conclusion
Sector of employment and occupational class play a role in SA due to CMDs in young employees. These findings should be considered when identifying high-risk groups for SA in the young working population.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Over the past decades, research has shown that the rates of common mental disorders (CMDs), i.e., depressive, anxiety and stress-related disorders, are high in young adults in many Western countries, including Sweden [1]. According to recent statistics from the World Health Organization (WHO), CMDs account for the largest proportion of mental disorders in children and adolescents [2]. Almost 20% of the population in the WHO European Region aged 10–19 years are estimated to have a mental disorder, of which CMDs accounts for over 40% [2].
CMDs are characterized by having an early age of onset [3], recurrent episodes as well as high levels of comorbid disorders, including substance use disorders and musculoskeletal diseases [3, 4].
Studies have further shown that CMDs in young age may have a potential negative effect on academic attainment, and subsequently on work opportunities [5], as CMDs can significantly reduce the individual’s work ability [6,7,8,9]. The loss of productivity associated with reduced work capacity is a very large burden to the individual and the society, if individuals face marginalization at the labor market in early age. In young adults in Sweden, the labor-market situation has become more problematic over the past decade, with youth unemployment rates higher than the OECD average [1]. Recent reports from Norway and Denmark have further shown an alarming increase in sickness absence (SA) in young adults [10], and particularly SA due to CMDs [6]. Mental disorders, and CMDs in particular, are now also the most common reason for SA in Sweden in younger ages [6]. Although several studies have shown that SA due to CMDs is far more common in a group of young adults who are not employed [1], studies on prevalence and incidence rates of SA due to CMDs in young adults who are employed are lacking [11]. The literature is even more limited regarding SA among young workers employed in the private sector. This is somewhat surprising, as up to 80% of young employees in Sweden work in the private sector [12]. Moreover, previous research focusing on differences in SA between labor market sectors, such as private and public sectors is scarce [13,14,15], especially in young employees.
Two contradictory theoretical viewpoints have been put forward either claiming differences or similarities regarding organizational and management structures as well as psychosocial work stress in public and private sectors [16]. Likewise, studies have found or failed to find differences regarding the psychosocial work environment in these two sectors [17]. Those studies finding differences found that job stress was higher in the public sector. It can, therefore, by hypothesized that SA due to CMDs might be higher in the public compared to the private sector, as an adverse psychosocial work environment has been linked to sickness absence due to these disorders [18]. Studies on these associations are, however, lacking to date.
Within the public sector, those employed in certain occupational groups, such as health care professionals, have been pointed out as having a markedly elevated risk for any SA [10, 19] and SA due to CMDs in particular [20, 21]. Within the private sector on the other hand, a higher risk of SA has been found in employees working in service occupations, whereas lower SA rates have been observed within business and finance professionals [19]. Still studies examining whether similar associations in these sectors also can be found in young workers are lacking to date. With respect to SA, identifying high-risk groups of professionals is of importance when targeting individuals at risk, and to increase our understanding of the determinants of SA due to CMDs.
Occupational class is also associated with physical and psychosocial working conditions, that may affect health and work. Occupational class is often characterized as non-manual and manual, the latter often having higher risk of work disability due to CMDs [21,22,23]. A recent Finnish study examined the magnitude of occupational class differences in all-cause SA in younger adults in the public sector and found that the SA rates in both women and men were highest in manual workers [24]. Whether similar differences for SA due to CMDs also hold for young employees in the private sector has been less studied to date. Research on the relationship between employment sector and SA due to CMDs is also restricted, especially regarding the younger working population.
The current register-based study used a large cohort of nearly 665,000 employed individuals between the ages of 19 and 29 years in Sweden, to investigate: (i) the associations between sector of employment, occupational class, and SA due to CMDs; and (ii) within each sector, the associations between different types of employment branches and SA due to CMDs.
Materials and methods
Study population
The study population was defined from the Longitudinal Integration Database for Health Insurance and Labor Market Studies (LISA) register [25]. This register contains data from the labor market and from the educational and social sectors. We included all individuals, aged 19–29 years residing in Sweden on December 31st, 2009 (n = 1,310,264). Only those classified as being in employment in the register in 2009 were included (n = 758,846). Those with incomplete or missing information on occupational class (n = 93,708, 12.3%) were excluded. Finally, we excluded individuals who were on DP in 2009 (n = 1,555, 0.2%). The final study population comprised 663,583 individuals, of whom 79% were working in the private sector.
We used the unique (de-identified) Swedish personal identity number to link information from several population-based registers. The National Patient Register (NPR) includes information on inpatient care since 1987 and for specialized outpatient care since 2001. Diagnoses in NPR are coded according to the International Classification of Diseases version 10 (ICD-10). The Cause of Death Register (CDR) comprises information on all deaths of Swedish residents since 1952. Finally, the Micro-data for analyses of the social insurance (MiDAS) register covers detailed data on SA and DP from 1994 onwards.
Sector of employment and occupational class
Sector of employment, i.e., private or public sector in which the individuals worked in 2009 was obtained from LISA. We used the Swedish Standard Classification of Occupations, obtained from LISA in 2009 [25], to categorize [26] and study manual and non-manual employees separately. We further categorized individuals according to the branches in which they worked in 2009. Here we used the Swedish Standard Industrial Classification (acronym SNI), which is based on EU’s recommended standard NACE Rev.2, the European Classification of Economic Activities [27]. More specifically, the following seven categories were studied: Industry occupations (including agriculture, forestry and fishing; mining and quarrying; manufacturing; electricity, gas, steam and air conditioning supply; water supply; sewerage etc.); Service occupations (including information and communication; financial and insurance activities; real estate activities etc.); Wholesale and retail trade; Accommodation and food service activities; Transportation (including occupations within transportation and storage); Construction; Education, and Health and social services. In the analyses, those with missing (n = 4755) were treated as a separate group.
Sickness absence (SA)
In Sweden, all residents aged 16–65 years who have income from work, unemployment benefits, parental benefits or student benefits are entitled to sickness benefits from the Social Insurance Agency (SIA), if unable to work due to disease or injury. Sickness benefits amount up to 80% of lost income. For those employed, the employer usually pays for the first 14 days of an SA spell. Thus, data on most of the short SA spells are not available in the MiDAS register, from which we obtained all diagnosis-specific sick-leave spells during the follow-up period 2010–2016. SA due to CMDs were defined as having at least one sick-leave spell with a main diagnosis for major depressive disorders (code according to the International Classification of Diseases version 10, ICD-10: F32–33), phobic anxiety disorders (ICD-10: F40), other anxiety disorders (ICD-10: F41), obsessive–compulsive disorders (ICD-10: F42) and reaction to severe stress and adjustment disorders (ICD-10: F43). In addition, we examined long-term sickness absence (LTSA) due to CMDs, defined as having a number of net SA days > 90 days during follow-up and short-term absence (≤ 90 days).
Confounders
Several demographic characteristics with known associations to both work factors, SA and CMDs were considered as potential confounders. These included age, sex, highest attained educational level, family situation, type of residential area, country of birth and all-cause LTSA in 2009 (please see Table 1 for information on categorization of the confounders). We also took into consideration psychiatric morbidity at baseline (defined as inpatient or specialized outpatient care with a main diagnosis for mental disorder in 2009 (ICD-10: F00–F99), as well as somatic morbidity in 2009 (defined as inpatient or specialized outpatient care with a main diagnosis for somatic disease) (defined in Table 2). Missing values in any confounder were grouped as separate categories in the multivariate analyses.
Statistical analysis
Statistically significance of differences between groups (Table 1) was evaluated by χ2 tests. Multivariate analyses were conducted with Cox regression models of time to first SA due to CMDs (any length and LTSA, respectively). Results are presented as Hazard Ratios (HR) with 95% confidence intervals (CIs). We assessed person-years at risk by totaling the years that the individuals were alive and living in Sweden during the follow-up period. The entry date was defined as January 1st, 2010, and the exit date as the date of first outcome, date of death, date of DP, date of emigration, or the end of follow-up (December 31st, 2016). We present the crude estimates and the estimates adjusted for all covariates described above. Analyses were conducted in SAS 9.4 (SAS Institute Inc., Cary, NC).
Sensitivity analyses
As both SA and CMDs are more common in women [4, 19, 28, 29], we carried out sex-stratified analyses (presented as supplementary tables). In additional sensitivity analyses, we excluded 18,502 individuals with mental disorder in 2009 and re-ran the analyses. Here, mental disorders were defined as either being sickness absent with a psychiatric diagnosis (ICD-10: F00–99) or being treated in inpatient or specialized outpatient care with a psychiatric diagnosis in the same year. Last, in separate analyses we compared characteristics for those excluded due to missing data on occupational class with the individuals included in the study.
Results
Sociodemographic characteristics of the study population are presented in Table 1. The majority of individuals worked in the private sector (79% vs 21%). Moreover, those working in the private sector were slightly younger, more often males, had a lower educational level, and were more often living in a big city area than employees in the public sector (p < 0.001). Within the private sector, 77% were manual workers (compared to 60% of those working in the public sector). Non-manual workers in the private sector were more likely to be females and to have college or university degree, when compared to manual workers in the same sector.
Table 2 presents work- and health-related characteristics for the cohort, stratified by sector of employment and occupational class. In the private sector, a large proportion (30%) worked within industry occupations (30%), followed by service occupations (29%). Public sector employees on the other hand were more likely to work in education (54%). Of them especially manual workers had slightly higher levels of psychiatric and somatic morbidity and SA at baseline compared to workers in the private sector.
Sector of employment was associated with SA due to CMDs (Table 3), such that public sector employees had an elevated risk when compared with individuals employed in the private sector [adjusted HR (aHR) for SA (any number of days): 1.31 (95% CI 1.29–1.33) and for LTSA: 1.29 (95% CI 1.26–1.32)]. Overall, manual workers had a slightly elevated risk for SA due to CMDs compared to non-manual workers. When stratifying the analyses by sector of employment, manual workers in the public sector had a particularly increased risk for SA due to CMDs when compared to non-manual workers in the same sector (aHR for SA (any number of days): 1.13 (95% CI 1.09–1.18) and for LTSA: 1.11 (95% CI 1.05–1.17)). These patterns were not observed in the private sector.
Tables 4 and 5 show the HRs for SA due to CMDs by occupational class and employment branch in private and public sector employees, respectively. For private sector employees, in both manual and non-manual workers, those employed in education and health and social services evidenced the highest rates and risks of SA due to CMDs. In manual workers, when compared to employees in industry occupations, highest HRs for any SA were observed in health and social services [aHR: 1.43 (95% CI 1.37–1.50), and for LTSA in education (aHR: 1.45 (95% CI 1.31–1.61)]. Construction workers (a majority of which were males) on the other hand evidenced the lowest risk for both outcomes. In non-manual workers, those employed in education had the highest risk of SA (any days) [aHR: 1.45 (95% CI 1.33–1.59)] as well as of LTSA [aHR: 1.35 (95% CI 1.20–1.53)] when compared to non-manual workers in industry occupations (Table 4). Similar tendencies were observed for public sector employees (Table 5), but due to small numbers, adjusted estimates were not statistically significant.
In sensitivity analyses stratified by sex (see Supplementary Tables 1 and 2), we found sex differences in employment branches. For instance, in the private sector, 72% of the women worked in service, wholesale and retail trade, compared to 33% of the men. A large proportion of men was found in industry and construction occupations (see Supplementary Table 1). In both the private and public sector, women were also more likely to work in health and social services compared to men. During the follow-up women had markedly higher rates of SA and LTSA due to CMDs compared to men (see Supplementary Table 2). Moreover, a significant association between occupational class and SA was seen for women, but not for men [aHR for SA (any days) in women: 1.05 (95% CI 1.03–1.08), and in men: 1.01 (95% CI 0.97–1.06)].
We also carried out sensitivity analyses excluding individuals with a treated mental disorder at baseline (see Supplementary Table 3). Results from these analyses were similar to the main analyses.
Analyses not shown revealed that individuals excluded due to missing on occupational class were more likely to be younger, male, born abroad and to possess less education compared to those included in the study. They had slightly lower rates of SA due to CMDs compared to the final study sample.
Discussion
Key findings
In this population-based cohort study of 663,583 young employees in Sweden, we found that sector of employment was associated with SA due to CMDs, such that public sector workers had an elevated risk when compared with private sector employees. Moreover, manual workers had a slightly elevated risk for SA due to CMDs compared to non-manual workers. Within the private sector, in both manual and non-manual workers, those employed in education and health and social services evidenced the highest rates and risks of SA due to CMDs. The lowest risks of both outcomes were seen in construction workers. Similar tendencies were also observed in public sector employees.
Findings in relation to other studies
In our study, 10% of the young adults were sickness absent due to CMDs during the follow-up period (Table 3). The proportion was slightly higher (15%) in public sector employees, who had a higher risk of both short- and long-term SA due to CMDs compared to those working in the private sector. These findings are in line with some earlier studies, demonstrating a higher prevalence of all-cause SA in the public sector [19]. To the best of our knowledge, our study is the first to also examine LTSA due to CMDs in the young working population. Our study showed that in general, manual workers had a higher risk compared to non-manual workers. These findings, which have been confirmed in earlier studies [21,22,23] were observed in both sectors of employment.
When we further analyzed type of employment branch and SA due to CMDs, private sector employees in education and health and social services stood out as having highest rates of SA due to CMDs (Table 4). Moreover, among manual workers, those working in service occupations also had an elevated risk of SA when compared with employees in industry occupations, which is consistent with earlier research [19]. In public sector employees, occurrence of SA due to CMDs was quite low when stratified by employment branch groups. Nevertheless, those employed in health and social services had highest rates of SA due to CMDs, which is in accordance with some prior studies [20, 21].
The higher rate of SA due to CMDs found among young public sector employees may have various underlying reasons. First of all, we observed a higher psychiatric and somatic morbidity in public sector employees, which may explain the higher SA rates. Still, analyses have been adjusted for previous specialized health care. We also noticed higher SA rates at baseline in public sector employees. Occupational class differences in SA in general [21, 24, 30,31,32] and due to mental disorders [21, 31] are known. In our study, manual workers had a higher risk of SA due to CMDs compared to non-manual workers, both in the private and public sector. One explanation for the socioeconomic inequalities in depression-related SA is that manual workers may be exposed to less favorable working conditions [22], such as heavy physical work demands and uncomfortable working positions, all of which have been identified as a predictor of SA. Here, it is also important to consider that the association between occupational class and SA due to CMDs may vary between those who seek treatment and those who do not. It has been shown that socioeconomic status play a part in treatment-seeking, even in Sweden, a country with universal access to healthcare [33]. The effect of socioeconomic status on the risk of sickness absence due to CMDs is, therefore, multifaceted. Here pathways to early marginalization might be driven by both health selection and social causation processes, which are likely to be strongly intertwined [34]. As CMDs are often characterized by an early age of onset, problems might already arise in adolescence and young adulthood when affected individuals may not fully develop knowledge and competencies or psychological and cognitive capabilities [35]. Such competencies and capabilities are necessary for achieving certain educational and occupational levels. Particularly the accumulation of disadvantages over the life course may take a long-term toll on health through a process that puts people already facing serious adversities at risk for continued exposure to further adverse circumstances [36]. Individuals exposed to social inequalities and marginalization at the labor market may be trapped in a self-perpetuating cycle involving stressful life and workplace circumstances, poor mental health and restrictions in social and occupational functioning leading to long periods of work disability [36, 37]. Strategies targeting adolescents with poor psychosocial life conditions (i.e., before entrance in the labor market) are, therefore, advisable to prevent early labor market marginalization in young adults.
Moreover, differences in psychosocial work environment may explain these findings as it has consistently been shown to be of great importance for mental health. Psychosocial work stressors that have been pointed out as risk factors for CMDs include job strain, low decision latitude, low social support, high psychological demands, effort–reward imbalance, and high job insecurity. In addition, there may be other factors contributing to the socioeconomic differences in SA due to mental disorders. For example, comorbid mental and somatic disorders are more common in lower SES groups [11, 38], and similar tendencies were also observed in our study. In addition, the socioeconomic gradient in overall sickness absence could also be attributed to health behaviors, which tend to be more detrimental in manual occupations.
With respect to differences in employment branches, higher SA levels have been observed in individuals employed in the health and social work sector, which was also demonstrated in our study on young employees. These findings have among others been explained by the unfavorable psychosocial and physical work conditions more present in these branches [39].
Strengths and limitations
The strengths of this study include the longitudinal population-based design, use of national registers with high completeness and validity, and practically no loss to follow-up. Moreover, with the large sample size, we were able to conduct detailed analyses of different employment branches, and ability to adjust for a range of important confounders. Still a number of important limitations need to be considered when interpreting the study results. First, the register does not contain information about the first 14 days of the SA spell, as these are usually paid by the employer. Therefore, those with SA < 14 days will be misclassified as not having the outcome. This potential outcome misclassification could lead to an underestimation of the studied associations. Second, with respect to comorbidity, there is a potential risk of unmeasured residual confounding as morbidity was only measured by specialized health care. The lack of data on occupational class throughout the entire follow-up period might have led to over- or underestimation of the reported estimates. Last, we did not have information on factors reflecting the work environment. This may be especially relevant regarding the psychosocial work environment, as this may be of importance for the studied associations.
Conclusion
In conclusion, this study of young employees in Sweden suggests that public sector workers, and those working in manual occupations are particularly at risk for SA due to CMDs. Within different employment branches, those working in health care and education were identified as having an elevated risk of SA due to CMDs. These findings should be considered when identifying high-risk groups for SA in the young working population.
References
OECD (2013) Youth in Sweden, mental ill-health and the transition into the labor market. In: mental health and work. OECD Publishing, Sweden. https://doi.org/10.1787/9789264188730-en
World Health Organization (2018) Adolescent mental health in the European Region. http://www.euro.who.int/__data/assets/pdf_file/0005/383891/adolescent-mh-fs-eng.pdf?ua=1. Accessed 01 Sep 2020
Kessler RC, Amminger GP, Aguilar-Gaxiola S et al (2007) Age of onset of mental disorders: a review of recent literature. Curr Opin Psychiatry 20(4):359–364. https://doi.org/10.1097/YCO.0b013e32816ebc8c
Jacobi F, Wittchen HU, Holting C et al (2004) Prevalence, co-morbidity and correlates of mental disorders in the general population: results from the German health interview and examination survey (GHS). Psychol Med 34(4):597–611. https://doi.org/10.1017/S0033291703001399
Veldman K, Reijneveld SA, Ortiz JA et al (2015) Mental health trajectories from childhood to young adulthood affect the educational and employment status of young adults: results from the TRAILS study. J Epidemiol Commun Health 69(6):588–593. https://doi.org/10.1136/jech-2014-204421
Social Insurance Agency (2017) Social insurance in figures 2017
Mauramo E, Lallukka T, Lahelma E et al (2018) Common mental disorders and sickness absence: a register-linkage follow-up study among finnish municipal employees. J Occup Environ Med 60(6):569–575. https://doi.org/10.1097/JOM.0000000000001289
Stansfeld SA, Fuhrer R, Head J (2011) Impact of common mental disorders on sickness absence in an occupational cohort study. Occup Environ Med 68(6):408–413. https://doi.org/10.1136/oem.2010.056994
Koopmans PC, Roelen CA, Groothoff JW (2008) Sickness absence due to depressive symptoms. Int Arch Occup Environ Health 81(6):711–719. https://doi.org/10.1007/s00420-007-0243-7
Krane L, Johnsen R, Fleten N et al (2014) Sickness absence patterns and trends in the health care sector: 5-year monitoring of female municipal employees in the health and care sectors in Norway and Denmark. Hum Resour Health 12:37. https://doi.org/10.1186/1478-4491-12-37
Ervasti J, Mattila-Holappa P, Joensuu M et al (2017) Predictors of depression and musculoskeletal disorder related work disability among young, middle-aged, and aging employees. J Occup Environ Med 59(1):114–119. https://doi.org/10.1097/JOM.0000000000000921
Statistics Sweden (2018) Labour Force Surveys (LFS) 2018. https://www.scb.se/hitta-statistik/statistik-efter-amne/arbetsmarknad/arbetskraftsundersokningar/arbetskraftsundersokningarna-aku/#_Tabellerochdiagram
Virtanen P, Siukola A, Lipiainen L et al (2017) Trajectory analyses of sickness absence among industrial and municipal employees. Occup Med (Lond) 67(2):109–113. https://doi.org/10.1093/occmed/kqw104
Lidwall U, Marklund S (2006) What is healthy work for women and men?—A case-control study of gender- and sector-specific effects of psycho-social working conditions on long-term sickness absence. Work 27(2):153–163
Hussey L, Turner S, Thorley K et al (2012) Work-related sickness absence as reported by UK general practitioners. Occup Med (Lond) 62(2):105–111. https://doi.org/10.1093/occmed/kqr205
Scott PG, Falcone S (1998) Comparing public and private sector organizations: an exploratory analysis of three frameworks. Am Rev Public Adm 28:126–146. https://doi.org/10.1177/027507409802800202
Macklin D, Smith L, Dollard M (2007) Public and private sector work stress: workers compensation, levels of distress and job satisfaction, and the demand-control-support model. Aust J Psychol 58(3):130–143
Silva-Junior JS, Fischer FM (2014) Long-term sickness absence due to mental disorders is associated with individual features and psychosocial work conditions. PLoS ONE 9(12):e115885. https://doi.org/10.1371/journal.pone.0115885
Social Insurance Agency (2018) Social insurance report 2018. https://www.forsakringskassan.se/wps/wcm/connect/5b9d37a9-a56d-4453-896f-fed299534d91/socialforsakringsrapport-2018-2.pdf?MOD=AJPERES&CVID. Accessed 05 Jan 2021
Rantonen O, Alexanderson K, Pentti J et al (2017) Trends in work disability with mental diagnoses among social workers in Finland and Sweden in 2005–2012. Epidemiol Psychiatr Sci 26(6):644–654. https://doi.org/10.1017/S2045796016000597
Leinonen T, Viikari-Juntura E, Husgafvel-Pursiainen K et al (2018) Cause-specific sickness absence trends by occupational class and industrial sector in the context of recent labour market changes: a Finnish panel data study. BMJ Open 8(4):e019822. https://doi.org/10.1136/bmjopen-2017-019822
Pekkala J, Blomgren J, Pietilainen O et al (2017) Occupational class differences in diagnostic-specific sickness absence: a register-based study in the Finnish population, 2005–2014. BMC Public Health 17(1):670. https://doi.org/10.1186/s12889-017-4674-0
Ervasti J, Vahtera J, Pentti J et al (2013) Depression-related work disability: socioeconomic inequalities in onset, duration and recurrence. PLoS ONE 8(11):e79855. https://doi.org/10.1371/journal.pone.0079855
Sumanen H, Lahelma E, Pietilainen O et al (2017) The magnitude of occupational class differences in sickness absence: 15-year trends among young and middle-aged municipal employees. Int J Environ Res Public Health. https://doi.org/10.3390/ijerph14060625
Ludvigsson JF, Svedberg P, Olen O et al (2019) The longitudinal integrated database for health insurance and labour market studies (LISA) and its use in medical research. Eur J Epidemiol 34(4):423–437. https://doi.org/10.1007/s10654-019-00511-8
Thell M (2015) Rekommenderad indelning av arbetare och tjänstemän utifrån SSYK kod [Recommended identification of blue and white collar workers, based on SSYK code]. Statistics Sweden: Yrkesregistret, Stockholm
Eurostat (2008) NACE Rev. 2. Statistical classification of economic activities in the European community
Stansfeld SA, Pike C, McManus S et al (2013) Occupations, work characteristics and common mental disorder. Psychol Med 43(5):961–973. https://doi.org/10.1017/S0033291712001821
Mastekaasa A (2014) The gender gap in sickness absence: long-term trends in eight European countries. Eur J Public Health 24(4):656–662. https://doi.org/10.1093/eurpub/cku075
Virtanen M, Kawachi I, Oksanen T et al (2011) Socio-economic differences in long-term psychiatric work disability: prospective cohort study of onset, recovery and recurrence. Occup Environ Med 68(11):791–798. https://doi.org/10.1136/oem.2010.061101
Melchior M, Krieger N, Kawachi I et al (2005) Work factors and occupational class disparities in sickness absence: findings from the GAZEL cohort study. Am J Public Health 95(7):1206–1212. https://doi.org/10.2105/AJPH.2004.048835
Kristensen TR, Jensen SM, Kreiner S et al (2010) Socioeconomic status and duration and pattern of sickness absence. A 1-year follow-up study of 2331 hospital employees. BMC Public Health 10:643. https://doi.org/10.1186/1471-2458-10-643
Kosidou K, Dalman C, Lundberg M et al (2011) Socioeconomic status and risk of psychological distress and depression in the Stockholm public health cohort: a population-based study. J Affect Disord 134(1–3):160–167. https://doi.org/10.1016/j.jad.2011.05.024
Dohrenwend BP, Levav I, Shrout PE et al (1992) Socioeconomic status and psychiatric disorders: the causation-selection issue. Science 255(5047):946–952. https://doi.org/10.1126/science.1546291
Goodman A, Joyce R, Smith JP (2011) The long shadow cast by childhood physical and mental problems on adult life. Proc Natl Acad Sci USA 108(15):6032–6037. https://doi.org/10.1073/pnas.1016970108
McLeod JD, Fettes DL (2007) Trajectories of failure: the educational careers of children with mental health problems. AJS 113(3):653–701. https://doi.org/10.1086/521849
Mittendorfer-Rutz E, Hensing G, Westerlund H et al (2013) Determinants in adolescence for adult sickness absence in women and men: a 26-year follow-up of a prospective population based cohort (Northern Swedish cohort). BMC Public Health 13:75. https://doi.org/10.1186/1471-2458-13-75
Björkenstam E, Helgesson M, Gustafsson K et al (2021) Occupational class and employment sector differences in common mental disorders: a longitudinal Swedish cohort study. Eur J Public Health. https://doi.org/10.1093/eurpub/ckab091
Aagestad C, Tyssen R, Sterud T (2016) Do work-related factors contribute to differences in doctor-certified sick leave? A prospective study comparing women in health and social occupations with women in the general working population. BMC Public Health 16:235. https://doi.org/10.1186/s12889-016-2908-1
Funding
Open access funding provided by Karolinska Institute. This work was supported by a research grant from AFA Insurance (Grant No. 180290).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethics approval
Approved by the ethical committee in Stockholm, Sweden (dnr: 2016/1533–32).
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Björkenstam, E., Helgesson, M., Gustafsson, K. et al. Sickness absence due to common mental disorders in young employees in Sweden: are there differences in occupational class and employment sector?. Soc Psychiatry Psychiatr Epidemiol 57, 1097–1106 (2022). https://doi.org/10.1007/s00127-021-02152-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-021-02152-3