Abstract
Purpose
Examine to what extent adults affected by recent potentially traumatic events (PTE) with different PTSD-symptom levels are more at risk for post-event loneliness than non-affected adults are in the same study period.
Methods
We extracted data from the Dutch longitudinal LISS panel to measure pre-event loneliness (2011) and post-event loneliness (2013 and 2014), pre-event mental health problems (2011), PTE and PTSD symptoms (2012). This panel is based on a traditional random sample drawn from the population register by Statistics Netherlands.
Results
Results of the multinomial logistic regression analyses showed that affected adults with high levels of PTSD symptoms were more at risk for high levels of post-event loneliness than affected adults with very low PTSD-symptom levels and non-affected adults, while controlling for pre-event loneliness, pre-event mental health problems and demographics. However, affected adults with very low levels of PTSD symptoms compared to non-affected adults were less at risk for medium and high levels of post-event loneliness while controlling for the same variables. Yet, pre-event loneliness appeared to be the strongest independent predictor of loneliness at later stages: more than 80% with high pre-event levels had high post-event levels at both follow-ups.
Conclusions
Remarkably, potentially traumatic events have depending on PTSD-symptom levels both negative and positive effects on post-event loneliness in favor of affected adults with very low PTSD symptoms levels. However, post-event levels at later stages are predominantly determined by pre-event loneliness levels.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The adverse effects of potentially traumatic events on (mental) health such as (traffic) accidents, (intimate partner) violence, life-threatening diseases, (sudden) death of a significant other and disasters are well-documented nowadays. Affected adults may suffer from various post-event stress symptoms such as fear and anxiety, grief and sadness, frustrations and anger, pain, cardiovascular problems, sleep problems and fatigue in the short, medium and long term. A variable minority suffer from mental disorders such as acute stress disorder, major depression and posttraumatic stress disorder [1,2,3,4,5,6,7,8]. However, the consequences of potentially traumatic events (PTE) are not restricted to (severe) (mental) health problems. PTE may affect other important resource in life such as safety and justice, work and income, social networks and relationships that may cause stress and negatively affect well-being. Importantly, each year a significant minority of the adults is confronted with PTE [9, 10].
People affected by PTE strive to restore important resources lost [11, 12]. To a certain degree, they possess the capability to manage one’s personal functioning in the myriad of environmental demands of the aftermath of PTE, also depending on the consequences of the PTE. Coping self-efficacy levels of the affected may help to reduce sources of stress and stress symptoms [13,14,15]. The presence of help and support from family, friends, colleagues, peers as well as involved professionals may further help to reduce both sources of stress as well as stress symptoms. Higher levels of perceived social support, and especially emotional support, are associated with lower levels of mental health problems in general and post-event mental health problems such as PTSD-symptomatology [16,17,18,19]. However, on the long term (persistent) problems and how people cope with them may reduce support [18, 20,21,22].
Therefore, loneliness will likely hinder post-event recovery efforts. Post-event experiences of unpleasant or inadmissible lack of (quality of) certain relationships [23] could increase the risk for ongoing severe posttraumatic stress symptoms. Non-trauma studies in the past decades have shown that loneliness, i.e. the subjective feeling referring to the perceived inadequacy of one’s social relationships [23,24,25,26,27,28], is clearly negatively associated with health. In a recent overview of 40 systematic reviews and meta-analysis of studies on the health consequences of loneliness, Leigh-Hunt et al. [29] concluded that there is consistent evidence linking loneliness to increased all-cause mortality, worse mental health and negative cardiovascular outcomes.
An important question in this perspective is to what extent potentially traumatic events (PTE) and PTE-related symptoms contribute to post-trauma loneliness. Insight in these factors may help to develop and target post-event mental health policies and interventions, to reduce or prevent loneliness. To date, many correlations of loneliness have been identified varying from employment to low self-esteem [25, 26, 28], but a limited number of studies focussed on PTE and related symptoms as predictors of loneliness.
For example, Hawthorne [30] assessed the association between lifetime trauma exposure and social isolation, a concept strongly related to loneliness [31]. In this cross-sectional study, Australian adults with three or more lifetime trauma exposures were more at risk for current social isolation than those with two or less. However, when current depression disorders were added to the list of eight predictors of social isolation, lifetime exposure was not an independent predictor. The results of the cross-sectional study of Palgi et al. [32] partly differ from the study of Hawthorne [30]. They showed that lifetime potential traumatic events among older US adults were positively related to loneliness. Adults with two or more lifetime events were more at risk for loneliness than adults without these experiences, while current depressive symptoms were taken into account too. In a cross-sectional study among older US veterans of Kuwert et al. [33], the number of lifetime traumatic events, current PTSD and depression symptoms were significantly associated with current loneliness over and above other variables, such as demographics and support. The cross-sectional study of Lasgaard et al. [34] demonstrated that having a life-threatening somatic condition was an independent risk factor for both moderate and severe loneliness over and above a list of demographic, work- and health-related variables. However, recalled lifetime trauma exposure or events may be sensitive to recall bias, influencing the strength of the associations between both [35, 36]. One of the exceptions, among others, is becoming a widow. The possible effects of being a widow was assessed in the large cross-sectional study of Victor et al. [37] among older people in Great Britain. It showed that widowed compared to married persons were more at risk for loneliness, over and above for (recalled) changes in loneliness in past 10 years, health and other variables.
Solomon et al. [38] conducted a three-wave post-war study among Israeli veterans covering a period of 20 years. Findings showed that loneliness levels were higher at all waves among veterans with combat stress reaction (CSR; succumb to stress and suffer a psychic breakdown on the battlefield) compared to soldiers without CSR. Baseline PTSD symptom levels did not predict future loneliness levels, although they were significantly related on a cross-sectional level. The two-wave study of Cohen-Mansfield et al. [39] among older persons in Israel showed that the number of lifetime traumatic events were independently associated with loneliness at the first wave, especially among married persons, over and above demographics, health variables and social network variables. However, lifetime traumatic events were not associated with becoming lonely in the period of 3.5 years between both waves in contrast to poorer health.
These findings suggest that potentially traumatic events as well as post-event posttraumatic stress symptoms, besides pre-event mental health, may increase the risk for post-event loneliness in the short and medium term. However, it is unclear to what extent these variables remain significant predictors of post-event loneliness when pre-event loneliness is taken into account. For instance, in the longitudinal study of Cacioppo et al. [40], loneliness among older people in the US was relatively stable over a period of 3 years, and loneliness at baseline appeared to be a significant, strong and dominant independent predictor of loneliness at follow-ups compared to, although also significant predictors, social support and depression symptoms at baseline. In addition, in their systematic review of 54 prospective longitudinal studies of PTSD, DiGangi et al. [41] came to the worrying conclusion that many variables, previously considered outcomes of trauma, are pre-trauma risk factors. These findings underscore the necessity of, when studying the effects of trauma on loneliness, prospective longitudinal study designs with pre-trauma measures on loneliness. However, to the best of our knowledge, to date such studies are absent.
Aim of the present study is assess to what extent potentially traumatic events and posttraumatic stress predict post-trauma loneliness using such a rigorous prospective study design, with pre-event and post-event measures of loneliness and a comparison group of non-affected adults. Main research questions are: (a) to what extent are adults affected by a PTE and subgroups with low to high levels of posttraumatic stress symptom more at risk for loneliness at later stages than non-affected adults? And (b) do affected adults with low levels of posttraumatic stress symptom differ from affected adults with higher levels of symptoms in post-event loneliness?
Based on the outcomes of previous studies on predictors of loneliness, we controlled for the possible effects of pre-event mental health, pre-event loneliness, age, gender, having a partner, and education level. We focus on relatively recent acute potentially traumatic events that assessed the predictive values for loneliness at two follow-ups with a 1-year interval.
Methods
Procedures and participants
CentERdata (Tilburg, the Netherlands) operates the Longitudinal Internet Studies for the Social Sciences-panel (LISS-panel) starting in 2007 [42]. This panel, based on a traditional random sample drawn from the population register by Statistics Netherlands, consists of about 7000 individuals with a yearly attrition rate of about 10%. They are frequently invited to complete online surveys (more information about the LISS-panel and how to gain free access can be found in English at: http://www.lissdata.nl). There are several so-called core studies that are repeated each year in the same period (with a few exceptions), such as the core studies on health that are conducted each year November–December.
Proposals for studies, such as the studies on trauma we included in the present study (see below), are first evaluated by the Board of Overseers, the Internal Review Board. During the recruitment of the panel, respondents who agreed to participate in the panel received a confirmation e-mail, and a letter with login code. With the login code provided, they could confirm their willingness to participate and immediately start the first interview (i.e. double consent was ensured, for details see [43]).
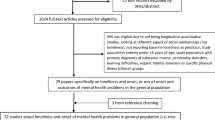
Using this panel, in 2012 three surveys on trauma were conducted (T2a, Aprilresponse = 78.4%; T2b, Augustresponse = 83.5%, T2c, Decemberresponse = 86.3%) [14, 43]. In total, 4857 respondents participated in all three surveys on trauma and their data was extracted for this study. We also extracted data from studies on Social Integration and Leisure to obtain data on pre- and post-event loneliness, that were conducted in the spring of 2011 (T1a, February–Marchresponse = 63.1%), 2013 (T3, February–Marchresponse = 86.0%), and of 2014 (T4, February–Marchresponse = 86.0%). To obtain data on pre-event mental health problems, we extracted data from a survey on health conducted at the end of 2011 (T1b, November–December 2011, response = 77.2%). In total, 3244 respondents participated in these seven surveys.
We next made a distinction between by PTE’s affected respondents and comparison respondents not confronted with PTE’s or other life events in the 2 years before T2a and not between T2a and T2c (Nno PTE = 1513; questions on PTE see below). With respect to the affected respondents, we also excluded respondents confronted with PTE’s in the 2 years before T2a to ascertain that they (also) were not confronted with PTE’s about a year before T1, or between T1 and T2a. We finally selected respondents confronted with a PTE between T2a and T2b, and/or between T2b and T2c (ntotal PTE = 285).
Variables
Loneliness
Pre- and post-event loneliness was assessed at T1a, T3 and T4 using the six-item De Jong Gierveld Loneliness Scale [44]. Respondents are asked to rate items such as ‘I often feel deserted’ and ‘there are enough people I can count on in case of a misfortune’ on three-point Likert scales (1 = yes, 2 = more or less, 3 = no). For the present study, we calculated the total score after recoding the three negative formulated items (0.76 ≤ Cronbach’s Alpha’s ≤ 0.81 across 3 loneliness assessments). For the present study, we calculated the total score after recoding the three negative formulated items, but we did not use the prior dichotomization of the answer categories [45]. The reason was that the total score scale of loneliness without prior dichotomization enabled the categorization of sub groups with different levels of loneliness with almost equal cell counts somewhat better [Spearman’s rank (rho) correlation between scales with and without prior dichotomization is 0.99]. According to the cut-offs of the manualFootnote 1 about 10% (n = 176) had severe loneliness scores.
Mental health problems
Pre-event mental health problems were examined at T1b using the Mental Health Index or Inventory (5-item sub scale of the MOS 36-item short-form health survey) [46, 47]. Respondents were asked to rate their mental health during the past month on six-point Likert scales, such as ‘This past month I felt very anxious’ and ‘I felt depressed and gloomy’ (1 = never, 2 = seldom, 3 = sometimes, 4 = often, 5 = mostly, 6 = continuously). After recoding the third and fifth item, the total scores were computed (Cronbach’s Alpha = 0.84).
Potentially traumatic events
Confrontations with potentially traumatic events were examined at T2a, T2b and T2c. Respondents were administered a list of ten potentially traumatic events [i.e.: serious threat(s); physical violence; robbery; traffic accident; airplane incident; fire; burglary; serious infection/contamination such as HIV, legionella, poison; sexual violence/abuse; death of significant other/colleague] and an open question with regard to having experienced another potentially traumatic event in the past 2 years not listed that were recoded afterwards [14, 43]. In case respondents were confronted with more than one event in the past 2 years, they were asked to focus on the most drastic event (1 = 1 week ago, 2 = 2 weeks ago, 3 = 3 weeks ago, 4 = 4 weeks ago, 5 = 1–2 months ago, 6 = 3–4 months ago, 7 = 5–6 months ago, 8 = 7–12 months ago, 9 = more than 1 year ago). In case respondents reported life events that cannot be considered PTE (such as conflicts in the family, job loss) and were not confronted with PTE, they were excluded from the analyses.
Posttraumatic stress symptoms
To assess PTSD-symptom severity (DSM-IV), the 15-item impact of event scale (IES) [48, 49] assessing intrusion and avoidance reactions during the past week was administered at T2c. In addition, the seven hyper arousal items from the IES-R [50] were added while the original scoring system of the IES was retained. This approach has been used in previous research [15] and has the benefit of comparability with results obtained using the original IES, while still allowing for the measurement of all three symptom clusters (avoidance, re-experiencing, hyper arousal) of PTSD (DSM-IV). Factor analysis confirmed the general three-factor structure [15]. Affected respondents were asked, while taking (the most recent) potential traumatic event in mind, to rate items such as: during the past week ‘I thought about it when I did not mean to’ or ‘I stayed away from reminders of it’ and ‘I had trouble concentrating’ on four-point Likert sales (0 = not at all, 1 = rarely, 3 = sometimes, 5 = often). We call this instrument the IESplus (Cronbach’s Alpha = 0.94).
In Fig. 1, we have presented a graphical overview of the surveys and the nature of the assessments (main topics).
Data analysis
For the present study, several total scores were recoded. Because of the skewness loneliness scores at T1a, T3 and T4 (for instance SkewnessT1a = 1.494, SE Skewness = 0.058), scores were recoded (based on T1a data) into relatively high (6 thru 15; 30.5%), medium (16, 17; 30.6%) and low levels of loneliness (18; 38.9%). With respect to PTE and posttraumatic stress reactions five PTE groups were composed:
-
1.
Respondents without PTE (not in 2 years before T2a, and not between T2a and T2c);
-
2.
Affected respondents with very low PTSD-symptom levels (PTE between T2a and T2c, and IESplus ≤ 5);
-
3.
Affected respondents with low PTSD-symptom levels (PTE between T2a and T2c, and 6 ≤ IEplus ≤ 17);
-
4.
Affected respondents with medium PTSD-symptom levels (PTE between T2a and T2c, and 18 ≤ IEplus ≤ 40); and
-
5.
Affected respondents with high PTSD-symptom levels (PTE between T2a and T2c, and IEplus ≥ 41).
The range of IESplus scores in subgroups 2–5 were chosen to obtain more or less equal numbers of respondents in each subgroup as much as possible, although this categorization is somewhat arbitrary.
The total scores of mental health problems (MHP) were divided into three levels with a more or less equal numbers of respondents: i.e. relatively low (5–8; 32.7%), medium (9–11; 34.3%), and high levels of MHP (12–hi; 33.0%) to be able to present results in the tables in a uniform way.
Because the dependent variables had three values (low, medium, high), multivariate multinomial logistic regression (MMLR) analyses were conducted with pre-event loneliness/satisfaction at T1a (2011), mental health problems at T1b (2011), PTE group membership (T2c, 2012) and as predictors. Age, gender, having a partner and education level were also added as predictors. As such, the MMLR analyses assessed to what extent the aforementioned variables predict (a) medium levels of loneliness/satisfaction at T3 (medium versus low) and (b) predict high levels of loneliness/satisfaction at T3 (high versus low).
Results
The characteristics of the affected and non-affected respondents are presented in Table 1. According to chi-squared tests, the groups did not significantly differ on any variable of Table 1. Of the affected, 27 (9.5%) were confronted with violence/crime, 30 (10.5%) with accidents/disasters, 226 (79.3%) with the death significant other, and 6 (2.1%) with various PTE (such as suicide). In addition, 85 (29.8%) reported very low PTSD-symptom levels, 69 (24.2%) low PTSD-symptom levels, 80 (28.1%) medium PTSD-symptom levels, and 51 (17.9%) high PTSD-symptom levels.
Analyses among total study sample of affected and non-affected respondents
The main results of the MMLR analyses are presented in Table 2. The complete tables can be obtained from the first author.
Table 2 shows that pre-event levels of loneliness (2011) were the strongest significant independent predictors for loneliness at T3 and T4. Analyses among those with low or medium levels of loneliness at T3 (2013) showed that the group with medium levels of loneliness at T1a (2011) had significant more often medium levels at T3 compared those with low levels of loneliness at T1a (2011). With respect to those with low or high levels of loneliness at T3 (2013), respondents with high pre-event levels of loneliness at T1a (2011) had significantly more often had high post-event levels of loneliness at T3 (2013) than those with low loneliness levels at T1a (2011). Table 2 shows the same pattern with respect to the prediction of loneliness at 2014 (T4).
Within the group of respondents with low or medium levels of loneliness at T3 (2013), affected respondents with very low PTSD-symptom levels compared to non-affected respondents significantly less often had medium levels of loneliness at T3 (2013). The same analyses among those with low or high levels of loneliness at T3 (2013) showed a similar result: affected respondents with low PTSD-symptom scores had significant less high loneliness levels at T3 (2013) than the non-affected respondents. However, there was a statistical trend (0.05 ≤ p < 0.10) that affected respondents with high levels of PTSD symptoms (n = 36) more often had high levels of loneliness than non-affected respondents. The other affected groups did not differ significantly from non-affected respondents.
A similar pattern was found predicting loneliness at T4 (2014), although affected respondents with high PTSD-symptom levels more often had high levels of loneliness than non-affected respondents at T4 (2014). The affected respondents with very low PTSD-symptom levels did not have significantly less high levels of loneliness compared to non-affected respondents. Table 2, furthermore, shows that pre-event mental health problems were independent significant predictors for post-event loneliness at both follow-ups. For instance, among those with low or high loneliness levels at T3 (2013), respondents with high pre-event levels of mental health problems more often had high levels of post-event loneliness at both follow-ups than those with low pre-event levels of mental health problems.
Analyses among the affected respondents only
To assess differences between sub groups of affected residents, the MMLR analyses were repeated among this sub-group (n = 283) with the affected respondents with very low levels of PTSD-symptoms as reference group. Finding are presented in Table 3. Affected respondents with high PTSD-symptom levels more often had medium levels of loneliness at T3 (2013) than those with very low levels of PTSD-symptoms. In addition, they more often had high levels of loneliness at T3 (2013) and T4 (2014).
Additional and identical analyses with being affected (PTE is yes or no) as predictor instead of the five categories based on PTE and PTSD-symptoms showed that PTE did not significantly (p < 0.05) and independently predict post-event loneliness at both follow-ups (data not shown).
Discussion
Aim of the present study was to examine to what extent adults affected by potentially traumatic events (PTE) with different levels of posttraumatic stress symptom are more at risk for post-event loneliness at different post-event stages than non-affected adults, while taking pre-event loneliness and pre-event mental health problems into account.
Main findings
Remarkably, we found both negative as well as positive effects of PTE and PTSD symptoms on post-event loneliness.
The results of the multivariate multinomial logistic regression analyses showed that affected respondents with high levels of PTSD-symptoms were more at risk for relatively high levels of loneliness at the second follow-up than non-affected respondents. There was a statistical trend that they were also more at risk for high levels of loneliness at the first survey than non-affected. However, with respect to the prediction of high levels of loneliness no significant differences were found between non-affected at the one side and affected respondents with low and medium levels of PTSD-symptoms on the other side. In addition, respondents with different levels of posttraumatic stress symptoms were not more at risk for medium levels of loneliness than non-affected respondents at both follow-ups. However, in line with previous research on loneliness and social support [40, 51, 52], pre-event loneliness appeared to be a strong predictor of post-event loneliness at both follow-ups.
Pre-event mental health problems were also clearly associated with loneliness at follow-ups: existing mental health problems were a risk factor for loneliness about one and two years later. The analyses among the affected respondents revealed that, in contrast to, for example, the study of Solomon et al. [38], affected adults with very low PTSD-symptom levels were less at risk for high levels of loneliness at both follow-ups than affected respondents with high levels of PTSD-symptoms. Moreover, the affected respondents with very low levels of PTSD-symptoms were less at risk for medium and high levels of loneliness than non-affected respondents at the first follow-up and less at risk for medium levels of loneliness at the second follow-up.
Social causation
How can these contrasting negative and positive findings be explained? Kaniasty and Norris [53] showed two causal pathways in which social support and PTSD-symptoms could influence each other, specifically social causation and the social selection. In social causation, the lack of social support will increase the chances for the development of PTSD-symptoms at later stages, but in social selection higher PTSD-symptom levels will decrease social support at later stages. The outcomes of the comparisons between affected respondents with very low levels of PTSD-symptoms and affected residents with high levels of PTSD-symptoms are in line with the social selection perspective: higher PTSD-symptom levels were predictive of higher loneliness levels [54]. The positive association between pre-event mental health problems and higher post-event perceived loneliness also points to the presence of social selection.
Our results are also in line with the cognitive model of Ehlers and Clark [20]. Victims suffering from PTSD symptoms may appraise their situation as very negative and see their reactions to the event as indicators that they have changed for the worst, and not that their reaction are part of a normal process. This may lead to social withdrawal and therefore higher levels of loneliness. An important element in this process is the response of family, friends and colleagues. They may find it difficult to respond because of the PTE persons experienced and especially their posttraumatic stress symptoms, and therefore avoid talking about experiences and problems. This is also expressed by associations between PTSD and, among others, social anxiety and family problems [55].
Our finding that affected residents with very low PTSD-symptom levels were even less lonely that non-affected residents may also fit in the cognitive model Ehlers and Clark [20]. A possible explanation in this perspective is that victims experienced a potential traumatic event but because of the absence of mild or severe PTSD-symptoms these problems no longer form a barrier making it more convenient for family and friends to respond, talk about it, and provide recognition resulting in a decrease in loneliness. Future longitudinal research is warranted to confirm (or reject) our findings and explanation that PTE in the absence of mild-severe PTSD-symptoms decrease loneliness. However, these results and the social selection perspective do show support that PTSD interventions directed towards more severe PTSD symptomology could benefit from addressing social functioning problems.
Limitations and strengths
Several characteristics and limitations need to be discussed. The prospective comparative design to assess the effects of PTE and PTSD-symptoms on post-event loneliness can be considered a major strength of our study. We excluded respondents that were affected by PTE in the past 2 years, to ascertain as much as possible that findings were not biased by previous events and their possible effects on loneliness. Comparisons between affected and non-affected showed that pre-event loneliness levels as well as pre-event mental health problems were similar between both groups (as well as demographic characteristics). To the best of our knowledge, to date no study assessed the effects of PTE and PTSD-symptoms using such a rigorous study design. We examined the effects of recent potentially traumatic events. We did not examine the effects of events experiences during childhood, such as child sexual abuse and childhood physical abuse [56].
We used well-validated questionnaires to examine mental health problems, loneliness, and posttraumatic stress symptoms. We did not conduct clinical interviews to assess posttraumatic stress disorder that would have enriched our study. In addition, although social support and loneliness are related concepts, we have no data on either pre- or post-event social support. We assessed the predictive values of PTE and PTSD-symptoms for loneliness at two follow-ups with a 1-year time interval, and focused on the effects of relatively recent PTE. Future research should focus on the long-term effects of PTE and PTSD symptoms on loneliness, and the possible effects of re-victimization and child abuse on loneliness.
There was a gap of about 3 months between the measurement of (pre-event) mental health (T1a) and (pre-event) loneliness (T1b). However, since previous research has shown that these mental health problems are rather stable [57], we do not expect that this gap influenced our findings. There was also a gap of about 2–3 months between the PTSD-symptomatology (T2c) and the second or post-event loneliness assessment (T3). The last loneliness assessment (T4) took place 1 year later. We have no information about confrontations with PTE after the last PTE examination (December 2012) and these events and/or related PTSD-symptomatology may have weakened associations, especially with respect to last follow-up assessment of loneliness (T4).
Another possible explanation of the absence of large differences between non-affected and affected people with relatively high levels of PTSD symptoms is an underreporting of loneliness among these affected respondents because of the negative (emotional) connotation of loneliness. However, to prevent this problem the De Jong Gierveld Loneliness Scale was constructed without using the word loneliness, although items are directly related to the conceptual ideas of loneliness, [25]. For this reason, we consider this explanation not very plausible.
Finally, a previous study [57], using the LISS panel including the surveys on trauma, has shown that the non-response did not or hardly affect the mental health scores: “Those participating in 1, 2, 3, 4, 5, 6 or 7 surveys did not differ on three of the four health variables. The significant differences in mental health between those participating in 7 surveys and other groups were (very) small according to Cohens D and did not show a clear pattern (p. 469)”.
Implications for further research
It was outside the aim of the present study to assess differences between pre-event situational versus pre-event chronic loneliness, besides the fact that numbers of affected respondents in our study were too low to analyze possible differences. However, in future research this distinction may be relevant given the results of for instance the longitudinal study of Shiovitz-Ezra and Ayalon [58]. Both situationally, loneliness and chronic loneliness were associated with a greater risk for all-cause mortality when controlled for demographics and health confounders, but chronic loneliness was a stronger predictor.
The study of Fokkema et al. [59] revealed differences in loneliness levels between older adults of 14 EU countries, while controlling for demographics, health, social embeddedness and support exchange. In addition, Koenen et al. [60] showed that, based on a comparison of 26 population WHO World Mental Health Surveys, lifetime and 12-month prevalence of PTSD differed between countries. Therefore, future prospective research is needed among population-based samples in other countries to assess the influence of country or context differences and strengths of associations between potential traumatic events, PTSD symptomatology and loneliness.
The finding that victims with high levels of PTSD-symptoms are more at risk for high levels of loneliness than non-affected adults and PTE affected adults with low levels of PTSD raises the question how this risk can be prevented or reduced. Two recent reviews, however, not specifically aimed at trauma, are of relevance here. The review of Mann et al. [61] on interventions to reduce loneliness demonstrated that, although ‘changing cognitions’ had the most promising emerging evidence according to the authors, no interventions had robust evidence. The review of Webber and Fendt-Newlin [62] on the effects of social participation interventions for people, including those provided by mental health services, with mental health problems concluded “A wide range of approaches are used to help improve the social participation of people with mental health problems, though evidence of their effectiveness is minima (p.)”. These results indicate that further research on interventions is needed to address this problem in general and specifically with respect to potential traumatic events.
Finally
In either way, the paramount role of pre-event loneliness suggests that post-event social problems might be rooted in a wider context of social dysfunction of the affected individual, rather than to be directly induced by the traumatic experience. In either way, the paramount role of pre-event loneliness suggests that for the early identification of those at risk for post-event social problems, the assessment of pre-event loneliness should be included.
Change history
08 March 2018
In the original article, Tables 2 and 3 have published with incorrect alignment. The correct tables are given below. The original article was corrected.
References
Abbey G, Thompson SB, Hickish T, Heathcote D (2015) A meta-analysis of prevalence rates and moderating factors for cancer-related post-traumatic stress. Disord Psychooncol 24:371–381. https://doi.org/10.1002/pon3654
Birkley EL, Eckhardt CI, Dykstra RE (2016) Posttraumatic stress disorder symptoms, intimate partner violence, and relationship functioning: a meta-analytic review. J Trauma Stress 29:397–405. https://doi.org/10.1002/jts22129
Bryant RA, Friedman MJ, Spiegel D, Ursano R, Strain J (2011) A review of acute stress disorder in DSM-5. Depress Anxiety 28:802–817. https://doi.org/10.1002/da.20737
Christiansen DM (2017) Posttraumatic stress disorder in parents following infant death: a systematic review. Clin Psychol Rev 51:60–74. https://doi.org/10.1016/jcpr201610007
Kristensen P, Weisæth L, Heir T (2012) Bereavement and mental health after sudden and violent losses: a review. Psychiatry 75:76–97. https://doi.org/10.1521/psyc20127517
Neria Y, Nandi A, Galea S (2008) Post-traumatic stress disorder following disasters: a systematic review. Psychol Med 38:467–480 https://doi.org/10.1017/S0033291707001353
Rona RJ, Burdett H, Bull S, Jones M, Jones N, Greenberg N, Wessely S, Fear NT (2016) Prevalence of PTSD and other mental disorders in UK service personnel by time since end of deployment: a meta-analysis. BMC Psychiatry. https://doi.org/10.1186/s12888-016-1038-8
Rytwinski NK, Scur MD, Feeny NC, Youngstrom EA (2013) The co-occurrence of major depressive disorder among individuals with posttraumatic stress disorder: a meta-analysis. J Trauma Stress 26:299–309. https://doi.org/10.1002/jts21814
Darves-Bornoz JM, Alonso J, de Girolamo G et al (2008) Main traumatic events in Europe: PTSD in the European study of the epidemiology of mental disorders survey. J Trauma Stress 21:455–462. https://doi.org/10.1002/jts20357
Hentschel S, Eid M, Kutscher T (2016) The influence of major life events and personality traits on the stability of affective well-being. J Happiness Stud 2016 18:719–741. https://doi.org/10.1007/s10902-016-9744-y
Hobfoll SE (1989) Conservation of resources a new attempt at conceptualizing stress. Am Psychol 44:513–524 https://doi.org/10.1037/0003-066X443513
Hobfoll SE (2002) Social and psychological resources and adaptation. Rev Gen Psychol 6:307–324. https://doi.org/10.1037//1089-268064307
Benight CC, Bandura A (2004) Social cognitive theory of posttraumatic recovery: the role of perceived self-efficacy. Behav Res Ther 42:1129–1148. https://doi.org/10.1016/j.brat.2003.08.008
Bosmans MWG, van der Velden PG (2015) Longitudinal interplay between posttraumatic stress symptoms and coping self-efficacy: a four-wave prospective study. Soc Sci Med 134:23–29. https://doi.org/10.1016/j.socscimed.2015.04.007
Luszczynska A, Benight CC, Cieslak R (2009) Self-efficacy and health-related outcomes of collective trauma: a systematic review. Eur Psychol 14:51–62. https://doi.org/10.1027/1016-9040.14.1.51
Johnson JG, Cohen P, Dohrenwend BP, Link BG, Brook JS (1999) A longitudinal investigation of social causation and social selection processes involved in the association between socioeconomic status and psychiatric disorders. J Abnorm Psychol 108:490–499. https://doi.org/10.1037/0021-843x1083490
Kaniasty K, Norris FH (2008) Longitudinal linkages between perceived social support and posttraumatic stress symptoms: sequential roles of social causation and social selection. J Trauma Stress 21:274–281. https://doi.org/10.1002/jts.20334
Kaniasty K, Norris FH (1992) Social support and victims of crime: Matching event, support, and outcome. Am J Comm Psychol 20:211–241 https://doi.org/10.1007/bf00940837
Platt JM, Lowe SR, Galea S, Norris FH, Koenen KC (2016) A Longitudinal study of the bidirectional relationship between social support and posttraumatic stress following a natural disaster. J Trauma Stress 29:205–213. https://doi.org/10.1002/jts.22092
Ehlers A, Clark DM (2000) A cognitive model of posttraumatic stress disorder. Behav Res Ther 38:319–345. https://doi.org/10.1016/S0005-7967(99)00123-0
Laffaya C, Cavella S, Drescher K, Rosen C (2008) Relationships among PTSD symptoms, social support, and support source in veterans with chronic PTSD. J Trauma Stress 21:394–401. https://doi.org/10.1002/jts.20348
Shallcross S, Arbisi PA, Polusny MA, Kramer MD, Erbes CR (2016) Social causation versus social erosion: comparisons of causal models for relations between support and PTSD symptoms. J Trauma Stress 29:167–175. https://doi.org/10.1002/jts.22086
de Jong Gierveld J (1989) Personal relationships, social support, and loneliness. J Soc Pers Relat 6:197–221
Cacioppo JT, Patrick B (2008) Loneliness: human nature and the need for social connection. W.W Norton & Company, New York
de Jong Gierveld J (1998) A review of loneliness: concept and definitions, determinants and consequences. Rev Clin Gerontol 8:73–80
Ejlskov L, Wulff J, Bøggild H, Kuh D, Stafford M (2017) Assessing the relative importance of correlates of loneliness in later life Gaining insight using recursive partitioning. Aging Mental Health. https://doi.org/10.1080/13607863201713706908
Hawkley LC, Cacioppo JT (2010) Loneliness matters: a theoretical and empirical review of consequences and mechanisms. Ann Behav Med 40:218–227 https://doi.org/10.1007/s12160-010-9210-8
Heinrich LM, Gullone E (2006) The clinical significance of loneliness: a literature review. Clin Psychol Rev 26:695–718. https://doi.org/10.1016/j.cpr.2006.04.002
Leigh-Hunt N, Bagguley D, Bash K, Turner V, Turnbull S, Valtorta N, Caan W (2017) An overview of systematic reviews on the public health consequences of social isolation and loneliness. Public Health 152:157–171. https://doi.org/10.1016/j.puhe.2017.07.035
Hawthorne G (2008) Perceived social isolation in a community sample: its prevalence and correlates with aspects of peoples’ lives. Soc Psychiatry Psychiatr Epidemiol 43:140–150. https://doi.org/10.1007/s00127-007-0279-8DO
Oshagan H, Allen RL (1992) Three loneliness scales: an assessment of their measurement properties. J Pers Assess 59:380–409. https://doi.org/10.1207/s15327752jpa5902_13
Palgi Y, Shrira A, Ben-Ezra M, Shiovitz-Ezra S, Ayalon L (2012) Self- and other-oriented potential lifetime traumatic events as predictors of loneliness in the second half of life. Aging Ment Health 16:423–430. https://doi.org/10.1080/13607863.2011.638903
Kuwert P, Knaevelsrud C, Pietrzak RH (20140 Loneliness among older veterans in the United States: results from the National Health and Resilience in Veterans Study. Am J Geriatr Psychiatry 22: 564–569. https://doi.org/10.1016/j.jagp.2013.02.013
Lasgaard M, Friis K, Shevlin M (2016) “Where are all the lonely people?” A population-based study of high-risk groups across the life span. Soc Psychiatry Psychiatr Epidemiol 51:1373–1384 https://doi.org/10.1007/s00127-016-1279-3
Brewin CR (2013) Autobiographical memory for trauma: update on four controversies. Memory 15:227–248. https://doi.org/10.1080/09658210701256423
van Giezen AE, Arensman E, Spinhoven P, Wolters G (2005) Consistency of memory for emotionally arousing events: a review of prospective and experimental studies. Clin Psychol Rev 25:935–953. https://doi.org/10.1016/j.cpr.2005.04.011
Victor RC, Scambler SJ, Bowling A, Bond J (2005) The prevalence of, and risk factors for, loneliness in later life: a survey of older people in Great Britain. Aging Soc 25:357–375. https://doi.org/10.1017/S0144686X04003332
Solomon Z, Bensimon M, Greene T, Horesh D, Ein-Dor T (2015) Loneliness trajectories: the role of posttraumatic symptoms and social support. J Loss Trauma 20:1–21. https://doi.org/10.1080/15325024.2013.815055
Cohen-Mansfield J, Shmotkin D, Goldberg S (2009) Loneliness in old age: longitudinal changes and their determinants in an Israeli sample. Int Psychogeriatr 21:1160–1170. https://doi.org/10.1017/S1041610209990974
Cacioppo JT, Hughes ME, Waite LJ, Hawkley LC, Thisted RA (2006) Loneliness as a specific risk factor for depressive symptoms: cross-sectional and longitudinal analyses. Psychol Aging 21:140–151. https://doi.org/10.1037/0882-7974.21.1.140
DiGangi JA, Gomez D, Mendoza L, Jason LA, Keys CB, Koenen KC (2013) Pretrauma risk factors for posttraumatic stress disorder: a systematic review of the literature. Clin Psychol Rev 33:728–744. https://doi.org/10.1016/jcpr201305002
Scherpenzeel A, Das M (2011) True longitudinal and probability-based internet panels: evidence from The Netherlands. In: Das M, Ester P, Kaczmirek L (eds) Social and behavioral research and the internet: advances in applied methods and research strategies. Taylor & Francis, New York, pp 77–104
van der Velden PG, Bosmans MW, Scherpenzeel AC (2013) The burden of research on trauma for respondents: a prospective and comparative study on respondents evaluations and predictors. PLoS One. https://doi.org/10.1371/journal.pone.0077266
de Jong Gierveld J, van Tilburg TG (2006) A 6-item scale for overall, emotional, and social loneliness confirmatory tests on survey data. Res Aging 28:582–598. https://doi.org/10.1177/0164027506289723
de Jong Gierveld J, van Tilburg TG (1999) Manual of the loneliness scale, Department of Social Research Methodology (ISBN 90–9012523-X). VU University, Amsterdam
Means-Christensen AJ, Arnau RC, Tonidandel AM, Bramson R, Meagher MW (2005) An efficient method of identifying major depression and panic disorder in primary care. J Behav Med 28:565–572. https://doi.org/10.1007/s10865-005-9023-6
Ware JE, Sherbourne CD (1992) The MOS 36-item short-form health survey, SF-36: conceptual framework and item selection. Med Care 30:473–483
Horowitz M, Wilner N, Alvarez W (1979) Impact of event scale: a measure of subjective stress. Psychosom Med 41:209–218
van der Ploeg E, van der Mooren TT, Kleber RJ, van der Velden PG, Brom D (2004) Construct validation of the Dutch version of the impact of event scale. Psychol Assess 16:16–26. https://doi.org/10.1037/1040-3590.16.1.16
Weiss DR, Marmar CR (1997) The impact of events scale-revised. In: Wilson JP (ed) Assessing psychological trauma and PTSD. Guilford Press, New York, pp 399–411
Chan CS, Lowe SR, Weber E, Rhodes JE (2015) The contribution of pre- and postdisaster social support to short- and long-term mental health after Hurricanes Katrina: a longitudinal study of low-income survivors. Soc Sci Med 138:38–43. https://doi.org/10.1016/j.socscimed.2015.05.037
Lowe SR, Chan CS, Rhodes JE (2010) Pre-hurricane perceived social support protects against psychological distress: a longitudinal analysis of low-income mothers. J Consult Clin Psychol 78:551–560. https://doi.org/10.1037/a0018317
Kaniasty K, Norris F (2008) Longitudinal linkages between perceived social support and posttraumatic stress symptoms: sequential roles of social causation and social selection. J Trauma Stress 21:274–281. https://doi.org/10.1002/jts.20334
Clapp JD, Beck JG (2008) Understanding the relationship between PTSD and social support: the role of negative network orientation. Behav Res Ther 47:237–244. https://doi.org/10.1016/j.brat.2008.12.006
Frueh BC, Turner SM, Beidel DC, Cahill SP (2001) Assessment of social functioning in combat veterans with PTSD. Aggress Violent Beh 6:79–90. https://doi.org/10.1016/S1359-1789(99)00012-9
Shevlin M, McElroy E, Murphy J (2015) Loneliness mediates the relationship between childhood trauma and adult psychopathology: evidence from the adult psychiatric morbidity survey. Soc Psychiatry Psychiatr Epidemiol 50:591–601. https://doi.org/10.1007/s00127-014-0951-8
Velden PG van der, Bosmans MWG, Meulen van der E, Vermunt JK (2016) Pre-event trajectories of mental health and health-related disabilities, and post-event traumatic stress symptoms and health: a 7-wave population-based study. Psychiatry Res 30:246–466-473. https://doi.org/10.1016/j.psychres.2016.10.024
Shiovitz-Ezra S, Ayalon L (2010) Situational versus chronic loneliness as risk factors for all-cause mortality. Int Psychogeriatr 22:455–462. https://doi.org/10.1017/S1041610209991426
Fokkema T, De Jong Gierveld J, Dykstra PA (2012) Cross-national differences in older adult loneliness. J Psychol 146:201–228. https://doi.org/10.1080/00223980.2011.631612
Koenen KC, Ratanatharathorn A, Ng L et al (2017) Posttraumatic stress disorder in the World Mental Health Surveys. Psychol Med 47:2260–2274. https://doi.org/10.1017/S0033291717000708
Mann F, Bone JK, Lloyd-Evans B, Frerichs J, Pinfold V, Ma R, Wang J, Johnson S (2017) A life less lonely: the state of the art in interventions to reduce loneliness in people with mental health problems. Soc Psychiatry Psychiatr Epidemiol 52:627–638. https://doi.org/10.1007/s00127-017-1392-y
Webber M, Fendt-Newlin M (2017) A review of social participation interventions for people with mental health problems. Soc Psychiatry Psychiatr Epidemiol 52:369–380. https://doi.org/10.1007/s00127-017-1372-2
Funding
The work of the first author of this study was conducted as part of the Pieter van Vollenhoven Chair at INTERVICT, Tilburg University, sponsored by the Dutch Victim Support Foundation (Fonds Slachtofferhulp).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical standards
The manuscript does not contain clinical studies or patient data.
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
A correction to this article is available online at https://doi.org/10.1007/s00127-018-1493-2.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
van der Velden, P.G., Pijnappel, B. & van der Meulen, E. Potentially traumatic events have negative and positive effects on loneliness, depending on PTSD-symptom levels: evidence from a population-based prospective comparative study. Soc Psychiatry Psychiatr Epidemiol 53, 195–206 (2018). https://doi.org/10.1007/s00127-017-1476-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-017-1476-8