Abstract
Purpose
This study sought to investigate time to remission from depression in a community-based sample of adults followed for 12 years.
Methods
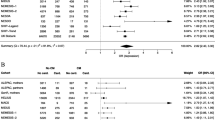
Data were derived from the National Population Health Survey (1994/5–2006/7 and 1996/7–2008/9). Fully 1,128 adults were included who were depressed at baseline according to DSM-III/CIDI-SF criteria. Kaplan–Meier and Cox proportional hazards procedures were used to determine time to remission and the demographic (e.g., gender and marital status), psychosocial (e.g., social support and adverse childhood experience) and health-related (e.g., pain, health conditions and alcohol use) factors with which it is associated.
Results
More than three quarters of the sample (77 %) no longer screened positive for depression at 2 years, and nearly the entire sample (94 %) had remitted by 12 years. Adverse childhood experiences (i.e., childhood abuse and parental additions), lack of social support, the presence of pain and health conditions (i.e., migraines, arthritis and back pain) each predicted more time to remission. The only factor associated with time to remission in the multivariate analysis was a history of childhood physical abuse.
Conclusions
Most community members with depression get better after 2 years and nearly all will have remitted, at least once, by 12 years. The results of this study may help guide the development of interventions for chronic depression that focus on early prevention of childhood abuse.
Similar content being viewed by others
References
Moussavi S, Chatterji S, Verdes E, Tandon A, Patel V, Ustun B (2007) Depression, chronic diseases, and decrements in health: results from the World Health Surveys. Lancet 370:851–858
World Health Organization (2004) The global burden of disease: 2004 update. http://www.who.int/healthinfo/global_burden_disease/2004_report_update/en/index.html. Accessed April 9, 2013
Casacalenda N, Perry JC, Looper K (2002) Remission in major depressive disorder: a comparison of pharmacotherapy, psychotherapy, and control conditions. Am J Psychiatry 159:1354–1360
Dawson MY, Michalak EE, Waraich P, Anderson JE, Lam RW (2004) Is remission of depressive symptoms in primary care a realistic goal? A meta-analysis. BMC Fam Pract 5:19
Trivedi MH, Corey-Lisle PK, Guo Z, Lennox RD, Pikalov A, Kim E (2009) Remission, response without remission, and nonresponse in major depressive disorder: impact on functioning. Int Clin Psychopharmacol 24:133–138
Hirschfeld RMA (2000) Psychosocial Predictors of Outcome in Depression. http://www.acnp.org/G4/GN401000107/. Accessed June 20, 2013
Tranter R, O’Donovan C, Chandarana P, Kennedy S (2002) Prevalence and outcome of partial remission in depression. J Psychiatry Neurosci 27:241–247
Donohue JM, Pincus HA (2007) Reducing the societal burden of depression: a review of economic costs, quality of care and effects of treatment. Pharmacoeconomics 25:7–24
Bakish D (2001) New standard of depression treatment: remission and full recovery. J Clin Psychiatry 62(Suppl 26):5–9
Keller MB (2003) Past, present, and future directions for defining optimal treatment outcome in depression: remission and beyond. JAMA 289:3152–3160
Richards D (2011) Prevalence and clinical course of depression: a review. Clin Psychol Rev 31:1117–1125
Holzel L, Harter M, Reese C, Kriston L (2011) Risk factors for chronic depression—a systematic review. J Affect Disord 129:1–13
Conradi HJ, de Jonge P, Ormel J (2008) Prediction of the three-year course of recurrent depression in primary care patients: different risk factors for different outcomes. J Affect Disord 105:267–271
Rhebergen D, Lamers F, Spijker J, de Graaf R, Beekman AT, Penninx BW (2012) Course trajectories of unipolar depressive disorders identified by latent class growth analysis. Psychol Med 42:1383–1396
Szadoczky E, Rozsa S, Zambori J, Furedi J (2004) Predictors for 2-year outcome of major depressive episode. J Affect Disord 83:49–57
Bockting CL, Spinhoven P, Koeter MW, Wouters LF, Schene AH, Depression Evaluation Longitudinal Therapy Assessment Study Group (2006) Prediction of recurrence in recurrent depression and the influence of consecutive episodes on vulnerability for depression: a 2-year prospective study. J Clin Psychiatry 67:747–755
Nelson JC, Zhang Q, Deberdt W, Marangell LB, Karamustafalioglu O, Lipkovich IA (2012) Predictors of remission with placebo using an integrated study database from patients with major depressive disorder. Curr Med Res Opin 28:325–334
Spijker J, de Graaf R, Bijl RV, Beekman AT, Ormel J, Nolen WA (2004) Determinants of persistence of major depressive episodes in the general population. Results from the Netherlands Mental Health Survey and Incidence Study (NEMESIS). J Affect Disord 81:231–240
van den Brink RH, Ormel J, Tiemens BG, Smit A, Jenner JA, van der Meer K et al (2002) Predictability of the one-year course of depression and generalized anxiety in primary care. Gen Hosp Psychiatry 24:156–163
Meyers B (2002) Predictors of early recovery from major depression among persons admitted to community-based clinics: an observational study. Arch Gen Psychiatry 59:729–735
De Almeida Fleck MP, Simon G, Herrman H, Bushnell D, Martin M, Patrick D et al (2005) Major depression and its correlates in primary care settings in six countries. 9-month follow-up study. British J Psychiatry 186:41–47
Barkow K, Maier W, Ustun TB, Gansicke M, Wittchen HU, Heun R (2003) Risk factors for depression at 12-month follow-up in adult primary health care patients with major depression: an international prospective study. J Affect Disord 76:157–169
Bracke P (2000) The three-year persistence of depressive symptoms in men and women. Soc Sci Med 51:51–64
Conradi H, DeJonge P, Ormel J (2008) Prediction of the three-year course of recurrent depression in primary care patients: different risk factors for different outcomes. J Affect Disord 105:267–271
Melartin TK, Rytsala HJ, Leskela US, Lestela-Mielonen PS, Sokero TP, Isometsa ET (2004) Severity and comorbidity predict episode duration and recurrence of DSM-IV major depressive disorder. J Clin Psychiatry 65:810–819
Nasser EH, Overholser JC (2005) Recovery from major depression: the role of support from family, friends, and spiritual beliefs. Acta Psychiatr Scand 111:125–132
Harkness KL, Bagby RM, Kennedy SH (2012) Childhood maltreatment and differential treatment response and recurrence in adult major depressive disorder. J Consult Clin Psychol 80:342–353
Nanni V, Uher R, Danese A (2012) Childhood maltreatment predicts unfavorable course of illness and treatment outcome in depression: a meta-analysis. Am J Psychiatry 169:141–151
Miniati M, Rucci P, Benvenuti A, Frank E, Buttenfield J, Giorgi G et al (2010) Clinical characteristics and treatment outcome of depression in patients with and without a history of emotional and physical abuse. J Psychiatr Res 44:302–309
Ciudad A, Alvarez E, Roca M, Baca E, Caballero L, Garcia de Polavieja P et al (2012) Early response and remission as predictors of a good outcome of a major depressive episode at 12-month follow-up: a prospective, longitudinal, observational study. J Clin Psychiatry 73:185–191
Fuller-Thomson E, Battiston M, Gadalla T, Shaked Y, Raza F (in press) Remission from depression among adults with arthritis: a 12-year follow-up of a population-based study. Depress Res Treat. http://www.hindawi.com/journals/drt/aip/
Kroenke K, Shen J, Oxman TE, Williams JW Jr, Dietrich AJ (2008) Impact of pain on the outcomes of depression treatment: results from the RESPECT trial. Pain 134:209–215
Babyak M, Blumenthal JA, Herman S, Khatri P, Doraiswamy M, Moore K et al (2000) Exercise treatment for major depression: maintenance of therapeutic benefit at 10 months. Psychosom Med 62:633–638
Kloiber S, Ising M, Reppermund S, Horstmann S, Dose T, Majer M et al (2007) Overweight and obesity affect treatment response in major depression. Biol Psychiatry 62:321–326
Boschloo L, Vogelzangs N, van den Brink W, Smit JH, Veltman DJ, Beekman AT et al (2012) Alcohol use disorders and the course of depressive and anxiety disorders. Br J Psychiatry 200:476–484
Health Statistics Division, Statistics Canada (1995) National Population Health Survey 1994-95: Overview. http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SurvId=3225&SurvVer=0&SDDS=3225&InstaId=15280&InstaVer=1&lang=en&db=imdb&adm=8&dis=2. Accessed June 20, 2013
Statistics Canada (2012) National Population Health Survey-Household Component—Longitudinal (NPHS). http://www23.statcan.gc.ca:81/imdb/p2SV.pl?Function=getSurvey&SDDS=3225&lang=en&db=imdb&adm=8&dis=2. Accessed March 11, 2013
Kessler RC, Andrews G, Mroczek D, Uston B, Wittchen H (1998) The World Health Organization Composite International Diagnostic Interview Short Form (CIDI-SF). Int J Methods Psychiatr Res 7:171–185
Andrews G, Peters L (1998) The psychometric properties of the composite international diagnostic interview. Soc Psychiatry Psychiatr Epidemiol 33:80–88
Mulder RT, Joyce PR, Frampton CM, Luty SE, Sullivan PF (2006) Six months of treatment for depression: outcome and predictors of the course of illness. Am J Psychiatry 63:95–100
Oldehinkel AJ, Ormel J, Neeleman J (2000) Predictors of time to remission from depression in primary care patients: do some people benefit more from positive life changes than others? J Abnorm Psychol 109:299–307
Parker G, Wilhelm K, Mitchell P, Gladstone G (2000) Predictors of 1-year outcome in depression. Aust N Z J Psychiatry 34:56–64
Penza KM, Heim C, Nemeroff CB (2003) Neurobiological effects of childhood abuse: implications for the pathophysiology of depression and anxiety. Arch Women’s Ment Health 6:15–22
McCrory E, De Brito SA, Viding E (2012) The link between child abuse and psychopathology: a review of neurobiological and genetic research. J R Soc Med 105:151–156
Shonkoff JP, Boyce WT, McEwen BS (2009) Neuroscience, molecular biology, and the childhood roots of health disparities: building a new framework for health promotion and disease prevention. JAMA 301:2252–2259
Marmot M, Allen J, Bell R, Bloomer E, Goldblatt P (2012) Consortium for the European Review of Social Determinants of Health and the Health Divide. WHO European review of social determinants of health and the health divide. Lancet 380:1011–1029
Scott KL, Lishak V (2012) Intervention for maltreating fathers: statistically and clinically significant change. Child Abuse Negl 36:680–684
Mead N, Lester H, Chew-Graham C, Gask L, Bower P (2010) Effects of befriending on depressive symptoms and distress: systematic review and meta-analysis. Br J Psychiatr 196:96–101
Hardt J, Rutter M (2004) Validity of adult retrospective reports of adverse childhood experiences: review of the evidence. J Child Psychol Psychiatry 45:260–273
Lizardi H, Klein DN (2005) Long-term stability of parental representations in depressed outpatients utilizing the parental bonding instrument. J Nerv Ment Dis 193:183–188
Andrade L, Caraveo-Anduaga J, Berglund P, Bijl R, De Graaf R, Vollebergh W et al (2003) The epidemiology of major depressive episodes: results from the International Consortium of Psychiatric Epidemiology (ICPE) Surveys. Int J Methods Psychiatr Res 12:3–21
Kohn R, Saxena S, Levav I, Saraceno B (2004) The treatment gap in mental health care. Bull World Health Organ 82:858–866
Messias E, Eaton WW, Grooms AN (2011) Income inequality and depression prevalence across the United States: an ecological study. Psychiatr Serv 62:710–712
Chen YY, Subramanian SV, Acevedo-Garcia D, Kawachi I (2005) Women’s status and depressive symptoms: a multilevel analysis. Soc Sci Med 60:49–60
Acknowledgments
The first author (Esme Fuller-Thomson) would like to gratefully acknowledge support received from the Sandra Rotman Endowed Chair in Social Work. We wish to thank Statistics Canada and the Social Sciences and Humanities Council of Canada for permission to access the longitudinal form of the National Population Health Survey via the Research Data Center (RDC) at the University of Toronto. We are also grateful to the staff at the Toronto RDC for their help in accessing the data. The opinions expressed herein are our own and do not represent the views of Statistics Canada.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fuller-Thomson, E., Battiston, M., Gadalla, T.M. et al. Bouncing back: remission from depression in a 12-year panel study of a representative Canadian community sample. Soc Psychiatry Psychiatr Epidemiol 49, 903–910 (2014). https://doi.org/10.1007/s00127-013-0814-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00127-013-0814-8