Abstract
Aims/hypothesis
Dietary patterns characterised by high intakes of vegetables may lower the risk of pre-eclampsia and premature birth in the general population. The effect of dietary patterns in women with type 1 diabetes, who have an increased risk of complications in pregnancy, is not known. The aim of this study was to investigate the relationship between dietary patterns and physical activity during pregnancy and maternal complications and birth outcomes in women with type 1 diabetes. We also compared dietary patterns in women with and without type 1 diabetes.
Methods
Diet was assessed in the third trimester using a validated food frequency questionnaire in participants followed prospectively in the multi-centre Environmental Determinants of Islet Autoimmunity (ENDIA) study. Dietary patterns were characterised by principal component analysis. The Pregnancy Physical Activity Questionnaire was completed in each trimester. Data for maternal and birth outcomes were collected prospectively.
Results
Questionnaires were completed by 973 participants during 1124 pregnancies. Women with type 1 diabetes (n=615 pregnancies with dietary data) were more likely to have a ‘fresh food’ dietary pattern than women without type 1 diabetes (OR 1.19, 95% CI 1.07, 1.31; p=0.001). In women with type 1 diabetes, an increase equivalent to a change from quartile 1 to 3 in ‘fresh food’ dietary pattern score was associated with a lower risk of pre-eclampsia (OR 0.37, 95% CI 0.17, 0.78; p=0.01) and premature birth (OR 0.35, 95% CI 0.20, 0.62, p<0.001). These associations were mediated in part by BMI and HbA1c. The ‘processed food’ dietary pattern was associated with an increased birthweight (β coefficient 56.8 g, 95% CI 2.8, 110.8; p=0.04). Physical activity did not relate to outcomes.
Conclusions/interpretation
A dietary pattern higher in fresh foods during pregnancy was associated with sizeable reductions in risk of pre-eclampsia and premature birth in women with type 1 diabetes.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Women with type 1 diabetes have a substantially increased risk of adverse maternal and perinatal outcomes, including pre-eclampsia, premature birth and infants born large for gestational age [1, 2]. Healthier dietary patterns during pregnancy have been associated with more favourable pregnancy and birth outcomes in the general population [3,4,5]. Analysis of dietary patterns has the advantage of examining the effect of overall diet, rather than being restricted to individual nutrients or foods. By providing a broader picture of food and nutrient consumption, dietary patterns may be more predictive of disease risk [6]. In the general population, dietary patterns during pregnancy characterised by high intakes of vegetables, plant foods and vegetable oils, or a high adherence to a Mediterranean-style dietary pattern pre-pregnancy, are associated with a moderately lower risk of developing hypertensive disorders of pregnancy (HDP), including pre-eclampsia [3, 4]. Dietary patterns characterised by high intakes of vegetables, fruits, wholegrains, low-fat dairy and lean protein foods are associated with a lower risk of preterm birth [5] and those characterised by high intakes of refined grains, processed meat and foods high in saturated fat or sugar with lower birthweight [5]. Increased physical activity and reduced sedentary behaviour during pregnancy have also been associated with moderately reduced risk of pre-eclampsia and gestational hypertension in the general population [7, 8].
Attention to nutrition is essential for women with type 1 diabetes during pregnancy, both for optimal glycaemic control and to meet increased nutritional requirements. However, to date no studies have investigated the impact of dietary intake during pregnancy on maternal and birth outcomes in women with type 1 diabetes.
The primary aim of this study was to investigate the relationship between dietary patterns and physical activity during pregnancy with maternal complications and birth outcomes in a large cohort of women with type 1 diabetes followed prospectively in the Environmental Determinants of Islet Autoimmunity (ENDIA) study. We also aimed to compare their dietary patterns with women without type 1 diabetes who also participated in ENDIA.
Methods
Study design and participants
Data were collected prospectively as part of the ENDIA study, a national Australian longitudinal prospective pregnancy/birth cohort study with the overall aim to determine the early-life exposures that drive the development of type 1 diabetes [9]. In this study, all women were investigated according to the ENDIA protocol at 3 month intervals during pregnancy from the time of recruitment until birth, and their children in the neonatal period. Investigation included clinical measurements, clinical outcomes and questionnaires assessing nutrition, exercise and lifestyle.
ENDIA recruited 1488 pregnant women or those with a child less than 6 months of age between February 2013 and November 2019, where the child had a first-degree relative with type 1 diabetes. Women were excluded from the study if they had an inadequate understanding of English to provide consent and responses to questionnaires. This analysis included all women who completed at least one diet or physical activity questionnaire during pregnancy; women with twin or triplet pregnancies were excluded.
The ENDIA study was reviewed and approved by the study’s lead Human Research Ethics Committee at the Women’s and Children’s Health Network under the National Mutual Acceptance Scheme (current approval no. 2020/HRE01400) and at all participating study sites. Conduct in Western Australia was approved by the Women and Newborn Health Service Ethics Committee (ref. no. RGS0000002639). ENDIA is registered on the Australian New Zealand Clinical Trials Registry (ACTRN12613000794707). All women provided written informed consent and were free to withdraw from the study at any time.
Demographic and clinical data
Pre-pregnancy weight and maternal demographics were self-reported by participants at their first appointment. Pre-pregnancy BMI (kg/m2) was calculated using pre-pregnancy reported weight and height measured at the first visit. Maternal weight was measured at each visit and additional weight measurements collected at routine clinic visits were obtained from medical records. If pre-pregnancy weight was missing, the earliest weight available in the first trimester was used to estimate pre-pregnancy BMI. Gestational weight gain was calculated as the difference between the last weight measured during the third trimester of pregnancy and the pre-pregnancy weight or first weight recorded during pregnancy. Pregnancy data (including parity, HbA1c, medications and medical complications) and birth outcomes (gestational age at birth, birthweight and neonatal hypoglycaemia) were obtained from hospital medical records. Socioeconomic status was calculated using postcode at enrolment using the Socio-Economic Indexes for Areas Index of Relative Socio-Economic Advantage and Disadvantage (SEIFA IRSAD). This index is derived from national Census variables related to both advantage and disadvantage, for example household income and level of education [10]. Remoteness was classified using the Modified Monash Model [11], which defines a location according to geographical remoteness, as defined by the Australian Bureau of Statistics, and town size.
HDP were verified using medical record review according to International Society for the Study of Hypertension in Pregnancy classification [12] and included gestational hypertension (new onset of hypertension after 20 weeks’ gestation), pre-eclampsia (hypertension occurring for the first time after 20 weeks, associated with proteinuria and/or organ involvement), superimposed pre-eclampsia (pre-eclampsia superimposed on chronic hypertension), eclampsia and HELLP (haemolysis, elevated liver enzymes and low platelets) syndrome. Prematurity was defined as birth before 37 weeks’ gestation. Neonatal hypoglycaemia was defined as blood glucose level in the newborn of less than 2.6 mmol/l within the first 72 h post birth.
HbA1c was measured using either point-of-care or laboratory testing methods, commonly a Vantage analyser (Siemens Diagnostics, Camberley, UK) or a Variant analyser (Bio-Rad Laboratories, Hercules, CA, USA). All medical laboratories were accredited by the National Association of Testing Authorities, Australia, against the international standard ISO 15189 Medical laboratories, which mandates that all analytes in a laboratory’s test menu be subject to the Royal College of Pathologists of Australasia Quality Assurance Programs [13]. The first HbA1c measurement available during pregnancy (usually conception or first trimester) was used and analysis controlled for gestational week of measurement.
Dietary and lifestyle measures
Diet was assessed using the Dietary Questionnaire for Epidemiological Studies version 2 (DQESv2), a self-administered 74-item food frequency questionnaire [14] validated in women of child-bearing age (16–48 years) [15]. Participants completed the questionnaire during their third trimester of pregnancy and were asked to assess their diet since the start of pregnancy. The DQESv2 provided daily intakes (in grams) of specific foods and beverages. The 101 individual food items were combined into 19 food item categories based on nutrient content and culinary usage [16] (electronic supplementary material [ESM] Table 1) for the analysis of dietary patterns. Consumption of each food item was converted into daily servings by adjusting the intake for serving size as described in the Australian Dietary Guidelines [17]. The total number of servings per day were calculated by summing the numbers of servings consumed per day for all food items in each of the five food groups of the Australian Dietary Guidelines.
Physical activity was measured during each trimester using the Pregnancy Physical Activity Questionnaire (PPAQ) [18], a validated self-report questionnaire that measures the time spent participating in 32 activities grouped into different types of activity (i.e. sedentary, light, moderate and vigorous activity). Participants could add two physical activities not listed in the questionnaire, where the intensities were individually estimated using the Compendium of Physical Activities [19]. The duration of time spent in each activity was multiplied by its intensity (i.e. metabolic equivalent of task [MET]) and summed to calculate the mean weekly energy expenditure, expressed as MET-hours/week.
Statistical analysis
To account for the potential correlation between data from the same participant during different pregnancies (i.e. a participant included in the study more than once), a random intercept for each participant was included in each model. Analyses were restricted to participants with complete data as missing data were minimal for outcomes and confounders used in analyses (as reported in tables). R statistical software version 4.3.1 [20] and a significance level of 5% was used for all analyses. Results for adjusted models are reported unless otherwise specified.
Dietary patterns for pregnancies with and without type 1 diabetes
Dietary patterns were derived using principal component analysis (PCA) on dietary data based on 19 food item categories from all women with and without type 1 diabetes. The resulting principal components, derived in decreasing order of importance, were a linear combination of the food items. The number of dietary patterns (principal components) identified was based on eigenvalues >1.5 and on identification of a break point in the scree plot [21]. Food item categories with a factor loading of ±0.30 or more were considered important contributors of each dietary pattern [22]. Scores for each principal component were obtained by summing up observed intakes of the component food items weighted by the factor loading and indicate the extent to which the participant’s diet conformed to the respective dietary pattern. A logistic regression mixed model was used to compare dietary patterns in women with and without type 1 diabetes using the principal component scores from each dietary pattern. Potential confounders (age, pre-pregnancy BMI and parity) were included in the model.
Association between dietary patterns and physical activity, and maternal complications and birth outcomes in pregnancies with type 1 diabetes
Analysis of associations between dietary patterns and outcomes were planned only for the women with type 1 diabetes, as maternal complications and adverse birth outcomes are about fivefold more prevalent in women with type 1 diabetes in Australia. Maternal outcomes were HDP (categorised as gestational hypertension or pre-eclampsia/eclampsia/HELLP), and birth outcomes were prematurity, gestational age at birth, birthweight and neonatal hypoglycaemia. Exposures were dietary patterns (participant principal components scores) and physical activity (mean MET-hours/week for total activity, sedentary activity, and moderate and vigorous activity). Models that investigated associations with physical activity included nested random intercept terms, visits within pregnancies within the same participant (to account for the fact that each mother could have completed up to three questionnaires for each pregnancy), and were adjusted for the gestational age when the questionnaire was completed.
Prematurity (<37 weeks’ gestation) and neonatal hypoglycaemia (blood glucose level <2.6 mmol/l) were fitted in separate mixed logistic regression models. A separate mixed multinomial logistic regression model was used for the HDP categories. For continuous outcomes—HbA1c, gestational age at birth and birthweight—separate linear mixed models were fitted. Potential confounders (maternal age, parity and SEIFA IRSAD percentile) were adjusted for in all models. Birthweight was also adjusted for gestation at birth. To make the results more interpretable, participant scores identified from PCA were rescaled such that a one-unit change in principal component score represented the IQR from 25th percentile to 75th percentile. The mean intake of food group servings was calculated from participants in each quartile of principal component scores for the ‘fresh food’ dietary pattern. The difference in intake between the highest and lowest quartile was calculated to correspond to a one-unit change of the rescaled scores.
Mediation analyses
Potential mediators of the association between dietary pattern and pre-eclampsia and premature birth were HbA1c and BMI. Model-based causal mediation analysis with quasi-Bayesian Monte Carlo simulation (10,000 simulation) was performed [23] using the ‘mediation’ R package. While pre-pregnancy BMI is not strictly a mediator temporally between diet and pre-eclampsia (i.e. it was measured before the time covered by the diet questionnaire), it is an available proxy for early pregnancy BMI before weight increases. Therefore, the influence of pre-pregnancy BMI was also investigated as a mediator between diet and pre-eclampsia using model-based causal mediation analysis.
Sensitivity analyses
Sensitivity analyses were conducted excluding participants from the PCA if they reported an unrealistic energy intake (energy <4500 kJ/day or >20,000 kJ/day, n=109, including 82 with type 1 diabetes) [24] and if they had gestational diabetes (n=51) or type 2 diabetes (n=1). All models were then refitted with the resulting principal components scores. Separate sensitivity analyses were also conducted for the outcomes of pre-eclampsia and prematurity which excluded women with a parity greater than 0 (i.e. included only nulliparous women) as the risk of pre-eclampsia and premature birth are substantially influenced by parity and complications in a prior pregnancy.
Results
Participants
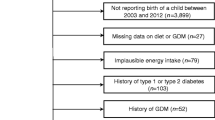
This analysis included 973 women who had 1124 pregnancies (725 pregnancies with type 1 diabetes and 399 pregnancies without type 1 diabetes) (Fig. 1). The 1124 pregnancies were representative of the full ENDIA cohort (1453 pregnancies and 1214 unique participants) in terms of maternal age, BMI, parity, socioeconomic demographics, and including the relative proportion of participants with and without type 1 diabetes [25]. Clinical characteristics and pregnancy and birth outcomes for participants included in this analysis are outlined in Table 1. Premature birth was mainly iatrogenic via induction of labour (22%) or Caesarean birth without labour (58%). Spontaneous premature labour occurred for the remaining 20% of participants with premature birth. A substantially higher proportion of women with type 1 diabetes had maternal complications and adverse birth outcomes (Table 1).
The DQESv2 was completed during 983 pregnancies with and without type 1 diabetes at a median gestational age of 33.8 (IQR 32.1–35.9) weeks. The PPAQ was completed during 406 pregnancies in early pregnancy at a median gestation of 12.5 (IQR 10.1–14.7) weeks, 786 pregnancies in mid pregnancy at 23.9 (IQR 20.7–26.3) weeks and 979 pregnancies in late pregnancy at 34.1 (IQR 32.1–35.9) weeks.
Dietary patterns in pregnancies with and without type 1 diabetes
Two principal components together explained 29% of the variation amongst the 19 food item categories, and they were retained to best describe the dietary patterns of all participants (Table 2; ESM Fig. 1). The first component was termed ‘processed food’ because of the high loading for processed snacks, red and processed meat, pizza and refined grains. The second component was termed ‘fresh food’ because of the high loading for nuts, vegetables and fruit.
Women with type 1 diabetes were more likely to have a ‘fresh food’ pattern (OR 1.19, 95% CI 1.07, 1.31; p=0.001) and less likely to have a ‘processed food’ pattern than those without type 1 diabetes (OR 0.89, 95% CI 0.82, 0.96; p=0.002). Women with type 1 diabetes who were in the highest quartile of the ‘fresh food’ pattern principal component scores were older, had a lower BMI and HbA1c, and a higher socioeconomic status than women with type 1 diabetes in the lowest quartile (Table 3). The median values of servings for most food groups were below the Australian Dietary Guideline recommendations for both groups.
Association between dietary patterns and maternal complications and birth outcomes in pregnancies with type 1 diabetes
In women with type 1 diabetes, a one-unit increase in the rescaled scores of the ‘fresh food’ pattern was associated with a decreased likelihood of pre-eclampsia and premature birth (Fig. 2). The ‘fresh food’ pattern was associated with an increased gestational age at birth (β coefficient 0.38 weeks, 95% CI 0.23, 0.53; p<0.001). No association was detected between dietary pattern and gestational hypertension. The ‘processed food’ pattern was associated with an increased birthweight (β coefficient 56.8 g, 95% CI 2.8, 110.8; p=0.04). There were no associations between dietary pattern and neonatal hypoglycaemia. A diet more aligned with the ‘fresh food’ pattern was associated with modestly lower HbA1c (β coefficient −2.79 mmol/mol, 95% CI −4.20, −1.38; p<0.001) and a diet more aligned with the ‘processed food’ pattern was associated with a higher HbA1c (β coefficient 1.31 mmol/mol, 95% CI 0.06, 2.55; p=0.039).
Association between dietary patterns (‘processed food’ dietary pattern or ‘fresh food’ dietary pattern) and maternal complications and birth outcomes in women with type 1 diabetes (n=615). Values are presented as ORs with 95% CIs for an increase of one IQR in dietary pattern principal components score. Models were adjusted for age, parity and socioeconomic status
The difference in food group servings between the highest and lowest quartile of principal component scores for the ‘fresh food’ dietary pattern was, on average, an additional 1.15 servings of fruit, 1.12 servings of vegetables, 0.30 serving of dairy, 0.38 serving of grains, and 1.14 servings of lean meats, poultry, fish, eggs, tofu, legumes/beans; and 0.75 less serving of discretionary items (foods high in calories, saturated fat, added sugar and/or added salt).
Association between physical activity and maternal complications and birth outcomes in pregnancies with type 1 diabetes
Total physical activity was associated with gestational age at birth (β coefficient 0.06 weeks, 95% CI 0.01, 0.11; p=0.014) and birthweight (β coefficient 36.6 g, 95% CI 16.4, 56.7; p<0.001) in the unadjusted models only. Sedentary activity was associated with birthweight (β coefficient −58.8 g, 95% CI −79.2, −38.0; p<0.001) in the unadjusted model only. Moderate and vigorous activity was associated with birthweight (β coefficient 30.2 g, 95% CI 10.2, 50.3; p=0.003) in the unadjusted model only. There were no other associations between physical activity and either maternal complications or birth outcomes in the adjusted models.
Mediation analyses
Separate mediation analyses showed that 27% (p=0.026) of the effect of the ‘fresh food’ pattern on pre-eclampsia and 23% (p<0.001) of the effect on premature birth was the result of the mediation pathway through HbA1c, while 26% (p=0.030) of the effect on pre-eclampsia and 14% (p=0.006) of the effect on premature birth was a result of the mediation pathway through maternal BMI (ESM Fig. 2).
Sensitivity analyses
Removing women with other types of diabetes from the women without type 1 diabetes group when undertaking PCA did not change the associations between dietary patterns and outcomes. After excluding participants who reported an unrealistic energy intake and refitting all models, the standard errors of model coefficients increased slightly for ‘fresh food’ dietary pattern and pre-eclampsia, as expected from a small reduction in the sample size (ESM Table 2a). In addition, an increase in the ‘processed food’ pattern was now associated with an increased likelihood of gestational hypertension (OR 2.29, 95%CI 1.11, 4.72; p=0.024) and premature birth (OR 1.54, 95% CI 1.04, 2.27; p=0.030), and a decrease in gestational age at birth (β coefficient −0.16 weeks, 95% CI −0.31, −0.01; p=0.033). A sensitivity analysis of only nulliparous participants showed no changes for pre-eclampsia and premature birth (ESM Table 2b).
Discussion
We report the first large comprehensive investigation of dietary patterns and physical activity during pregnancy in 973 women (1124 pregnancies) with and without type 1 diabetes followed prospectively in the same cohort, and their association with complications and birth outcomes in women with type 1 diabetes. In 615 women with type 1 diabetes, a ‘fresh food’ dietary pattern was associated with a reduction in risk of pre-eclampsia by 63% and of premature birth by 65%. Importantly, relatively small increments in fresh food intake in the daily diet separated those women with type 1 diabetes in the highest quartile from those in the lowest quartile of the ‘fresh food’ pattern, suggesting that sustained small changes in daily intake could be associated with sizeable improvements in outcomes. A lower score for the ‘fresh food’ pattern was associated with modestly higher HbA1c levels, where HbA1c was one mediator, along with BMI, of the associations between diet and maternal complications and birth outcomes. Women with type 1 diabetes were more likely to have a ‘fresh food’ dietary pattern in pregnancy than those without type 1 diabetes. Even so, the majority of women did not meet Australian dietary recommendations for pregnancy, irrespective of their type 1 diabetes status.
The approximately fivefold increased risk of both pre-eclampsia and premature birth in women with type 1 diabetes make our findings, and the opportunities they present for dietary intervention, particularly relevant. Dietary patterns characterised by high intake of foods with antioxidative and anti-inflammatory properties such as vegetables, fruits, wholegrains, fish, legumes and pulses, predominant in the ‘fresh food’ pattern, may reduce inflammation that contributes to both pre-eclampsia and premature birth [26]. Many women find it difficult to consume recommended dietary intakes during pregnancy [27,28,29,30]. Consistent with other international studies of type 1 diabetes in pregnancy [31], the ENDIA mothers’ mean intakes, even in the highest quartile of the ‘fresh food’ dietary pattern, only met recommended fruit and dairy intakes. To therefore better estimate dietary changes in women with type 1 diabetes that would be needed to reduce risk of pre-eclampsia and premature birth, we looked at the mean differences in food group serving intake between the lowest and highest quartile of principal component scores for the ‘fresh food’ dietary pattern. Reassuringly, this equated to relatively small increments per day: one-third more serving of both dairy and grains, and one serving of lean meat, one serving of fruit, one serving of vegetables and three-quarter less serving of discretionary items or junk food. Dietary patterns with higher intakes of fruits and vegetables have been associated with similar sized risk reduction in pre-eclampsia and premature birth in the general population as we report in type 1 diabetes [3, 5]. Dietary interventions in the general population have also reduced these complications, which is encouraging for women with type 1 diabetes in light of our findings [32, 33].
Limited studies have examined physical activity levels during pregnancy in type 1 diabetes [34, 35]. The lack of association that we describe for adjusted models between exercise and HDP and birth outcomes has been described by others, but for early pregnancy exercise only, and in smaller numbers [35]. Sedentary behaviour in early pregnancy may be higher in women developing pre-eclampsia [35] but larger studies are needed. Despite reporting higher levels of total physical activity than other studies [35, 36], we found no beneficial association with outcomes.
Strengths of our study are the multi-centre design and, to our knowledge, this is the largest single prospective study globally to investigate dietary patterns and physical activity in pregnancies with type 1 diabetes. The ENDIA participants were relatively comparable with the population who gave birth in Australia [37]. They were of similar age, parity and rates of overweight and obesity, although a higher proportion of ENDIA participants were born in Australia, achieved tertiary education and had modestly higher socioeconomic status. Further, rates of pregnancy complications and birth outcomes were comparable with other type 1 diabetes in pregnancy cohorts in Australia [38, 39] and Europe [40, 41].
Our study has several limitations. First, as above, higher socioeconomic status and level of education may limit the generalisability to all pregnancies with type 1 diabetes. As positive social determinants of health, they may influence the diet, physical activity and pregnancy/birth outcomes. Although the food frequency questionnaire is a valid and reliable tool covering long-term food intake, it is self-reported and limited by memory recall and the foods listed in the questionnaire. Participants may have been influenced more by their current dietary intakes in their third trimester. Over- and under-reporting is common with food frequency questionnaires so a sensitivity analysis was conducted excluding those with ‘unrealistic’ energy intakes. A ‘processed food’ dietary pattern was then associated with increased risk of gestational hypertension (2 times the odds) and premature birth (1.5 times the odds) in women with type 1 diabetes; this additional finding is consistent with the main findings of the study. The majority of ‘unrealistic’ reporters under-reported their dietary intake (97%). Foods with a negative health image, like processed foods, are more likely to be under-reported [42]. Serving size for discretionary items may also be smaller than expected (e.g. half a chocolate bar). While HbA1c is a practical measure of glycaemic control, it cannot assess glucose variability. Continuous glucose monitoring would have provided a more comprehensive assessment of glycaemic control and variability, but these metrics were not available. In relation to maternal BMI, pre-pregnancy weights were self-reported as participants enrolled after they became pregnant. Australian maternity practice has changed recently to not weigh women regularly during pregnancy, which also limited the number of data points for gestational weight gain. A further clinical practice is that large for gestational age babies and babies from pregnancies with type 1 diabetes are often treated prophylactically for hypoglycaemia, thus limiting our ability to assess the association of diet and this outcome.
In conclusion, the benefits associated with a diet higher in fresh food in reducing pre-eclampsia and prematurity in the general population are also detectable in type 1 diabetes. Even though most women were not meeting the Australian Dietary Guidelines, it is a reassuring message that smaller, more achievable differences in dietary intake have the potential to reduce the risk of pre-eclampsia and premature birth significantly. This is encouraging for women with type 1 diabetes, who bear the burden of a much higher risk of these complications. Our findings offer the potential to reduce their risk of pre-eclampsia and premature birth with early pre-conception and systematic advice of the benefits of a fresh food diet rich in vegetables, fruit, nuts, fish and grains.
Abbreviations
- DQESv2:
-
Dietary Questionnaire for Epidemiological Studies version 2
- ENDIA:
-
Environmental Determinants of Islet Autoimmunity
- HDP:
-
Hypertensive disorders of pregnancy
- HELLP:
-
Haemolysis, elevated liver enzymes and low platelets
- MET:
-
Metabolic equivalent of task
- PCA:
-
Principal component analysis
- PPAQ:
-
Pregnancy Physical Activity Questionnaire
- SEIFA IRSAD:
-
Socio-Economic Indexes for Areas Index of Relative Socio-Economic Advantage and Disadvantage
References
Persson M, Norman M, Hanson U (2009) Obstetric and perinatal outcomes in type 1 diabetic pregnancies: a large, population-based study. Diabetes Care 32(11):2005–2009. https://doi.org/10.2337/dc09-0656
McCarthy EA, Williamson R, Shub A (2019) Pregnancy outcomes for women with pre-pregnancy diabetes mellitus in Australian populations, rural and metropolitan: A review. Aust N Z J Obstet Gynaecol 59(2):183–194. https://doi.org/10.1111/ajo.12913
Brantsaeter AL, Haugen M, Samuelsen SO et al (2009) A dietary pattern characterized by high intake of vegetables, fruits, and vegetable oils is associated with reduced risk of preeclampsia in nulliparous pregnant Norwegian women. J Nutr 139(6):1162–1168. https://doi.org/10.3945/jn.109.104968
Schoenaker DA, Soedamah-Muthu SS, Callaway LK, Mishra GD (2015) Prepregnancy dietary patterns and risk of developing hypertensive disorders of pregnancy: results from the Australian Longitudinal Study on Women’s Health. Am J Clin Nutr 102(1):94–101. https://doi.org/10.3945/ajcn.114.102475
Chia A-R, Chen L-W, Lai JS et al (2019) Maternal dietary patterns and birth outcomes: a systematic review and meta-analysis. Adv Nutr 10(4):685–695. https://doi.org/10.1093/advances/nmy123
Hu FB (2002) Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol 13(1):3–9. https://doi.org/10.1097/00041433-200202000-00002
Spracklen CN, Ryckman KK, Triche EW, Saftlas AF (2016) Physical activity during pregnancy and subsequent risk of preeclampsia and gestational hypertension: a case control study. Matern Child Health J 20(6):1193–1202. https://doi.org/10.1007/s10995-016-1919-y
Davenport MH, Ruchat S-M, Poitras VJ et al (2018) Prenatal exercise for the prevention of gestational diabetes mellitus and hypertensive disorders of pregnancy: a systematic review and meta-analysis. Br J Sports Med 52(21):1367–1375. https://doi.org/10.1136/bjsports-2018-099355
Penno MA, Couper JJ, Craig ME et al (2013) Environmental determinants of islet autoimmunity (ENDIA): a pregnancy to early life cohort study in children at-risk of type 1 diabetes. BMC Pediatr 13(1):124. https://doi.org/10.1186/1471-2431-13-124
Australian Bureau of Statistics (2018) Census of Population and Housing: Socio-Economic Indexes for Areas (SEIFA), Australia, 2016. ABS, Canberra, Australia. Available from https://www.abs.gov.au/ausstats/abs@.nsf/mf/2033.0.55.001. Accessed 28 June 2021
Australian Government Department of Health (2019) Modified Monash Model. Available from https://www.health.gov.au/topics/rural-health-workforce/classifications/mmm. Accessed 26 May 2021
Brown MA, Magee LA, Kenny LC et al (2018) The hypertensive disorders of pregnancy: ISSHP classification, diagnosis & management recommendations for international practice. Pregnancy Hypertens 13:291–310. https://doi.org/10.1016/j.preghy.2018.05.004
Royal College of Pathologists of Australasia Quality Assurance Programs (2021) Chemical Pathology Archives. Available from https://rcpaqap.com.au/products/chemical/. Accessed 2 Sept 2021
Giles GG, Ireland PD (1996) Dietary Questionnaire for Epidemiological Studies (Version 2). Cancer Council Victoria, Melbourne
Hodge A, Patterson AJ, Brown WJ, Ireland P, Giles G (2000) The Anti Cancer Council of Victoria FFQ: relative validity of nutrient intakes compared with weighed food records in young to middle-aged women in a study of iron supplementation. Aust N Z J Public Health 24(6):576–583. https://doi.org/10.1111/j.1467-842x.2000.tb00520.x
Ashby-Mitchell K, Peeters A, Anstey KJ (2015) Role of dietary pattern analysis in determining cognitive status in elderly Australian adults. Nutrients 7(2):1052–1067. https://doi.org/10.3390/nu7021052
National Health and Medical Research Council (2013) Australian Dietary Guidelines. Department of Health and Ageing. Australian Government, Canberra, Australia
Chasan-Taber L, Schmidt MD, Roberts DE, Hosmer D, Markenson G, Freedson PS (2004) Development and validation of a Pregnancy Physical Activity Questionnaire. Med Sci Sports Exerc 36(10):1750–1760. https://doi.org/10.1249/01.mss.0000142303.49306.0d
Ainsworth BE, Haskell WL, Herrmann SD et al (2011) 2011 Compendium of physical activities: a second update of codes and MET values. Med Sci Sports Exerc 43(8):1575–1581. https://doi.org/10.1249/MSS.0b013e31821ece12
R Core Team (2023) R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing. Vienna, Austria
Cattell RB (1966) The Scree Test for the number of factors. Multivariate Behav Res 1(2):245–276. https://doi.org/10.1207/s15327906mbr0102_10
Kline P (1994) An Easy Guide to Factor Analysis. Routledge, London
Tingley D, Yamamoto T, Hirose K, Keele L, Imai K (2014) mediation: R package for causal mediation analysis. J Stat Softw 59(5):1–38. https://doi.org/10.18637/jss.v059.i05
Meltzer HM, Brantsaeter AL, Ydersbond TA, Alexander J, Haugen M (2008) Methodological challenges when monitoring the diet of pregnant women in a large study: experiences from the Norwegian Mother and Child Cohort Study (MoBa). Matern Child Nutr 4(1):14–27. https://doi.org/10.1111/j.1740-8709.2007.00104.x
Thomson RL, Oakey H, Haynes A et al (2024) Environmental Determinants of Islet Autoimmunity (ENDIA) longitudinal prospective pregnancy to childhood cohort study of Australian children at risk of type 1 diabetes: parental demographics and birth information. BMJ Open Diabetes Res Care 12(4):e004130. https://doi.org/10.1136/bmjdrc-2024-004130
Giugliano D, Ceriello A, Esposito K (2006) The effects of diet on inflammation: emphasis on the metabolic syndrome. J Am Coll Cardiol 48(4):677–685. https://doi.org/10.1016/j.jacc.2006.03.052
Bookari K, Yeatman H, Williamson M (2017) Falling short of dietary guidelines - What do Australian pregnant women really know? A cross sectional study. Women Birth 30(1):9–17. https://doi.org/10.1016/j.wombi.2016.05.010
Lee A, Muggli E, Halliday J, Lewis S, Gasparini E, Forster D (2018) What do pregnant women eat, and are they meeting the recommended dietary requirements for pregnancy? Midwifery 67:70–76. https://doi.org/10.1016/j.midw.2018.09.005
Wilkinson SA, Schoenaker DAJM, de Jersey S et al (2022) Exploring the diets of mothers and their partners during pregnancy: findings from the Queensland Family Cohort pilot study. Nutr Diet 79(5):602–615. https://doi.org/10.1111/1747-0080.12733
Slater K, Rollo ME, Szewczyk Z, Ashton L, Schumacher T, Collins C (2020) Do the dietary intakes of pregnant women attending public hospital antenatal clinics align with Australian Guide to Healthy Eating recommendations? Nutrients 12(8):2438. https://doi.org/10.3390/nu12082438
Neoh SL, Grisoni JA, Feig DS, Murphy HR, Group CC (2020) Dietary intakes of women with Type 1 diabetes before and during pregnancy: a pre-specified secondary subgroup analysis among CONCEPTT participants. Diabet Med 37(11):1841–1848. https://doi.org/10.1111/dme.13937
Khoury J, Henriksen T, Christophersen B, Tonstad S (2005) Effect of a cholesterol-lowering diet on maternal, cord, and neonatal lipids, and pregnancy outcome: a randomized clinical trial. Am J Obstet Gynecol 193(4):1292–1301. https://doi.org/10.1016/j.ajog.2005.05.016
Imhoff-Kunsch B, Briggs V, Goldenberg T, Ramakrishnan U (2012) Effect of n-3 long-chain polyunsaturated fatty acid intake during pregnancy on maternal, infant, and child health outcomes: a systematic review. Paediatr Perinat Epidemiol 26(Suppl):191–107. https://doi.org/10.1111/j.1365-3016.2012.01292.x
Vézina-Im L-A, Morin CM, Desroches S (2021) Sleep, diet and physical activity among adults living with type 1 and type 2 diabetes. Can J Diabetes 45(7):659–665. https://doi.org/10.1016/j.jcjd.2021.01.013
Do NC, Vestgaard M, Ásbjörnsdóttir B et al (2020) Physical activity, sedentary behavior and development of preeclampsia in women with preexisting diabetes. Acta Diabetol 57(5):559–567. https://doi.org/10.1007/s00592-019-01459-7
Ásbjörnsdóttir B, Ronneby H, Vestgaard M et al (2019) Lower daily carbohydrate consumption than recommended by the Institute of Medicine is common among women with type 2 diabetes in early pregnancy in Denmark. Diabetes Res Clin Pract 152:88–95. https://doi.org/10.1016/j.diabres.2019.05.012
Australian Institute of Health and Welfare (2019) Australia’s mothers and babies 2017—in brief. AIHW, Canberra, Australia. Available from https://www.aihw.gov.au/reports/mothers-babies/australias-mothers-and-babies-2017-in-brief/summary. Accessed 2 September 2019
Abell SK, Boyle JA, de Courten B et al (2016) Contemporary type 1 diabetes pregnancy outcomes: impact of obesity and glycaemic control. Med J Aust 205(4):162–167. https://doi.org/10.5694/mja16.00443
Immanuel J, Flack J, Wong VW et al (2021) The ADIPS pilot national diabetes in pregnancy benchmarking programme. Int J Environ Res Public Health 18(9):4899. https://doi.org/10.3390/ijerph18094899
Murphy HR, Howgate C, O’Keefe J et al (2021) Characteristics and outcomes of pregnant women with type 1 or type 2 diabetes: a 5-year national population-based cohort study. Lancet Diabetes Endocrinol 9(3):153–164. https://doi.org/10.1016/s2213-8587(20)30406-x
Jensen DM, Damm P, Moelsted-Pedersen L et al (2004) Outcomes in type 1 diabetic pregnancies: a nationwide, population-based study. Diabetes Care 27(12):2819–2823. https://doi.org/10.2337/diacare.27.12.2819
Macdiarmid J, Blundell J (1998) Assessing dietary intake: who, what and why of under-reporting. Nutr Res Rev 11(2):231–253. https://doi.org/10.1079/NRR19980017
Joseph FA, Hyett JA, Schluter PJ et al (2020) New Australian birthweight centiles. Med J Aust 213(2):79–85. https://doi.org/10.5694/mja2.50676
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Acknowledgements
The authors thank the co-ordinators, laboratory staff, project management team, and especially the ENDIA families for their dedication to continuing this important research. A list of members of the ENDIA study team can be found in the ESM.
Data availability
Data used in this study were derived from the ENDIA study. Data from the ENDIA study are available upon reasonable request via email to the corresponding author or endia@adelaide.edu.au.
Funding
Open Access funding enabled and organized by CAUL and its Member Institutions. This research was supported by JDRF Australia, the recipient of the Commonwealth of Australia grant for Accelerated Research under the Medical Research Future Fund, and with funding from the Leona M. and Harry B. Helmsley Charitable Trust (grant key 3-SRA-2023-1374-M-N, 3-SRA-2020-966-M-N, 1-SRA-2019-871-M-B, 4-SRA-2015-127-M-B), The National Health and Medical Research Council of Australia (Centre of Research Excellence for the Protection of Pancreatic Beta Cell and project grant APP1025083) and Diabetes SA. The study funders were not involved in the design of the study; the collection, analysis and interpretation of data; writing the report; and did not impose any restrictions regarding the publication of the report.
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
RLT and JJC conceived the study. RLT, JJC, HO, GS and KP designed the study. RLT, JJC, PA, MASP, KJM, RB, PGC, MEC, EAD, TH, LCH, AH, GS, PJV and JMW collected data required for the study and oversaw implementation of ethical practice and the ENDIA protocol at the clinical sites. JDB performed the statistical analysis and HO supervised the statistical analysis. ROS contributed to data curation and supervised the storage and maintenance of all data for the study. RLT, JDB, JJC and HO wrote the manuscript. All authors provided critical revision and approved the final version of the manuscript. RLT and HO are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Thomson, R.L., Brown, J.D., Oakey, H. et al. Dietary patterns during pregnancy and maternal and birth outcomes in women with type 1 diabetes: the Environmental Determinants of Islet Autoimmunity (ENDIA) study. Diabetologia (2024). https://doi.org/10.1007/s00125-024-06259-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00125-024-06259-5