Abstract
Aims/hypothesis
The objective of the Hypoglycaemia REdefining SOLutions for better liVES (Hypo-RESOLVE) project is to use a dataset of pooled clinical trials across pharmaceutical and device companies in people with type 1 or type 2 diabetes to examine factors associated with incident hypoglycaemia events and to quantify the prediction of these events.
Methods
Data from 90 trials with 46,254 participants were pooled. Analyses were done for type 1 and type 2 diabetes separately. Poisson mixed models, adjusted for age, sex, diabetes duration and trial identifier were fitted to assess the association of clinical variables with hypoglycaemia event counts. Tree-based gradient-boosting algorithms (XGBoost) were fitted using training data and their predictive performance in terms of area under the receiver operating characteristic curve (AUC) evaluated on test data. Baseline models including age, sex and diabetes duration were compared with models that further included a score of hypoglycaemia in the first 6 weeks from study entry, and full models that included further clinical variables. The relative predictive importance of each covariate was assessed using XGBoost’s importance procedure. Prediction across the entire trial duration for each trial (mean of 34.8 weeks for type 1 diabetes and 25.3 weeks for type 2 diabetes) was assessed.
Results
For both type 1 and type 2 diabetes, variables associated with more frequent hypoglycaemia included female sex, white ethnicity, longer diabetes duration, treatment with human as opposed to analogue-only insulin, higher glucose variability, higher score for hypoglycaemia across the 6 week baseline period, lower BP, lower lipid levels and treatment with psychoactive drugs. Prediction of any hypoglycaemia event of any severity was greater than prediction of hypoglycaemia requiring assistance (level 3 hypoglycaemia), for which events were sparser. For prediction of level 1 or worse hypoglycaemia during the whole follow-up period, the AUC was 0.835 (95% CI 0.826, 0.844) in type 1 diabetes and 0.840 (95% CI 0.831, 0.848) in type 2 diabetes. For level 3 hypoglycaemia, the AUC was lower at 0.689 (95% CI 0.667, 0.712) for type 1 diabetes and 0.705 (95% CI 0.662, 0.748) for type 2 diabetes. Compared with the baseline models, almost all the improvement in prediction could be captured by the individual’s hypoglycaemia history, glucose variability and blood glucose over a 6 week baseline period.
Conclusions/interpretation
Although hypoglycaemia rates show large variation according to sociodemographic and clinical characteristics and treatment history, looking at a 6 week period of hypoglycaemia events and glucose measurements predicts future hypoglycaemia risk.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Hypoglycaemia is an acute complication of diabetes management that may occur as a consequence of insulin or insulin secretagogue therapy [1]. The negative consequences (physical, psychological and behavioural) of hypoglycaemia are a constant source of concern for people treated with these agents and those who provide care for them [2]. For some individuals, fear of hypoglycaemia prevents them from achieving recommended glycaemic targets, increasing their risk of a range of complications [3]. Conversely, fear of hyperglycaemia can lead to over-use of insulin and more frequent hypoglycaemia [4]. A greater understanding of predictors of hypoglycaemia may enable healthcare professionals to better advise people with diabetes how to avoid hypoglycaemia events while also maintaining optimal glycaemic control. Prediction of hypoglycaemia risk could also inform clinical decision making and clinical trial entry criteria or enable hypoglycaemia prevention strategies. Several studies [5,6,7] have identified factors associated with the occurrence of hypoglycaemia events but further understanding of causal relationships between clinical risk factors and, in particular, a range of definitions for hypoglycaemia outcomes, would enable targeted interventions for individuals at increased hypoglycaemia risk.
Hypoglycaemia rates should be, and often are, used as a safety endpoint in clinical trials investigating the effect of glucose-lowering therapies. Accurate identification of the efficacy of different insulins in not only maintaining glycaemic control but also limiting hypoglycaemia is of fundamental importance to people with type 1 diabetes or insulin-treated type 2 diabetes. Consequently, a thorough understanding of hypoglycaemia risk and its predictors across clinical trial participants at baseline could be of interest to evaluate hypoglycaemia events during the trial.
The EU-funded Hypoglycaemia REdefining SOLutions for better liVEs (Hypo-RESOLVE) project brought people with diabetes together with academic, clinical and industry partners with the joint goal of identifying and quantifying predictors and consequences of hypoglycaemia [1]. As part of this initiative a database was created of clinical trial data provided by several pharmaceutical and medical device industry partners, involving people with type 1 or type 2 diabetes in whom data on hypoglycaemia events had been captured during the trial. In this pre-specified analysis, we leveraged this pooled dataset to examine the association of clinical variables collected at study baseline and during the trial with incident hypoglycaemia events and quantified how well the events could be predicted with these data.
Methods
Data and cohort
Trial data from 26 clinical trials involving 12,247 people living with type 1 diabetes and 65 trials involving 34,007 people living with type 2 diabetes were provided by industry partners. All trials involved people with diabetes who were taking glucose-lowering medication with hypoglycaemia risk, mostly insulin. The raw trial data were standardised, harmonised and pooled in a unique hypo-RESOLVE database by the Swiss Institute of Bioinformatics, using the Clinical Data Interchange Consortium (CDISC) Study Data Tabulation Model Implementation Guide (SDTMIG 3.2) format [8] (see electronic supplementary material [ESM] Methods for details). In addition, the bespoke domain XH was created for hypoglycaemia event data, obtained from self-recorded episodes in participants’ diaries and serious adverse event declaration from clinical trials. The trials did not use continuous glucose monitoring (CGM). Some episodes were asymptomatic episodes noted on self-monitored blood glucose that met the agreed thresholds for hypoglycaemia, and some were symptomatic episodes. Level 3 (see below) episodes did not require a blood glucose measurement as this was not part of the definition, although it was often recorded. Some level 3 episodes were derived also from serious adverse event reporting. Each hypoglycaemia event was characterised by an event date, a blood glucose measurement (if available) and self-treatment status.
Despite the availability of raw data from each clinical trial, many trials had idiosyncratic data structures or collection procedures that precluded data harmonisation into the pooled database. These issues resulted in the exclusion of certain individuals and covariates due to the high levels of missingness introduced when integrating the data from these trials. We therefore first excluded individuals who met the following criteria: did not pass trial screening; lacked observation start or end dates; had missing age, sex or diabetes duration information; or had more than 20% missingness for hypoglycaemia event data. A hypoglycaemia event was considered missing if the event lacked a date of occurrence or it lacked a glucose measurement while simultaneously being either denoted as a self-treated event or the self-treatment status was missing.
Definitions of hypoglycaemia
Blood glucose measurements and whether assistance was required to handle each hypoglycaemia event was used to define hypoglycaemia in our analyses, irrespective of each trial’s own definition in the pooled dataset.
The International Hypoglycaemia Study Group (IHSG) [9] proposed three levels of hypoglycaemia that have been accepted recently by the European Medicines Agency (EMA) [10] and, as draft guidance, by the US Food and Drug Administration (FDA) [11]. Currently, these are as follows:
-
Level 1 hypoglycaemia alert events, defined as any event with a recorded blood glucose level of less than 3.9 mmol/l but not less than 3.0 mmol/l
-
Level 2 hypoglycaemia events, defined as any hypoglycaemia event with a recorded blood glucose level below 3.0 mmol/l
-
Level 3 hypoglycaemia events (severe hypoglycaemia), defined as any hypoglycaemia event in which the individual was unable to self-treat due to severe cognitive impairment, irrespective of glucose measurement
Within the pooled clinical trial dataset, level 3 was any event in the XH table that was both symptomatic and not self-treated.
Using these levels, we considered three separate classifications of hypoglycaemia event in our analyses:
-
Level 1 or worse: any hypoglycaemia event meeting the criteria of either level 1, level 2 or level 3
-
Level 2 or worse: any hypoglycaemia event meeting the criteria of either level 2 or level 3
-
Level 3
Candidate covariates
We sought to examine the association of subsequent hypoglycaemia with a wide range of variables that have either been previously reported as associated with hypoglycaemia or for which an association might reasonably be expected and for which data were available in a sufficient number of trials or participants. In addition to age, sex (as reported by the investigator of the clinical trial) and diabetes duration we considered the following candidate covariates in our analysis: total daily insulin dose; insulin regimen (basal, basal bolus, or premix); insulin origin (human vs analogue); self-monitored blood glucose; variability based on self-monitored blood glucose; HbA1c; eGFR as defined by the CKD-EPI equation [12]; systolic BP; diastolic BP; medical history of complications of diabetes (CVD, retinopathy, neuropathy, nephropathy); total cholesterol; LDL-cholesterol; HDL-cholesterol; triglycerides; BMI; ethnicity; and use of concomitant medications (glucose-lowering drugs, antihypertensives, systemic antibiotics, systemic oral anti-inflammatory agents, psychoactive agents, sex hormones, anti-epilepsy drugs, antithyroid drugs, cessation of systemic steroids).
Medical history covariates were defined by relevant Medical Dictionary for Regulatory Activities (MedDRA) terms and drug categories were defined using ATC codes (ESM Tables 1, 2).
Since we considered that an individual’s recent history of hypoglycaemia was likely to be an important predictor of future hypoglycaemia events, and since this information would ordinarily be available in a clinical setting, we used the first 6 weeks following the date of randomisation into their clinical trials (an arbitrary minimum time period in which to estimate a typical hypoglycaemia baseline) to obtain measures of baseline hypoglycaemia incidence, baseline blood glucose and blood glucose variability for each participant. Follow-up time and events after this first 6 weeks were then used in the evaluation of associations and predictions. A simple hypoglycaemia score was arbitrarily defined as the weighted sum of the number of level 1, 2 and 3 hypoglycaemia event counts in a 6 week period, with a 1:2:3 ratio between level 1, 2 and 3 event counts, respectively. Since the hypoglycaemia score was estimated after randomisation, the independent effect of the randomised insulin origin and regimen was not distinguishable in multivariate models.
Blood glucose variability was characterised by the CV calculated as the ratio of the SD to the mean of blood glucose within a 6 week time interval, as the CV is one of the most commonly used measures of this variable.
Missingness, evaluability and imputation
All continuous covariates were categorised as either having an evaluable continuous value or as being missing. For covariates such as sex and ethnicity, the covariate was either considered evaluable or missing. For drug exposure and medical history covariates, if at least one person in a given trial had the covariate recorded we considered all the participants in that trial to be evaluable for these covariates, otherwise we regarded the covariates as non-evaluated in a given trial.
Covariates were imputed on a per-trial basis using the R package Amelia (version 1.7.6; https://cran.r-project.org/web/packages/Amelia/index.html), provided the covariate was present for at least 80% of participants in that trial.
Statistical methods
Data set-up
We structured our data in a longitudinal format, with time slices of 6 weeks. Time was measured relative to the entry date of each individual. Individuals exited the study at the earliest of the end of participation in the clinical trial or date of death.
Rates of hypoglycaemia
We first examined how much heterogeneity there was in the crude incidence rates of hypoglycaemia events at the three levels across clinical trials. A large degree of heterogeneity was expected given the varying entry criteria across trials and this had important implications for the potential of confounding of association by trial number.
Minimally adjusted associations with hypoglycaemia
To quantify the association of a range of clinical covariates with each hypoglycaemia outcome, we used multivariate generalised linear mixed models (GLMMs). For each analysis, the number of hypoglycaemia events experienced by an individual during a time slice was the measured outcome. We employed a Poisson mixed model for our analysis with random intercept for individual to account for any over-dispersion since the count of hypoglycaemia events is time-updated. This is as opposed to negative-binomial regression, which erroneously assumes that observations across individuals are exchangeable.
All analyses were performed for type 1 and type 2 diabetes separately. Separate GLMMs, adjusted for age, sex and diabetes duration, for participants with known insulin regimen were fit to investigate the adjusted association of each candidate covariate after imputation. We adjusted models for study identifier to account for confounding due to different trial entry criteria and populations. The covariate value for the first 6 weeks from study entry was used in the models, with only events after this time being considered in the analysis. The hypoglycaemia event rate was assumed to be constant across time slices for the same participant.
Prediction modelling
For multivariate prediction modelling, further exclusion criteria to the cohort were applied for each analysis separately. We dropped the following from consideration in our analysis: participants with unknown insulin regimen; any covariates with more than 20% missingness; any individual who had missingness in any retained candidate covariate; and concomitant medications where less than 5% of individuals were recorded as using them. We also dropped all participants in studies where there were 15 or fewer hypoglycaemia events in total across the study of the level corresponding to the outcome of the specific analysis, as such trials had too little information to contribute to the model. Data were partitioned in a 70:30 training:test split stratified by trial.
The prediction task was to predict the number of hypoglycaemia events from start of study (6 weeks post-randomisation) to end of study.
For each hypoglycaemia outcome, we fitted three models: (1) a baseline model that included age, sex, diabetes duration and study identifier; (2) a baseline model also including the hypoglycaemia score; and (3) a full model (also including the hypoglycaemia score). For the full model, all covariates meeting missingness criteria, separately for type 1 and type 2 diabetes, were included from the candidate set. In all models, the participant was included as a random effect.
Although our models predicted the number of hypoglycaemia events, for summarisation purposes the AUC for the binary outcome of the number of hypoglycaemia events at the threshold of being more or less than the 90th centile within the trial was computed. Prediction modelling included 18 models (two diabetes cohorts, three prediction outcomes and three comparator model types).
XGBoost implements a tree-based gradient boosting algorithm to fit predictive models [13]. We fitted XGBoost models using the training split to perform a threefold cross-validation grid-search (parameters are given in ESM Methods). The selected model was then evaluated on the test split where test log(likelihood) and AUC were evaluated. The difference in test log(likelihood) between two models provided the strength of evidence that one model had greater predictive performance than the other; a difference in test log(likelihood) of 6.9 natural log units is asymptotically equivalent to a p value less than 0.005 for comparison of nested models [14].
Results
Data availability
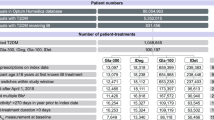
The data, after exclusion criteria, consisted of 46,254 individuals with 31,577 person-years observed (mean follow-up of 0.68 years), with data collected from 90 unique trials. There were 12,247 participants with type 1 diabetes from 26 clinical trials and 34,007 participants with type 2 diabetes from 65 trials. During follow-up, there was a total of 841,401 (approximately 88 per person-year) and 309,655 (approximately 14 per person-year) level 1 or worse hypoglycaemia events in the type 1 and type 2 diabetes cohorts, respectively. For level 2 or worse, there were 334,086 (approximately 35 per person-year) and 76,987 (approximately three per person-year) hypoglycaemia events in the type 1 and type 2 diabetes cohorts, respectively. For level 3 hypoglycaemia, there were 4719 (approximately 0.49 per person-year) and 3414 (approximately 0.15 per person-year) events in the type 1 and type 2 diabetes cohorts, respectively.
Cohort characteristics are presented in Tables 1 and 2, separated by type of diabetes, and provide numbers of evaluable participants after imputation for each covariate.
ESM Tables 3–8 show the covariates considered for inclusion in multivariate prediction models, including those specifically included for each hypoglycaemia classification.
Hypoglycaemia event rates
Rates of hypoglycaemia varied between trials, as shown for each hypoglycaemia level in ESM Figs 1, 2. For example, for type 1 diabetes, of trials where a level 3 hypoglycaemia event was recorded, the median hypoglycaemia event rate was 20.5 events/100 participants per year and the highest rate was 409 events/100 participants per year. For type 2 diabetes, the median level 3 hypoglycaemia event rate was 4.8 events/100 participants per year and the highest rate was 850.7 events/100 participants per year (individuals from this trial did not contribute to further analyses for level 3 outcomes; the next highest rate was 186.7 events/100 participants per year). Due to this high variability between trials all analyses were adjusted by trial.
Minimally adjusted associations with hypoglycaemia
For type 1 diabetes, the number of people with available data ranged between 7613 and 12,247. Power was greatest to detect associations with total events overall since the numbers of level 2 and level 3 hypoglycaemia events were much lower than for level 1. As shown in Table 3, the following were associated with greater frequency of hypoglycaemia overall (level 1 or worse) and with at least a consistent direction of effect for the more severe levels; female sex; longer diabetes duration; lower HbA1c; greater self-monitored glucose and glucose variability; higher score for hypoglycaemia across the 6 week baseline period; using human rather than analogue only insulin; lower BMI; lower diastolic BP; lower total cholesterol; lower triglycerides; and use of anti-inflammatory and psychoactive drugs. Black or African American ethnicity was associated with fewer hypoglycaemia events than White ethnicity. Those with more complications had fewer hypoglycaemic events, though for level 3 the data were too sparse and the directions inconsistent with that for events overall. A lower insulin dose at the end of the baseline period was associated with more subsequent hypoglycaemia events in this minimally adjusted analysis.
For type 2 diabetes, the number of people with available covariate data ranged between 24,900 and 34,007. As shown in Table 4, the following covariates were associated with more hypoglycaemia events overall (level 1 or worse) and with at least a consistent direction of effect for more severe levels: older age; female sex; longer diabetes duration; more glucose variability; higher score for hypoglycaemia across the 6 week baseline period; use of human rather than analogue only insulin; use of premix or basal bolus rather than basal insulin; lower eGFR; lower systolic and diastolic BP; lower total cholesterol; lower triglycerides; using concomitant oral glucose-lowering drugs; and exposure to other drug classes including psychoactive drugs. Black ethnicity, African American ethnicity and ethnicity other than White was associated with fewer hypoglycaemia events than White ethnicity.
Thus the main difference in direction in these minimally adjusted associations when comparing type 1 diabetes with type 2 diabetes were associations with more of the examined drug classes in type 2 diabetes where such concomitant use was more frequent. Since these associations were minimally adjusted, they were descriptive rather than necessarily indicative of causality.
See ESM Tables 9 and 10 for associations between risk factors and hypoglycaemia where missing data was not imputed.
Prediction modelling
Here the goal was to evaluate how risk factor status at baseline predicted the hypoglycaemia risk across the duration of the trial. The final numbers of individuals in training and testing after exclusion for missingness are shown in Table 5.
Prediction of any hypoglycaemia event of any severity was greater than for more sparse events requiring assistance (level 3 hypoglycaemia) in both types of diabetes (Tables 6, 7). For prediction of level 1 or worse hypoglycaemia during the whole follow-up period, the AUC with the full model was 0.835 (0.826, 0.844) in type 1 diabetes and was 0.840 (0.831, 0.848) in type 2 diabetes. For level 3 hypoglycaemia the AUC was lower, at 0.689 (0.667, 0.712) for type 1 diabetes and 0.705 (0.662, 0.748) for type 2 diabetes. As shown in Tables 6 and 7, the increment in AUC compared with the baseline model was substantial when the score for hypoglycaemia in the 6 week baseline phase was included with the other covariates in the full model, contributing a little more. This was confirmed by the XGBoost importance procedure on the full models shown in Tables 8 and 9. The calculated ‘gain’ measure from this procedure captured the relative importance of inclusion of a given covariate to improving model fit.
Discussion
The Hypo-RESOLVE database brought together a large volume of prospective data on hypoglycaemia in type 1 and type 2 diabetes from clinical trials of glucose-lowering agents. The dataset is one of the largest reported to date for examining risk factors and prediction of hypoglycaemia. We show that many factors associated with having greater frequency of hypoglycaemia are common to type 1 and type 2 diabetes. Of particular note is a consistent finding that there is a higher rate of hypoglycaemia in the female sex than in the male sex for both type of diabetes. Ethnic differences were also observed that deserve further exploration and confirmation in other datasets. In both type 1 and type 2 diabetes a higher rate of hypoglycaemia was observed in individuals using human insulin, either alone or combined, than in those using analogue only insulin.
More drug categories were associated with more hypoglycaemia in type 2 diabetes than in type 1 diabetes. Furthermore, lower eGFR was associated with greater frequency of hypoglycaemia in type 2 diabetes. In both types of diabetes use of psychotropic drugs was associated with more hypoglycaemia events suggesting that careful consideration of the need for such drugs is warranted in those experiencing frequent or severe hypoglycaemia. Greater self-monitored glucose variability and more recent hypoglycaemia were also associated with the prospective risk of hypoglycaemia in both type 1 and type 2 diabetes. An association between lower insulin dose at the end of the baseline data collection period of weeks 1 to 6 and subsequent hypoglycaemia may be expected due to dose adjustments in response to a higher incidence of hypoglycaemia events during this period.
The multivariate analyses showed that future hypoglycaemia risk was highly predictable and that almost all of this prediction is obtainable from an individual’s recent hypoglycaemia history rather than these other associated characteristics. These data suggest that a formal prediction model would be unnecessary since recent history of hypoglycaemia is usually available from patients and their healthcare professionals. However, our data provide validation of the methodology and highlight potentially modifiable risk factors, including choice of insulin and concurrent medications, that should be considered in attempts to ameliorate hypoglycaemia risk.
Comparison with existing literature
Our study differs from many in being larger, involving a population drawn from clinical trials and, importantly, using a consistent set of definitions of hypoglycaemia. Our data replicate some well-recognised associations for hypoglycaemia, validating our methodology, such as worse hypoglycaemia risk with longer diabetes duration [15] and less frequent hypoglycaemia with insulin analogue [16,17,18,19,20]. Associations with less frequent hypoglycaemia with insulin in our study is not explained by differences in diabetes duration since within trial duration was similar, reflecting the randomisation, and since our method of analysis is akin to summarising the within-trial associations across all trials. The link between impaired renal function in type 2 diabetes is also widely reported [21, 22]. Links between polypharmacy and increased hypoglycaemia risk in people with type 2 diabetes are well described and may be driven both by increasing frailty and interactions between therapeutic agents themselves [23]. The link with non-steroidal anti-inflammatory drug use is interesting. Some drugs of this class are recognised to cause hypoglycaemia through a mechanism that may involve modulation of ion channel activities, either in the pancreatic beta cell or central nervous system glucose-sensing neurons [24]. Our data are consistent with reports of increased hypoglycaemia risk for the female sex in cohorts including both diabetes types [25, 26] and in type 2 diabetes cohort s [27,28,29,30], although, conversely, a small number of studies of cohorts including both diabetes types report the male sex to be at increased risk of hypoglycaemia [31,32,33]. A possible explanation for increased hypoglycaemia risk for the female sex is that they have less pronounced counterregulatory response during experimental hypoglycaemia than the male sex [34]. There could also be a differential distribution between sexes in other unmeasured confounders, such as comorbidities or concurrent medications, that could affect hypoglycaemia risk. Other factors determining trial participation (e.g. socioeconomic status) may confound the ethnicity association we found and thus this warrants further investigation.
It is worth noting that in both types of diabetes greater glucose variability was clearly a risk factor for more frequent hypoglycaemia. The existing literature supports an association between increased glucose variability and increased hypoglycaemia risk [35, 36]. However, the literature for HbA1c and hypoglycaemia risk is controversial as multiple studies report an association between low HbA1c and increased risk [27, 37,38,39], and multiple studies report no association [40,41,42,43,44]. A 6 week history of increased hypoglycaemia frequency was the most important predictive factor, as expected, and is consistent with cohorts including both types of diabetes [45,46,47,48] and type 2 diabetes cohort s [40, 48,49,50].
We found rates of level 3 hypoglycaemia that were lower than US-based estimates from ambidirectional panel survey data [51] but higher than estimates from Scotland for rates of hypoglycaemia requiring emergency medical treatment [52]
Limitations of this analysis
The use of trial data allowed us to bring together a large dataset wherein hypoglycaemia of differing severity level was well characterised and captured, unlike in many population studies. However, it also presented several challenges. A substantial challenge was that the trials represented very different subpopulations, with prior severe hypoglycaemia within 12 months being an exclusion criteria in many trials. Widely varying incidence rates for all levels of hypoglycaemia necessitated the study number being required as a covariate in the analysis to avoid confounding by study entry criteria. Absolute rates of hypoglycaemia within these trials cannot be generalised, although useful information on predictors of hypoglycaemia remain despite the intervention setting of these trials. Furthermore while we had good capture of many important variables, several variables that would be of interest to examine in relation to hypoglycaemia, such as C-peptide levels in type 1 diabetes [42], were not available in these trials. There was a high level of missingness for some variables requiring imputation. Other variables, such as late diabetic complication status, were only crudely assessed as present/absent and not all trials routinely captured all concurrent medications.
Finally, trial entrants were not necessarily representative of the general population living with diabetes and, while this limits the generalisability of the observed incidence rates of hypoglycaemia and sociodemographic features that might be confounded by association with other determinants of hypoglycaemia, it is likely that among trial participants the relationship between most clinical characteristics and hypoglycaemia is preserved.
Conclusions
The key findings from this large study are generalisable: a small number of variables along with recent hypoglycaemia rate over a 6 week period provide the level of prediction of future hypoglycaemia at varying levels of severity that would be useful in several settings; and other associated clinical characteristics add little to prediction over the time horizon we studied. Such settings might include selection of people with diabetes into clinical trials, raising alerts as to high risks that require immediate mitigation. or prioritising those to be given scarce resources such as CGM or semi-closed/closed loop systems. Finally, the data reinforce our view that careful capture and consideration of recent hypoglycaemia history and review of glucose monitoring data and modifiable risk factors are fundamental to providing good clinical care in diabetes.
Abbreviations
- CGM:
-
Continuous glucose monitoring
- GLMM:
-
Generalised linear mixed model
- Hypo-RESOLVE:
-
Hypoglycaemia REdefining SOLutions for better liVEs
References
de Galan BE, McCrimmon RJ, Ibberson M et al (2020) Reducing the burden of hypoglycaemia in people with diabetes through increased understanding: Design of the hypoglycaemia redefining solutions for better liVEs (hypo-resolve) project. Diabetic Medicine 37:1066–1073. https://doi.org/10.1111/dme.14240
Amiel SA (2021) The consequences of hypoglycaemia. Diabetologia 64:963–970. https://doi.org/10.1007/s00125-020-05366-3
Fidler C, Christensen TE, Gillard S (2011) Hypoglycaemia: an overview of fear of hypoglycemia, quality- of-life, and impact on costs. J Med Econ 14:646–655. https://doi.org/10.3111/13696998.2011.610852
Lin YK, Richardson CR, Dobrin I et al (2022) Beliefs around hypoglycemia and their impacts on hypoglycemia outcomes in individuals with type 1 diabetes and high risks for hypoglycemia despite using advanced diabetes technologies. Diabetes Care 45:520–528. https://doi.org/10.2337/dc21-1285
McCoy RG, Lipska KJ, Van Houten HK, Shah ND (2020) Association of cumulative multimorbidity, glycemic control and medication use with hypoglycemia-related emergency department visits and hospitalizations among adults with diabetes. JAMA Netw Open 3:e1919099–e1919099. https://doi.org/10.1001/jamanetworkopen.2019.19099
Silbert R, Salcido-Montenegro A, Rodriguez-Gutierrez R et al (2018) Hypoglycemia among patients with type 2 diabetes: epidemiology, risk factors, and prevention strategies. Diabetes Epidemiol 18. https://doi.org/10.1007/s11892-018-1018-0
Weinstock RS, DuBose SN, Bergenstal RM et al (2015) Risk factors associated with severe hypoglycemia in older adults with type 1 diabetes. Diabetes Care 39:603–610. https://doi.org/10.2337/dc15-1426
Clinical Data Interchange Standards Consortium (2013) CDISC study data tabulation model implementation guide: human clinical trials version 3.2. Available from https://www.cdisc.org/standards/foundational/sdtmig/sdtmig-v3-2. Accessed 08 June 2023
International Hypoglycameia Study Group (2017) Glucose concentrations of less than 3.0 mmol/l (54 mg/dL) should be reported in clinical trials: A joint position statement of the american diabetes association and the european association for the study of diabetes. Diabetes Care 40:155–157. https://doi.org/10.2337/dc16-2215
Committee for Medicinal Products for Human Use (2023) Guideline on clinical investigation of medicinal products in the treatment or prevention of diabetes mellitus. Available from https://ema.europa.eu/en/documents/scientific-guideline/guideline-clinical-investigation-medicinal-products-treatment-prevention-diabetes-mellitus-revision_en-0.pdf. Accessed 08 June 2023
Food and Drug Administration Center for Drug Evaluation and Research (2023) Diabetes mellitus: Efficacy endpoints for clinical trials investigating antidiabetic drugs and biological products guidance for industry. Draft guidance. Available from https://fda.gov/media/168475/download. Accessed 27 July 2023
Pattaro C, Riegler P, Stifter G et al (2013) Estimating the glomerular filtration rate in the general population using different equation: effects on classification and association. Nephron Clin Pract 123:102–11. https://doi.org/10.1159/000351043
Chen T, Guestrin C (2016) XGBoost: A scalable tree boosting system. In: Proceedings of the 22nd ACM SIGKDD International Conference On Knowledge Discovery And Data Mining. ACM, New York, NY, USA, pp 785–794
Stone M (1977) An asymptotic equivalence of choice of model by cross-validation and Akaike’s criterion. J R Stat Soc Ser B (Methodological) 39:44–47. https://doi.org/10.1111/j.2517-6161.1977.tb01603.x
Weinstock RS, Xing D, Maahs DM et al (2013) Severe hypoglycemia and diabetic ketoacidosis in adults with type 1 diabetes: results from the T1D Exchange clinic registry. J Clin Endocrinol Metab 98:3411–3419. https://doi.org/10.1210/jc.2013-1589
Rys P, Wojciechowski P, Rogoz-Sitek A et al (2015) Systematic review and meta-analysis of randomized clinical trials comparing efficacy and safety outcomes of insulin glargine with NPH insulin, premixed insulin preparations or with insulin detemir in type 2 diabetes mellitus. Acta Diabetol 52:649–662. https://doi.org/10.1007/s00592-014-0698-4
Mullins P, Sharplin P, Yki-Jarvinen H et al (2007) Negative binomial meta-regression analysis of combined glycosylated hemoglobin and hypoglycemia outcomes across eleven Phase III and IV studies of insulin glargine compared with neutral protamine Hagedorn insulin in type 1 and type 2 diabetes mellitus. Clin Ther 29:1607–1619. https://doi.org/10.1016/j.clinthera.2007.08.020
Bazzano LA, Lee LJ, Shi L et al (2008) Safety and efficacy of glargine compared with NPH insulin for the treatment of Type 2 diabetes: a meta-analysis of randomized controlled trials. Diabet Med 25:924–932. https://doi.org/10.1111/j.1464-5491.2008.02517.x
Monami M, Marchionni N, Mannucci E (2008) Long-acting insulin analogues versus NPH human insulin in type 2 diabetes: a meta-analysis. Diabetes Res Clin Pract 81:184–189. https://doi.org/10.1016/j.diabres.2008.04.007
Caeiro G, Romero SA, Solis SE et al (2020) Type 2 diabetes. Prevalence of hypoglycemia in public versus private health care system. Medicina (B Aires) 80:203–210
Zoungas S, Patel A, Chalmers J et al (2010) Severe hypoglycemia and risks of vascular events and death. N Engl J Med 363:1410–1418. https://doi.org/10.1056/NEJMoa1003795
WisitKaewput RR, Thongprayoon Charat, Cheungpasitporn W (2020) Incidence and risk factors associated with outpatient hypoglycemia in patients with type 2 diabetes and chronic kidney disease: a nationwide study. Endocr Res 45:217–225. https://doi.org/10.1080/07435800.2020.1792921
Freeman J (2019) Management of hypoglycemia in older adults with type 2 diabetes. Postgrad Med 131:241–250. https://doi.org/10.1080/00325481.2019.1578590
Li J, Zhang N, Ye B et al (2007) Non-steroidal anti-inflammatory drugs increase insulin release from beta cells by inhibiting ATP-sensitive potassium channels. Br J Pharamcol 151:483–493. https://doi.org/10.1038/sj.bjp.0707259
Haukka J, Hoti F, Erästö P et al (2013) Evaluation of the incidence and risk of hypoglycemic coma associated with selection of basal insulin in the treatment of diabetes: a Finnish register linkage study. Pharmacoepidemiol Drug Saf 22:1326–1335. https://doi.org/10.1002/pds.3534
Galindo RJ, Ali MK, Funni SA et al (2022) Hypoglycemic and hyperglycemic crises among U.S. Adults with diabetes and end-stage kidney disease: population-based study, 2013–2017. Diabetes Care 45:100–107. https://doi.org/10.2337/dc21-1579
Huang B, Jiang Q, Wu T et al (2022) Hypoglycemia unawareness identified by continuous glucose monitoring system is frequent in outpatients with type 2 diabetes without receiving intensive therapeutic interventions. Diabetol Metab Syndr 14:180. https://doi.org/10.1186/s13098-022-00959-x
Lee SE, Kim KA, Son KJ et al (2021) Trends and risk factors in severe hypoglycemia among individuals with type 2 diabetes in Korea. Diabetes Res Clin Pract 178:108946. https://doi.org/10.1016/j.diabres.2021.108946
Li P, Geng Z, Ladage VP et al (2019) Early hypoglycaemia and adherence after basal insulin initiation in a nationally representative sample of Medicare beneficiaries with type 2 diabetes. Diabetes Obes Metab 21:2486–2495. https://doi.org/10.1111/dom.13832
Rathmann W, Charbonnel B, Gomes MB et al (2020) Socioeconomic factors associated with hypoglycaemia in patients starting second-line glucose-lowering therapy: the DISCOVER study. Diabetes Res Clin Pract 165:108250. https://doi.org/10.1016/j.diabres.2020.108250
Guzmán G, Martínez V, Yara JD et al (2020) Glycemic control and hypoglycemia in patients treated with insulin pump therapy: an observational study. J Diabetes Res 2020:1581726. https://doi.org/10.1155/2020/1581726
Jensen MH, Hejlesen O, Vestergaard P (2021) Epidemiology of hypoglycaemic episodes leading to hospitalisations in Denmark in 1998–2018. Diabetologia 64:2193–2203. https://doi.org/10.1007/s00125-021-05507-2
McCoy RG, Galindo RJ, Swarna KS et al (2021) Sociodemographic, clinical, and treatment-related factors associated with hyperglycemic crises among adults with type 1 or type 2 diabetes in the US from 2014 to 2020. JAMA Netw Open 4:e2123471. https://doi.org/10.1001/jamanetworkopen.2021.23471
Diamond MP, Jones T, Caprio S et al (1993) Gender influences counterregulatory hormone responses to hypoglycemia. Metabolism 42:1568–1572. https://doi.org/10.1016/0026-0495(93)90152-E
Long C, Tang Y, Huang J et al (2022) Association of long-term visit-to-visit variability of HbA1c and fasting glycemia with hypoglycemia in type 2 diabetes mellitus. Front Endocrinol (Lausanne) 13:975468. https://doi.org/10.3389/fendo.2022.975468
DeVries JH, Bailey TS, Bhargava A et al (2019) Day-to-day fasting self-monitored blood glucose variability is associated with risk of hypoglycaemia in insulin-treated patients with type 1 and type 2 diabetes: a post hoc analysis of the SWITCH Trials. Diabetes Obes Metab 21:622–630. https://doi.org/10.1111/dom.13565
Chalew S, Kamps J, Jurgen B et al (2020) The relationship of glycemic control, insulin dose, and race with hypoglycemia in youth with type 1 diabetes. J Diabetes Complications 34:107519. https://doi.org/10.1016/j.jdiacomp.2019.107519
Ling Q, Lu J, Li X et al (2020) Value of capillary glucose profiles in assessing risk of nocturnal hypoglycemia in type 1 Diabetes Based on Continuous Glucose Monitoring. Diabetes Ther 11:915–925. https://doi.org/10.1007/s13300-020-00787-0
Hong S, Presswala L, Harris YT et al (2020) Hypoglycemia in patients with type 2 diabetes mellitus and chronic kidney disease: a prospective observational study. Kidney 360(1):897–903. https://doi.org/10.34067/KID.0001272020
Chantzaras A, Yfantopoulos J (2022) Evaluating the incidence and risk factors associated with mild and severe hypoglycemia in insulin-treated type 2 diabetes. Value Health Reg Issues 30:9–17. https://doi.org/10.1016/j.vhri.2021.10.005
Chen NC, Chen CL, Shen FC (2022) The risk factors of severe hypoglycemia in older patients with dementia and type 2 diabetes mellitus. J Pers Med 12. https://doi.org/10.3390/jpm12010067
Jeyam A, Colhoun H, McGurnaghan S et al (2021) Clinical impact of residual C-peptide secretion in type 1 diabetes on glycemia and microvascular complications. Diabetes Care 44:390–398. https://doi.org/10.2337/dc20-0567
Takagi S, Miura J, Takita M et al (2022) Factors associated with hypoglycemia unawareness and severe hypoglycemia in type 1 diabetes mellitus patients. J Diabetes Investig 13:2018–2026. https://doi.org/10.1111/jdi.13886
Wan H, Wen B, Wang X et al (2021) Effect of baseline characteristics on hypoglycaemia risk with insulin glargine 100 U/mL: post hoc analysis of the BEYOND 7 study. Diabetes Ther 12:2359–2369. https://doi.org/10.1007/s13300-021-01112-z
Beck RW, Bergenstal RM, Riddlesworth TD et al (2018) Validation of time in range as an outcome measure for diabetes clinical trials. Diabetes Care 42:400–405. https://doi.org/10.2337/dc18-1444
Gubitosi-Klug RA, Braffett BH, White NH et al (2017) Risk of severe hypoglycemia in type 1 diabetes over 30 years of follow-up in the DCCT/EDIC study. Diabetes Care 40:1010–1016. https://doi.org/10.2337/dc16-2723
Jeon JY, Kim SR, Kim HJ et al (2016) Risk factors of severe hypoglycemia requiring medical assistance and neurological sequelae in patients with diabetes: a case-control study. Medicine (Baltimore) 95:e5365
Iwase M, Komorita Y, Fujii H et al (2020) Incidence of severe hypoglycemia and its association with serum adiponectin in japanese patients with type 1 and insulin-treated type 2 diabetes: The Fukuoka Diabetes Registry. J Diabetes Investig 11:1258–1264. https://doi.org/10.1111/jdi.13253
Festa A, Heller SR, Seaquist E et al (2017) Association between mild and severe hypoglycemia in people with type 2 diabetes initiating insulin. J Diabetes Complications 31:1047–1052. https://doi.org/10.1016/j.jdiacomp.2016.12.014
Zhong VW, Juhaeri J, Cole SR et al (2018) Hba1c variability and hypoglycemia hospitalization in adults with type 1 and type 2 diabetes: a nested case-control study. J Diabetes Complications 32:203–209. https://doi.org/10.1016/j.jdiacomp.2017.10.008
Ratzki-Leewing A, Black JE, Kahkoska AR et al (2023) Severe (level 3) hypoglycaemia occurrence in a real-world cohort of adults with type 1 or type 2 diabetes mellitus (iNPHORM, united states). Diabetes Obes Metab 25:3736–3747. https://doi.org/10.1111/dom.15268
Wang H, Donna PT, Leese CJ et al (2017) Temporal changes in frequency of severe hypoglycaemia treated by emergency medical services in types 1 and 2 diabetes: a population-based data-linkage cohort study. Clin Diabetes Endocrinol 3:7. https://doi.org/10.1186/s40842-017-0045-0
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Data availability
The data underlying the results presented in the study come from the Hypo-RESOLVE data repository, which will be maintained for a 2 year period following the end of the Hypo-RESOLVE project. Enquiries about third-party researcher data access and associated access criteria should be sent to the Hypo-RESOLVE data access committee (Jakob Haardt J.Haardt@eurice.eu / Mark Ibberson Mark.Ibberson@sib.swiss; or via https://hypo-resolve.eu/contact).
Funding
This project has received funding from the Innovative Medicines Initiative 2 Joint Undertaking (JU) under grant agreement no. 777460. The JU receives support from the European Union’s Horizon 2020 research and innovation programme and the European Federation of Pharmaceutical Industries and Associations and T1DExchange, JDRF, International Diabetes Federation and Helmsley Charitable Trust. The industry partners supporting the JU include Abbott Diabetes Care, Eli Lilly, Medtronic, Novo Nordisk and Sanofi-Aventis. Results reflects only the authors’ views and JU is not responsible for any use that may be made of the information it contains. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Authors’ relationships and activities
HMC has research grants from JDRF and Diabetes UK. She has participated in a speakers bureau, on an advisory board for Novo Nordisk, on an advisory panel for Bayer AG, and is a shareholder of Roche Pharmaceuticals and Bayer AG. SH has participated on advisory boards for Eli Lilly and Novo Nordisk and on a speakers bureau for Novo Nordisk and has received honorarium via his institution from Medtronic. He has consulted for Vertex Pharma, Zucara Pharmaceuticals and Zealand Pharma. AS is an employee of, and holds shares in, Novo Nordisk. UP-B received personal honorarium for lectures, presentations and expert testimony from Sanofi and Novo Nordisk and is a member of the editorial board of Diabetologia. BEdG is a member of the editorial board of Diabetologia. RJM received personal honorarium for lectures, and presentations from Sanofi and Novo Nordisk, and support for travel to lecture at an educational event from Sanofi. He is a non-executive member of NHS Tayside Health Board. MR is an employee of, and holds shares in, Eli Lilly and Company. SAA has served on Advisory Boards for Vertex Pharmaceuticals and spoken at educational events sponsored by Sanofi and Novo Nordisk. M-AG is an employee of, and holds shares in, Novo Nordisk. All other authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
BEdG, UP-B, M-AG, MR, SAA, SH, JL, YQ, RJM, PMM and HMC contributed to the initial analysis plan, including the literature review on important risk factors of hypoglycaemia, that informed this analysis. DK, AS and MI were involved in data cleaning, harmonisation, quality control and databasing of the data. JM coded the data analysis. BEdG, UP-B, M-AG, MR, SAA, SH, JL, YQ, RJM, SM, LB, WB, PMM and HMC contributed to the interpretation of the data. JM and HMC drafted the initial manuscript. All authors made critically important contributions to manuscript revision and all authors approved the final version. HMC is the guarantor and, as such, is responsible for the integrity of the work as a whole.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mellor, J., Kuznetsov, D., Heller, S. et al. Risk factors and prediction of hypoglycaemia using the Hypo-RESOLVE cohort: a secondary analysis of pooled data from insulin clinical trials. Diabetologia (2024). https://doi.org/10.1007/s00125-024-06177-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00125-024-06177-6