Abstract
Aims/hypothesis
Previous studies have suggested that glucose variability may accelerate atherosclerosis progression in people with type 2 diabetes. Current guidelines recommend assessing glycaemic control using continuous glucose monitoring (CGM), which provides a comprehensive glycaemic profile to supplement HbA1c measurement. However, the association between CGM-derived metrics and atherosclerosis progression is not entirely clear.
Methods
This exploratory study used baseline data and data obtained after 104 weeks from an ongoing prospective, multicentre, observational study. Six hundred study participants with type 2 diabetes and no apparent history of symptomatic cardiovascular disease underwent CGM and ultrasonographic atherosclerosis measurements of the carotid arteries, including the intima–media thickness (IMT) and grey-scale median (GSM), at baseline and 104 weeks. Non-invasive ultrasonic tissue characterisation of the carotid artery wall or plaque using the GSM reflects vascular composition. Multivariate regression models were used to analyse the association between CGM-derived indices, mainly time in range (TIR) and CV, and changes in carotid atherosclerosis index values.
Results
Over the 104-week study period, there were modest increases in mean IMT (from 0.759±0.153 to 0.773±0.152 mm, p<0.001) and thickened-lesion GSM (from 43.5±19.5 to 53.9±23.5 units, p<0.001), but no significant changes in common carotid artery maximum-IMT (from 1.109±0.442 to 1.116±0.469 mm, p=0.453) or mean GSM (from 48.7±19.3 to 49.8±20.8 units, p=0.092). In a linear regression model with adjustment for possible atherosclerotic risk factors, including HbA1c, TIR and CV at baseline were significantly associated with the annual change in mean GSM (regression coefficient per 10% increase in TIR 0.52; 95% CI 0.06, 0.98; Hochberg-adjusted p value 0.038; regression coefficient per 1% increase in CV −0.12; 95% CI −0.22, −0.02; Hochberg-adjusted p value 0.038). TIR and CV at baseline were also significantly associated with the annual change in thickened-lesion GSM (regression coefficient per 10% increase in TIR 0.95; 95% CI 0.12, 1.79; Hochberg-adjusted p value 0.038; regression coefficient per 1% increase in CV −0.19; 95% CI −0.36, −0.01; Hochberg-adjusted p value 0.038). Participants who achieved target CGM-derived metrics at baseline, as proposed by an international consensus, showed significant annual changes in mean GSM compared with those who did not (0.94±6.88 vs −0.21±6.19 units/year, p=0.007).
Conclusions/interpretation
TIR and CV were significantly associated with changes in the tissue characteristics of the carotid artery wall.
Trial registration
University Hospital Medical Information Network Clinical Trials Registry, number UMIN000032325
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Type 2 diabetes is an independent risk factor for CVD, which is a major cause of death [1]. Given that the main cause of diabetic complications is damage to tissues and organs caused by persistent hyperglycaemia [2], achieving optimal glycaemic control is important to prevent the development and progression of CVD in people with this condition.
HbA1c is the gold standard for assessing glycaemic control. Current guidelines developed by the ADA, the EASD and the Japan Diabetes Society have set an HbA1c control target of less than 7% (53 mmol/mol) for optimal diabetes management [3,4,5,6]. However, the ADA and EASD guidelines specify that HbA1c has a number of limitations [6, 7]. While some studies have demonstrated strong associations between HbA1c levels and diabetic complications [8, 9], several large clinical trials have failed to show that intensive glycaemic control based on HbA1c has beneficial effects on CVD onset in people with type 2 diabetes [10,11,12]. This is most likely because HbA1c does not provide information on all glycaemic abnormalities that may play an important role in the development of CVD, such as glucose variability [13] and hypoglycaemia [14], although to our knowledge no prospective intervention studies have examined the relationship between glucose variability and CVD. Continuous glucose monitoring (CGM) has emerged as the optimal method to obtain a comprehensive glycaemic profile that includes such data. In particular, the consensus report by ADA and EASD recommended that assessments of glycaemic control include not only HbA1c measurement but also time in range (TIR), defined as the percentage of the time spent within the target glucose range, because TIR is a useful metric of glycaemic control [6, 7].
Importantly, a recent cohort study in 6225 people with diabetes demonstrated that lower TIR assessed by CGM during hospitalisation was associated with an increased risk of all-cause and CVD mortality during a median follow-up of 6.9 years [15]. In addition, cross-sectional studies have demonstrated that TIR and/or glucose variability metrics are significantly associated with carotid artery intima–media thickening [16], the tissue characteristics of the carotid artery wall [17] and arterial stiffness [18, 19]. However, the association of TIR and glucose variability metrics with the progression of atherosclerosis has not yet been fully elucidated.
Carotid ultrasonography is a simple, non-invasive and inexpensive procedure for assessing the severity of atherosclerosis [20], while non-invasive ultrasonic tissue characterisation of the carotid artery wall or plaque using the grey-scale median (GSM) reflects vascular composition [21]. Lesions containing abundant lipids and haemorrhagic components are more echolucent (lower GSM), whereas stable components, including fibrous and calcified tissue, are more echogenic (higher GSM). A previous study demonstrated that people with type 2 diabetes had more echolucent plaques than those without the condition [22]. In addition, a recent study indicated that people with type 2 diabetes were at higher risk of CVD if they had low GSM plaques than if they did not [23]. Also, we recently showed that the change in mean GSM over time was useful for predicting CVD events in people with type 2 diabetes [24].
In this exploratory study, we investigated the relationship of TIR and glucose variability metrics with changes in carotid atherosclerosis, including intime–media thickness (IMT) and the tissue characteristics of the carotid artery wall, in people with type 2 diabetes with no apparent history of symptomatic CVD.
Methods
Study design
This study was an exploratory sub-analysis of an ongoing observational, prospective cohort study investigating the relationships between glucose fluctuations evaluated using CGM and the incidence of composite cardiovascular events over a 5-year follow-up period [25]. The primary aim of this study was to assess the relationship between TIR and CV at baseline, and changes in IMT and GSM over 104 weeks, with adjustment for conventional risk factors. The secondary aim was to assess the association of other CGM-derived metrics and HbA1c with changes in IMT and GSM. This study used cohort study data obtained at baseline and at 104 weeks. This study has been registered in the University Hospital Medical Information Network Clinical Trials Registry, which is a non-profit organisation in Japan that meets the requirements of the International Committee of Medical Journal Editors (UMIN000032325).
Study population
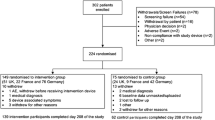
The study population consisted of Japanese people with type 2 diabetes who regularly attend the outpatient diabetes clinics of 34 institutions across Japan. The study design, inclusion criteria and exclusion criteria have been published previously [25] and are described in electronic supplementary material (ESM) Methods. Briefly, the study enrolled outpatients aged ≥30 years and ≤80 years who were on a stable glucose-lowering treatment regimen, defined as no changes in glucose-lowering medications (including new prescriptions) for 6 months before written informed consent was obtained, and with no anticipated changes in glucose-lowering medication from the time of enrolment until the application of CGM sensors. Insulin dose changes were allowed. People with a history of symptomatic cardiovascular events were excluded. Information on how representative this study sample was of the larger population of interest in terms of age, sex, ethnicity, regional and socioeconomic factors was not available. Sex and race/ethnicity were self-reported.
Consecutive people attending the clinic were screened. People who met the eligibility criteria were asked to participate in the present study. A total of 1000 people who met the eligibility criteria were recruited between May 2018 and March 2019. One person withdrew consent. Among the 999 participants, 600 for whom baseline carotid ultrasound images were obtained were included in this analysis. The protocol was approved by the institutional review board of each participating institution in compliance with the Declaration of Helsinki and current legal regulations in Japan. Written informed consent was obtained from all participants after a full explanation of the study.
Biochemical tests
Blood samples were obtained after overnight fasting. Renal function, lipid levels and HbA1c (standardised according to the National Glycohaemoglobin Standardisation Program) were measured using standard techniques. Urinary albumin excretion was measured by a latex agglutination assay using a spot urine sample. The eGFR was calculated using a previously defined formula [26].
Continuous glucose monitoring using the FreeStyle Libre Pro
The FreeStyle Libre Pro CGM (FLP-CGM) device (Abbott Japan), which measures glucose levels every 15 min for up to 14 days, was used at baseline as previously reported [18, 25] and at 104 weeks. Other than wearing the FLP-CGM, there were no restrictions on participants’ daily lives. Downloaded datasets were analysed. Glucose variability was assessed based on the glucose CV [7]. CV (%) was calculated by dividing the SD by the mean of the corresponding glucose readings. TIR was defined as the percentage of time within the target range of 3.9–10.0 mmol/l. Time above range (TAR) >10 and >13.9 mmol/l (TAR>10 mmol/l and TAR>13.9 mmol/l) were defined as the percentages of time above the corresponding blood glucose levels. Time below range (TBR) <3.9 and <3.0 mmol/l (TBR<3.9 mmol/l and TBR<3.0 mmol/l) were defined as the percentages of time below the corresponding blood glucose levels [7]. Mean glucose, CV, TIR, TAR and TBR are among the primary measurable outcomes of CGM [27]. As a previous study demonstrated that FLP-CGM was less accurate during the first 24 h after insertion (from the first day to the second day) and during the last 4 days of its 14-day lifetime [28], we analysed FLP-CGM data obtained over the middle 8-day period.
Measurement of carotid IMT
Ultrasonographic scans of the carotid artery were performed by expert sonographers who had been specifically trained to perform the prescribed study examination using the same equipment in each setting, as reported previously [29, 30]. Briefly, the extracranial common carotid artery (CCA), the carotid bulb and the internal carotid artery in the neck were scanned bilaterally in transverse projections and at least three different longitudinal projections; in addition, the site of greatest thickness, including plaque lesions, was identified along the arterial walls. The IMT represents the distance between two parallel echogenic lines corresponding to the vascular lumen and the adventitia. To avoid inter-reader variability, all scans were electronically stored and emailed to the central office (IMT Evaluation Committee, Osaka, Japan) to be read in random order by a single experienced reader who was blinded to the clinical characteristics of the participants, using Intimascope automated digital edge-detection software (MediaCross, Japan) [29, 30]. The software system calculates the mean of approximately 200 IMT values in the segment that is 2 cm proximal to the dilation of the carotid bulb (mean IMT-CCA), and CCA-max-IMT was defined as the higher of the right and left values.
The echogenicity of the arterial wall was evaluated based on the GSM method, with a grey-scale range of 0–255 (where 0 is the darkest tone and 255 is the brightest), as described previously [17]. Adobe Photoshop software version 7.0 (Adobe Systems, USA) was used for image standardisation and calculation of grey-scale values. The methods used for GSM measurement are shown in detail in Fig. 1.
Methods of GSM evaluation. Standardisation of the B-mode image was performed using a curve option, so that the GSM for blood ranged from 0 to 5 and that for the adventitia ranged from 185 to 195. (a) The right and left mean IMT areas (intima–media complex of the segment 2 cm proximal to dilation of the carotid bulb) were then delineated using a freehand tool (red frame), and the GSM of the selected area was read from the entire delineated area. The mean GSM was defined as the average of the right and left values. (b) If there were atherosclerotic thickened lesions (focal IMT ≥1.0 mm), the GSM of these lesions was measured using the same method in the right and left arteries. We defined these atherosclerotic thickened lesions as ‘carotid plaque’. The lesions were delineated using a freehand tool (red frame), and the GSM value of each carotid plaque was read from the entire delineated area. If multiple thickened lesions were found in the same individual, the lesion with the greatest thickness was subjected to GSM measurement separately in the left and right carotids, and then the lower of the right and left values, defined as ‘thickened-lesion GSM’, was used as the representative value
The annual change in each value was calculated as (final value − initial value)/observation period. The intra-reader CVs for mean IMT, CCA-max-IMT and GSM measurements were 2.0%, 2.7% and 2.9%, respectively, for 40 consecutively replicated measurements [17].
Statistical analysis
The results are presented as mean ± SD or median (IQR) for continuous variables, and as number (proportion) of patients for categorical variables. Changes from baseline to 104 weeks were assessed using the one-sample t test and Wilcoxon’s signed-rank test for continuous variables, and McNemar’s test for categorical variables. A pre-specified multivariate linear regression analysis was performed to investigate whether FLP-CGM-derived metrics were associated with changes in index values for carotid atherosclerosis, which included mean IMT-CCA, CCA-max-IMT, mean GSM and thickened-lesion GSM. The model included the following pre-specified conventional risk factors [18, 31]: age, sex, index values for carotid atherosclerosis, BMI, duration of diabetes, HbA1c, systolic BP, total cholesterol, HDL-cholesterol, triacylglycerols, uric acid, eGFR, urinary albumin excretion, presence of diabetic retinopathy, smoking status, alcohol consumption, use of insulin therapy, use of angiotensin-converting enzyme inhibitors and/or angiotensin II receptor blockers, use of statins and use of anti-platelet agents at baseline [32,33,34,35,36,37]. The Hochberg method was used to control multiple testing [38] as a post hoc analysis.
Next, we performed a pre-specified sensitivity analysis to investigate the relationship between FLP-CGM-derived metrics and the progression of carotid atherosclerosis. Participants were divided into three groups based on tertiles of FLP-CGM-derived metrics at baseline. Trend association across these groups was evaluated by linear regression analysis adjusted for age, sex and each index value for carotid atherosclerosis at baseline.
Finally, we performed a post hoc sensitivity analysis to investigate how atherosclerosis progression was affected by achieving target CGM-derived metrics proposed by an international consensus [27]. To do this, we classified participants into two groups: those who did or did not achieve all target CGM-derived metrics at baseline: TIR >70%, TAR>10 mmol/l <25%, TAR>13.9 mmol/l <5%, TBR<3.9 mmol/l <4% and TBR<3.0 mmol/l <1%. Comparison between the two groups was performed using a linear regression model adjusted for potential conventional risk factors for atherosclerosis.
All statistical tests were two-sided with a 5% significance level. All analyses were performed using SAS software version 9.4 (SAS Institute, USA).
Results
Participants’ demographic and background characteristics, and changes in clinical parameters during the study period
The data of 600 participants with type 2 diabetes were available at baseline. Forty-seven participants did not undergo carotid ultrasonography at 104 weeks: 35 were lost to follow-up and 12 refused to undergo the examination. The baseline clinical characteristics of the 600 participants are summarised in Table 1. The mean age was 64.9±9.2 years, 63.2% were male, and the mean HbA1c was 7.0±0.8% (53.5±9.0 mmol/mol). Over 104 weeks of follow-up, HbA1c was not significantly changed, and there was a modest but significant increase in CV. With respect to other conventional atherosclerotic risk factors, BMI was slightly decreased, and renal function was slightly deteriorated, as determined by eGFR. The frequency of use of oral glucose-lowering agents, anti-hypertensive agents, statins and anti-platelet agents increased significantly during the 104-week study period.
A modest but significant increase in mean IMT was observed over 104 weeks, but there was no significant change in CCA-max-IMT. The annual changes in mean IMT and CCA-max-IMT were 0.008±0.046 and 0.004±0.128 mm/year, respectively. For GSM, a modest but significant increase in thickened-lesion GSM was observed over 104 weeks, but there was no significant change in mean GSM. The annual changes in mean GSM and thickened-lesion GSM were 0.48±6.63 and 5.3±11.6 units/year, respectively.
Relationship between CV and TIR at baseline, and changes in IMT and GSM
The primary aim of this study was to use multivariate linear regression analysis to assess the relationship between CV and TIR at baseline, and changes in IMT and GSM over 104 weeks. CV and TIR were not associated with the annual changes in mean IMT or CCA-max-IMT (Table 2). However, CV and TIR were significantly associated with the annual changes in mean GSM and thickened-lesion GSM (Table 3). As CV at baseline increased by 1%, mean GSM decreased by 0.12 units/year. As TIR at baseline increased by 10%, mean GSM increased by 0.52 units/year. Similarly, as CV at baseline increased by 1%, thickened-lesion GSM decreased by 0.19 units/year. As TIR at baseline increased by 10%, thickened-lesion GSM increased by 0.95 units/year.
Association of FLP-CGM-derived metrics and HbA1c at baseline with changes in IMT and GSM
The secondary aim of this study was to use multivariate linear regression analysis to assess the relationship between other FLP-CGM-derived metrics, which included mean glucose, TAR>10 mmol/l, TBR<3.9 mmol/l and HbA1c at baseline, and changes in IMT and GSM over 104 weeks. Neither FLP-CGM-derived metrics nor HbA1c were associated with changes in mean IMT, CCA-max-IMT, mean GSM or thickened-lesion GSM after adjusting for multiple testing (Table 4).
Relationship between FLP-CGM-derived metrics and changes in index values for carotid atherosclerosis
Next, we performed a pre-defined sensitivity analysis to investigate the relationship between FLP-CGM-derived metrics and the progression of carotid atherosclerosis. Participants were divided into three groups based on tertiles of FLP-CGM-derived metrics at baseline. There was no significant association between FLP-CGM-derived metrics classified by tertiles and the annual changes in mean IMT and CCA-max-IMT in a linear regression model adjusted for age, sex and each IMT value at baseline (ESM Table 1). In a linear regression model adjusted for age, sex and mean GSM at baseline, lower CV and higher TIR classified by tertiles were significantly associated with an annual increase in mean GSM (ESM Table 1). Also, in a linear regression model adjusted for age, sex and thickened-lesion GSM at baseline, lower mean glucose, CV, TAR>13.9 mmol/l and higher TIR classified by tertiles were significantly associated with an annual increase in thickened-lesion GSM (ESM Table 1). However, no significant association was observed between HbA1c values classified by tertile and the annual changes in all index values for carotid atherosclerosis (ESM Table 1).
Relationship between changes in FLP-CGM-derived metrics and changes in index values for carotid atherosclerosis
We performed a pre-specified exploratory analysis to investigate the relationship between changes in FLP-CGM-derived metrics from baseline to 104 weeks and the progression of carotid atherosclerosis over 104 weeks. There were no significant relationships between changes in FLP-CGM-derived metrics and the annual changes in any of the index values for carotid atherosclerosis (ESM Table 2). In addition, in adjusted linear regression models, no significant association was observed between changes in FLP-CGM-derived metrics and the annual changes in these values (ESM Tables 3 and 4).
Relationship between FLP-CGM-derived metrics and carotid atherosclerosis among groups based on achievement of target CGM-derived metrics
Finally, we performed a post hoc sensitivity analysis to investigate how atherosclerosis progression was affected by achieving target CGM-derived metrics. Participants were divided into two groups based on whether or not they achieved target CGM-derived metrics at baseline. There was a significant difference in annual change in mean GSM between participants who achieved the target CGM-derived metrics and those who did not after adjustment for other conventional potential risk factors for atherosclerosis (Table 5).
Discussion
To our knowledge, this is the first study to reveal that TIR and CV are associated with changes in ultrasonic tissue characteristics of the carotid artery wall, even after adjusting for various risk factors, including HbA1c. In addition, participants who achieved the target CGM-derived metrics proposed by the international consensus demonstrated significant annual changes in mean GSM compared with those who did not. These results underscore the importance of including these CGM-derived metrics as a part of optimal diabetes management in conjunction with HbA1c, and indicate the need for further studies to clarify the threshold of change in GSM for predicting CVD and to assess whether targeting TIR and CV could prevent the progression of atherosclerosis and/or CVD onset.
A previous study demonstrated that every 10 unit/year increment in mean GSM was associated with an approximately 73% risk reduction in CVD [24]. Accordingly, the increase in mean GSM of approximately 1 unit/year found in participants with lower CV and higher TIR classified by tertiles, and those who achieved the target CGM metrics may be clinically relevant. Thus, achieving glycaemic control using CGM may be beneficial for reducing the risk of CVD. However, observing changes in thickened-lesion GSM is also useful for evaluating the progression of atherosclerosis. Notably, we found that there was a significant greater change in thickened-lesion GSM in participants with lower CV and higher TIR classified by tertiles, and thickened-lesion GSM change was numerically but non-significantly greater in participants who achieved the target CGM metrics than in those who did not. Theoretically, assessment of thickened lesions in the carotid arteries, including plaque, is more useful for predicting future CVD than the evaluation of mean GSM. However, it remains largely unknown whether longitudinal changes in thickened-lesion GSM are associated with the risk of CVD. This may be because the thickened carotid lesions evaluated at baseline were not necessarily always the same as those evaluated at other follow-up points, because of the inability to track changes in individual thickened lesions over time. At present, it is reasonable to state that changes in mean GSM constitute a more reproducible and reliable marker for predicting CVD.
Previous cross-sectional studies demonstrated that glucose variability was associated with coronary or carotid plaque tissue characteristics [17, 39, 40]. In addition, to our knowledge, the current study is the first to provide evidence that CV was associated with changes in ultrasonic tissue characteristics of the carotid artery wall. Furthermore, the relationship between TIR, which may comprehensively reflect both glycaemic level and glycaemic variability [41], and mean GSM change or thickened-lesion GSM change, did not reach significance after adjusting for CV (data not shown), suggesting that glycaemic variability may be a major contributor. Although the exact mechanism of how glucose variability contributes to the tissue characteristics of the carotid vascular wall remains unclear, we propose the following possible scenario. Previous studies have shown that glucose variability induces inflammation and increases oxidative stress to a greater extent than chronic persistent hyperglycaemia [42], thus contributing to vascular damage. In agreement with these data, endothelial cell apoptosis caused by oxidative stress was more pronounced after intermittent hyperglycaemia than after persistent hyperglycaemia [43]. Accordingly, vascular walls may be damaged more by glucose variability than by chronic persistent hyperglycaemia.
In cross-sectional studies, the relationship between glucose variability and IMT is inconsistent [16, 17, 19]. In addition, we found no significant association between FLP-CGM-derived metrics, including glucose variability metrics, and annual changes in mean IMT and CCA-max-IMT. Thus, it remains inconclusive whether glucose variability affects carotid IMT. Previous studies demonstrated that people with type 2 diabetes had a greater mean IMT than those without [44, 45], and their annual increase in IMT (0.034 mm/year) was also greater (0.007–0.008 mm/year in a healthy population) [33]. Our study enrolled people with a stable glucose-lowering treatment regimen and no apparent history of symptomatic CVD who visited an outpatient clinic for routine medical care. Therefore, our participants had relatively low HbA1c levels as well as higher TIR and lower CV. Also, BP and lipid variables were relatively well controlled, and BMI was not very high. Not surprisingly, the mean IMT of 0.759 mm in our participants was relatively low, and the annual changes in mean IMT (0.008 mm/year) and CCA-max-IMT (0.004 mm/year) were smaller than those in a previous prospective cohort study [46]. Under these conditions, glucose variability may not greatly contribute to the progression of carotid IMT. Further studies are needed to clarify these relationships.
It remains unclear why FLP-CGM-derived metrics were associated with the annual changes in GSM but not the changes in IMT. This may be because IMT and GSM have different relationships with major atherosclerosis risk factors [32, 47]. Furthermore, carotid IMT and GSM reflect different pathogenic processes of atherosclerosis, even though the two variables are modestly correlated with each other [32]. A previous study examining the morphological features of early human atherosclerosis demonstrated that, in atherosclerosis-prone arteries, including carotid arteries, extracellular lipid deposition begins to occur in the outer layer of pre-existing lesions with diffuse intimal thickening [48]. As the lesion progresses, lipids continue to accumulate in the outer layer of the thickened intima of the fatty streak, but do not cause a biologically important change in intimal thickness [49]. Then, stimulated macrophages accumulate in the fatty streak and infiltrate the accumulated lipid, leading to pathological intimal thickening with foam cells [49]. Accordingly, a change in tissue characteristics can precede IMT thickening in the early stage of atherosclerosis. Taken together, it is possible that persistent hyperglycaemia, glucose fluctuations and/or hypoglycaemia differentially affect IMT thickening and tissue characteristics of the vascular wall.
The strengths of this study included its relatively large sample size and multicentre design. However, the study had several limitations. First, it was a short-term, observational study, and therefore had drawbacks similar to all analyses of this type. Second, FLP-CGM-derived metrics were evaluated based on FLP-CGM measurements obtained during limited periods of 8 consecutive days at baseline and at 104 weeks. Thus, these metrics may not represent the participants’ overall glycaemic control. To most accurately assess baseline glucose variability using FLP-CGM, we only recruited people who were on a stable glucose-lowering treatment regimen. In addition, we employed a blind CGM system that prevented participants from altering their lifestyle behaviours based on the results of glucose readings. However, FLP-CGM measurements at 104 weeks were not performed in all participants and were obtained in the absence of any treatment restrictions. Last-minute changes in medications may greatly affect FLP-CGM metrics. This limitation may have made it difficult to evaluate the relationships between changes in FLP-CGM metrics and changes in index values for carotid atherosclerosis. Similarly, post hoc analysis showed no significant associations between mean values in FLP-CGM-derived metrics at baseline and 104 weeks and the annual changes in these values (data not shown). Repeated FLP-CGM measurements during the study period would have been required to clarify this point. Third, potential confounders were not included in the multivariate regression analysis. In particular, changes in the frequency of medication use, including use of glucagon-like peptide-1 antagonists, may have affected the results. Fourth, we recruited Japanese people with type 2 diabetes and without a history of symptomatic CVD. Given these inclusion criteria, a very limited number of people with carotid artery stenosis were included, although approximately 80% of participants had one or more carotid plaques at baseline. In addition, our participants had a TIR of approximately 80% and a CV of approximately 26% at baseline and 104 weeks. Accordingly, in our participants, TIR was more than acceptable and CV was much lower than the target CGM-derived metrics proposed by an international consensus [27], suggesting that blood glucose in our participants was relatively well controlled. These constraints may have limited the generalisability of our results. Finally, multiple testing in exploratory and sensitivity analyses increases the chance of false-positive findings, and thus our results should be interpreted with caution.
In conclusion, TIR and CV were significantly associated with changes in the tissue characteristics of the carotid artery wall, independently of HbA1c, in people with type 2 diabetes and no apparent history of symptomatic CVD. Thus, in conjunction with HbA1c, these metrics may provide useful information for predicting atherosclerotic changes.
Abbreviations
- CCA:
-
Common carotid artery
- CGM:
-
Continuous glucose monitoring
- FLP-CGM:
-
FreeStyle Libre Pro continuous glucose monitoring
- GSM:
-
Grey-scale median
- IMT:
-
Intima–media thickness
- TAR:
-
Time above range
- TBR:
-
Time below range
- TIR:
-
Time in range
References
Rawshani A, Rawshani A, Franzen S et al (2017) Mortality and cardiovascular disease in type 1 and type 2 diabetes. N Engl J Med 376(15):1407–1418. https://doi.org/10.1056/NEJMoa1608664
Rask-Madsen C, King GL (2013) Vascular complications of diabetes: mechanisms of injury and protective factors. Cell Metab 17(1):20–33. https://doi.org/10.1016/j.cmet.2012.11.012
Araki E, Goto A, Kondo T et al (2020) Japanese clinical practice guideline for diabetes 2019. Diabetol Int 11(4):1020–1076. https://doi.org/10.1111/jdi.13306
Davies MJ, D’Alessio DA, Fradkin J et al (2018) Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 61(12):2461–2498. https://doi.org/10.1007/s00125-018-4729-5
UK Prospective Diabetes Study (UKPDS) Group (1998) Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 352(9131):837–853. https://doi.org/10.1016/S0140-6736(98)07019-6
Davies MJ, Aroda VR, Collins BS et al (2022) Management of hyperglycaemia in type 2 diabetes, 2022. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 65(12):1925–1966. https://doi.org/10.1007/s00125-022-05787-2
El-Sayed NA, Aleppo G, Aroda VR et al (2023) 6. Glycemic targets: standards of care in diabetes-2023. Diabetes Care 46(Suppl 1):S97–S110. https://doi.org/10.2337/dc23-S006
Stratton IM, Adler AI, Neil HA et al (2000) Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ 321(7258):405–412. https://doi.org/10.1136/bmj.321.7258.405
Diabetes Control and Complications Trial Research Group (1995) The relationship of glycemic exposure (HbA1c) to the risk of development and progression of retinopathy in the Diabetes Control and Complications Trial. Diabetes 44(8):968–983. https://doi.org/10.2337/diab.44.8.968
Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME et al (2008) Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 358(24):2545–2559. https://doi.org/10.1056/NEJMoa0802743
ADVANCE Collaborative Group, Patel A, MacMahon S et al (2008) Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med 358(24):2560–2572. https://doi.org/10.1056/NEJMoa0802987
Duckworth W, Abraira C, Moritz T et al (2009) Glucose control and vascular complications in veterans with type 2 diabetes. N Engl J Med 360(2):129–139. https://doi.org/10.1056/NEJMoa0808431
Su G, Mi SH, Tao H et al (2013) Impact of admission glycemic variability, glucose, and glycosylated hemoglobin on major adverse cardiac events after acute myocardial infarction. Diabetes Care 36(4):1026–1032. https://doi.org/10.2337/dc12-0925
Goto A, Arah OA, Goto M, Terauchi Y, Noda M (2013) Severe hypoglycaemia and cardiovascular disease: systematic review and meta-analysis with bias analysis. BMJ 347:f4533. https://doi.org/10.1136/bmj.f4533
Lu J, Wang C, Shen Y et al (2021) Time in range in relation to all-cause and cardiovascular mortality in patients with type 2 diabetes: a prospective cohort study. Diabetes Care 44(2):549–555. https://doi.org/10.2337/dc20-1862
Lu J, Ma X, Shen Y et al (2020) Time in range is associated with carotid intima-media thickness in type 2 diabetes. Diabetes Technol Ther 22(2):72–78. https://doi.org/10.1089/dia.2019.0251
Taya N, Katakami N, Mita T et al (2021) Associations of continuous glucose monitoring-assessed glucose variability with intima-media thickness and ultrasonic tissue characteristics of the carotid arteries: a cross-sectional analysis in patients with type 2 diabetes. Cardiovasc Diabetol 20(1):95. https://doi.org/10.1186/s12933-021-01288-5
Wakasugi S, Mita T, Katakami N et al (2021) Associations between continuous glucose monitoring-derived metrics and arterial stiffness in Japanese patients with type 2 diabetes. Cardiovasc Diabetol 20(1):15. https://doi.org/10.1186/s12933-020-01194-2
Foreman YD, van Doorn W, Schaper NC et al (2021) Greater daily glucose variability and lower time in range assessed with continuous glucose monitoring are associated with greater aortic stiffness: The Maastricht Study. Diabetologia 64(8):1880–1892. https://doi.org/10.1007/s00125-021-05474-8
Katakami N, Matsuoka TA, Shimomura I (2019) Clinical utility of carotid ultrasonography: application for the management of patients with diabetes. J Diabetes Invest 10(4):883–898. https://doi.org/10.1111/jdi.13042
El-Barghouty NM, Levine T, Ladva S, Flanagan A, Nicolaides A (1996) Histological verification of computerised carotid plaque characterisation. Eur J Vasc Endovasc Surg 11(4):414–416. https://doi.org/10.1016/s1078-5884(96)80172-9
Ostling G, Hedblad B, Berglund G, Goncalves I (2007) Increased echolucency of carotid plaques in patients with type 2 diabetes. Stroke 38(7):2074–2078. https://doi.org/10.1161/STROKEAHA.106.480830
Irie Y, Katakami N, Kaneto H et al (2013) The utility of ultrasonic tissue characterization of carotid plaque in the prediction of cardiovascular events in diabetic patients. Atherosclerosis 230(2):399–405. https://doi.org/10.1016/j.atherosclerosis.2013.08.015
Katakami N, Mita T, Gosho M et al (2018) Clinical utility of carotid ultrasonography in the prediction of cardiovascular events in patients with diabetes: a combined analysis of data obtained in five longitudinal studies. J Atheroscler Thromb 25(10):1053–1066. https://doi.org/10.5551/jat.43141
Mita T, Katakami N, Okada Y et al (2019) Protocol of a prospective observational study on the relationship between glucose fluctuation and cardiovascular events in patients with type 2 diabetes. Diabetes Ther 10(5):1565–1575. https://doi.org/10.1007/s13300-019-0665-8
Matsuo S, Imai E, Horio M et al (2009) Revised equations for estimated GFR from serum creatinine in Japan. Am J Kidney Dis 53(6):982–992. https://doi.org/10.1053/j.ajkd.2008.12.034
Battelino T, Danne T, Bergenstal RM et al (2019) Clinical targets for continuous glucose monitoring data interpretation: recommendations from the international consensus on time in range. Diabetes Care 42(8):1593–1603. https://doi.org/10.2337/dci19-0028
Boscari F, Galasso S, Acciaroli G et al (2018) Head-to-head comparison of the accuracy of Abbott FreeStyle Libre and Dexcom G5 mobile. Nutr Metab Cardiovasc Dis 28(4):425–427. https://doi.org/10.1016/j.numecd.2018.01.003
Mita T, Katakami N, Shiraiwa T et al (2016) Sitagliptin attenuates the progression of carotid intima-media thickening in insulin-treated patients with type 2 diabetes: the Sitagliptin Preventive Study of Intima-Media Thickness Evaluation (SPIKE): a randomized controlled trial. Diabetes Care 39(3):455–464. https://doi.org/10.2337/dc15-2145
Mita T, Katakami N, Yoshii H et al (2016) Alogliptin, a dipeptidyl peptidase 4 inhibitor, prevents the progression of carotid atherosclerosis in patients with type 2 diabetes: the Study of Preventive Effects of Alogliptin on Diabetic Atherosclerosis (SPEAD-A). Diabetes Care 39(1):139–148. https://doi.org/10.2337/dc15-0781
Wakasugi S, Mita T, Katakami N et al (2021) Associations between continuous glucose monitoring-derived metrics and diabetic retinopathy and albuminuria in patients with type 2 diabetes. BMJ Open Diabetes Res Care 9(1):e001923. https://doi.org/10.1136/bmjdrc-2020-001923
Peters SA, Lind L, Palmer MK et al (2012) Increased age, high body mass index and low HDL-C levels are related to an echolucent carotid intima-media: the METEOR study. J Intern Med 272(3):257–266. https://doi.org/10.1111/j.1365-2796.2011.02505.x
Yokoyama H, Katakami N, Yamasaki Y (2006) Recent advances of intervention to inhibit progression of carotid intima-media thickness in patients with type 2 diabetes mellitus. Stroke 37(9):2420–2427. https://doi.org/10.1161/01.STR.0000236632.58323.cd
Alonso N, Traveset A, Rubinat E et al (2015) Type 2 diabetes-associated carotid plaque burden is increased in patients with retinopathy compared to those without retinopathy. Cardiovasc Diabetol 14:33. https://doi.org/10.1186/s12933-015-0196-1
Nakade Y, Toyama T, Furuichi K et al (2015) Impact of kidney function and urinary protein excretion on intima-media thickness in Japanese patients with type 2 diabetes. Clin Exp Nephrol 19(5):909–917. https://doi.org/10.1007/s10157-015-1088-0
Lu C, Weng R, Wu W, Wang Y, Gu X (2021) Moderate alcohol consumption and carotid intima-media thickness in type 2 diabetes. Asia Pacific J Clin Nutr 30(3):497–503. https://doi.org/10.6133/apjcn.202109_30(3).0016
Ke JF, Wang JW, Zhang ZH, Chen MY, Lu JX, Li LX (2021) Insulin therapy is associated with an increased risk of carotid plaque in type 2 diabetes: a real-world study. Frontiers Cardiovasc Med 8:599545. https://doi.org/10.3389/fcvm.2021.599545
Hochberg Y (1988) A sharper Bonferroni procedure for multiple tests of significance. Biometrika 75(4):800–802. https://doi.org/10.1093/biomet/75.4.800
Okada K, Hibi K, Gohbara M et al (2015) Association between blood glucose variability and coronary plaque instability in patients with acute coronary syndromes. Cardiovasc Diabetol 14:111. https://doi.org/10.1186/s12933-015-0275-3
Kuroda M, Shinke T, Sakaguchi K et al (2015) Association between daily glucose fluctuation and coronary plaque properties in patients receiving adequate lipid-lowering therapy assessed by continuous glucose monitoring and optical coherence tomography. Cardiovasc Diabetol 14:78. https://doi.org/10.1186/s12933-015-0236-x
Lu J, Ma X, Zhang L et al (2020) Glycemic variability modifies the relationship between time in range and hemoglobin A1c estimated from continuous glucose monitoring: a preliminary study. Diabetes Res Clin Pract 161:108032. https://doi.org/10.1016/j.diabres.2020.108032
Ceriello A, Esposito K, Piconi L et al (2008) Oscillating glucose is more deleterious to endothelial function and oxidative stress than mean glucose in normal and type 2 diabetic patients. Diabetes 57(5):1349–1354. https://doi.org/10.2337/db08-0063
Quagliaro L, Piconi L, Assaloni R, Martinelli L, Motz E, Ceriello A (2003) Intermittent high glucose enhances apoptosis related to oxidative stress in human umbilical vein endothelial cells: the role of protein kinase C and NAD(P)H-oxidase activation. Diabetes 52(11):2795–2804. https://doi.org/10.2337/diabetes.52.11.2795
Temelkova-Kurktschiev TS, Koehler C, Leonhardt W et al (1999) Increased intimal-medial thickness in newly detected type 2 diabetes: risk factors. Diabetes Care 22(2):333–338. https://doi.org/10.2337/diacare.22.2.333
Mitsuhashi N, Onuma T, Kubo S, Takayanagi N, Honda M, Kawamori R (2002) Coronary artery disease and carotid artery intima-media thickness in Japanese type 2 diabetic patients. Diabetes Care 25(8):1308–1312. https://doi.org/10.2337/diacare.25.8.1308
Bosevski M, Stojanovska L (2015) Progression of carotid-artery disease in type 2 diabetic patients: a cohort prospective study. Vasc Health Risk Manag 11:549–553. https://doi.org/10.2147/VHRM.S79079
Jung M, Parrinello CM, Xue X et al (2015) Echolucency of the carotid artery intima-media complex and intima-media thickness have different cardiovascular risk factor relationships: the Women’s Interagency HIV Study. J Am Heart Assoc 4(2):e001405. https://doi.org/10.1161/JAHA.114.001405
Nakashima Y, Chen YX, Kinukawa N, Sueishi K (2002) Distributions of diffuse intimal thickening in human arteries: preferential expression in atherosclerosis-prone arteries from an early age. Virchows Archiv 441(3):279–288. https://doi.org/10.1007/s00428-002-0605-1
Nakashima Y, Fujii H, Sumiyoshi S, Wight TN, Sueishi K (2007) Early human atherosclerosis: accumulation of lipid and proteoglycans in intimal thickenings followed by macrophage infiltration. Arterioscler Thromb Vasc Biol 27(5):1159–1165. https://doi.org/10.1161/ATVBAHA.106.134080
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Acknowledgements
The authors wish to thank the study investigators listed in ESM Table 5 and the participants for their contributions to this study.
Data availability
All data generated or analysed during this study are included in this article or its supplementary material files. Further enquiries may be directed to the corresponding author.
Funding
This study was financially supported by the Japan Agency for Medical Research and Development under grant number JP20ek0210105 (to HW) and the Manpei Suzuki Diabetes Foundation (to HW). However, the authors declare that these funding sources had no role in the development of this manuscript.
Authors’ relationships and activities
TO and HW have received research funds from Abbott Japan. HW is a member of the advisory board of Abbott Japan. NK has received lecture fees from Abbott Japan. IS received an interview honorarium from Abbott Japan, and a chair/discussant honorarium from Terumo Corp. The authors declare that there are no other relationships or activities that might bias, or be perceived to bias, their work.
Contribution statement
All authors meet the International Committee of Medical Journal Editors criteria for authorship for this manuscript. All authors contributed to the study design and were involved in all stages of manuscript development. TM drafted the manuscript. RI and MG, who are both statisticians, were primarily responsible for data analysis. All authors collected, analysed and interpreted the data, reviewed and edited the manuscript, and approved the final manuscript. HW is the principal guarantor of this work, has full access to all study data, and takes responsibility for the integrity of the data and the accuracy of data analysis. All authors have read and agreed to publication of the manuscript.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Mita, T., Katakami, N., Okada, Y. et al. Continuous glucose monitoring-derived time in range and CV are associated with altered tissue characteristics of the carotid artery wall in people with type 2 diabetes. Diabetologia 66, 2356–2367 (2023). https://doi.org/10.1007/s00125-023-06013-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-023-06013-3