Abstract
Aims/hypothesis
Islet autoantibodies (AAbs) are detected in >90% of individuals with clinically suspected type 1 diabetes at disease onset. A single AAb, sometimes at low titre, is often detected in some individuals, making their diagnosis uncertain. Type 1 diabetes genetic risk scores (GRS) are a useful tool for discriminating polygenic autoimmune type 1 diabetes from other types of diabetes, particularly the monogenic forms, but testing is not routinely performed in the clinic. Here, we used a type 1 diabetes GRS to screen for monogenic diabetes in individuals with weak evidence of autoimmunity, i.e. with a single AAb at disease onset.
Methods
In a pilot study, we genetically screened 142 individuals with suspected type 1 diabetes, 42 of whom were AAb-negative, 27 of whom had a single AAb (single AAb-positive) and 73 of whom had multiple AAbs (multiple AAb-positive) at disease onset. Next-generation sequencing (NGS) was performed in 41 AAb-negative participants, 26 single AAb-positive participants and 60 multiple AAb-positive participants using an analysis pipeline of more than 200 diabetes-associated genes.
Results
The type 1 diabetes GRS was significantly lower in AAb-negative individuals than in those with a single and multiple AAbs. Pathogenetic class 4/5 variants in MODY or monogenic diabetes genes were identified in 15/41 (36.6%) AAb-negative individuals, while class 3 variants of unknown significance were identified in 17/41 (41.5%). Residual C-peptide levels at diagnosis were higher in individuals with mutations compared to those without pathogenetic variants. Class 3 variants of unknown significance were found in 11/26 (42.3%) single AAb-positive individuals, and pathogenetic class 4/5 variants were present in 2/26 (7.7%) single AAb-positive individuals. No pathogenetic class 4/5 variants were identified in multiple AAb-positive individuals, but class 3 variants of unknown significance were identified in 19/60 (31.7%) patients. Several patients across the three groups had more than one class 3 variant.
Conclusions/interpretation
These findings provide insights into the genetic makeup of patients who show weak evidence of autoimmunity at disease onset. Absence of islet AAbs or the presence of a single AAb together with a low type 1 diabetes GRS may be indicative of a monogenic form of diabetes, and use of NGS may improve the accuracy of diagnosis.
Graphical abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.

Introduction
Type 1 diabetes is a disorder of glucose homeostasis, and patients require lifelong daily insulin injections. Type 1 diabetes is considered a multifactorial autoimmune disease in which several common genetic variants combined with environmental factors are thought to contribute to disease risk [1, 2]. Type 1 diabetes is caused by T cell-mediated killing of insulin-producing beta cells, and risk of type 1 diabetes is associated with the presence of measurable autoantibodies (AAbs) in the patients’ sera [3, 4]. Even though the pathogenesis of type 1 diabetes involves T cells, the immune markers are primarily serum AAbs to pancreatic islet antigens. To date, five islet-specific AAbs have been reported: against insulin (IAA), GAD65 (GADA), insulinoma antigen-2 (IA-2A), zinc transporter 8 (ZnT8A) and tetraspanin-7 (TSPAN7A) [5, 6]. Patients who are positive for at least one of these AAbs are diagnosed with T1Da, which is the most frequent form of type 1 diabetes diagnosed in paediatric age groups [7, 8]. Conversely, AAb-negative patients are diagnosed as having T1Db, and account for up to 10% of newly diagnosed patients [9, 10]. Recent studies have shown that AAb-negative patients often have MODY, or, less frequently, permanent neonatal diabetes mellitus (PNDM) or syndromic forms, e.g. Wolfram syndrome [11,12,13,14,15]. The most common subtypes of MODY are caused by mutations in glucokinase (GCK), hepatocyte nuclear factor-1α (HNF1A) and hepatocyte nuclear factor-4α (HNF4A) genes. The former needs no treatment, while the latter two may be treated with low-dose sulfonylureas [16]. Hence, diagnosing MODY may lead to use of specific non-insulin targeted treatments and avoidance of insulin, with a positive impact on the quality of life of the affected individuals and their families, while reducing costs for the healthcare system.
Very-early-onset diabetes often occurs in patients with monogenic autoimmune disease (MAID) due to mutations in genes encoding forkhead box P3 (FOXP3), autoimmune regulator (AIRE), IL-2 receptor alpha (IL-2Rα), signal transducer and activator of transcription (STAT)-1, STAT-3 and STAT-5B, cytotoxic T-lymphocyte-associated antigen 4 (CTLA-4) and lipopolysaccharide-responsive and beige-like anchor protein (LRBA) [17,18,19,20,21,22]. Approximately 20–50% of these patients have no detectable islet-specific AAbs, although the disease is clearly immune-mediated. In several of these patients, diabetes and other autoimmune features are often the first clinical manifestations. Diagnosing MAID is crucial for patients’ prognosis and clinical management. For example, it may enable personalised treatment using abatacept, a CTLA-4 mimetic, in patients with mutations in CTLA4 and LRBA [23, 24].
From a clinical and epidemiological standpoint, patients who are AAb-positive comprise a heterogeneous group of patients. For example, studies on the natural history of diabetes performed by TrialNet and other consortia showed that some patients develop type 1 diabetes very rapidly when aged younger than 5 years and with low C-peptide levels that decline faster than in adults after diagnosis [25, 26]. Studies conducted post mortem on pancreases from individuals in the JDRF Network for Pancreatic Organ Donors revealed significant variability in the proportion of residual insulin-containing islets (ICIs) in individuals with recent-onset disease [27]. Histopathological evaluation of donors with recent-onset type 1 diabetes showed that insulitis differs according to age, suggesting the existence of two type 1 diabetes endotypes (T1DE): T1DE1, with onset at age <13 years, characterised by CD20high insulitis and with islets rich in CD8+ T cells, with few residual ICIs, and evidence of abnormal insulin processing in the remaining beta cells, and T1DE2, with onset at age ≥13 years, characterised by CD20low insulitis with fewer CD8+ T cells, more residual ICIs, and normal insulin processing [28,29,30]. Hence, there is a definite need to develop genetic testing that is able to effectively diagnose type 1 diabetes, differentiate it from other forms of diabetes, and perhaps identify disease endotypes.
Recently, several type 1 diabetes genetic risk scores (GRS) have been developed based on SNPs in HLA and non-HLA type 1 diabetes risk genes (approximately 30–40 SNPs). Such scores are able to discriminate type 1 diabetes from type 2 diabetes, monogenic diabetes from type 1 diabetes, and MAID from early-onset type 1 diabetes associated with poly-autoimmunity [31, 32]. The type 1 diabetes GRS is much lower in individuals with no islet AAbs at disease onset, especially in those with MODY [33]. Thus, the absence of islet AAb at disease onset and a low type 1 diabetes GRS are good indicators of MODY and monogenic forms of diabetes. However, some patients have a single and/or low-titre islet AAbs at disease onset, and there are no recommendations as to whether they should be genetically tested. The aim of the present pilot study was to identify the discriminatory power of a type 1 diabetes GRS in identifying monogenic forms of diabetes in a cohort of 142 diabetic patients with either multiple AAbs, a single AAb or no evidence of autoimmune diabetes (islet AAbs). The patients’ DNA was sequenced using a next-generation sequencing (NGS) panel, and analysed using a pipeline of more than 200 diabetes-associated genes, including those known to cause MODY, PNDM, MAID, primary immunodeficiency and diabetes-associated syndromes.
Methods
Study population
Individuals with diabetes were recruited retrospectively from patients referred to San Raffaele Hospital between 2013 and 2021 (see electronic supplementary material [ESM] Fig. 1) who met the following criteria: a diagnosis of hyperglycaemia (i.e. fasting plasma glucose concentration ≥7.0 mmol/l or random venous plasma glucose concentration ≥11.1 mmol/l or a plasma glucose concentration ≥11.1 mmol/l 2 h after an OGTT) at paediatric or adult age and no reported prior family history of monogenic diabetes. The selected patients included 73 patients with multiple islet AAbs, 27 individuals who were positive for a single islet AAb, and 42 without islet AAbs. General characteristics of study participants are reported in ESM Table 1. Of the 142 individuals included in our study, 65 were female (45.8%). DNA samples (saliva or peripheral blood) were collected, and clinical characteristics and symptoms at diagnosis were obtained from medical records. The DNA from 41 AAb-negative patients, 26 single AAb-positive patients and 60 multiple AAb-positive patients was sequenced by NGS. Genetic data from 330 non-diabetic individuals were included as control.
AAb analysis
Analysis of IAA, GADA, IA-2A and ZnT8A was performed centrally at the Autoimmunity Laboratory of San Raffaele Hospital using either commercial kits (RSR, Cardiff, UK) or in-house luciferase immunoprecipitation systems (LIPS) and radiobinding assay (RBA) tests. The cut-off for positivity was set in each test as indicated by the manufacturer for commercial kits or to the 99th percentile of values measured in a cohort of blood donors.
C-peptide measurement
Serum C-peptide levels in random non-fasting blood samples were measured at San Raffaele Hospital using standard methods.
Calculation of the type 1 diabetes GRS
We calculated a type 1 diabetes GRS, as a measure of an individual’s genetic susceptibility to type 1 diabetes, by typing 30 common genetic variants associated with type 1 diabetes [31]. DNA was extracted from saliva or peripheral blood samples using QIAamp DNA Mini and Blood Mini kits (Qiagen, Germany) or the Maxwell RSC automatic extractor (Promega, USA) according to the manufacturer’s instructions. The analysis of four SNPs associated with HLA risk haplotypes DR3 and DR4-DQ8 was performed by droplet digital PCR (Bio-Rad, USA). The remaining 26 SNPs located in other susceptibility genes were typed using the high-throughput OpenArray system (Life Technologies, USA) [34]. The score was generated by summing the effective allele dosage for each variant multiplied by the natural log (loge) of the odds ratio as previously described [31].
Next-generation sequencing
Whole-exome sequencing was performed in 67 samples of genomic DNA (ESM Fig. 2) using a Nextera DNA Flex for Enrichment kit (Illumina, USA) and xGen Exome Hybridization panel version 1.0 probes (Integrated DNA Technologies, USA), according to the manufacturer’s instructions. The libraries were sequenced on the NovaSeq 6000 platform (2 × 100 bp) (Illumina). Clinical exome-targeted enrichment sequencing of genomic DNA, including more than 4800 genes, was performed on 60 samples using TruSight One (Illumina) (ESM Fig. 2). Targeted resequencing including exon–intron 50-base boundaries was performed on the Illumina NextSeq500 platform, according to the manufacturer’s protocol, with paired-end 300-cycle sequencing.
Reads obtained by whole-exome sequencing were aligned using the BWA-MEM aligner version 0.7.15 (https://github.com/lh3/bwa) on the hg19 reference genome [35]. Annotation was performed using databases such as dbSNP version 151 [36] and dbNSFP version 4.0a [37, 38]. Selection of genes associated with hereditary forms of diabetes, type 1 diabetes-associated polymorphisms and immune-mediated diseases was performed in silico and included the 212 genes listed in ESM Table 2. Functional effect prediction was performed using SnpEff software version 4.3t [39], and only variants with moderate or high impact were considered, together with those that had an effect involving a splice site. Read alignment and variant calling in clinical exome-sequenced samples were performed using BaseSpace Onsite (Illumina), and then variants were annotated using Variant Studio (Illumina). BAM files were visualised using Integrative Genome Viewer software (http://broadinstitute.org/software/igv/). Among the called variants, all the common variants with a MAF >1% in the GnomAD database (https://gnomad.broadinstitute.org/) [40] were filtered out. Classification of variants with respect to their clinical significance and according to the American College of Medical Genetics and Genomics/Association for Molecular Pathology standards [41] was performed based on evidence from genomic and locus-specific databases, in silico predictions and experimental data in the literature. Variants of unknown significance (class 3), those that are probably pathogenetic (class 4) or pathogenetic (class 5) were included in the study and confirmed by Sanger sequencing.
Ethics approval
The study was approved by the San Raffaele Hospital Ethics Board (study titles: Gene T1D and TIGET004-DRI003). All participants and parents of participants who were less than 18 years old provided a signed informed consent for participation in the study.
Statistical analysis
All analyses were performed using R software version 4.2.1 (https://www.R-project.org) [42]. One-way ANOVA was used to compare the means of continuous variables across multiple groups (>2), e.g. AAb groups (with or without the combination of family history and other autoimmune diseases). The post hoc Tukey honest significant differences test was used for comparisons across two groups, with correction of p values for the number of comparisons between groups. To compare the frequency of categorical variables across groups, Fisher’s exact test was used.
Results
AAb-negative diabetic individuals with low type 1 diabetes GRS have pathogenetic class 4/5 variants
Over a period of 8 years (2013–2021), 810 children newly diagnosed with diabetes have been referred to the Pediatric Diabetology Unit of the Pediatrics and Neonatology Department of San Raffaele Hospital. Individuals suspected of having type 1 diabetes underwent AAb testing for four major islet AAbs (IAA, IA-2A, GADA and ZnT8A) as a part of routine clinical care. The majority of patients with diabetes (83.3%) were diagnosed as having T1Da (one or more AAb), with the remainder being diagnosed with T1Db (no AAbs, 7.8%), type 2 diabetes (2.5%), MODY (2.2%), PNDM (0.6%) and other types (e.g. Wolfram syndrome, 0.6%) (ESM Fig. 1a). Within the paediatric cohort suspected of having type 1 diabetes, 89 had a single islet AAb at disease onset (ESM Fig. 1b).
In this pilot study, we randomly selected 69 individuals with weak evidence of autoimmunity, i.e. AAb-negative (n=42) or single AAb-positive (one AAb, n=27), irrespective of age at disease onset. Two additional cohorts of individuals diagnosed with type 1 diabetes at a paediatric age (<18 years) with multiple AAbs (n=73) or not diabetic (n=330) were used as controls. The characteristics of the diabetic patients are provided in ESM Table 1. All 142 diabetic patients were analysed using the type 1 diabetes GRS, and 127 (89.4%) were also analysed using NGS (either clinical or whole-exome sequencing) (ESM Fig. 2).
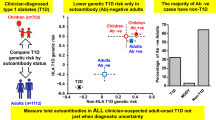
No significant differences in sex or age at disease onset were observed across the three groups (ESM Fig. 3a, b). Children who were multiple AAb-positive showed a similar prevalence of all AAbs except for IAA (GADA 85%; IA-2A 75%; ZnT8A 81%; IAA 52%), while most individuals with a single AAb were positive for GADA (63%) followed by IA-2A, ZnT8A and IAA (7%, 15% and 11%, respectively) (ESM Fig. 3c, d). The type 1 diabetes GRS was calculated as previously described [31], and was significantly different across the three groups (p=4.4 × 10−8; ANOVA) (Fig. 1a). AAb-negative participants had a lower type 1 diabetes GRS compared with both single and multiple AAb-positive patients (adjusted p values =0.00008 and <10−7, respectively; ANOVA post hoc tests) (Fig. 1a). AAb-negative participants showed also higher residual C-peptide levels at onset compared with multiple AAb-positive patients (adjusted p value =0.0003; ANOVA post hoc tests) (Fig. 1b), in line with previous reports [33, 43].
AAb-negative individuals show a lower type 1 diabetes GRS, with higher BMI and residual C-peptide levels at onset, and in several cases show a clear genetic cause for their diabetes. Patients were classified as AAb-negative (AAb−, n=42), single AAb-positive (single AAb+, n=27) and multiple AAb-positive (multiple AAb+, n=73). (a) Calculated type 1 diabetes GRS; (b) residual C-peptide levels at onset; (c) BMI; (d) the number of class 5 variants (green bars) and class 4 variants (blue bars) found in each reported gene among AAb-negative patients. Circles indicate values for each patient; boxplots show the median and IQR for each group. *p<0.05, ***p<0.001 across two groups as shown. T1D, type 1 diabetes
A genetic pipeline comprising genes causing MODY, PNDM, MAID, primary immunodeficiency, syndromic diabetes-associated diseases and type 1 diabetes risk genes identified in genome-wide association studies (GWAS), was used to genetically screen 127 samples (ESM Table 2). Class 4 and 5 pathogenetic variants in MODY genes and syndromic diabetes genes were identified in 15/41 AAb-negative individuals (36.6%; one adult and 14 children). The MODY subtypes identified were: MODY type 2 (GCK) in 11 patients (26.8%), MODY type 10 (INS) in one patient (2.4%) and MODY type 6 (NEUROD1) in one patient (2.4%) (Fig. 1d and Table 1). Pathogenetic variants in the SLC29A3 and WFS1 syndromic genes were identified in two individuals (Fig. 1c and Table 1), with the latter having two WFS1 variants in compound heterozygosity. Among the AAb-negative patients, 17/41 (41.5%) had class 3 variants of unknown significance. In 13 of these patients (three adults, ten children), class 3 variants were present in the absence of class 4/5 variants. In seven patients, class 3 variants were present in more than one gene (Table 1). No significant differences in the type 1 diabetes GRS, age at onset and residual C-peptide levels were observed between AAb-negative patients with no variants and those with class 3 or class 4/5 variants (ESM Fig. 4).
AAb-negative and single and multiple AAb-positive individuals were further divided according to their family history of diabetes and the presence of an additional autoimmune disease (ESM Table 3). The type 1 diabetes GRS showed an almost linear median increase from AAb-negative individuals to those with multiple AAbs having a family history for type 1 diabetes and/or additional autoimmunity (ESM Fig. 5a). A lack of type 1 diabetes HLA risk alleles (absence of either DR3 or DR4-DQ8, X/X) was observed in AAb-negative individuals, particularly those without a family history for type 1 diabetes and/or an additional autoimmunity (ESM Fig. 5b). In summary, AAb-negative individuals without a family history of diabetes and/or additional autoimmunity had mutations that are rare in the general population, in genes that predominantly cause MODY.
Single AAb-positive diabetic individuals test positive for monogenic causes of diabetes
When AAb-positive individuals were divided into those with family history for type 1 diabetes and/or the presence of additional autoimmunity, no differences were observed in the distribution of islet AAbs (ESM Fig. 6). Most single AAb-positive individuals had islet AAb levels that were much lower than those observed in multiple AAb-positive children with type 1 diabetes (ESM Fig. 7). When single AAb-positive individuals were genetically tested by NGS, pathogenetic variants (class 5), probably pathogenetic variants (class 4) and variants of unknown significance (class 3) were identified in 12/26 individuals (46.2%) (Fig. 2a and Table 2). MODY class 5 pathogenetic variants were identified in 2/26 patients (7.7%), comprising one case of MODY type 3 (HNF1A) and one case of HNF1B MODY (a gene that is also associated with type 2 diabetes). Interestingly, the individual with HNF1B MODY had a large deletion (exons 1–8) in HNF1B and two additional variants in the PNDM genes ABCC8 (class 4) and GATA6 (class 3). This patient had an age at onset of 39 years and positivity for ZnT8A. Diabetes in the patient with the HNF1A mutation appeared at 13 years of age in the presence of GADA only. Class 3 variants in genes such as IFIH1, GCKR, UCP2 and SH2B3, four genes that are associated with diabetes risk, were identified in 11/26 (42.3%) single AAb-positive patients. Two patients had variants in AIRE, one in association with variants in the IL6 gene; one patient had variants in the GLIS3 and SLC5A1 genes; one patient had a variant in RFX6, a beta cell gene; one patient had a variant in KLF11, a MODY gene; one patient had a variant in SLC29A3, a gene previously described in an individual with syndromic diabetes [44] (Table 2). Of note, the class 3 variants identified in single AAb-positive diabetic individuals were either absent in the 330 non-diabetic individuals or had a low allele frequency (allele frequency range 0.45–0.9%) (Table 2).
Single AAb-positive patients harbour pathogenetic variants in MODY genes. Seventeen probably pathogenetic variants (class ≥3) were found in 12/26 single AAb-positive patients by clinical exome sequencing. Patients were stratified according to the presence of variants: single AAb-positive without a significant variant (n=14), single AAb-positive with at least one variant of class ≥3 (n=12) and multiple AAb-positive (n=73). (a) Number of class 5 (yellow bars), class 4 (green bar) and class 3 (blue bars) variants found in each of the indicated genes; (b) calculated type 1 diabetes GRS; (c) age at onset; (d) residual C-peptide levels at diabetes diagnosis. Circles indicate values for each patient; boxplots show the median and IQR for each group. T1D, type 1 diabetes
The type 1 diabetes GRS in single AAb-positive patients with variants of class ≥3 was generally high, and comparable to that observed in single AAb-positive individuals without variants and in multiple AAb-positive patients (Fig. 2b). Interestingly, the two individuals with a single AAb and pathogenetic MODY mutations showed the lowest type 1 diabetes GRS (<0.27). No significant differences were found in the age at disease onset or the residual C-peptide levels between the single AAb-positive group (with or without class ≥3 variants) and multiple AAb-positive individuals (Fig. 2c, d).
Rare class 3 variants of unknown significance are identified in multiple AAb-positive type 1 diabetes
We applied our NGS pipeline in 60 multiple AAb-positive individuals diagnosed with type 1 diabetes at a paediatric age (<18 years) to assess the contribution of low-frequency and rare genetic variants to disease susceptibility. No class 4 or 5 pathogenetic variants were found, but low-frequency class 3 variants of unknown significance were identified in 19/60 individuals (31.7%), nine of whom presented with several variants in two or more genes (Fig. 3a and Table 3). Class 3 variants identified in multiple AAb-positive individuals were absent in the 330 non-diabetic individuals or had a very low allele frequency (7/34 variants, allele frequency range 0.15–1.5%) (Table 3).
Class 3 variants of unknown significance in multiple AAb-positive type 1 diabetes patients. (a) Number of class ≥3 variants found in each indicated gene in multiple AAb-positive patients analysed by NGS (n=60) (only class 3 variants found in this group). (b) Venn diagram of the class 3, class 4 and class 5 variants shared across single and multiple AAb-positive individuals. (c, d) Type 1 diabetes GRS (c) and residual C-peptide levels (d) at onset of diabetes in multiple AAb-positive patients diagnosed before (blue) or after 13 years of age (green) (age <13 and age ≥13 being proxies of T1DE1 and T1DE2, respectively). (e) Pie charts showing the frequency of class 3 variants in multiple AAb-positive patients stratified by age at onset < or ≥13 years old. T1D, type 1 diabetes
Low-frequency coding variants in CASP8 and CASP10 genes that are associated with autoimmune lymphoproliferative syndrome [45, 46] were identified in three patients, with compound heterozygosity in one of them (Fig. 3a and Table 3). Class 3 variants of unknown significance in LYST, RAG2, IL23R, UNC13D and STIM1, genes that are associated with primary immunodeficiency, were found in five patients (Fig. 3a and Table 3), with one patient having a variant in both IL23R and UNC13D. Class 3 variants in beta cell-associated genes, i.e. GLIS3, EIF2AK3, SLC19A2, MYT1 and SLC2A1, were found in four patients, with one patient having a variant both in GLIS3 and EIF2AK3 (Fig. 3a and Table 3) [47, 48]. Class 3 variants in the type 1 diabetes genes FUT2 and RNLS, identified by GWAS, and in genes that play critical roles in insulin resistance and glucose metabolism, AKT2 and SREBF1, were identified in two patients for each category (Fig. 3a and Table 3) [49,50,51]. Some class 3 variants of unknown significance in genes that are suspected of involvement in diabetes were found, such as SPTA1 in four patients and DICER1 in two patients (Fig. 3a and Table 3). Except for one gene, GLIS3, there was no genetic overlap between the rare class ≥3 genetic variants identified in single and multiple AAb-positive individuals (Fig. 3b and ESM Fig. 8).
T1DE1, an immune-driven type 1 diabetes endotype, seems to manifest in individuals with disease onset at <13 years, while T1DE2, which is characterised by a less immune-driven and more beta cell-driven signature, manifests at an older age (≥13 years). To identify whether the type 1 diabetes GRS can distinguish T1DE1 from T1DE2, multiple AAb-positive individuals were separated according to their age of disease onset. No statistically significant differences were found between the type 1 diabetes GRS and residual C-peptide levels in multiple AAb-positive individuals with type 1 diabetes onset before or after 13 years of age (Fig. 3c, d). Similarly, the prevalence of class 3 variants was not significantly different between multiple AAb-positive individuals with disease onset before or after 13 years of age 13 (23.2% vs 35.3%, respectively) (Fig. 3e).
Combined GRS/AAb algorithm to determine benefit of NGS in type 1 diabetes precision diagnosis
The type 1 diabetes GRS applied in our cohort of patients discriminated polygenic type 1 diabetes from MODY, albeit with imperfect performance, as demonstrated by a receiver operating characteristic (ROC)–AUC analysis (Fig. 4a, b). Patient stratification according to GRS quartiles, as described by Patel et al [33], and AAb status (ESM Table 4) suggested an improved algorithm for selection of patients who may benefit from an NGS analysis by including individuals with weak evidence of autoimmunity and low GRS in addition to those already recommended by current guidelines (Fig. 4c) [11].
Development of a combined GRS/AAb algorithm to recommend NGS for precision diagnosis of type 1 diabetes. Patients were stratified according to the presence of class 4/5 mutations in MODY genes and the number of AAbs. (a) ROC curve analysis of GRS discriminates autoimmune, polygenic type 1 diabetes from MODY with acceptable performance. (b) Distribution of GRS and mutations/variants in new-onset patients with type 1 diabetes. (c) Proposed algorithm for selection of patients with potential monogenic diabetes for NGS analysis. Genetic testing is recommended in all individuals with diabetes onset at <1 year of age and/or consanguineous parents, those without islet AAbs or markers of type 2 diabetes at disease onset, and patients with one type 1 diabetes AAb and a GRS below the median for single AAb-positive individuals (i.e. <0.274). CES, clinical exome sequencing; T1D, type 1 diabetes; WES, whole exome sequencing; yr, year
Discussion
Type 1 diabetes is known to have a significant genetic component, as confirmed by family- and twin-based studies [52, 53]. The aetiology of type 1 diabetes in paediatric-onset multiple AAb-positive individuals is hypothesised to be driven mainly by the HLA and the compound effect of non-HLA SNPs identified by GWAS. These genetic associations represent common and mid-frequency genetic variants with small effect sizes, and can explain only a small proportion of heritability of type 1 diabetes. Our original hypothesis was that monogenic diabetes genes or other rare pathogenetic variants may also underlie some cases of type 1 diabetes. We therefore examined the genetic background of individuals with diabetes, with a particular focus on young individuals who presented with a single or no islet AAbs at the time of disease diagnosis in comparison with patients with the classical multiple AAb-positive phenotype. Our pilot study corroborates previous findings showing that a significant proportion of AAb-negative individuals have pathogenetic class 4/5 variants in MODY genes and also in genes associated with PNDM and syndromic diseases such as Wolfram syndrome [14, 54]. Several of these AAb-negative patients showed no signs of additional autoimmunity, presented with elevated C-peptide levels, and later were confirmed to have MODY despite the lack of a family history of monogenic diabetes. Moreover, our study shows that genetic testing of single AAb-positive individuals can identify MODY or other monogenic causes of diabetes in approximately 8% of such patients. Of note, the single AAb-positive individuals with MODY pathogenetic variants had a rather low type 1 diabetes GRS. On the other hand, no class 4/5 pathogenetic variants were identified in multiple AAb-positive individuals with paediatric onset of diabetes. The inclusion of class 3 variants of unknown significance in the analysis provided additional information on the possible underlying genetic predisposition to type 1 diabetes. Across all patients and irrespective of AAb status, rare class 3 variants were identified in immune and beta cell genes that may predispose to diabetes. Hence, our genomic approach provides support for the concept that an oligogenic cause of type 1 diabetes may be present in a proportion of single and multiple AAb-positive individuals.
The originality and strength of our study stem from the fact that patients were sequenced for more than 4800 genes, with a high coverage (median 103 ×), and the gene discovery pipeline included 212 genes previously associated with various forms of diabetes, including MODY, PNDM, MAID, primary immunodeficiency and syndromic diseases, as well as genes predisposing to type 1 diabetes that were previously identified in GWAS. One of the limitations of our retrospective study was the fact that only a proportion of the patients who presented with type 1 diabetes at our institute were included, either because of a lack of archived biological samples, which are necessary for NGS, or gaps in the clinical and AAb diagnostic records. Moreover, TSPAN7A, a recently discovered type 1 diabetes AAb [6], was not tested as part of routine diagnostics, suggesting that some patients may have been misclassified as AAb-negative. Nevertheless, our results identified syndromic conditions in individuals who were negative for two or more islet AAbs at disease onset, reinforcing previous hypotheses and suggesting new hypotheses. Importantly, some of the patients diagnosed with monogenic diabetes were switched to the recommended clinical management according to their mutation type. Based on data obtained from this and previous studies, we consider that strong islet seropositivity to more than one AAb at onset is a reasonable exclusion criterion for progressing to genetic testing in a person with diabetes. While we obviously advocate for testing for all four major AAbs in all individuals at the time of disease onset, positivity for a single AAb should constitute one of the criteria for requesting calculation of a type 1 diabetes GRS, to be potentially followed by an NGS analysis. The cost of genotyping individual SNPs has fallen dramatically, and calculation of a type 1 diabetes GRS may soon become a relatively accessible and inexpensive tool to aid disease diagnosis. Our present study adds to previous studies of genetic screening based on a GRS, and underlies the need to include individuals with single AAb positivity in the pipeline for identification of patients affected by monogenic forms of diabetes.
Similarly to type 2 diabetes, rare genetic variants may also contribute to disease risk and pathogenesis in autoimmune diabetes, and are probably distributed across the coding and non-coding regions of numerous genes [55]. In our small cohort of multiple AAb-positive patients, disease susceptibility was probably mostly driven by the individuals’ HLA and known GWAS-based genetic risk loci. However, the exome signals we identified may include additional small contributors to autoimmune diabetes risk and/or pathogenesis. Despite its relatively small size, our study is a first step towards the discovery of rare genetic underpinnings of a complex disease and their potential association with pathophysiological mechanisms underlying disease endotypes. We believe that some of our observations are interesting and hopefully will stimulate further research in this direction. Although this will probably require study of extremely large cohorts of samples, it may lead to identification of unique causative factors and novel therapeutic targets.
Taken together, our study contributes to the roadmap for identifying diabetic patients who are suitable for genetic testing to define diabetes type. This will lead to more appropriate disease management and treatment, with an impact on quality of life. Furthermore, the healthcare system will benefit from reductions in the cost of insulin treatment and patient monitoring.
Data availability
The datasets generated and/or analysed during the current study are available from the corresponding authors on reasonable request.
Abbreviations
- AAb:
-
Autoantibody
- CTLA-4:
-
Cytotoxic T-lymphocyte-associated protein 4
- GADA:
-
Autoantibodies to GAD65
- GRS:
-
Genetic risk score
- GWAS:
-
Genome-wide association study
- IAA:
-
Autoantibodies to insulin
- IA-2A:
-
Autoantibodies to insulinoma antigen-2
- ICI:
-
Insulin-containing islet
- MAID:
-
Monogenic autoimmune disease
- NGS:
-
Next-generation sequencing
- PNDM:
-
Permanent neonatal diabetes mellitus
- ROC:
-
Receiver operating characteristic
- STAT:
-
Signal transducer and activator of transcription
- T1DE:
-
Type 1 diabetes endotypes
- TSPAN7A:
-
Autoantibodies to tetraspanin-7
- ZnT8A:
-
Autoantibodies to zinc transporter 8
References
Van Belle TL, Coppieters KT, Von Herrath MG (2011) Type 1 diabetes: etiology, immunology, and therapeutic strategies. Physiol Rev 91(1):79–118. https://doi.org/10.1152/physrev.00003.2010
Atkinson MA, Eisenbarth GS, Michels AW (2014) Type 1 diabetes. Lancet 383(9911):69–82. https://doi.org/10.1016/S0140-6736(13)60591-7
Ziegler AG, Rewers M, Simell O et al (2013) Seroconversion to multiple islet autoantibodies and risk of progression to diabetes in children. JAMA 309(23):2473–2479. https://doi.org/10.1001/jama.2013.6285
Steck AK, Vehik K, Bonifacio E et al (2015) Predictors of progression from the appearance of islet autoantibodies to early childhood diabetes: The Environmental Determinants of Diabetes in the Young (TEDDY). Diabetes Care 38(5):808–813. https://doi.org/10.2337/dc14-2426
Lampasona V, Liberati D (2016) Islet autoantibodies. Curr Diab Rep 16(6):53. https://doi.org/10.1007/s11892-016-0738-2
McLaughlin KA, Richardson CC, Ravishankar A et al (2016) Identification of tetraspanin-7 as a target of autoantibodies in type 1 diabetes. Diabetes 65(6):1690–1698. https://doi.org/10.2337/db15-1058
Mayer-Davis EJ, Kahkoska AR, Jefferies C et al (2018) ISPAD Clinical Practice Consensus Guidelines 2018: Definition, epidemiology, and classification of diabetes in children and adolescents. Pediatr Diabetes 19(Suppl 27):7–19. https://doi.org/10.1111/pedi.12773
Couper JJ, Haller MJ, Greenbaum CJ et al (2018) ISPAD Clinical Practice Consensus Guidelines 2018: Stages of type 1 diabetes in children and adolescents. Pediatr Diabetes 19(Suppl 27):20–27. https://doi.org/10.1111/pedi.12734
Hameed S, Ellard S, Woodhead HJ et al (2011) Persistently autoantibody negative (PAN) type 1 diabetes mellitus in children. Pediatr Diabetes 12(3 Pt 1):142–149. https://doi.org/10.1111/j.1399-5448.2010.00681.x
Wang J, Miao D, Babu S et al (2007) Prevalence of autoantibody-negative diabetes is not rare at all ages and increases with older age and obesity. J Clin Endocrinol Metab 92(1):88–92. https://doi.org/10.1210/jc.2006-1494
Hattersley AT, Greeley SAW, Polak M et al (2018) ISPAD Clinical Practice Consensus Guidelines 2018: The diagnosis and management of monogenic diabetes in children and adolescents. Pediatr Diabetes 19(Suppl 27):47–63. https://doi.org/10.1111/pedi.12772
Riddle MC, Philipson LH, Rich SS et al (2020) Monogenic diabetes: from genetic insights to population-based precision in care. Reflections From a Diabetes Care Editors’ Expert Forum. Diabetes Care 43(12):3117–3128. https://doi.org/10.2337/dci20-0065
Chung WK, Erion K, Florez JC et al (2020) Precision medicine in diabetes: a Consensus Report from the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 63(9):1671–1693. https://doi.org/10.1007/s00125-020-05181-w
Li M, Wang S, Xu K et al (2020) High prevalence of a monogenic cause in Han Chinese diagnosed with type 1 diabetes, partly driven by nonsyndromic recessive WFS1 mutations. Diabetes 69(1):121–126. https://doi.org/10.2337/db19-0510
Bonfanti R, Colombo C, Nocerino V et al (2009) Insulin gene mutations as cause of diabetes in children negative for five type 1 diabetes autoantibodies. Diabetes Care 32(1):123–125. https://doi.org/10.2337/dc08-0783
Barbetti F, D’Annunzio G (2018) Genetic causes and treatment of neonatal diabetes and early childhood diabetes. Best Pract Res Clin Endocrinol Metab 32(4):575–591. https://doi.org/10.1016/j.beem.2018.06.008
Johnson MB, De Franco E, Lango Allen H et al (2017) Recessively inherited LRBA mutations cause autoimmunity presenting as neonatal diabetes. Diabetes 66(8):2316–2322. https://doi.org/10.2337/db17-0040
Flanagan SE, Haapaniemi E, Russell MA et al (2014) Activating germline mutations in STAT3 cause early-onset multi-organ autoimmune disease. Nat Genet 46(8):812–814. https://doi.org/10.1038/ng.3040
d’Hennezel E, Bin Dhuban K, Torgerson T, Piccirillo C (2012) The immunogenetics of immune dysregulation, polyendocrinopathy, enteropathy, X linked (IPEX) syndrome. J Med Genet 49(5):291–302. https://doi.org/10.1136/jmedgenet-2012-100759
Schwab C, Gabrysch A, Olbrich P et al (2018) Phenotype, penetrance, and treatment of 133 cytotoxic T-lymphocyte antigen 4-insufficient subjects. J Allergy Clin Immunol 142(6):1932–1946. https://doi.org/10.1016/j.jaci.2018.02.055
Proekt I, Miller CN, Lionakis MS, Anderson MS (2017) Insights into immune tolerance from AIRE deficiency. Curr Opin Immunol 49:71–78. https://doi.org/10.1016/j.coi.2017.10.003
Fabbri M, Frixou M, Degano M, Fousteri G (2019) Type 1 diabetes in STAT protein family mutations: regulating the Th17/Treg equilibrium and beyond. Diabetes 68(2):258–265. https://doi.org/10.2337/db18-0627
Lo B, Zhang K, Lu W et al (2015) Autoimmune disease. Patients with LRBA deficiency show CTLA4 loss and immune dysregulation responsive to abatacept therapy. Science 349(6246):436–440. https://doi.org/10.1126/science.aaa1663
Rowshanravan B, Halliday N, Sansom DM (2018) CTLA-4: a moving target in immunotherapy. Blood 131(1):58–67. https://doi.org/10.1182/blood-2017-06-741033
Bollyky JB, Xu P, Butte AJ et al (2015) Heterogeneity in recent-onset type 1 diabetes – a clinical trial perspective. Diabetes Metab Res Rev 31(6):588–594. https://doi.org/10.1002/dmrr.2643
Arif S, Leete P, Nguyen V et al (2014) Blood and islet phenotypes indicate immunological heterogeneity in type 1 diabetes. Diabetes 63(11):3835–3845. https://doi.org/10.2337/db14-0365
Pugliese A, Vendrame F, Reijonen H, Atkinson MA, Campbell-Thompson M, Burke GW (2014) New insight on human type 1 diabetes biology: nPOD and nPOD-transplantation. Curr Diab Rep 14(10):530. https://doi.org/10.1007/s11892-014-0530-0
Leete P, Oram RA, McDonald TJ et al (2020) Studies of insulin and proinsulin in pancreas and serum support the existence of aetiopathological endotypes of type 1 diabetes associated with age at diagnosis. Diabetologia 63(6):1258–1267. https://doi.org/10.1007/s00125-020-05115-6
Damond N, Engler S, Zanotelli VRT et al (2019) A map of human type 1 diabetes progression by imaging mass cytometry. Cell Metab 29(3):755–768.e5. https://doi.org/10.1016/j.cmet.2018.11.014
Carré A, Richardson SJ, Larger E, Mallone R (2021) Presumption of guilt for T cells in type 1 diabetes: lead culprits or partners in crime depending on age of onset? Diabetologia 64(1):15–25. https://doi.org/10.1007/s00125-020-05298-y
Oram RA, Patel K, Hill A et al (2016) A type 1 diabetes genetic risk score can aid discrimination between type 1 and type 2 diabetes in young adults. Diabetes Care 39(3):337–344. https://doi.org/10.2337/dc15-1111
Johnson MB, Patel KA, De Franco E et al (2018) A type 1 diabetes genetic risk score can discriminate monogenic autoimmunity with diabetes from early-onset clustering of polygenic autoimmunity with diabetes. Diabetologia 61(4):862–869. https://doi.org/10.1007/s00125-018-4551-0
Patel KA, Oram RA, Flanagan SE et al (2016) Type 1 diabetes genetic risk score: a novel tool to discriminate monogenic and type 1 diabetes. Diabetes 65(7):2094–2099. https://doi.org/10.2337/db15-1690
Broccanello C, Gerace L, Stevanato P (2020) QuantStudioTM 12K Flex OpenArray® system as a tool for high-throughput genotyping and gene expression analysis. Methods Mol Biol 2065:199–208. https://doi.org/10.1007/978-1-4939-9833-3_15
Li H (2013) Aligning sequence reads, clone sequences and assembly contigs with BWA-MEM. arXiv:1303.3997 [q-bio.GN]. https://doi.org/10.48550/arXiv.1303.3997
Sherry ST, Ward MH, Kholodov K et al (2001) dbSNP: the NCBI database of genetic variation. Nucleic Acids Res 29(1):308–311. https://doi.org/10.1093/nar/29.1.308
Liu X, Jian X, Boerwinkle E (2011) dbNSFP: a lightweight database of human nonsynonymous SNPs and their functional predictions. Hum Mutat 32(8):894–899. https://doi.org/10.1002/humu.21517
Liu X, Li C, Mou C, Dong Y, Tu Y (2020) dbNSFP v4: a comprehensive database of transcript-specific functional predictions and annotations for human nonsynonymous and splice-site SNVs. Genome Med 12(1):103. https://doi.org/10.1186/s13073-020-00803-9
Cingolani P, Platts A, Wang LL et al (2012) A program for annotating and predicting the effects of single nucleotide polymorphisms, SnpEff: SNPs in the genome of Drosophila melanogaster strain w1118; iso-2; iso-3. Fly (Austin) 6(2):80–92. https://doi.org/10.4161/fly.19695
Karczewski KJ, Francioli LC, Tiao G et al (2020) The mutational constraint spectrum quantified from variation in 141,456 humans. Nature 581(7809):434–443. https://doi.org/10.1038/s41586-020-2308-7
Richards S, Aziz N, Bale S et al (2015) Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med 17(5):405–424. https://doi.org/10.1038/gim.2015.30
R Core Team (2020) R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria
Besser REJ, Shepherd MH, McDonald TJ et al (2011) Urinary C-peptide creatinine ratio is a practical outpatient tool for identifying hepatocyte nuclear factor 1-α/hepatocyte nuclear factor 4-α maturity-onset diabetes of the young from long-duration type 1 diabetes. Diabetes Care 34(2):286–291. https://doi.org/10.2337/dc10-1293
Morgan NV, Morris MR, Cangul H et al (2010) Mutations in SLC29A3, encoding an equilibrative nucleoside transporter ENT3, cause a familial histiocytosis syndrome (Faisalabad histiocytosis) and familial Rosai–Dorfman disease. PLoS Genet 6(2):e1000833. https://doi.org/10.1371/journal.pgen.1000833
Chun HJ, Zheng L, Ahmad M et al (2002) Pleiotropic defects in lymphocyte activation caused by caspase-8 mutations lead to human immunodeficiency. Nature 419(6905):395–399. https://doi.org/10.1038/nature01063
Tripodi SI, Mazza C, Moratto D et al (2016) Atypical presentation of autoimmune lymphoproliferative syndrome due to CASP10 mutation. Immunol Lett 177:22–24. https://doi.org/10.1016/j.imlet.2016.07.001
Zhang W, Feng D, Li Y, Iida K, McGrath B, Cavener DR (2006) PERK EIF2AK3 control of pancreatic β cell differentiation and proliferation is required for postnatal glucose homeostasis. Cell Metab 4(6):491–497. https://doi.org/10.1016/j.cmet.2006.11.002
Wen X, Yang Y (2017) Emerging roles of GLIS3 in neonatal diabetes, type 1 and type 2 diabetes. J Mol Endocrinol 58(2):R73–R85. https://doi.org/10.1530/JME-16-0232
Cho H, Mu J, Kim JK et al (2001) Insulin resistance and a diabetes mellitus-like syndrome in mice lacking the protein kinase Akt2 (PKBβ). Science 292(5522):1728–1731. https://doi.org/10.1126/science.292.5522.1728
George S, Rochford JJ, Wolfrum C et al (2004) A family with severe insulin resistance and diabetes due to a mutation in AKT2. Science 304(5675):1325–1328. https://doi.org/10.1126/science.1096706
Shimomura I, Hammer RE, Richardson JA et al (1998) Insulin resistance and diabetes mellitus in transgenic mice expressing nuclear SREBP-1c in adipose tissue: model for congenital generalized lipodystrophy. Genes Dev 12(20):3182–3194. https://doi.org/10.1101/gad.12.20.3182
Redondo MJ, Jeffrey J, Fain PR, Eisenbarth GS, Orban T (2008) Concordance for islet autoimmunity among monozygotic twins. N Engl J Med 359(26):2849–2850. https://doi.org/10.1056/NEJMc0805398
Chen Y-G, Cabrera SM, Jia S et al (2014) Molecular signatures differentiate immune states in type 1 diabetic families. Diabetes 63(11):3960–3973. https://doi.org/10.2337/db14-0214
Marchand L, Li M, Leblicq C et al (2021) Monogenic causes in the Type 1 Diabetes Genetics Consortium cohort: low genetic risk for autoimmunity in case selection. J Clin Endocrinol Metab 106(6):1804–1810. https://doi.org/10.1210/clinem/dgab056
Flannick J, Mercader JM, Fuchsberger C et al (2019) Exome sequencing of 20,791 cases of type 2 diabetes and 24,440 controls. Nature 570(7759):71–76. https://doi.org/10.1038/s41586-019-1231-2
Authors’ relationships and activities
The authors declare that there are no relationships or activities that might bias, or be perceived to bias, their work.
Funding
This study was supported by JDRF Innovative Award 1-INO-2019-789-S to GFo.
Author information
Authors and Affiliations
Contributions
PC, IM, MF, TJ, LM, SC, SBondesan, EZ, NC and SBonfiglio contributed to the acquisition, analysis and interpretation of genetic data. VDG, CB, VF, AL, AC, GFr, AR, CM, MS, FS, VC, GB, AS, AP, MPC and FU contributed to the acquisition, analysis and interpretation of clinical data. IM, VL and GFo drafted the article. PC, EB, RB, MB, AA, MS, LP, VL and GFo contributed to the conception and design of the study and revised it critically. All authors contributed to revising the article and approved the final version of the manuscript. GFo takes full responsibility for the work as a whole, including the study design, access to data and the decision to submit and publish the manuscript.
Corresponding authors
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Paola Carrera and Ilaria Marzinotto are joint first authors
Supplementary information
ESM
(PDF 1.27 mb)
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Carrera, P., Marzinotto, I., Bonfanti, R. et al. Genetic determinants of type 1 diabetes in individuals with weak evidence of islet autoimmunity at disease onset. Diabetologia 66, 695–708 (2023). https://doi.org/10.1007/s00125-022-05865-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-022-05865-5