Abstract
Aims/hypothesis
It is unclear whether glucose per se has a causal impact on risk of stroke and whether glucose-lowering drugs reduce this risk. This is important for the choice of treatment for individuals at risk. We tested the hypotheses that high plasma glucose has a causal impact on increased risk of ischaemic stroke, and that glucose-lowering drugs reduce this risk.
Methods
Using a Mendelian randomisation design, we examined 118,838 individuals from two Copenhagen cohorts, the Copenhagen General Population Study and the Copenhagen City Heart Study, and 440,328 individuals from the MEGASTROKE study. Effects of eight glucose-lowering drugs on risk of stroke were summarised by meta-analyses.
Results
In genetic, causal analyses, a 1 mmol/l higher plasma glucose had a risk ratio of 1.48 (95% CI 1.04, 2.11) for ischaemic stroke in the Copenhagen studies. The corresponding risk ratio from the MEGASTROKE study combined with the Copenhagen studies was 1.74 (1.31, 2.18). In meta-analyses of glucose-lowering drugs, the risk ratio for stroke was 0.85 (0.77, 0.94) for glucagon-like peptide-1 receptor agonists and 0.82 (0.69, 0.98) for thiazolidinediones, while sulfonylureas, dipeptidyl peptidase-4 inhibitors, sodium–glucose cotransporter 2 inhibitors, α-glucosidase inhibitors, meglitinides and metformin individually lacked statistical evidence of an effect on stroke risk.
Conclusions/interpretation
Genetically high plasma glucose has a causal impact on increased risk of ischaemic stroke. Treatment with glucose-lowering glucagon-like peptide-1 receptor agonists and thiazolidinediones reduces this risk. These results may guide clinicians in the treatment of individuals at high risk of ischaemic stroke.
Graphical abstract

Similar content being viewed by others

Introduction
The global prevalence of adults having diabetes mellitus is estimated to be 9.3% in 2019, rising to 10.2% by 2030 [1]. Individuals with diabetes are 1.5 times more likely to have a stroke compared with individuals without, and the prevalence of stroke is 8.4% in individuals with diabetes [1, 2]. In observational studies, high concentrations of plasma glucose have been associated with increased risk of coronary artery disease and ischaemic stroke in individuals with and without diabetes [3,4,5].
Current European Society of Cardiology (ESC), EASD and ADA guidelines have recommendations for patients with type 2 diabetes and a high risk of acute coronary syndrome, heart failure or kidney disease, but do not include recommendations for individuals at a high risk of stroke [6,7,8]. Also, the current recommendation for individuals with diabetes and at high risk of cardiovascular disease is to treat with metformin, and, if this fails, with the addition of a sodium–glucose cotransporter 2 (SGLT2) inhibitor or a glucagon-like peptide-1 receptor agonist (GLP1-RA). However, it is not known whether high plasma glucose has a causal impact on increased risk of ischaemic stroke and therefore whether a similar treatment should be recommended for individuals at high risk of ischaemic stroke. Guidelines help improve quality of diagnosis and care [9], and more specific recommendations on glycaemic control and treatment of diabetes may help reduce the risk of stroke in individuals at high risk.
It is unclear whether the previously documented genetic, causal effect of high plasma glucose on risk of coronary heart disease [3], and an effect of glucose-lowering drugs on reduced risk of coronary artery disease [10], also extend to risk of ischaemic stroke. We therefore tested the hypotheses that high plasma glucose has a genetic, causal impact on risk of ischaemic stroke, and that glucose-lowering drugs reduce this risk.
To investigate whether plasma glucose per se has a causal impact on risk of ischaemic stroke, we used a Mendelian randomisation design. This approach utilises the random assortment of alleles at conception to largely circumvent confounding and reverse causation, as often seen in observational studies [11]. The study design is shown in electronic supplementary material (ESM) Fig. 1. In two cohorts from the Danish general population, the Copenhagen General Population Study (CGPS) and the Copenhagen City Heart Study (CCHS), we: (1) tested whether non-fasting plasma glucose concentrations were associated with risk of ischaemic stroke observationally; (2) tested if genetic variants with known functions and effects on plasma glucose concentrations [3, 12] had similar effects in individuals from the general population; (3) tested whether genetic variants associated with high plasma glucose concentrations also were associated with increased risk of ischaemic stroke, as an indication of causality; (4) performed instrumental variable analysis to obtain causal risk estimates for a 1 mmol/l higher plasma glucose concentration; and (5) validated our results using summary-level data on plasma glucose from the Meta-Analyses of Glucose and Insulin-related traits Consortium (MAGIC) [13,14,15] and ischaemic stroke endpoint data from MEGASTROKE [16, 17]. Finally, to examine whether glucose-lowering treatment reduces the risk of stroke, we combined data from randomised clinical intervention studies on glucose-lowering drugs in a meta-analysis.
Methods
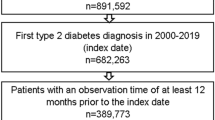
Participants
We included individuals from two similar prospective studies of the Danish general population, the CGPS (n = 107,143) and the CCHS (n = 18,732) [3, 18]. Combining the two general population studies for observational examinations yielded a total of 125,875 individuals of which 118,838 had available genotypes. For additional information refer to the ESM Methods, Participants.
Endpoints
Diagnoses of ischaemic stroke (WHO ICD 8th edition [ICD8] and 10th edition [ICD10] codes, ICD8: 433–434; ICD10: I63) were collected by reviewing all hospital admissions and diagnoses entered in the national Danish Patient Registry and all causes of death entered in the national Danish Causes of Death Registry. For additional information on the diagnostic criteria and validation of diagnoses, refer to the ESM Methods, Diagnostic criteria of ischaemic stroke. Follow-up time began at the first inclusion into a study and ended with censoring at date of death, occurrence of an event, emigration (n = 868) or end of follow-up on 13 December 2018, whichever came first.
Covariates
Non-fasting plasma glucose, total cholesterol, HDL-cholesterol, triacylglycerols and C-peptide were measured using standard hospital assays (Thermo Fisher Scientific, Germany). LDL-cholesterol was calculated using the Friedewald equation if plasma triacylglycerols were ≤4.0 mmol/l and measured by a direct enzymatic method at higher triacylglycerol concentrations. More information on covariates is in the ESM Methods, Covariates.
Genotyping
An ABI PRISM 7900HT (Applied Biosystems, USA) and TaqMan-based assays were used to genotype for glucose-associated genotypes rs10811661 (upstream of CDKN2A and CDKN2B), rs11708067 (ADCY5), rs2191349 (DGKB), rs2943641 (IRS1), rs4607517 (GCK), rs560887 (G6PC2), rs7578326 (IRS1), rs7776061 (GMDS-AS1), rs7903146 (TCF7L2) and rs864745 (JAZF1). These are the genotypes with the strongest effect on plasma glucose in genome-wide association studies; their functions are well known [13] and pleiotropic effects have not been observed. The genetic variants explain 0.3% of the variation in plasma glucose (F = 80.7) in the Copenhagen studies. An externally weighted allele score was constructed by summation of glucose-increasing alleles, weighted by frequency and impact size on plasma glucose. As sensitivity analyses, we estimated the same risks of stroke using seven genetic variants used in a previous paper [19] and using the original 16 genetic variants identified in the first genome-wide association study on glucose traits, although the 16 genetic variants were only available in 23,240 individuals [13] (ESM Table 1).
Statistical analyses
We used StataSE 16.1. (StataCorp, College Station, TX, USA). Deviation from the Hardy–Weinberg equilibrium was tested using Pearson’s χ2 test. Tests for trend across ordered categories of glucose concentrations and the weighted allele score were by the non-parametric Cuzick’s extension of a Wilcoxon rank sum test. We include two closely related but conceptually different genetic analyses: one is using an externally weighted polygenic score where genetic variation is directly associated with plasma glucose, potential confounders/factors in biological pathway/pleiotropic factors and risk of stroke, while the second uses genetically predicted plasma glucose which then is associated with potential confounders/factors in biological pathway/pleiotropic factors and risk of stroke. The latter so-called instrumental variable analysis is used since this allows for direct comparison between genetic and observational analyses of corresponding effect sizes for 1 mmol/l increase in respectively predicted and measured plasma glucose on association with confounders/factors in biological pathway/pleiotropic factors and risk of stroke (see below).
To test whether high plasma glucose was associated with increased risk of ischaemic stroke, we used restricted cubic splines with five knots, selected using the Akaike’s information criterion [20]. Model adjustments were done in three steps: a simple Model A, including adjustment for age, sex and year of birth; Model B, adjusting for potential confounders, including adjustment for age, sex, year of birth, LDL-cholesterol, hypertension, atrial fibrillation, use of lipid-lowering medication, smoking, alcohol consumption, physical activity, education and menopause for women; and Model C, adding to Model B adjustments for covariates potentially in the biological pathway from plasma glucose to risk of ischaemic stroke; that is, BMI, plasma triacylglycerols and HDL-cholesterol. Adjustment for year of birth was included to accommodate changes in diagnostic criteria and treatment over calendar time. To test whether type 2 diabetes mellitus was observationally associated with ischaemic stroke, we used Cox regression models adjusted as above. To test whether the glucose alleles were associated with plasma glucose concentration and risk of ischaemic stroke, simple linear regression and Cox regression models adjusted for age, sex and year of birth were used.
For potential confounders/factors in biological pathway/pleiotropic factors, logistic and linear regressions were used to assess whether the potential confounders/factors in biological pathway/pleiotropic factors were observationally associated with plasma glucose concentrations and ischaemic stroke. An assumption of the Mendelian randomisation design is that the genetic instrument should influence risk of ischaemic stroke only through the exposure of interest, i.e. plasma glucose (ESM Fig. 1). To test this, two-stage least-squares regression with predicted plasma glucose from internal weights found during the first of the two stages for instrumental variable analysis was used to test for association with potential confounders/factors in biological pathway/pleiotropic factors using the user-written ivreg2 and ivpois commands [21], and expressed as an OR for a 1 mmol/l higher plasma glucose.
To test for potential confounding/factors in biological pathway/pleiotropic effects and to compare these potential effects, the association between observational plasma glucose/genetically predicted plasma glucose and continuous covariates was tested using linear regression for observational estimates and two-stage least-squares regression for genetically predicted plasma glucose as described above.
The causal effect of a 1 mmol/l higher plasma glucose concentration on risk of ischaemic stroke was also estimated using instrumental variable analysis by two-stage least-squares regression as described above. The statistical strength of the genetic instrument was confirmed by F statistics for the weighted allele score of 80.7, where F > 10 is considered acceptable [22].
To validate the results and to increase power and generalisability across populations, we conducted a two-sample Mendelian randomisation analysis with summary-level data from MAGIC, including 133,010 individuals without type 2 diabetes [14], and the MEGASTROKE [17] study, with 34,217 cases with ischaemic stroke and 406,111 control participants, including the same genetic variants used in the Copenhagen studies. The MAGIC and MEGASTROKE cohorts are described in the ESM Methods, Statistical analyses, two-sample Mendelian randomisation and the genetic variants used are listed in ESM Table 1. In the present study, data from MEGASTROKE with estimates from European populations were used. Estimates of the causal effect of plasma glucose on risk of ischaemic stroke from summary-level data were obtained by regression analyses using inverse-variance-weighted and Egger regression [23], using the user-written mregger command in Stata [23, 24]. Because Egger regression did not indicate pleiotropy, results were reported as inverse-variance-weighted estimates with Egger estimates also reported in Fig. 3 and the ESM figures. A causal effect summary estimate for the Copenhagen studies and the MEGASTROKE study was obtained for ischaemic stroke by meta-analysis using the metan command. Heterogeneity among studies was low (I2 = 0.02, p = 0.88).
Meta-analysis
To examine whether glucose-lowering drugs reduce the risk of fatal and non-fatal stroke, we performed meta-analyses combining results from clinical randomised trials on the eight most used glucose-lowering drug classes. PubMed, Web of Science and ClinicalTrials.gov were searched for studies. Randomised controlled trials reporting the effect of glucose lowering on risk of stroke and with more than 12 months’ duration of treatment were included. Eligible studies were limited to those in which the sole difference between the intervention and the control group was the drug of interest. For descriptions of methods, search criteria and details of studies included, refer to the ESM Methods, Statistical analyses, Meta-analyses and the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) flow diagrams in ESM Figs 2–9.
Ethics approval
Studies were approved by the Herlev and Gentofte Hospital and by Danish ethical committees (KF-100.2039/91, KF-01-144/01, H-KF-01-144/01). Written informed consent was obtained from participants.
Results
Of 125,875 individuals from the Danish general population, 35% had baseline non-fasting plasma glucose concentrations <5.0 mmol/l, 42% 5.0–5.9 mmol/l, 14% 6.0–6.9 mmol/l and 8.4% had concentrations ≥7.0 mmol/l, with fasting plasma glucose concentrations <6.0 mmol/l considered normal, 6.0–6.9 mmol/l as potentially having impaired glucose tolerance and ≥7.0 mmol/l as potentially having diabetes. During a median of 9.8 years of follow-up (range: 0–42), 5497 individuals developed an ischaemic stroke. Individuals with non-fasting plasma glucose ≥7.0 mmol/l vs <6.0 mmol/l were older; were more often men; had higher plasma triacylglycerol concentrations and BMI; had lower HDL-cholesterol; more often had hypertension, atrial fibrillation, diabetes, an alcohol intake above 14/21 (women/men) units per week and less than 8 years of education; and were less physically active (Table 1 and by study population in ESM Table 2).
Non-fasting glucose and risk of ischaemic stroke: observational estimates
In observational analyses of the general population studies, glucose concentrations above the median of 5.2 mmol/l were associated with a linear increase in age- and sex-adjusted risk of ischaemic stroke (Fig. 1, Model A, upper panel). Multifactorial adjustment attenuated this association (Fig. 1, Model B, middle panel) which was again attenuated when covariates potentially in the biological pathway were also adjusted for (Fig. 1, Model C, lower panel). Multifactorial-adjusted HR for ischaemic stroke was 1.51 (95% CI 1.37, 1.66; p < 0.001) in individuals with type 2 diabetes mellitus vs without (ESM Fig. 10).
Observational prospective risk of ischaemic stroke as a function of plasma glucose concentration in individuals in the general population. Model adjustments were done in three steps: (a) a simple model including adjustment for age, sex and year of birth (Model A); (b) adjusting for potential confounders, including adjustment for age, sex, year of birth, LDL-cholesterol, hypertension, atrial fibrillation, use of lipid-lowering medication, smoking, alcohol consumption, physical activity, education and menopause for women (Model B); and (c) adding to Model B adjustments for covariates potentially in the biological pathway from plasma glucose to risk of ischaemic stroke; that is, BMI, plasma triacylglycerols and HDL-cholesterol (Model C). The solid line is HR, and dashed lines indicate 95% CIs derived from restricted cubic spline regression. To convert glucose values to mg/dl, multiply by 18.02
Genotype and non-fasting plasma glucose
Individuals with a weighted glucose allele score above the 90th percentile had a 4.3% higher plasma glucose compared with those with an allele score below the 20th percentile (Fig. 2). The association of deciles of externally weighted allele scores with plasma glucose is shown in ESM Fig. 11.
Genetic prospective risk of ischaemic stroke as a function of increasing number of weighted alleles in percentile categories. Cox regressions were performed with age as timescale; that is, age adjusted and adjustment for sex and birth year. Follow-up time began at the establishment of the national Danish Patient Registry (1 January 1977) or on the 20th birthday of the individual, whichever came last. ∆%, percentage difference in non-fasting glucose. To convert glucose values to mg/dl, multiply by 18.02
Genotypes and risk of ischaemic stroke: genetic estimates
Both plasma glucose concentration and risk of ischaemic stroke increased stepwise as a function of externally weighted glucose alleles in percentile categories. Using Cox regression, the age-adjusted HR for ischaemic stroke was 1.19 (1.07, 1.32; p < 0.001) in individuals with the highest number of glucose-increasing alleles compared with those with the lowest number of alleles (Fig. 2). Genotype distributions did not deviate from Hardy–Weinberg expectations (p > 0.05).
Potential confounding factors/factors in biological pathway/pleiotropic factors
Age, sex, BMI, plasma C-peptide, hypertension, atrial fibrillation, smoking, physical activity, alcohol consumption, years of education and menopausal status were strongly associated with both plasma glucose and/or risk of ischaemic stroke and may therefore confound the observational associations (ESM Fig. 12).
Plasma glucose predicted from the genetic allele score was associated with only a modest change in BMI (0.48 kg/m2 lower BMI per 1 mmol/l higher genetically predicted plasma glucose), and with none of the other measured covariates, indicating that major pleiotropic effects through any of the above-mentioned factors are not likely in the genetic Mendelian randomisation analyses (ESM Fig. 13).
Causal effect of glucose on risk of ischaemic stroke
In genetic, causal analyses, a 1 mmol/l higher predicted plasma glucose had a risk ratio for ischaemic stroke of 1.48 (95% CI 1.04, 2.11; p = 0.028) (Fig. 3). In sensitivity analyses, using seven or 16 genetic variants, or excluding individuals with diabetes mellitus, gave similar results (ESM Fig. 14). Observationally, a 1 mmol/l higher measured non-fasting plasma glucose had an age- and sex-adjusted HR for ischaemic stroke of 1.13 (1.11, 1.14; p < 0.001), a multifactorial-adjusted HR for ischaemic stroke of 1.06 (1.04, 1.08; p < 0.001) and an HR for ischaemic stroke of 1.05 (1.03, 1.07; p < 0.001) after further adjustment for factors potentially in the biological pathway (Fig. 3).
Risk of ischaemic stroke for a 1 mmol/l higher observationally and causal, genetically determined plasma glucose concentration. Observational HRs were calculated using Cox regression. Because the observational associations between glucose concentrations and ischaemic stroke were only linear at glucose concentrations above the population median (5.2 mmol/l) (Fig. 1), estimates were limited to glucose concentrations above the median. Model adjustments for observational analyses were done in three steps: a simple model including adjustment for age, sex and year of birth (Model A, upper estimate); adjusting for potential confounders, including adjustment for age, sex, year of birth, LDL-cholesterol, hypertension, atrial fibrillation, use of lipid-lowering medication, smoking, alcohol consumption, physical activity, education and menopause for women (Model B, middle estimate); and adding to Model B adjustments for covariates potentially in the biological pathway from plasma glucose to risk of ischaemic stroke; that is, BMI, plasma triacylglycerols and HDL-cholesterol (Model C, lower estimate). Risk ratios for genetically higher plasma glucose were derived from instrumental variable analyses. Causal, genetic risk was also estimated using summary-level data from the MEGASTROKE study on the same ten genetic variants and tested in MAGIC using inverse-variance weighted and Egger regression. The combined result for the Copenhagen studies and MEGASTROKE was using the inverse-variance weighted estimate from MEGASTROKE. IVW, inverse-variance weighted
Using summary-level genetic data from the MEGASTROKE study, the risk ratio for ischaemic stroke for a 1 mmol/l higher predicted plasma glucose was 1.93 (1.55, 2.41; p < 0.001) in an inverse-variance-weighted analysis and 1.79 (1.31, 2.44; p < 0.001) in Egger regression (Fig. 3); results were similar whether ten, seven or 16 genetic variants were used (ESM Fig. 15). The risk for the ischaemic stroke subtypes large artery stroke and small vessel stroke and a combined diagnosis of any stroke showed similar risks, while there was no causal association of glucose with the subtype cardioembolic stroke (ESM Fig. 15).
Combining genetic estimates for risk of ischaemic stroke for a 1 mmol/l higher predicted plasma glucose in the Copenhagen studies and the MEGASTROKE study, the corresponding risk ratio was 1.74 (1.31, 2.18; p < 0.001) (Fig. 3).
Meta-analyses of glucose-lowering drugs
We identified a total of 48 trials eligible for inclusion (ESM Table 3 and individual study estimates in ESM Figs 16–22).
The risk ratio of stroke was 0.85 (95% CI 0.77, 0.94) for GLP1-RA (ΔHbA1c: −6.6 mmol/mol [−0.6%]) and 0.82 (0.69, 0.98) for thiazolidinediones (ΔHbA1c: −1.1 mmol/mol [−0.1%]), while sulfonylureas (ΔHbA1c: −10.9 mmol/mol [−1.0%]), dipeptidyl peptidase-4 inhibitors (ΔHbA1c: −1.1 mmol/mol [−0.1%]), SGLT2 inhibitors (ΔHbA1c: −5.5 mmol/mol [−0.5%]), α-glucosidase inhibitors (ΔHbA1c: −7.7 [−0.7%]), meglitinides (ΔHbA1c: −2.2 mmol/mol [−0.2%]) and metformin (ΔHbA1c: −7.7 mmol/mol [−0.7%]) individually lacked statistical evidence of reduced stroke risk (Fig. 4). Metformin had a borderline effect with a relative risk of 0.66 (0.42, 1.06); however, the studies on metformin were relatively small with few events.
Meta-analyses of risk of stroke (fatal and non-fatal) for randomised clinical intervention trials of more than 12 months’ duration for eight classes of commonly used glucose-lowering drugs. Large diamonds represent summary estimates with 95% CIs. Only one study on meglitinides was included, which is why this is represented by the estimate for this specific study. The solid vertical line represents the reference line of no risk (relative risk = 1). The broken vertical red line and diamond represent the summary estimate of all studies. For information on the individual randomised trials, refer to ESM Methods, Statistical analyses, Meta-analyses, ESM Table 3 and ESM Figs 16–22. ΔeAG, change in estimated average glucose
Test for heterogeneity was low among all studies of glucose-lowering drugs on risk of stroke combined (I2 < 3.8%; p > 0.39), suggesting similar effects within all subclasses examined (ESM Figs 16–22). In all 48 glucose-lowering trials combined, risk of stroke was reduced, with a relative risk of 0.93 (0.88, 0.98; p = 0.01) for a weighted mean reduction in HbA1c of 4.7 mmol/mol (0.43%).
Discussion
We found that genetically high plasma glucose has a causal effect on increased risk of ischaemic stroke, and that treatment with glucose-lowering GLP1-RAs and thiazolidinediones reduces this risk. The reduction observed for GLP1-RAs and thiazolidinediones largely matched what is predicted from their effect on HbA1c in clinical intervention trials and from the genetic estimates in the Copenhagen studies combined with the MEGASTROKE study. These findings are relevant since current ESC [7], EASD [6] and ADA [6] guidelines focus on acute coronary syndrome, heart failure and kidney disease, and do not include recommendations for individuals at a high risk of stroke.
Previous observational studies have shown that ischaemic stroke is prevalent in individuals with diabetes. The Emerging Risk Factors Collaboration (530,083 individuals including 3799 with ischaemic stroke) reported an HR for ischaemic stroke of 2.27 (95% CI 1.95, 2.65) in individuals with diabetes vs without [4]. In the present study we found a similar increase in risk in individuals with diabetes vs without, but also a linear relationship without a threshold between glucose concentrations and risks of ischaemic stroke at glucose concentrations ≥5.8 mmol/l. A similar relationship has been observed for plasma glucose in the Asia Pacific Cohort Study Collaboration [25] and for an HbA1c above approximately 41 mmol/mol (5.9%) in the Atherosclerosis Risk in Communities (ARIC) study [5].
Previous Mendelian randomisation studies have reported causal effects of with type 2 diabetes vs without on risk of ischaemic stroke, with risk ratios of 1.12 (1.07, 1.17) [26] and 1.15 (1.04, 1.28) using genetic variants specifically associated with diabetes mellitus [27]. Studies on the genetic, causal effect of glucose and HbA1c have reported risk ratios for ischaemic stroke of 1.12 (0.98, 1.28) [26] and 1.23 (0.77, 1.95) [28], and, although not significant, estimates were in the same direction and overlap those from the present study, supporting a causal effect of glucose on risk of ischaemic stroke. In the present study, risk estimates for a 1 mmol/l higher plasma glucose concentration are very similar for the Copenhagen studies and the MEGASTROKE study. Although not all estimates were significant, causal estimates from Mendelian randomisation studies so far point in the same direction and suggest a causal effect of both high plasma glucose and diabetes mellitus on risk of stroke [26,27,28]. In the present study the causal effect of high plasma glucose on increased risk of ischaemic stroke was similar for all individuals and when excluding individuals with type 2 diabetes mellitus. Together, this underscores the importance of glycaemic control in reducing risk of stroke even in those without a diagnosis of diabetes mellitus.
The effect of long-term glucose lowering on risk of stroke has been modest in clinical trials, and significant reductions in risk in individual studies have only been reported for the GLP1-RA semaglutide with an HR of 0.61 (0.38, 0.99; p = 0.04; SUSTAIN 6) [29] and dulaglutide with an HR of 0.76 (0.62, 0.94; p = 0.01; Researching Cardiovascular Events with a Weekly Incretin in Diabetes [REWIND]) [30]. For the thiazolidinediones, a subgroup analysis of participants with more than 80% treatment adherence for pioglitazone had an HR of 0.64 (0.42, 0.99; p = 0.04; Insulin Resistance Intervention after Stroke [IRIS] trial) [31], and for recurrent stroke an HR of 0.53 (0.34, 0.85; p = 0.0085; PROspective pioglitazone Clinical Trial In macrovascular Events [PROactive]) [32]. Long-term intensive vs standard glycaemic control has not shown any reductions in risk of cardiovascular disease including stroke [33].
Combining data from studies on all drug classes as in the present meta-analysis, we observed an overall relative risk of 0.93 (0.88, 0.98; p = 0.01) for a mean 4.4 mmol/mol (0.4%) lower HbA1c. This risk reduction was driven by GLP1-RA studies with a combined risk ratio of 0.85 (0.77, 0.94; p = 0.002) and thiazolidinedione studies with a risk ratio of 0.82 (0.69, 0.98; p = 0.025).
GLP1-RA mimics the action of endogenous glucagon-like peptide-1 and stimulates insulin secretion, inhibits glucagon secretion, suppresses endogenous glucose production, reduces appetite and hunger signalling, increases insulin sensitivity secondary to weight loss and delays gastric emptying, thereby reducing postprandial hyperglycaemia. In the present study, GLP1-RA showed some heterogeneity with respect to effect on risk of stroke, with significant reductions in risk observed for the long-acting agonists dulaglutide [30] and semaglutide [29, 34], but no effect for the short-acting lixisenatide [35]. Randomised trials have shown significant reductions in HbA1c, weight, blood pressure, plasma triacylglycerols and NEFA for all GLP1-RAs [30, 35,36,37,38]. The largest effects have been observed for semaglutide, with reductions in HbA1c of 7.7 mmol/mol (0.7%), weight of 4.3 kg and systolic blood pressure of 2.6 mmHg, and 7% and 8% reductions in plasma triacylglycerols and NEFA, respectively. These changes may also contribute to the reduction in risk of stroke. The present findings are in line with results from a meta-analysis of seven GLP1-RAs observing a 15% reduced risk of non-fatal stroke, 19% reduced risk of fatal stroke and 24% reduced risk of total stroke. That meta-analysis also reported non-significant linear reduction in risk of stroke with lower HbA1c concentrations, but no association of reduced body weight with stroke [39].
Thiazolidinediones activate peroxisome proliferator-activated receptor-γ and have a direct effect on beta cells by increasing insulin secretion, preserving long-term beta cell function and having insulin-sensitising effects on skeletal and cardiac muscle, adipose tissue and the liver. Randomised trials of pioglitazone have shown significant reductions in HbA1c, blood pressure, plasma triacylglycerols, NEFA, C-reactive protein and TNF-α, and have improved endothelial function [10]. Similar effects have been reported for rosiglitazone, except that rosiglitazone increases plasma cholesterol and triacylglycerol concentrations [40]. Both pioglitazone and rosiglitazone increase the risk of peripheral oedema and heart failure [40, 41]. Use of rosiglitazone has been limited because of observations from the Diabetes Reduction Assessment with ramipril and rosiglitazone Medication (DREAM) study, with hazard ratios for cardiovascular disease of 1.37 (0.97, 1.94; p = 0.08) and for heart failure of 7.03 (1.60, 30.9; p = 0.01) [42].
Metformin significantly reduces HbA1c, body weight, blood pressure and plasma LDL-cholesterol [43]. Metformin is the most prescribed oral glucose-lowering drug worldwide and is recommended as first line therapy; however, randomised clinical trials on cardiovascular disease are small and existing evidence limited and conflicting. In the present meta-analysis, we observed a non-significant lower risk of stroke, mainly driven by the UK Prospective Diabetes Study (UKPDS) and The Comparative Outcomes Study of Metformin Intervention versus Conventional (COSMIC) Approach Study. Both studies have been criticised for their poor blinding and non-controlled comparator group. More evidence will have to await the Glucose-Lowering In Non-diabetic hyperglycaemia Trial (GLINT, ISRCTN34875079).
Strengths of the present study include examination of a large number of individuals from a genetically homogeneous general population, access to individual participant data of high validity, no losses to follow-up and the use of the Mendelian randomisation design which allows us to assess potential causal effects of glucose on risk of ischaemic stroke, minimising confounding and reverse causation. The causal effect of glucose on risk of ischaemic stroke was reproduced using a two-sample approach with data from the MEGASTROKE study, suggesting that the results may be generalisable to other settings. Also, examining the causal effect of glucose on stroke subtypes in the MEGASTROKE study showed a causal effect on large artery stroke and small vessel stroke, but as expected not on cardioembolic stroke, confirming the validity of the diagnoses.
Limitations include that some of the covariates adjusted for in multifactorial-adjusted observational analyses might be considered on the causal path to ischaemic stroke rather than simple confounders, which may falsely lead to small observational effect estimates of glucose on ischaemic stroke; however, such a potential problem largely does not appear to exist for genetic, causal associations. Nevertheless, the Mendelian randomisation study is limited by a small potential pleiotropic effect of BMI and potentially also by unmeasured factors, although we did not observe pleiotropy via LDL-cholesterol, triacylglycerols, HDL-cholesterol, C-peptide, systolic blood pressure, pack years smoked or alcohol intake. The causal effect of glucose on risk of stroke may be biased in the direction of a more extreme estimate because of linkage equilibrium among the genetic variants used in the main estimates; however, using only seven genetic variants not in linkage disequilibrium gave similar estimates. Population stratification is always a potential problem in genetic analyses; however, in the Copenhagen studies all individuals were white people of Danish descent; that is, the person herself/himself and both parents were all born in Denmark and were Danish citizens, minimising the risk of population stratification as an explanation for our results.
A limitation of the present meta-analysis is the diagnosis of stroke used in clinical randomised trials. Some studies stringently diagnose ischaemic stroke and haemorrhagic stroke (Copenhagen studies and MEGASTROKE), and some only diagnose fatal and non-fatal stroke, which may include ischaemic, cardioembolic and haemorrhagic strokes. This may reduce comparability between the genetic, causal glucose effect on risk of ischaemic stroke from the Copenhagen studies and the estimates of risk obtained from clinical trials. Also, in the present study we selected studies with more than 12 months’ treatment duration and only studies where the drug of interest was evaluated in a balanced design, i.e. the drug vs placebo, or the drug+metformin vs placebo+metformin. This excluded some studies but was done to increase the ability to detect vascular effects of each drug class.
Conclusion
Genetically high plasma glucose had a causal impact on risk of ischaemic stroke. This underscores the importance of glycaemic control in reducing risk of stroke. Treatment with GLP1-RAs and thiazolidinediones reduced the risk of stroke. These findings are relevant since current ESC [7], EASD [6] and ADA [6] recommendations focus on acute coronary syndrome, heart failure and kidney disease, and do not include recommendations for individuals at a high risk of stroke. Inclusion of ischaemic stroke in guidelines on treatment of diabetes and elevated plasma glucose may improve quality of patient diagnosis and care.
Data availability
The datasets analysed during the current study are not publicly available due to GDPR restrictions from the Danish Data Protection Agency, but summary-level data are available from the corresponding author upon reasonable request.
Abbreviations
- CCHS:
-
Copenhagen City Heart Study
- CGPS:
-
Copenhagen General Population Study
- ESC:
-
European Society of Cardiology
- GLP1-RA:
-
Glucagon-like peptide-1 receptor agonist
- MAGIC:
-
Meta-Analyses of Glucose and Insulin-related traits Consortium
- SGLT2:
-
Sodium–glucose cotransporter 2
References
Saeedi P, Petersohn I, Salpea P et al (2019) Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the International Diabetes Federation Diabetes Atlas, 9(th) edition. Diabetes Res Clin Pract 157:107843. https://doi.org/10.1016/j.diabres.2019.107843
Einarson TR, Acs A, Ludwig C, Panton UH (2018) Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc Diabetol 17(1):83
Benn M, Tybjaerg-Hansen A, McCarthy MI, Jensen GB, Grande P, Nordestgaard BG (2012) Nonfasting glucose, ischemic heart disease, and myocardial infarction: a Mendelian randomization study. J Am Coll Cardiol 59(25):2356–2365
Emerging Risk Factors Collaboration, Sarwar N, Gao P et al (2010) Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 375(9733):2215–2222. https://doi.org/10.1016/S0140-6736(10)60484-9
Selvin E, Steffes MW, Zhu H et al (2010) Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med 362(9):800–811. https://doi.org/10.1056/NEJMoa0908359
Buse JB, Wexler DJ, Tsapas A et al (2020) 2019 update to: Management of hyperglycaemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia 63(2):221–228. https://doi.org/10.1007/s00125-019-05039-w
Cosentino F, Grant PJ, Aboyans V et al (2020) 2019 ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J 41(2):255–323. https://doi.org/10.1093/eurheartj/ehz486
Inzucchi SE, Bergenstal RM, Buse JB et al (2012) Management of hyperglycaemia in type 2 diabetes: a patient-centered approach. Position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetologia. 55(6):1577–1596. https://doi.org/10.1007/s00125-012-2534-0
Woolf SH, Grol R, Hutchinson A, Eccles M, Grimshaw J (1999) Clinical guidelines: potential benefits, limitations, and harms of clinical guidelines. BMJ. 318(7182):527–530. https://doi.org/10.1136/bmj.318.7182.527
Ferrannini E, DeFronzo RA (2015) Impact of glucose-lowering drugs on cardiovascular disease in type 2 diabetes. Eur Heart J 36(34):2288–2296. https://doi.org/10.1093/eurheartj/ehv239
Benn M, Nordestgaard BG (2018) From genome-wide association studies to Mendelian randomization: novel opportunities for understanding cardiovascular disease causality, pathogenesis, prevention, and treatment. Cardiovasc Res 114(9):1192–1208. https://doi.org/10.1093/cvr/cvy045
Florez JC, Jablonski KA, Bayley N et al (2006) TCF7L2 polymorphisms and progression to diabetes in the Diabetes Prevention Program. N Engl J Med 355(3):241–250. https://doi.org/10.1056/NEJMoa062418
Dupuis J, Langenberg C, Prokopenko I et al (2010) New genetic loci implicated in fasting glucose homeostasis and their impact on type 2 diabetes risk. Nat Genet 42(2):105–116. https://doi.org/10.1038/ng.520
Scott RA, Lagou V, Welch RP et al (2012) Large-scale association analyses identify new loci influencing glycemic traits and provide insight into the underlying biological pathways. Nat Genet 44(9):991–1005. https://doi.org/10.1038/ng.2385
Hribal ML, Presta I, Procopio T et al (2011) Glucose tolerance, insulin sensitivity and insulin release in European non-diabetic carriers of a polymorphism upstream of CDKN2A and CDKN2B. Diabetologia. 54(4):795–802. https://doi.org/10.1007/s00125-010-2038-8
Malik R, Traylor M, Pulit SL et al (2016) Low-frequency and common genetic variation in ischemic stroke: the METASTROKE collaboration. Neurology. 86(13):1217–1226. https://doi.org/10.1212/WNL.0000000000002528
Malik R, Chauhan G, Traylor M et al (2018) Multiancestry genome-wide association study of 520,000 subjects identifies 32 loci associated with stroke and stroke subtypes. Nat Genet 50(4):524–537. https://doi.org/10.1038/s41588-018-0058-3
Benn M, Nordestgaard BG, Frikke-Schmidt R, Tybjaerg-Hansen A (2017) Low LDL cholesterol, PCSK9 and HMGCR genetic variation, and risk of Alzheimer’s disease and Parkinson’s disease: Mendelian randomisation study. BMJ. 357:j1648. https://doi.org/10.1136/bmj.j1648
Emanuelsson F, Marott SCW, Tybjaerg-Hansen A, Nordestgaard BG, Benn M (2020) Impact of glucose levels on micro- and macrovascular disease in the general population. A Mendelian randomization study. Diabetes Care 43(4):894–902. https://doi.org/10.2337/dc19-1850
Akaike H (1998) Information theory and an extension of the maximum likelihood principle. In: Parzen E, Tanabe K, Kitagawa G (eds) Selected papers of Hirotugu Akaike. Springer, New York, pp 199–213
Nichols A. Ivpois: Stata module for IV/GMM Poisson regression. Stata/SE 13 1 [Internet]. 2007. Available from: http://ideas.repec.org/c/boc/bocode/s456890.html. Accessed 21 Feb 2021
Lawlor DA, Harbord RM, Sterne JA, Timpson N, Davey Smith G (2008) Mendelian randomization: using genes as instruments for making causal inferences in epidemiology. Stat Med 27(8):1133–1163. https://doi.org/10.1002/sim.3034
Burgess S, Bowden J, Fall T, Ingelsson E, Thompson SG (2017) Sensitivity analyses for robust causal inference from Mendelian randomization analyses with multiple genetic variants. Epidemiology. 28(1):30–42. https://doi.org/10.1097/EDE.0000000000000559
Bowden J, Davey SG, Burgess S (2015) Mendelian randomization with invalid instruments: effect estimation and bias detection through Egger regression. Int J Epidemiol 44(2):512–525. https://doi.org/10.1093/ije/dyv080
Lawes CM, Parag V, Bennett DA et al (2004) Blood glucose and risk of cardiovascular disease in the Asia Pacific region. Diabetes Care 27(12):2836–2842. https://doi.org/10.2337/diacare.27.12.2836
Larsson SC, Scott RA, Traylor M et al (2017) Type 2 diabetes, glucose, insulin, BMI, and ischemic stroke subtypes: Mendelian randomization study. Neurology. 89(5):454–460. https://doi.org/10.1212/WNL.0000000000004173
Liu J, Rutten-Jacobs L, Liu M, Markus HS, Traylor M (2018) Causal impact of type 2 diabetes mellitus on cerebral small vessel disease: a Mendelian randomization analysis. Stroke. 49(6):1325–1331. https://doi.org/10.1161/STROKEAHA.117.020536
Au Yeung SL, Luo S, Schooling CM (2018) The impact of glycated hemoglobin (HbA1c) on cardiovascular disease risk: a Mendelian randomization study using UK Biobank. Diabetes Care 41(9):1991–1997. https://doi.org/10.2337/dc18-0289
Marso SP, Bain SC, Consoli A et al (2016) Semaglutide and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med 375(19):1834–1844
Gerstein HC, Colhoun HM, Dagenais GR et al (2019) Dulaglutide and cardiovascular outcomes in type 2 diabetes (REWIND): a double-blind, randomised placebo-controlled trial. Lancet. 394(10193):121–130. https://doi.org/10.1016/S0140-6736(19)31149-3
Spence JD, Viscoli CM, Inzucchi SE et al (2019) Pioglitazone therapy in patients with stroke and prediabetes: a post hoc analysis of the IRIS randomized clinical trial. JAMA Neurol 76(5):526–535. https://doi.org/10.1001/jamaneurol.2019.0079
Wilcox R, Bousser MG, Betteridge DJ et al (2007) Effects of pioglitazone in patients with type 2 diabetes with or without previous stroke: results from PROactive (PROspective pioglitAzone Clinical Trial In macroVascular Events 04). Stroke. 38(3):865–873. https://doi.org/10.1161/01.STR.0000257974.06317.49
Sardar P, Udell JA, Chatterjee S, Bansilal S, Mukherjee D, Farkouh ME (2015) Effect of intensive versus standard blood glucose control in patients with type 2 diabetes mellitus in different regions of the world: systematic review and meta-analysis of randomized controlled trials. J Am Heart Assoc 4(5):e001577
Kristensen SL, Rorth R, Jhund PS et al (2019) Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet Diabetes Endocrinol 7(10):776–785. https://doi.org/10.1016/S2213-8587(19)30249-9
Pfeffer MA, Claggett B, Diaz R et al (2015) Lixisenatide in patients with type 2 diabetes and acute coronary syndrome. N Engl J Med 373(23):2247–2257. https://doi.org/10.1056/NEJMoa1509225
Marso SP, Daniels GH, Brown-Frandsen K et al (2016) Liraglutide and cardiovascular outcomes in type 2 diabetes. N Engl J Med 375(4):311–322. https://doi.org/10.1056/NEJMoa1603827
Holman RR, Bethel MA, Mentz RJ et al (2017) Effects of once-weekly exenatide on cardiovascular outcomes in type 2 diabetes. N Engl J Med 377(13):1228–1239. https://doi.org/10.1056/NEJMoa1612917
Hernandez AF, Green JB, Janmohamed S et al (2018) Albiglutide and cardiovascular outcomes in patients with type 2 diabetes and cardiovascular disease (Harmony Outcomes): a double-blind, randomised placebo-controlled trial. Lancet. 392(10157):1519–1529. https://doi.org/10.1016/S0140-6736(18)32261-X
Bellastella G, Maiorino MI, Longo M, Scappaticcio L, Chiodini P, Esposito K, Giugliano D (2020) Glucagon-like peptide-1 receptor agonists and prevention of stroke systematic review of cardiovascular outcome trials with meta-analysis. Stroke. 51(2):666–669. https://doi.org/10.1161/STROKEAHA.119.027557
van Wijk JP, de Koning EJ, Martens EP, Rabelink TJ (2003) Thiazolidinediones and blood lipids in type 2 diabetes. Arterioscler Thromb Vasc Biol 23(10):1744–1749. https://doi.org/10.1161/01.ATV.0000090521.25968.4D
Dormandy JA, Charbonnel B, Eckland DJ et al (2005) Secondary prevention of macrovascular events in patients with type 2 diabetes in the PROactive Study (PROspective pioglitAzone Clinical Trial In macroVascular Events): a randomised controlled trial. Lancet. 366(9493):1279–1289. https://doi.org/10.1016/S0140-6736(05)67528-9
DREAM (Diabetes Reduction Assessment with ramipril and rosiglitazone Medication) Trial Investigators, Gerstein HC, Yusuf S et al (2006) Effect of rosiglitazone on the frequency of diabetes in patients with impaired glucose tolerance or impaired fasting glucose: a randomised controlled trial. Lancet 368(9541):1096–1105. https://doi.org/10.1016/S0140-6736(06)69420-8
Lundby-Christensen L, Tarnow L, Boesgaard TW et al (2016) Metformin versus placebo in combination with insulin analogues in patients with type 2 diabetes mellitus-the randomised, blinded Copenhagen Insulin and Metformin Therapy (CIMT) trial. BMJ Open 6(2):e008376. https://doi.org/10.1136/bmjopen-2015-008376
Acknowledgements
We are indebted to participants and staff of the Copenhagen General Population Study and the Copenhagen City Heart Study. We also thank the participants of MAGIC [13] and the MEGASTROKE study [16, 17] for their generous participation, and the consortia for making data publicly available. These results may guide clinicians in the treatment of individuals at high risk of ischaemic stroke.
Authors’ relationships and activities
BGN reports consultancy services for Novo Nordisk and Sanofi. The other authors have no conflicts of interest.
Funding
Funding sources were the Danish Council for Independent Research, Medical Sciences (DFF-4183-00171); Rigshospitalets Forskningsfond; and Herlev-Gentofte Hospital. The funding sources had no role in the study design, collection of data, writing of the report or decision to submit the article for publication.
Author information
Authors and Affiliations
Contributions
All authors take public responsibility for the content and contributed to the conception, study design and data collection of the work presented by the article. MB and FE were responsible for the literature search and statistical analyses, MB wrote the manuscript draft and all authors contributed to the revision of critically important content. MB and BGN take responsibility for the integrity and accuracy of the data and are the guarantors of this manuscript. All authors had full access to the data and have approved the final version to be published.
Corresponding author
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM
(PDF 648 kb)
Rights and permissions
About this article
Cite this article
Benn, M., Emanuelsson, F., Tybjærg-Hansen, A. et al. Impact of high glucose levels and glucose lowering on risk of ischaemic stroke: a Mendelian randomisation study and meta-analysis. Diabetologia 64, 1492–1503 (2021). https://doi.org/10.1007/s00125-021-05436-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-021-05436-0