Abstract
Aims/hypothesis
The aim of this study was to investigate the association of N-terminal pro-brain natriuretic peptide (NT-proBNP) with traditional cardiovascular risk factors and incident cardiovascular events in older people with type 2 diabetes.
Methods
In the prospective phase of the Edinburgh Type 2 Diabetes Study, 1066 men and women aged 60 to 75 years with type 2 diabetes mellitus were followed for 4 years; 112 participants had an incident cardiovascular event. At baseline, cardiovascular risk factors, pre-existing cardiovascular disease and levels of NT-proBNP were evaluated.
Results
Raised plasma NT-proBNP levels were associated with these classical cardiovascular risk factors: increased duration of diabetes, use of insulin, raised BMI, reduced HDL-cholesterol, reduced renal function and use of lipid-lowering and anti-hypertensive medication (all p < 0.05). In the prospective analysis, NT-proBNP was strongly associated with subsequent risk of all cardiovascular disease events (HR per one SD increase in NT-proBNP 1.39; 95% CI 1.10, 1.75), independent of cardiovascular risk factors traditionally used to predict vascular events. NT-proBNP was also independently associated with incident coronary artery disease events (1.48, 95% CI 1.10, 1.98). The addition of NT-proBNP to multivariate models improved the C-index by 0.019 for the ‘hard’ cardiac endpoint (fatal and non-fatal myocardial infarction).
Conclusions/interpretation
In older people with type 2 diabetes, NT-proBNP is associated with the development of coronary and cerebrovascular events, independent of a wide range of other vascular and metabolic risk factors, and may prove a useful addition to current vascular risk scores in diabetes populations.
Similar content being viewed by others
Introduction
Brain natriuretic peptide (BNP) is a 32 amino acid polypeptide released by the heart in response to increased pressure on the ventricular wall. On secretion, BNP is split into the biologically active peptide and the non-functional N-terminal fragment (NT-proBNP), which has a longer circulating half-life. NT-proBNP levels are used clinically to rule out heart failure on presentation with dyspnoea. Recently, a number of potentially useful markers, notably C-reactive protein [1], have been identified as candidates to improve the stratification of individuals according to their risk of developing subsequent cardiovascular disease (CVD). Indeed some clinical guidelines have started to recommend testing for such biomarkers in clinical settings [2], although the use of C-reactive protein for widespread testing remains debatable [1]. In a number of general population, primary prevention and high-risk cohort studies, NT-proBNP has been shown to be strongly associated with risk of CVD and appears to have prognostic value over and above that of traditional risk factors [3–9]. However, the ability of NT-proBNP to predict cardiovascular events in specific conditions such as type 2 diabetes is less extensively studied.
Current clinical risk scores perform inadequately in risk prediction in type 2 diabetes [10–12]. To date, most studies investigating the predictive value of NT-proBNP in diabetic patients have been limited, for example by small sample sizes [13, 14], predominantly male samples [15] or a short follow-up period [16]. One recently published study [17] suggests that NT-proBNP is a strong independent predictor of cardiovascular mortality in unselected older patients with type 2 diabetes; however, 36% of the cohort was below 65 years of age at baseline and the results did not include non-fatal cardiovascular events. These findings have now also been confirmed in patients selected to participate in a clinical trial [18].
The Edinburgh Type 2 Diabetes Study (ET2DS), established in 2007 as a representative cohort of elderly men and women with type 2 diabetes, living in Lothian, Scotland, provides a relatively unique opportunity to determine the association between baseline NT-proBNP levels and the subsequent development of cardiovascular outcomes in a large sample of elderly patients with type 2 diabetes. The aims of the current study were to investigate the association between NT-proBNP and variables related to an adverse cardiometabolic profile in type 2 diabetes and to explore the potential prognostic value of the peptide in terms of association with subsequent cardiovascular events over and above traditional cardiovascular risk factors.
Methods
Study population
The ET2DS is a population-based, prospective cohort study involving 1066 men and women aged between 60 and 75 years with established type 2 diabetes mellitus living in the Lothian region of central Scotland. In 2006/2007, participants were recruited at random using a comprehensive database of people with type 2 diabetes living in Lothian (the Lothian Diabetes Register). Data collected at baseline were based on physical examination and questionnaires on demographic characteristics, cardiovascular risk factors and angina, chest pain and myocardial infarction diagnoses. The recruitment of patients and study protocol of the ET2DS has been described in detail previously [19]. The ET2DS population has been shown previously to be largely representative of all patients aged 60–75 years with type 2 diabetes living in Lothian [20]. In 2010/2011, all surviving participants were followed-up for cardiovascular events. Use of routine data sources (record linkage) and GP/hospital notes as well as direct patient contact ensured that follow-up included all ET2DS participants.
All the study participants gave their informed consent and ethics permission was obtained from the Lothian Medical Research Ethics Committee.
Physical examination
ET2DS participants attended a dedicated research clinic at baseline for physical examination and blood sampling. Physical examination included measurement of height and weight for the calculation of BMI. A self-administered questionnaire was used to collect data on age, sex, diabetes history, social status, smoking habits and history of CVD. A venous blood sample was taken for measurement of HbA1c, total cholesterol, HDL-cholesterol and estimated GFR (eGFR). An early morning urine specimen was collected for measurement of urinary albumin and creatinine for calculation of the albumin:creatinine ratio (ACR). Systolic and diastolic brachial blood pressures were also measured and data on diabetic, and other, medication use were collected by questionnaire. The Scottish Index of Multiple Deprivation (SIMD) was used to assess social status and is defined by the Scottish Government as a composite index combining 38 indicators across seven domains (income, employment, health, education, skills and training, housing, geographic access and crime).
Determination of NT-proBNP
Fasting blood samples were taken at the research clinic and plasma was frozen for storage. Plasma NT-proBNP concentrations were determined using the Elecsys 2010 electrochemiluminescence method (Roche Diagnostics, Burgess Hill, UK), and calibrated using the manufacturer’s reagents. The manufacturer’s controls were used with limits of acceptability defined by the manufacturer. Low control coefficient of variation was 6.7% and high control coefficient of variation was 4.9%.
Assessment of CVD events
At baseline, data were recorded on self-reporting of a doctor’s diagnosis of CVD, the WHO chest pain and Edinburgh Claudication questionnaires (part of the self-completion participant questionnaire) and findings on a standard 12-lead ECG. Data were also collected from the Information Services Division (ISD) of National Health Service (NHS) Health Services Scotland on all medical and surgical discharges from Scottish hospitals since 1981 and all ICD-10 codes (www.who.int/classifications/icd/en/) for cardiovascular or cerebrovascular disease were extracted. These data were combined to assess prevalent CVD (myocardial infarction [MI], angina, transient ischaemic attack [TIA], stroke and diagnosis of heart failure) at baseline, according to predefined criteria [20]. The ICD-10 code for heart failure as a diagnosis on hospital discharge records was used to identify heart failure.
Four years after recruitment, participants were followed-up for new cardiovascular (CV) events using a combination of repeat self-completion questionnaire, repeat ISD record linkage for hospital discharge and death certificate data, and review of clinical case notes, as required. Criteria for fatal and non-fatal events were as follows. MI: (1) ICD-10 code for new MI on hospital discharge/death record, dated after baseline, plus either participant report of a doctor diagnosis of MI, positive WHO chest pain questionnaire for MI, report of MI on GP questionnaire (provided all the dates were consistent with the ICD-10-coded event) or ECG codes for MI that were not present at baseline; or (2) clinical criteria for MI met following scrutiny of hospital and/or GP notes. New angina (in participants without a diagnosis of angina at baseline): (1) ICD-10 code for angina as primary diagnosis on hospital discharge record, dated after baseline; or (2) at least two of (a) patient self-report of a doctor diagnosis of angina or of starting angina medication since baseline, (b) ECG codes for ischaemia that were not present at baseline and (c) positive WHO chest pain questionnaire; or (3) clinical diagnosis of angina on scrutiny of hospital notes. Fatal ischaemic heart disease (IHD): ICD-10 codes for IHD (other than MI) as the underlying cause of death from death certification data. Stroke: (1) ICD-10 code for stroke as primary diagnosis on hospital discharge/death record, dated after baseline; or (2) clinical criteria for stroke met on scrutiny of clinical notes in patients with either self-report of stroke or with non-primary ICD-10 hospital discharge/death code for stroke. TIA: (1) ICD-10 code for TIA as primary diagnosis on hospital discharge record; or (2) clinical criteria for TIA met on scrutiny of clinical notes in patients with either self-report of stroke or with non-primary ICD-10 hospital discharge code for stroke or TIA.
Statistical analysis
The distribution of NT-proBNP was right-skewed and was therefore log-transformed (using the natural logarithm, log e ) in all analyses, as was duration of diabetes, which was also heavily skewed. NT-proBNP and duration of diabetes are given as medians with interquartile range (IQR). All other continuous variables are given as means ± SD and the categorical variables are given as total numbers with corresponding percentages. The Pearson correlation coefficient and test of association were used to assess the relationships between NT-proBNP and continuous covariates. The relationships between NT-proBNP and categorical covariates were tested using one-way ANOVAs. The Cox proportional hazards model was used to assess the prognostic value of NT-proBNP to the risk of a cardiovascular event. An incident CV event was considered to be the first incident CV event (fatal and non-fatal MI or stroke, fatal IHD, angina and TIA) suffered by a patient since their initial baseline visit to the clinic. Results were summarised by HR with corresponding 95% confidence intervals and p values.
Analyses explored four different models: a crude model including NT-proBNP alone; a model adjusted for age, sex and baseline CVD status (presence of one or more cardiovascular events recorded at baseline); a model adjusted additionally for ‘traditional’ cardiovascular risk factors (age, sex, baseline CVD status, duration of diabetes, treatment of diabetes, lipid-lowering drugs, BP-lowering drugs, smoking status, BMI, systolic BP [sBP], diastolic BP [dBP]), HbA1c, HDL-cholesterol and total cholesterol; and a model adjusted additionally for traditional cardiovascular risk factors plus social status (represented by SIMD), eGFR and presence of microalbuminuria (defined as an ACR of >2.5 in men and >3.5 in women). Two sub-sets of overall cardiovascular events were considered during the analysis: coronary artery disease (CAD; fatal and non-fatal MI, angina and fatal IHD) and cerebrovascular disease (fatal and non-fatal stroke and TIA). In addition, a sensitivity analysis that included only ‘hard’ CV endpoints (fatal and non-fatal MI, fatal and non-fatal stroke and fatal IHD) was performed.
A p value of <0.05 was taken to be statistically significant.
Harrell’s C-index was calculated for all models [21] to assess predictive performance using the concordance between model predictions and observed outcomes. The C-index is a generalisation of the area under the receiver operator curve for survival data, and ranges from 0.5, which indicates no predictive ability in the model, to 1, which indicates that the model has perfect predictive ability. In predicting event-free survival, the C-index considers all possible pairs of participants, at least one of whom has experienced an event. The C-index is the overall probability of concordance between observed and predicted event-free survival time between pairs.
Results
Study characteristics at baseline and incident cardiovascular events
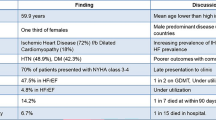
A total of 1066 participants (547 men and 519 women) were followed for 4 years. At baseline, the median NT-proBNP level was 75 pg/ml (IQR 37–169). The mean age of the study population was 67.9 ± 4.2 years; other characteristics of the participants are shown in Table 1. The baseline prevalence of MI, angina, stroke and TIA was 14% (n = 150), 28% (n = 298), 6% (n = 62) and 3% (n = 31), respectively. The baseline prevalence of heart failure was 5.3% (n = 56) and eight patients had a diagnosis of heart failure without the occurrence of a cardiovascular event (MI, angina, stroke or TIA).
A total of 112 first incident cardiovascular events (affecting 10.5% of the study population) occurred during the follow-up period of 4 years; 29 (2.7%) patients suffered a non-fatal MI and a further 5 (0.5%) died from MI; 27 (2.9%) developed angina; 28 (2.6%) suffered a non-fatal stroke and a further 3 (0.3%) died from stroke; 8 (1.0%) had a TIA and 12 (1.1%) died from IHD that was not specified as a fatal MI.
Association of NT-proBNP with cardiometabolic risk factors and vascular disease at baseline
At baseline, raised NT-proBNP levels were significantly associated with several aspects of an adverse CV risk profile (Table 1), including increasing age (r = 0.25, p < 0.001), higher BMI (r = 0.06, p < 0.05) and lower HDL-cholesterol levels (r = −0.07, p < 0.05). NT-proBNP levels were also lower in the least deprived fifth of deprivation index compared with levels in the most deprived category (geometric mean 73.94 pg/ml, 95% CI [65.36, 83.64] vs 97.10 pg/ml, 95% CI [78.13, 120.68]; p < 0.05). However, NT-proBNP levels were inversely associated with dBP (r = −0.14, p < 0.001) and total cholesterol (r = −0.10, p < 0.001). These findings may have been influenced by the high proportion of the study population taking lipid-lowering medication (85.7%) and anti-hypertensive medication (82.3%), especially given the statistically significant higher level of NT-proBNP in these groups compared with participants not taking the medication (geometric mean 83.87 pg/ml, 95% CI [77.51, 90.74] vs 67.67 pg/ml, 95% CI [56.58, 80.94] and 87.32 pg/ml, 95% CI [80.71, 94.48] vs 59.79 pg/ml, 95% CI [50.11, 71.33], respectively; p < 0.05 and p < 0.001, respectively). NT-proBNP levels were also associated with a more severe diabetes profile, with higher levels in participants who reported a longer duration of diabetes (r = 0.13, p < 0.001) and in those using insulin to control their diabetes compared with those using diet and tablets to control theirs (geometric mean 108.90 pg/ml, 95% CI [90.50, 131.05] vs 72.62 pg/ml, 95% CI [62.30, 84.65] and 77.41 pg/ml, 95% CI [70.76, 84.69], respectively; p < 0.001). However, apart from age, these associations with NT-proBNP were weak. The strongest associations were between raised NT-proBNP and lower renal function (eGFR correlation coefficient −0.33, p < 0.05; geometric mean 151.1 pg/ml, 95% CI [124.6, 183.2] vs 72.3 pg/ml, 95% CI [67.0, 78.0] for presence vs absence of microalbuminuria) and between NT-proBNP and prevalent CVD (geometric mean 374.53 pg/ml, 95% CI [282.96, 495.74] vs 75.04 pg/ml, 95% CI [69.88, 80.58]; 227.20 pg/ml, 95% CI [189.87, 271.87] vs 68.98 pg/ml, 95% CI [64.11, 74.22] and 164.86 pg/ml, 95% CI [144.09, 188.62] vs 61.98 pg/ml, 95% CI [57.36, 66.96] for presence vs absence of heart failure, MI and angina, respectively; all p < 0.001).
Association of NT-proBNP with incident cardiovascular events
Prior to any multivariate adjustment, a one SD increase in log NT-proBNP was associated with a 1.77-fold increase (p < 0.001) in the risk of all cardiovascular events, a 1.79-fold increase (p < 0.001) in the risk of CAD events and a 1.73-fold increase (p < 0.001) in the risk of cerebrovascular events. A statistically significant association of NT-proBNP with all CV events and with CAD persisted after multivariate adjustments that included baseline vascular disease and vascular risk factors (Table 2). The HRs for a one SD increase in log NT-proBNP were 1.46 (95% CI 1.19, 1.80) and 1.58 (95% CI 1.30, 1.93) for models adjusting for age, sex and baseline CV status that included or excluded heart failure, respectively. A one SD increase in log NT-proBNP was associated with a 1.39-fold increase (p = 0.006) in the risk of any CV event, after adjustment for baseline vascular disease, traditional CV risk factors, social status and reduced kidney function, and with a 1.48-fold increase (p = 0.009) in the risk of a CAD event. Meaningful multivariate analysis of the cerebrovascular disease subgroup was constrained by the small number of observed events in this group (n = 39, multi-adjusted HR 1.32, 95% CI 0.90, 1.93; p = 0.163) and was not considered further. Compared with these relatively large increases in risk associated with NT-proBNP levels, a one SD increase in total cholesterol was associated with a non-significant, 1.22-fold (95% CI 0.98, 1.52; p = 0.08) increase in risk of all cardiovascular events after full multivariate adjustment, with comparable figures of 1.25 (95% CI 1.00, 1.56; p = 0.04) for a one SD increase in sBP.
An overall change in the C-index was seen when comparing models with and without NT-proBNP (Table 2). The C-index improved by 0.008 with the addition of NT-proBNP to the fully adjusted model for all cardiovascular events and for CAD events.
Results appeared somewhat more robust when only ‘hard’ CV endpoints were considered, with fully adjusted HRs increasing to 1.86 (95% CI 1.25, 2.78; p = 0.002) for CAD and 1.51 (95% CI 1.13, 2.01; p = 0.006) for all CV events (Table 2)––the C-index point estimate difference was also greater when only hard CV endpoints were considered, improving by 0.019 and 0.013, respectively. Interestingly, given recent evidence on proteinuria as a strong vascular risk predictor [2], the C-index for model C did not improve when microalbuminuria was added after the inclusion of NT-proBNP, with the HR remaining unchanged.
Discussion
In older people with type 2 diabetes, plasma NT-proBNP levels were associated with several aspects of an adverse cardiometabolic profile: increased duration of diabetes, use of insulin, raised BMI, lower HDL-cholesterol, lower renal function and use of lipid-lowering and anti-hypertensive medication. In the prospective analysis, NT-proBNP was strongly associated with subsequent risk of CVD events, independent of such differences in cardiometabolic profile and a range of cardiovascular risk factors traditionally used to predict vascular events.
Our findings are consistent with those of previous studies that have found NT-proBNP to be increased in older patients with longer diabetes duration and to associate with higher sBP and impaired kidney function [11, 22]. Furthermore, we confirm that NT-proBNP levels are related to social class, with levels being higher in the most deprived group of diabetes patients, a finding which extends our similar observation in the predominantly non-diabetes WOSCOPS study population [3].
Our data support NT-proBNP as a potentially useful risk predictor in older patients with type 2 diabetes—a group of patients who are at an elevated risk of vascular disease. This confirms the recent findings of Bruno et al [17], who suggested that NT-proBNP may have a role as a marker of early CVD in a predominantly elderly study population. Although the improvements in the C-index following the inclusion of NT-proBNP are small and the clinical impact of including NT-proBNP requires further assessment, it has been proposed that the C-index can be insensitive when adding a new predictor to a model, even if such a predictor has an independent and statistically significant contribution to a prediction model [23]. Further large studies are needed to determine whether the same findings apply to younger patients with type 2 diabetes. However, recently published findings from the ADVANCE trial [18] found that NT-proBNP was a strong predictor of CV events and death, regardless of the age of the patient (younger or older than 67 years), suggesting that older age is not a prerequisite for the potential usefulness of NT-proBNP in long-term CV risk prediction. This result is also consistent with findings that the short-term (mean 11 months follow-up) predictive power of NT-proBNP was similar in patients both younger and older than 60 years of age [24].
Our finding that NT-proBNP is significantly associated with CV events, even after consideration of lipid-lowering and anti-hypertensive therapy, is particularly noteworthy. In this regard, it is notable that cholesterol levels in ET2DS participants were not predictive of events, likely in part because of the confounding effect of lipid-lowering treatment on lipid levels. Given that the vast majority of type 2 diabetes patients are on lipid-lowering therapy, our findings suggest NT-proBNP may be a particularly useful predictor in contemporary type 2 diabetes populations.
The strengths and weaknesses of the current study must be considered. The assessment of links between ‘novel’ biomarkers and incident vascular disease, independent of established cardiovascular risk factors and other biomarkers, can be difficult, owing to the inter-relationships between different measures of vascular disease and vascular risk factors, and the problems associated with comprehensive and accurate follow-up for vascular events over time (this goes some way to explaining inconsistencies in the current literature). Compared with some previous studies, the relatively larger size, population-based approach and prospective design with scrupulous assessment for incident CV events, are strengths of the current study. The use of an exclusively diabetic older population and the measurement of a large number of classical vascular risk factors and other strong predictors in diabetes (including diabetes duration, albuminuria and social class) has provided a unique contribution to the existing literature, which has neglected investigations in older diabetes patients, despite the increased prevalence of macrovascular disease in this population.
Future work in the ET2DS, which will include assessment of cardiovascular events over a longer follow-up period, will enable further, adequately powered risk prediction analysis, including the use of techniques such as net reclassification index. Such analysis will determine whether NT-proBNP adds additional value over specific CV risk scores that are currently used in diabetes. It will also be important to compare the predictive value of NT-proBNP with other ‘novel’ biomarkers of CV disease and to determine whether NT-proBNP is associated with other vascular-related complications of type 2 diabetes. In this respect, we have already shown that NT-proBNP is associated with age-related cognitive decline in the ET2DS [25, 26], a finding recently confirmed in older patients with CVD, or at an elevated risk, in the PROSPER study [27].
In conclusion, the present study confirms a relatively strong association of NT-proBNP with vascular outcomes in patients with type 2 diabetes, independently of a range of other vascular and metabolic risk factors, inclusive of diabetes duration and albuminuria. Further studies addressing NT-proBNP in vascular prediction in diabetes are indicated.
Abbreviations
- ACR:
-
Albumin:creatinine ratio
- BNP:
-
Brain natriuretic peptide
- CAD:
-
Coronary artery disease
- CV:
-
Cardiovascular
- CVD:
-
Cardiovascular disease
- dBP:
-
Diastolic BP
- eGFR:
-
Estimated GFR
- ET2DS:
-
Edinburgh Type 2 Diabetes Study
- GP:
-
General practitioner
- IHD:
-
Ischaemic heart disease
- IQR:
-
Interquartile range
- ISD:
-
Information Services Division
- MI:
-
Myocardial infarction
- NHS:
-
National Health Service
- NT-proBNP:
-
N-terminal pro-brain natriuretic peptide
- SIMD:
-
Scottish Index of Multiple Deprivation
- sBP:
-
Systolic BP
- TIA:
-
Transient ischaemic attack
References
Emerging Risk Factors Collaboration (2012) C-reactive protein, fibrinogen, and cardiovascular disease prediction. N Engl J Med 367:1310–1320
Rydén L, Grant P, Anker SD et al (2013) ESC guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD. Eur Heart J 34:3035–3087
Welsh P, Doolin O, Willeit P et al (2013) N-terminal pro-B-type natriuretic peptide and the prediction of primary cardiovascular events: results from 15-year follow-up of WOSCOPS. Eur Heart J 34:443–450
Wannamethee SG, Welsh P, Lowe GD et al (2011) N-terminal pro-brain natriuretic peptide is a more useful predictor of cardiovascular disease risk than C-reactive protein in older men with and without pre-existing cardiovascular disease. J Am Coll Cardiol 58:56–64
Linssen GCM, Bakker SJL, Voors AA et al (2010) N-terminal pro-B-type natriuretic peptide is an independent predictor of cardiovascular morbidity and mortality in the general population. Eur Heart J 31:120–127
Blankenberg S, Zeller T, Saarela O et al (2010) Contribution of 30 biomarkers to 10-year cardiovascular risk estimation in 2 population cohorts: the MONICA, risk, genetics, archiving, and monograph (MORGAM) biomarker project. Circulation 121:2388–2397
Kistorp C, Raymond I, Pedersen F, Gustafsson F, Faber J, Hildebrandt P (2005) N-terminal pro-brain natriuretic peptide, C-reactive protein, and urinary albumin levels as predictors of mortality and cardiovascular events in older adults. JAMA 293:1609–1616
Olsen MH, Hansen TW, Christensen MK et al (2007) N-terminal pro-brain natriuretic peptide, but not high sensitivity C-reactive protein, improves cardiovascular risk prediction in the general population. Eur Heart J 28:1374–1381
Wang TJ, Larson MG, Levy D et al (2004) Plasma natriuretic peptide levels and the risk of cardiovascular events and death. N Engl J Med 350:655–663
Simmons RK, Coleman RL, Price HC et al (2009) Performance of the UK prospective diabetes study risk engine and the Framingham risk equations in estimating cardiovascular disease in the EPIC-Norfolk cohort. Diabetes Care 32:708–713
van der Heijden AAWA, Ortegon MM, Niessen LW, Nijpels G, Dekker JM (2009) Prediction of coronary heart disease risk in a general, pre-diabetic, and diabetic population during 10 years of follow-up: accuracy of the Framingham, SCORE, and UKPDS risk functions: the Hoorn Study. Diabetes Care 32:2094–2098
van Dieren S, Beulens JWJ, Kengne AP et al (2012) Prediction models for the risk of cardiovascular disease in patients with type 2 diabetes: a systematic review. Heart 98:360–369
Gæde P, Hildebrandt P, Hess G, Parving HH, Pedersen O (2005) Plasma N-terminal pro-brain natriuretic peptide as a major risk marker for cardiovascular disease in patients with type 2 diabetes and microalbuminuria. Diabetologia 48:156–163
Tarnow L, Gall MA, Hansen BV, Hovind P, Parving HH (2006) Plasma N-terminal pro-B-type natriuretic peptide and mortality in type 2 diabetes. Diabetologia 49:2256–2262
Bhalla MA, Chiang A, Epshteyn VA et al (2004) Prognostic role of B-type natriuretic peptide levels in patients with type 2 diabetes mellitus. J Am Coll Cardiol 44:1047–1052
Huelsmann M, Neuhold S, Strunk G et al (2008) (2008) NT-proBNP has a nigh negative predictive value to rule-out short-term cardiovascular events in patients with diabetes mellitus. Eur Heart J 29:2259–2264
Bruno G, Landi A, Barutta F et al (2013) NH2-terminal probrain natriuretic peptide is a stronger predictor of cardiovascular mortality than C-reactive protein and albumin excretion rate in elderly patients with type 2 diabetes. Diabetes Care 36:2677–2682
Hillis GS, Welsh P, Chalmers J et al (2014) The relative and combined ability of high-sensitivity cardiac troponin T and N-terminal pro-B-type natriuretic peptide to predict cardiovascular events and death in patients with type 2 diabetes. Diabetes Care 37:295–303
Price JF, Reynolds RM, Mitchell RJ et al (2008) The Edinburgh type 2 diabetes study: study protocol. BMC Endocr Disord 8:18
Marioni RE, Strachan MWJ, Reynolds RM et al (2010) Association between raised inflammatory markers and cognitive decline in elderly people with type 2 diabetes: the Edinburgh Type 2 Diabetes Study. Diabetes 59:710–713
Harrell FE, Lee KL, Mark DB (1996) Multivariable prognostic models: issues in developing models, evaluating assumptions and adequacy, and measuring and reducing errors. Stat Med 15:361–387
Clodi M, Resl M, Neuhold S et al (2012) A comparison of NT-proBNP and albuminuria for predicting cardiac events in patients with diabetes mellitus. Eur J Prev Cardiol 19:944–951
Cook NR (2008) Statistical evaluation of prognostic versus diagnostic models: beyond the ROC curve. Open Clin Chem J 54:17–23
Resl M, Neuhold M, Riedl M et al (2011) NT-proBNP and cardiac events in older diabetic patients. Eur J Prev Cardiol 18:399–405
Feinkohl I, Sattar N, Welsh P et al (2012) Association of N-terminal pro-brain natriuretic peptide with cognitive function and depression in elderly people with type 2 diabetes. PLoS ONE 7:1–7
Feinkohl I, Keller M, Robertson CM et al (2013) Clinical and subclinical macrovascular disease as predictors of cognitive decline in older patients with type 2 diabetes: the Edinburgh Type 2 Diabetes Study. Diabetes Care 36:2779–2787
Wijsman LW, Sabayan B, van Vliet P et al (2014) N-terminal pro-brain natriuretic peptide and cognitive decline in older adults at high cardiovascular risk. Ann Neurol 76:213–222
Acknowledgements
The authors thank all patients and research staff involved in the ET2DS.
Funding
The sponsor for the ET2DS was the University of Edinburgh. The study was funded by the Medical Research Council (UK), the Chief Scientist Office of the Scottish Executive, Pfizer and Diabetes UK. The funders had no other role in the design, analysis or writing of this manuscript. CJW was supported in this work by NHS Lothian via the Edinburgh Health Services Research Unit.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Contribution statement
JFP and MWJS conceived and designed the ET2DS and oversaw the acquisition and analysis of data. For the current paper, AHP, JFP, NS, PW and CJW conceived the idea and designed the analysis, which was performed by AHP and IF. AHP, JFP, NS, PW and CJW wrote the paper. CMR, JRM and SM collected data and contributed to data analysis and interpretation. All authors contributed to interpretation of findings and preparation of the final manuscript, including commenting on the final draft. JFP and AHP are the guarantors of this work, and as such had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Author information
Authors and Affiliations
Corresponding authors
Additional information
Anna H. Price and Paul Welsh are joint first authors.
Naveed Sattar and Jackie F. Price are joint senior authors.
Rights and permissions
About this article
Cite this article
Price, A.H., Welsh, P., Weir, C.J. et al. N-terminal pro-brain natriuretic peptide and risk of cardiovascular events in older patients with type 2 diabetes: the Edinburgh Type 2 Diabetes Study. Diabetologia 57, 2505–2512 (2014). https://doi.org/10.1007/s00125-014-3375-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-014-3375-9