Abstract
Aims/hypothesis
The transcription factor nuclear factor-kappa-B (NFκB) is implicated in inflammatory responses, obesity and the metabolic syndrome, while immune cells appear to play a central role in mediating insulin resistance and can be used as a model to study inflammation and its relationship with insulin resistance. In peripheral blood mononuclear cells of overweight participants with the metabolic syndrome, we evaluated (1) the effect of diet-induced weight loss on the expression of genes involved in NFκB activation and (2) their association with insulin sensitivity. The genes studied were: TNF receptors TNFRSF1A and TNFRSF1B, and IL1R1, TLR4, TLR2, ICAM1, CCL5 and IKBKB.
Methods
We analysed data from 34 overweight participants with abnormal glucose metabolism and the metabolic syndrome, who were randomised to a weight-reduction (n = 24) or control group (n = 10) for 33 weeks. The mRNA expression was measured using real-time PCR. Measures of insulin and glucose homeostasis were assessed by IVGTT and OGTT.
Results
In general, the genes studied were downregulated after weight loss intervention. The changes in TLR4, TLR2, CCL5 and TNFRSF1A mRNA expression were associated with an increase in insulin sensitivity index independently of the change in waist circumference (p < 0.05). The change in IKBKB expression correlated with most of the changes in gene expression in the weight-reduction group.
Conclusions/interpretation
These results suggest that proteins encoded by CCL5, TLR2 and TLR4, and TNFRSF1A might contribute to insulin-resistant states that characterise obesity and the metabolic syndrome.
Trial registration: ClinicalTrials.gov NCT 00621205
Similar content being viewed by others
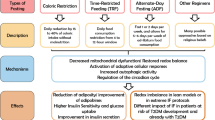
Introduction
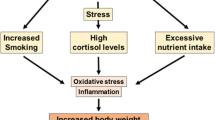
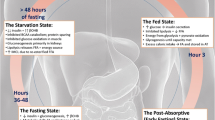
Obesity is characterised by a state of chronic low-grade inflammation [1, 2], which may contribute to the development of insulin resistance [3]. Lifestyle intervention, including weight loss, has been shown to improve insulin and glucose metabolism and to reduce abdominal obesity [4–9]. Moreover, individuals with the metabolic syndrome are at an increased risk of type 2 diabetes mellitus and cardiovascular diseases [10, 11].
We recently found that a long-term weight loss intervention in individuals with the metabolic syndrome altered gene expression of cytokines related to inflammation and the immune response in peripheral blood mononuclear cells (PBMCs). Moreover, the decrease in IL1B mRNA expression was associated with an improvement of insulin and glucose metabolism [9]. These findings and those of others suggest that these cells are a target for insulin action and can be used as a model to study inflammation and its relationship with insulin resistance [12–14]. Moreover, monocytes, which along with lymphocytes, are an important cell type in PBMCs, differentiate into macrophages in most tissues [15], including adipose tissue. PBMCs are also convenient for gene expression studies because they can be easily and repeatedly collected in sufficient quantities in contrast to adipose, muscle and liver tissues and could reflect the disturbance of insulin action.
The transcription factor nuclear factor-kappa-B (NFκB) is implicated in the regulation of inflammatory responses and control of the innate immune system [16, 17]. Recent studies have highlighted the role of NFκB and I-kappaB-kinase β (IKKβ) in the development of insulin resistance and type 2 diabetes mellitus [18, 19]. IKKβ is responsible for the phosphorylation and degradation of the inhibitor-kappaB complex, which enables the activation of NFκB [16]. Pro-inflammatory cytokines like TNF-α and IL1β stimulate NFκB activation through classical receptor-mediated mechanisms. Toll-like receptors (TLRs) are key regulators of immune responses. Thus TLR4, which is part of the bacterial lipopolysaccharide receptor, is an important bridge between innate and adaptive immunity and also triggers NFκB, with consequent production of cytokines such as TNF-α and IL1β [20–22].
Inflammatory processes are characterised by the migration of proliferating white blood cells from the circulation to the tissues [23]. The relevance of these activated immune cells and inflammation in the development of type 2 diabetes mellitus has recently been shown, and they appear to play a central role in mediating insulin resistance [24, 25]. In animal models, lack of IKKβ in immune cells fully protects from insulin resistance [24]. Moreover, there is speculation that nutrients can act through pathogen-sensing systems such as the TLRs, giving rise to metabolically or nutritionally induced inflammatory responses [26, 27].
Against this background, we evaluated: (1) the effect of diet-induced weight loss on the expression of genes associated with the activation of NFκB and encoding of receptors for TNF-α (TNFRSF1A and TNFRSF1B, IL1 (IL1R1) and TLRs 2 and 4 (TLR2 and TLR4); and (2) their association with the improvement of insulin sensitivity that occurred with weight loss. We also sought to evaluate: (1) mRNA expression of genes that are related to immunological and endothelial function, and are positively regulated by NFκB, e.g. CCL5, ICAM1 [20] and the pro-inflammatory mediator IKBKB; and (2) their association with the improvement in insulin sensitivity.
Methods
Participant recruitment and clinical investigation
Altogether 46 overweight or obese (BMI 28–40 kg/m2) participants aged 40 to 70 years with impaired fasting glucose (fasting plasma glucose concentration 5.6–7.0 mmol/l) or impaired glucose tolerance (2 h plasma glucose concentration 7.8–11.0 mmol/l) and at least two other features of the metabolic syndrome according to the Adult Treatment Panel III criteria [28] were randomised to a diet-induced weight-reduction (n = 28) or control group (n = 18) as previously described [7]. Of these, 24 participants randomised to the weight-reduction and ten participants randomised to the control group, all matched for age, sex, BMI and the status of glucose metabolism, were included in the present study as previously described [9]. Briefly, the weight-reduction group underwent a 12 week intensive weight-reduction period during which they followed detailed instructions given by a clinical nutritionist and based on a 4 day dietary record and an interview [29]. During the period between weeks 12 and 33 the minimum aim was to maintain the achieved reduction in weight using the same dietary prescription. Participants in the control group were advised to keep their dietary and lifestyle habits unchanged during the study. The intervention was performed in accordance with the standards of the Helsinki Declaration. The Ethics Committee of the District Hospital Region of Northern Savo and Kuopio University Hospital approved the study plan and all participants gave written informed consent.
Blood samples were drawn and anthropometric measurements (body weight, height, body fat mass and percentage body fat as assessed by bioimpedance [STA/BIA Body Composition Analyzer; Akern Bioresearch, Florence, Italy], and waist circumference) were carried out at baseline (week 0) and at the end of the study (week 33).
Glucose tolerance tests
A 2 h OGTT was performed with 75 g of glucose. Blood samples for plasma glucose and serum insulin were drawn at 0, 30 and 120 min. A frequently sampled IVGTT was performed according to the Minimal Model method as previously described [30]. The insulin sensitivity index (S I) was calculated by the MINMOD Millennium software [31].
Biochemical analyses
Biochemical analyses were performed in the Clinical Laboratory Centre of the Kuopio University Hospital and in the Department of Clinical Nutrition and Institute of Biomedicine of the University of Kuopio. Plasma glucose concentration was analysed by the hexokinase method (concentration range: 4–8 mmol/l; Thermo Clinical Labsystems, Vantaa, Finland). Insulin was determined by the chemiluminescence sandwich method using an automated system (ACS; Bayer, Tarrytown, NY, USA). The intra-assay and interassay CVs were 7.7% and 9.0%, respectively. Serum soluble (s) intercellular cell adhesion molecule-1 (ICAM-1) and chemokine (C-C motif) ligand 5 (CCL5) concentrations were measured by solid phase ELISA (Quantikine; R&D Systems, Minneapolis, MN, USA). The intra-assay and interassay CVs were 6.0 and 4.4%, respectively for sICAM-1 and 5.0 and 5.0%, respectively for CCL5.
Isolation of PBMCs, RNA extraction and real-time PCR analysis of gene expression
Samples were available for 24 participants of the weight-reduction group and ten participants of the control group. PBMCs were isolated from anticoagulated peripheral blood by density centrifugation for 10 min at 900 g and for another 10 min at 300 g using a reagent (Lymphoprep; Axis-Shield, Oslo, Norway) and total RNA was extracted using a kit (RNeasy Mini; Qiagen, Valencia, CA, USA) as previously described [9]. RNA was reverse-transcribed into cDNA using a kit (High-Capacity cDNA Archive; Applied Biosystems, Foster City, CA, USA) and real-time PCR was performed with TaqMan chemistry using ready-made assays from Applied Biosystems. Gene expression was normalised to an endogenous control (GAPDH gene). Measurements were done on samples from baseline (week 0) and end of the study (week 33).
Statistical analysis
Univariate general linear models were used to test changes in circulating sICAM-1 and CCL5 levels and variables of gene expression between weeks 0 and 33 with group as the fixed factor and the baseline measurement as a covariate whenever the baseline measurement had an effect on variable change and was different between groups. Because age influenced some of the changes in mRNA expression of the target genes, these variables were also included in the model. Within-group analyses were performed if either the overall variable change or treatment effect was significant. To test associations between gene expression and SI changes in the weight-reduction group, correlations were performed using partial correlation analyses adjusted for changes in body weight or waist circumference. Multivariate linear regression analyses were carried out to test for independent effects of changes in gene expression on changes in SI. Variables with a skewed distribution were log transformed before the analyses and are presented as medians (interquartile range). A p value of <0.05 was considered to be statistically significant. All analyses were performed using SPSS software version 14.0 for Windows (SPSS, Chicago, IL, USA).
Results
Characteristics of the participants at baseline and after the interventions
As already published [9], there were no differences in age, sex and variables related to body composition, insulin and glucose homeostasis, lipids, circulating inflammatory markers and blood pressure between groups at baseline (Table 1). Improvements in mean body weight (93.0 vs 88.4 kg), BMI (33.0 vs 31.4 kg/m2), waist circumference (108.3 vs 104.6 cm), body fat mass (34.5 vs 31.5 kg), percentage body fat (37.2 vs 35.8%) and S I (2.40 × 10–4 vs 2.62 × 10–4 min−1 [mU/l]−1; to convert values to SI units (min−1 [pmol/l]−1) multiply by 0.167) were observed only in participants from the weight-reduction group after week 33 of the intervention (p < 0.05 for all), but not in the control group (body weight 85.7 vs 85.7 kg, BMI 31.6 vs 31.5 kg/m2, waist circumference 104.1 vs 104.3 cm, body fat mass 31.4 vs 30.9 kg, percentage body fat 36.9 vs 36.4% and S I 2.64 × 10–4 vs 2.43 × 10–4 min−1 [mU/l]−1; p > 0.05 for all). Serum circulating levels of TNF-α, IL6 and high-sensitive C-reactive protein also decreased only in the weight loss group [9].
Changes in gene expression in PBMCs
In the weight-reduction group a decrease in both TNFRSF1A and TNFRSF1B mRNA expression occurred along with a decrease in IL1R1 and TLR4 expression (Fig. 1a). In the control group, by contrast, TNFRSF1A and TLR4 mRNA levels increased (Fig. 1b). The mRNA levels of TNFRSF1B did not change in the control group. However, a decrease in IL1R1 and an increase in TLR2 expression did occur, although for the latter conventional statistical significance was not reached (p = 0.06). In the weight-reduction group, no change in TLR2 mRNA expression was found (p = 0.25). A difference in the level of change between weight loss and control groups was seen only for TLR2 mRNA levels (p = 0.01).
mRNA expression of genes encoding surface ligands for cytokines and TLRs in the weight-reduction (n = 24) (a) and in the control (n = 10) (b) groups. Black bars, week 0; hatched bars, week 33. Data are means ± SEM normalised to GAPDH mRNA expression. *p < 0.05 for the change ([expression at week 33−expression at week 0] × 100/expression at week 0) after univariate analyses
We also looked at whether the weight loss intervention could have modulated other genes involved in NFκB activation. Weight loss significantly decreased mRNA levels of IKBKB, CCL5 and ICAM1 in PBMCs (Fig. 2), whereas in the control group, IKBKB mRNA levels increased and no change in ICAM1 and CCL5 expression was found (Fig. 2).
mRNA expression of genes encoding surface ligands for cytokines and TLRs in the weight-reduction (n = 24) (a) and in the control (n = 10) (b) groups. Black bars, week 0; hatched bars, week 33. Data are median and interquartile range for IKBKB and mean ± SEM for ICAM1 and CCL5 normalised to GAPDH mRNA expression. *p < 0.05 for the change ([expression at week 33−expression at week 0] × 100/expression at week 0) after univariate analyses
Correlations among gene expression changes and with changes in insulin sensitivity after weight loss
We observed that the decrease in TNFRSF1A expression correlated with the increase in SI when adjusted for change in body weight (r = −0.57, p = 0.007) or waist circumference (r = −0.58, p = 0.008). Moreover, the change in TLR2 also correlated with the change in SI (r = −0.48, p = 0.03). Adjustments for changes in body weight (r = −0.58, p = 0.008) or waist circumference (r = −0.66, p = 0.002) did not alter these associations. Furthermore, the decrease in TLR4 and in CCL5 mRNA expression correlated with increase in SI after weight loss when adjusted for changes in body weight or waist circumference (TLR4 r = −0.48, p = 0.03, r = −0.50, p = 0.02, respectively; CCL5 r = −0.50, p = 0.02, r = −0.43, p = 0.04, respectively). Adjustment for changes in body fat mass or percentage body fat instead of changes in body weight or waist circumference did not alter any of these correlations.
To control for the possible effect of changes in body weight and waist circumference on SI, multivariate linear regression analyses were carried out for each of these genes to test for independent effects of the fold changes in gene expression and the absolute change in body weight or waist circumference (independent variables) on changes in S I (dependent variable). In these models, the change in waist girth and the change in mRNA expression of TLR4, CCL5 or TNFRSF1A predicted the absolute change in S I in the weight-reduction group (Table 2). The same was true for the effect of the change in TLR2 mRNA expression on the change in S I (Table 2). Replacing the change in waist circumference in the models with the change in either body fat mass or percentage body fat generated similar results.
The correlations among the mRNA expression changes of the target genes studied are depicted in Table 3. Except for ICAM1, the changes in mRNA expression of the genes was in general significantly correlated among each other. In particular, the changes in CCL5 and TLR4 were highly correlated with each other and with all changes in the expression of the other target genes. We also tested correlations between a previously noted change in IL1B mRNA expression [9] and the changes in mRNA expression observed in the present study (Table 3).
Changes in concentrations of circulating sICAM-1 and CCL5
Circulating levels of CCL5 and sICAM-1 were measured before and after the intervention. Circulating levels of sICAM-1 did not change in either the weight-reduction or the control group from baseline to week 33 (weight-reduction 179 ± 41 vs 177 ± 37 pg/ml, control 202 ± 56 vs 212 ± 51 pg/ml; p = 0.09 and p = 0.10, respectively). The change between groups, however, was of borderline significance (p = 0.06). In the control group, serum levels of CCL5 were not different between week 0 and week 33 (77.61 ± 20.92 vs 84.24 ± 19.88 ng/ml, p = 0.12); however, in the weight-reduction group, they increased significantly after the intervention (82.25 ± 27.45 vs 85.47 ± 23.91 ng/ml, p = 0.01). The change in this serum marker was not different between groups (p = 0.65).
Discussion
In the present study we show that a 9 month period of sustained diet-induced weight loss and improvement of insulin sensitivity resulted in a decrease of mRNA expression of genes encoding surface cell receptors involved in the activation of NFκB and the immune-inflammatory response as measured in PBMCs of overweight glucose-intolerant individuals with the metabolic syndrome. We found that the downregulation of some of these genes such as TLR4, TNFRSF1A and CCL5 were independently associated with an improvement of S I. To the best of our knowledge these findings have not been described before.
NFκB is considered to be a primary regulator of inflammatory responses [16]. It can be activated by a variety of stimuli, including TNF-α, IL-1, T cell activation signals, growth factors and stress inducers [32]. The binding of these ligands to specific receptors such as TNF, IL1 and TLRs induces a proinflammatory response leading to new expression of the genes encoding these ligands. This activation also controls the gene expression of molecules involved in the production of secondary inflammatory mediators such as CCL5 and ICAM1. In the present study, the decrease in mRNA expression of CCL5 and ICAM1, IL1R1, TNFRSF1A and TNFRSF1B, and TLR4 after weight loss, and in particular of those genes encoding the surface cell receptors, could be interpreted as a lower state of activation of proinflammatory NFκB, although it was not our aim to measure NFκB activity itself. The fact that the decrease in IKBKB expression was generally highly associated with these markers supports our supposition. Indeed, in humans, obesity is associated with increased NFκB binding activity and IKBKB expression in circulating mononuclear cells [12, 13].
Macrophage infiltration in adipose tissue has been linked to obesity-related inflammation and insulin resistance [33, 34], and upregulation of CCL5 in visceral fat of obese individuals with the metabolic syndrome has recently been associated with markers of T cells and macrophages in this tissue [35]. Although we cannot directly conclude this, the correlation between the decrease in CCL5 expression and that in IKBKB and ICAM1 expression suggests that, besides NFκB activation, an interplay occurs between markers of endothelial function in immune cells on the one hand, and insulin and glucose metabolism after weight loss on the other. Conversely, circulating levels of sICAM-1 and CCL5 did not go in the same direction as gene expression in the present study, although these findings should be interpreted cautiously due to the relatively high CVs of the assays. Also, these discrepancies could be explained by the fact that CCL5 and ICAM-1 are produced by several other tissues in addition to PBMCs. On the other hand, increased mRNA expression may not necessarily be translated to protein and there may be other conditions that affect mRNA stability and mRNA translation. However, the decrease in expression of ICAM1 and CCL5 in PBMCs could play a role in avoiding the detrimental effect of the production of these molecules directly at sites of inflammation.
Interestingly, we found that after diet-induced weight loss the decrease in mRNA expression of TLR4 and TLR2, and CCL5 and TNFRSF1A was associated with an increase in insulin sensitivity. Glucose and insulin metabolism has been implicated in NFκB activation [36–39]. No correlation was found between IKBKB mRNA expression and SI changes, but the downregulation of genes associated with SI improvement was in general highly correlated with the change in IKBKB. Our data also suggest that TLR4 might also have an independent effect on the improvement in SI that was induced by weight loss.
Increasing adiposity also activates IKKβ, possibly through cytokines or even TLRs [20]. TLR4 has recently been suggested to be involved in the adverse effects of NEFA on tissues and processes that constitute the metabolic syndrome. Also NEFA seem to induce proinflammatory cytokine expression via TLR4, which appears to be required for induction of insulin resistance by NEFA [27]. Our results show that the association between the changes in TLR4, TLR2, TNFRSF1A and CCL5 mRNA expression and the improvement of S I was nonetheless independent of the diet-induced changes in waist circumference or body weight. We were unable to demonstrate a significant change in fasting serum NEFA levels after weight loss (data not shown). Nevertheless, the decrease in waist circumference and its independent effect on S I indicate a role for this abdominal fat mobilisation or oxidation, even if not reflected by serum NEFA levels [40].
Dietary components and exercise can also play a role in S I and possibly in TLR4 and CCL5 [6, 8, 41–47]. This study is too small to reliably assess the independent effect of physical activity and diet, but adjustment for changes in physical activity frequency, serum NEFA and energy-adjusted intake of total fat, saturated fat, monounsaturated fat, polyunsaturated fat or total fibre did not attenuate the independent effect of changes in waist circumference and TLR4, TLR2, TNFRSF1A or CCL5 on changes in S I (data not shown).
In obesity, the effect of weight loss on lowering circulating concentrations of TNF-α and its expression in sites of production [9, 48, 49] could have an impact on the decrease in TNF receptor mRNA expression, with consequences on the activation of NFκB [35, 50]. Moreover, the associations between both the downregulation of IL1B [9] and the changes in TLR4, TLR2, TNFRSF1A or CCL5 mRNA expression in PBMCs and the improvement of S I after weight loss in the present study supports this hypothesis. Immune cells are not only exposed to adipose, liver and other tissues, but also cross-talk with these tissues [26]. Consequently, gene expression in PBMCs might reflect metabolic and immune responses of adipocytes or hepatocytes, and probably also their communication with other sites such as pancreatic islets and skeletal muscle.
The major limitation of this study was the small sample size. However, the methods employed and the design of the study were complex, time-consuming and expensive, and therefore difficult to apply to a much larger group of participants. Since the control group was much smaller than the weight-reduction group, we cannot rule out the possibility that the lack of statistically significant changes might have been due to inadequate sample size. In the future, larger studies with more statistical power are needed. However, even with a small number of participants it was possible to observe significant changes and associations that are supported by the previous literature and biologically plausible. Because we could not measure markers related to oxidative stress and intracellular redox status, we cannot exclude the possibility of redox modulation of NFκB activation and other inflammatory processes in the improvement of S I [14]. Moreover, the variation among individuals in the magnitude of weight loss may have obscured some of the effects of long-term weight loss on changes in expression of the markers studied.
Our results clearly showed an association between the improvement of insulin sensitivity that occurred with weight loss and attenuation of the expression of genes encoding receptors of surface ligands (TLR4, TLR2, TNFRSF1A) and immune mediators (CCL5) that are involved in NFκB inflammatory signalling pathways in the PBMCs of men and women with disturbed glucose metabolism and the metabolic syndrome. Our findings may also be relevant with respect to migration of PBMCs to sites of inflammation such as adipose tissue, liver or endothelium. The mechanisms by which diet-induced weight loss modulated the changes in gene expression and the associations with changes in insulin sensitivity require further clarification.
Abbreviations
- CCL5:
-
chemokine (C-C motif) ligand
- ICAM-1:
-
intercellular cell adhesion molecule-1
- IKKβ:
-
I-kappaB-kinase β
- NFκB:
-
nuclear factor-kappa-B
- PBMCs:
-
peripheral blood mononuclear cells
- s:
-
serum-soluble
- SI :
-
insulin sensitivity index
- TLRs:
-
toll-like receptors
References
Engström G, Hedblad B, Stavenow L, Lind P, Janzon L, Lindgärde F (2003) Inflammation-sensitive plasma proteins are associated with future weight gain. Diabetes 52:2097–2101
Festa A, D'Agostino R Jr, Williams K et al (2001) The relation of body fat mass and distribution to markers of chronic inflammation. Int J Obes Relat Metab Disord 25:1407–1415
Wellen KE, Hotamisligil GS (2005) Inflammation, stress, and diabetes. J Clin Invest 115:1111–1119
Tuomilehto J, Lindström J, Eriksson JG et al (2001) Prevention of type 2 diabetes mellitus by changes in lifestyle among subjects with impaired glucose tolerance. N Engl J Med 344:1343–1350
Lindström J, Louheranta A, Mannelin M et al (2003) The Finnish Diabetes Prevention Study (DPS): Lifestyle intervention and 3-year results on diet and physical activity. Diabetes Care 26:3230–3236
Uusitupa M, Lindi V, Louheranta A, Salopuro T, Lindström J, Tuomilehto J (2003) Long-term improvement in insulin sensitivity by changing lifestyles of people with impaired glucose tolerance: 4-year results from the Finnish Diabetes Prevention Study. Diabetes 52:2532–2538
Kolehmainen M, Salopuro T, Schwab US et al (2008) Weight reduction modulates expression of genes involved in extracellular matrix and cell death: the GENOBIN study. Int J Obes (Lond) 32:292–303
Xiao C, Giacca A, Carpentier A, Lewis GF (2006) Differential effects of monounsaturated, polyunsaturated and saturated fat ingestion on glucose-stimulated insulin secretion, sensitivity and clearance in overweight and obese, non-diabetic humans. Diabetologia 49:1371–1379
de Mello VD, Kolehmainen M, Schwab U et al (2008) Effect of weight loss on cytokine messenger RNA expression in peripheral blood mononuclear cells of obese subjects with the metabolic syndrome. Metabolism 57:192–199
Laaksonen DE, Lakka HM, Niskanen LK, Kaplan GA, Salonen JT, Lakka TA (2002) Metabolic syndrome and development of diabetes mellitus: application and validation of recently suggested definitions of the metabolic syndrome in a prospective cohort study. Am J Epidemiol 156:1070–1077
Lakka HM, Laaksonen DE, Lakka TA et al (2002) The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA 288:2709–2716
Ghanim H, Aljada A, Hofmeyer D, Syed T, Mohanty P, Dandona P (2004) Circulating mononuclear cells in the obese are in a proinflammatory state. Circulation 110:1564–1571
Ghanim H, Aljada A, Daoud N, Deopurkar R, Chaudhuri A, Dandona P (2007) Role of inflammatory mediators in the suppression of insulin receptor phosphorylation in circulating mononuclear cells of obese subjects. Diabetologia 50:278–285
Dandona P, Aljada A, Mohanty P et al (2001) Insulin inhibits intranuclear nuclear factor kappaB and stimulates IkappaB in mononuclear cells in obese subjects: evidence for an anti-inflammatory effect? J Clin Endocrinol Metab 86:3257–3265
Ziegler-Heitbrock HW (2000) Definition of human blood monocytes. J Leukoc Biol 67:603–606
Barnes PJ, Karin M (1997) Nuclear factor-kappaB: a pivotal transcription factor in chronic inflammatory diseases. N Engl J Med 336:1066–1071
Li Q, Verma IM (2002) NF-kappaB regulation in the immune system. Nat Rev Immunol 2:725–734
Kim JK, Kim YJ, Fillmore JJ et al (2001) Prevention of fat-induced insulin resistance by salicylate. J Clin Invest 108:437–446
Yuan M, Konstantopoulos N, Lee J et al (2001) Reversal of obesity- and diet-induced insulin resistance with salicylates or targeted disruption of Ikkbeta. Science 293:1673–1677
Shoelson SE, Lee J, Goldfine AB (2006) Inflammation and insulin resistance. J Clin Invest 116:1793–1801
Doyle SL, O'Neill LA (2006) Toll-like receptors: from the discovery of NFkappaB to new insights into transcriptional regulations in innate immunity. Biochem Pharmacol 72:1102–1113
Vitseva OI, Tanriverdi K, Tchkonia TT et al (2008) Inducible toll-like receptor and NF-kappaB regulatory pathway expression in human adipose tissue. Obesity (Silver Spring) 16:932–937
Muller WA (2002) Leukocyte-endothelial cell interactions in the inflammatory response. Lab Invest 82:521–533
Arkan MC, Hevener AL, Greten FR et al (2005) IKK-beta links inflammation to obesity-induced insulin resistance. Nat Med 11:191–198
Cai D, Yuan M, Frantz DF et al (2005) Local and systemic insulin resistance resulting from hepatic activation of IKK-beta and NF-kappaB. Nat Med 11:183–190
Hotamisligil GS (2006) Inflammation and metabolic disorders. Nature 444:860–867
Shi H, Kokoeva MV, Inouye K, Tzameli I, Yin H, Flier JS (2006) TLR4 links innate immunity and fatty acid-induced insulin resistance. J Clin Invest 116:3015–3025
No authors listed (2001) Executive summary of the third report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III). JAMA 285:2486–2497
Krauss RM, Eckel RH, Howard B et al (2000) AHA Dietary Guidelines: revision 2000: A statement for healthcare professionals from the Nutrition Committee of the American Heart Association. Circulation 102:2284–2299
Sarkkinen E, Schwab U, Niskanen L et al (1996) The effects of monounsaturated-fat enriched diet and polyunsaturated-fat enriched diet on lipid and glucose metabolism in subjects with impaired glucose tolerance. Eur J Clin Nutr 50:592–598
Boston RC, Stefanovski D, Moate PJ, Sumner AE, Watanabe RM, Bergman RN (2003) MINMOD Millennium: a computer program to calculate glucose effectiveness and insulin sensitivity from the frequently sampled intravenous glucose tolerance test. Diabetes Technol Ther 5:1003–1015
Baldwin AS Jr (2001) Series introduction: the transcription factor NF-kappaB and human disease. J Clin Invest 107:3–6
Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW Jr (2003) Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest 112:1796–1808
Xu H, Barnes GT, Yang Q et al (2003) Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest 112:1821–1830
Wu H, Ghosh S, Perrard XD et al (2007) T cell accumulation and regulated on activation, normal T cell expressed and secreted upregulation in adipose tissue in obesity. Circulation 115:1029–1038
Kempf K, Rose B, Herder C et al (2007) The metabolic syndrome sensitizes leukocytes for glucose-induced immune gene expression. J Mol Med 85:389–396
González F, Rote NS, Minium J, Kirwan JP (2006) Increased activation of nuclear factor kappaB triggers inflammation and insulin resistance in polycystic ovary syndrome. J Clin Endocrinol Metab 91:1508–1512
Dhindsa S, Tripathy D, Mohanty P et al (2004) Differential effects of glucose and alcohol on reactive oxygen species generation and intranuclear nuclear factor-kB in mononuclear cells. Metabolism 53:330–334
Aljada A, Friedman J, Ghanim H et al (2006) Glucose ingestion induces an increase in intranuclear nuclear factor kB, a fall in cellular inhibitor kB, and an increase in tumor necrosis factor a messenger RNA by mononuclear cells in healthy human subjects. Metabolism 55:1177–1185
Votruba SB, Jensen MD (2007) Regional fat deposition as a factor in FFA metabolism. Annu Rev Nutr 27:149–163
Vessby B, Uusitupa M, Hermansen K et al (2001) Substituting dietary saturated for monounsaturated fat impairs insulin sensitivity in healthy men and women: The KANWU Study. Diabetologia 44:312–319
Ylonen K, Saloranta C, Kronberg-Kippila C, Groop L, Aro A, Virtanen SM (2003) Associations of dietary fiber with glucose metabolism in nondiabetic relatives of subjects with type 2 diabetes: the Botnia Dietary Study. Diabetes Care 26:1979–1985
Galisteo M, Duarte J, Zarzuelo A (2008) Effects of dietary fibers on disturbances clustered in the metabolic syndrome. J Nutr Biochem 19:71–84
Lee JY, Sohn KH, Rhee SH, Hwang D (2001) Saturated fatty acids, but not unsaturated fatty acids, induce the expression of cyclooxygenase-2 mediated through Toll-like receptor 4. J Biol Chem 276:16683–16689
Weatherill AR, Lee JY, Zhao L, Lemay DG, Youn HS, Hwang DH (2005) Saturated and polyunsaturated fatty acids reciprocally modulate dendritic cell functions mediated through TLR4. J Immunol 174:5390–5397
Gleeson M, McFarlin B, Flynn M (2006) Exercise and toll-like receptors. Exerc Immunol Rev 12:34–53
Connolly PH, Caiozzo VJ, Zaldivar F et al (2004) Effects of exercise on gene expression in human peripheral blood mononuclear cells. J Appl Physiol 97:1461–1469
Bruun JM, Verdich C, Toubro S, Astrup A, Richelsen B (2003) Association between measures of insulin sensitivity and circulating levels of interleukin-8, interleukin-6 and tumor necrosis factor-alpha. Effect of weight loss in obese men. Eur J Endocrinol 148:535–542
Dandona P, Weinstock R, Thusu K, Abdel-Rahman E, Aljada A, Wadden T (1998) Tumor necrosis factor-alpha in sera of obese patients: fall with weight loss. J Clin Endocrinol Metab 83:2907–2910
Zhi L, Leung BP, Melendez AJ (2006) Sphingosine kinase 1 regulates pro-inflammatory responses triggered by TNFalpha in primary human monocytes. J Cell Physiol 208:109–115
Acknowledgements
This work was supported financially by grants from Sigrid Juselius Foundation, the Academy of Finland (number 209445; number 211497), the State subsidy funding system (EVO) (numbers 5179, 5198), the Ministry of Education in Finland (number 125/722/2003), the Yrjö Johansson Foundation, the Finnish Foundation for Diabetes Research and the City of Kuopio. V. D. F. de Mello was a recipient of a scholarship from the Conselho Nacional de Desenvolvimento Científico e Tecnológico (National Council of Scientific and Technological Development), Brazil. U. Mager received a scholarship from the Austrian Academy of Sciences.
Duality of interest
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
de Mello, V.D.F., Kolehmainen, M., Pulkkinen, L. et al. Downregulation of genes involved in NFκB activation in peripheral blood mononuclear cells after weight loss is associated with the improvement of insulin sensitivity in individuals with the metabolic syndrome: the GENOBIN study. Diabetologia 51, 2060–2067 (2008). https://doi.org/10.1007/s00125-008-1132-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-008-1132-7