Abstract
Aims/hypothesis
Genome-wide association studies have recently identified novel type 2 diabetes susceptibility gene regions. We assessed the effects of six of these regions on insulin secretion as determined by a hyperglycaemic clamp.
Methods
Variants of the HHEX/IDE, CDKAL1, SLC30A8, IGF2BP2 and CDKN2A/CDKN2B genes were genotyped in a cohort of 146 participants with NGT and 126 with IGT from the Netherlands and Germany, who all underwent a hyperglycaemic clamp at 10 mmol/l glucose.
Results
Variants of CDKAL1 and IGF2BP2 were associated with reductions in first-phase insulin secretion (34% and 28%, respectively). The disposition index was also significantly reduced. For gene regions near HHEX/IDE, SLC30A8 and CDKN2A/CDKN2B we did not find significant associations with first-phase insulin secretion (7–18% difference between genotypes; all p > 0.3). None of the variants showed a significant effect on second-phase insulin secretion in our cohorts (2–8% difference between genotypes, all p > 0.3). Furthermore, the gene variants were not associated with the insulin sensitivity index.
Conclusions
Variants of CDKAL1 and IGF2BP2 attenuate the first phase of glucose-stimulated insulin secretion but show no effect on the second phase of insulin secretion. Our results, based on hyperglycaemic clamps, provide further insight into the pathogenic mechanism behind the association of these gene variants with type 2 diabetes.
Similar content being viewed by others
Introduction
The field of the genetics of type 2 diabetes mellitus is rapidly changing as a result of the discovery of a number of novel susceptibility loci in recent genome-wide association studies [1]. Until recently, only three confirmed genetic susceptibility loci were known that increase the risk of developing type 2 diabetes, i.e. TCF7L2, PPARG and KCNJ11. These loci are now extended with at least CDKAL1, IGF2BP2, HHEX/IDE, SLC30A8, CDKN2A/CDKN2B and FTO [1]. Of these novel genes, FTO plays a role in childhood and adult obesity and the other five regions may play a role in pancreatic beta cell development and/or insulin secretion. Recent clinical results involving glucose tolerance tests indeed show that these variants affect insulin secretion, at least within the limitations of the tests used [2–7].
We studied the effects of the strongest associated single-nucleotide polymorphisms (SNPs) in the reported gene regions on insulin secretion, as determined with a hyperglycaemic clamp. This technique is generally considered the gold standard method of quantifying glucose-induced insulin secretion. In contrast to the OGTT, the hyperglycaemic clamp allows direct quantification of the first and second phases of glucose-induced insulin secretion and of insulin-mediated glucose disposal under conditions of stable hyperglycaemia (10 mmol/l glucose). An advantage over the IVGTT is that the glucose peak reached in hyperglycaemic clamps does not differ between participants: this allows better determination of second-phase insulin secretion.
Using the hyperglycaemic clamp technique, we report the effect of novel type 2 diabetes mellitus gene variants on the first and second phases of glucose-stimulated insulin secretion during stable hyperglycaemia.
Materials and methods
Participants
Three independent studies from the Netherlands and Germany were used. The clinical characteristics of the study groups are given in Table 1. Details of these study groups and the clamp procedure have previously been described by ’t Hart et al. [8]. All participants underwent a hyperglycaemic clamp at 10 mmol/l glucose. First-phase insulin secretion was determined as the sum of insulin levels during the first 10 min of the clamp. Second-phase insulin secretion was determined as the mean of the insulin levels during the last 40 min of the clamp (80–120 min). The insulin sensitivity index (ISI) was calculated by relating the glucose infusion rate to the plasma insulin concentration during the last 40 min of the clamp. The disposition index (DI) was calculated by multiplying first-phase insulin secretion by the ISI. It is important to quantify insulin secretion in relation to insulin sensitivity to accurately assess beta cell function. However, as our methods of quantifying DI and ISI are not the gold standard methods, our measures may be biased and could either over- or understate the evidence for association.
Genotyping
We tested the SNPs rs7754840 (CDKAL1), rs4402960 (IGF2BP2), rs1111875 (HHEX/IDE), rs13266634 (SLC30A8), rs10811661 and rs564398 (CDKN2A/CDKN2B) in a Taqman allelic discrimination assay (Applied Biosystems, Foster City, CA, USA) according to the manufacturers’ instructions. The genotyping success rate was >98% and duplicate samples revealed no errors.
Statistics
All data are given as mean±SEM, median (interquartile range) or estimated mean (95% CI). We pooled data on all participants and tested the SNPs for association with first- and second-phase insulin secretion, ISI and DI. Variables that were not normally distributed were log-transformed before analysis. Associations were examined with an additive linear regression model (unadjusted and adjusted for age, sex, study centre, glucose tolerance status and BMI), this because genome-wide association studies have shown that the associations of these variants with type 2 diabetes mellitus are additive, the only exception being CDKAL1, for which other models also fit the data. The direction of the effects of the gene variants on the variables we tested were not significantly different between groups (NGT, IGT, study centres; all interaction terms p > 0.05; see Electronic supplementary material [ESM] Tables 1–12). A priori power calculations showed that the design used in this study would allow the detection of a difference of between 20 and 30% in first- and second-phase insulin secretion with 80% power (α < 0.05) depending on allele frequency. Results were regarded as significant at p < 0.05. Based on the previously published effects of these variants on type 2 diabetes susceptibility and insulin secretion and the consistency of the effects observed in the individual cohorts, we did not correct for multiple hypothesis testing. For all statistical analyses we used SPSS version 14.0 software (SPSS, Chicago, IL, USA).
Results
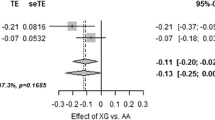
We studied the effects of the variants on insulin secretion with a hyperglycaemic clamp in participants with normal (n = 146) or impaired (n = 126) glucose tolerance from the Netherlands and Germany. Correction for possible confounders such as age, sex, BMI, study centre and glucose tolerance status did not affect our results essentially (Table 2). The results showed significantly reduced first-phase insulin secretion in the CDKAL1 and IGF2BP2 variants (p adj = 0.01 and p adj = 0.05, respectively; Table 2). The DI was also significantly reduced (p adj = 0.01 and p adj = 0.02, respectively). These variants showed however no significant effect on second-phase insulin secretion (Table 2). Analysis of CDKAL1 with a recessive model showed a better fit to our data (p rec = 0.002) and showed a 34% reduction in first-phase insulin secretion in homozygous carriers of the risk alleles compared with the other genotypes (Table 2, ESM Fig. 1). For IGF2BP2 the reduction in first-phase insulin secretion was 9% and 28% for heterozygous and homozygous carriers of the risk alleles respectively (Table 2, ESM Fig. 1). For the HHEX/IDE, SLC30A8 and CDKN2A/CDKN2B variants we did not find significant differences in insulin secretion between the different genotypes (Table 2, ESM Fig. 1). None of the SNPs was associated with ISI in our cohorts.
Discussion
We examined the effects of novel type 2 diabetes genetic variants on glucose-induced insulin secretion assessed with a hyperglycaemic clamp. We observed that the variants in CDKAL1 and IGF2BP2 were associated with reduced first-phase insulin secretion. Remarkably, second-phase insulin secretion remained intact.
Previously, several studies have investigated the effects of novel susceptibility loci on insulin secretion as assessed by the OGTT [2–4, 6, 7] or IVGTT [2, 4–6]. These studies reported that these gene variants were associated with reduced insulin secretion but not with insulin sensitivity. However, variable results have been published for some of the genes, e.g. IGF2BP2, HHEX/IDE, SLC30A8 and CDKN2A/CDKN2B. Our data, using the gold standard for measuring insulin secretion, show that variants of CDKAL1 and IGF2BP2 affect first-phase insulin secretion and DI, but not second-phase insulin secretion. A reduced DI reflects the failing adaptive capacity of pancreatic beta cells to a reduction in insulin sensitivity.
The results for IGF2BP2 agree with the results found by Grarup et al., in which there was also a reduced acute insulin response and decreased DI for homozygous carriers of the risk allele during an IVGTT [2]. However, they did not determine the effect of the variant in IGF2BP2 on the second phase of insulin secretion. Recently, Stancakova et al. reported for the CDKAL1 variant decreased first-phase insulin secretion but not second-phase insulin secretion during an IVGTT, which agrees with our results [6].
We did not detect significant effects of variants of HHEX/IDE, SLC30A8 and CDKN2A/CDKN2B on insulin secretion. One of the limitations of our study was the relatively small sample size and power to detect small differences in insulin secretion. The non-significant differences in first- and second-phase insulin secretion we observed ranged from 7 to 18% and 2 to 8%, respectively (Table 2, ESM Fig. 1). Based on these data, it seems that there is no (major) effect of these variants on second-phase insulin secretion. However, with an a priori power to detect only differences greater than 20%, larger studies or more sophisticated methods (such as the stepped hyperglycaemic clamp and deconvolution analyses) would be needed to investigate in detail the impact of these variants, especially on first-phase insulin secretion. In accordance with previous studies we did not observe effects of the variants on ISI.
Previously, we have shown that other confirmed type 2 diabetes mellitus susceptibility genes, such as TCF7L2 and KCNJ11, also do not affect glucose-stimulated insulin secretion during hyperglycaemic clamps [9, 10]. However, the German participants underwent a modified hyperglycaemic clamp using additional secretagogues, such as glucagon-like peptide-1 (GLP-1) and arginine [9]. Furthermore, glucagon levels were measured during the clamp. Using this modified hyperglycaemic clamp, we have shown previously that TCF7L2 and KCNJ11 are associated with impaired GLP-1-induced insulin secretion and reduced glucagon suppression, respectively [9, 10]. We thus hypothesised that similar defects could also be present in carriers of the novel gene variants. However, analyses of the six novel gene variants showed no impairment in either of these responses (data not shown).
In conclusion, we show that variants of the CDKAL1 and IGF2BP2 genes, which are known to be associated with type 2 diabetes mellitus, are associated with reduced first-phase insulin secretion and reduced DI. No major effect of these two variants or the other gene variants on second-phase insulin secretion or ISI was observed. The biological mechanism by which variants in CDKAL1 and IGF2BP2 could mediate their effects on the biphasic pattern of insulin secretion needs further investigation.
Abbreviations
- DI:
-
disposition index
- ISI:
-
insulin sensitivity index
- SNP:
-
single-nucleotide polymorphism
References
Zeggini E (2007) A new era for type 2 diabetes genetics. Diabet Med 24:1181–1186
Grarup N, Rose CS, Andersson EA et al (2007) Studies of association of variants near the HHEX, CDKN2A/B, and IGF2BP2 genes with type 2 diabetes and impaired insulin release in 10,705 Danish subjects: validation and extension of genome-wide association studies. Diabetes 56:3105–3111
Pascoe L, Tura A, Patel SK et al (2007) Common variants of the novel type 2 diabetes genes CDKAL1 and HHEX/IDE are associated with decreased pancreatic beta-cell function. Diabetes 56:3101–3104
Staiger H, Machicao F, Stefan N et al (2007) Polymorphisms within novel risk loci for type 2 diabetes determine beta-cell function. PLoS.ONE 2:e832
Staiger H, Stancakova A, Zilinskaite J et al (2008) A candidate type 2 diabetes polymorphism near the HHEX locus affects acute glucose-stimulated insulin release in European populations: results from the EUGENE2 study. Diabetes 57:514–517
Stancakova A, Pihlajamaki J, Kuusisto J et al (2008) SNP rs7754840 of CDKAL1 is associated with impaired insulin secretion in non-diabetic offspring of type 2 diabetic subjects (the EUGENE2 study) and in a large sample of men with normal glucose tolerance. J Clin Endocrinol Metab 94:1924–1930
Steinthorsdottir V, Thorleifsson G, Reynisdottir I et al (2007) A variant in CDKAL1 influences insulin response and risk of type 2 diabetes. Nat Genet 39:770–775
’t Hart LM, Fritsche A, Rietveld I et al (2004) Genetic factors and insulin secretion: gene variants in the IGF genes. Diabetes 53(Suppl 1):S26–S30
Schäfer SA, Tschritter O, Machicao F et al (2007) Impaired glucagon-like peptide-1-induced insulin secretion in carriers of transcription factor 7-like 2 (TCF7L2) gene polymorphisms. Diabetologia 50:2443–2450
Tschritter O, Stumvoll M, Machicao F et al (2002) The prevalent Glu23Lys polymorphism in the potassium inward rectifier 6.2 (KIR6.2) gene is associated with impaired glucagon suppression in response to hyperglycemia. Diabetes 51:2854–2860
Acknowledgements
The authors would like to thank the participants for their kind cooperation. The Dutch work in this study was supported by the Dutch Diabetes Research Foundation (Amersfoort, the Netherlands), the Netherlands Organisation for Health Research and Development, Research Institute for Diseases in the Elderly (RIDE program). The German work was supported by a grant from the Deutsche Forschungsgemeinschaft (KFO 114).
Duality of interest statement
The authors declare that there is no duality of interest associated with this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
L. M. ’t Hart and T. W. van Haeften contributed equally to this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM Table 1
(PDF 79.2 kb)
ESM Table 2
(PDF 79.0 kb)
ESM Table 3
(PDF 76.2 kb)
ESM Table 4
(PDF 77.0 kb)
ESM Table 5
(PDF 77.2 kb)
ESM Table 6
(PDF 76.2 kb)
ESM Table 7
(PDF 76.3 kb)
ESM Table 8
(PDF 77.1 kb)
ESM Table 9
(PDF 77.1 kb)
ESM Table 10
(PDF 76.8 kb)
ESM Table 11
(PDF 77.0 kb)
ESM Table 12
(PDF 77.1 kb)
ESM Fig. 1
Effect of susceptibility variants on (a) first-phase and (b) second-phase insulin secretion during hyperglycaemic clamps. Data are mean±SEM corrected for age, sex, BMI, study centre and glucose tolerance status using an additive model. Black bars, homozygous carriers of the wild-type allele; white bars, heterozygotes; dotted bars, homozygous carriers of the risk alleles. * p < 0.05, ** p < 0.01 (PDF 71.7 KB)
Rights and permissions
About this article
Cite this article
Groenewoud, M.J., Dekker, J.M., Fritsche, A. et al. Variants of CDKAL1 and IGF2BP2 affect first-phase insulin secretion during hyperglycaemic clamps. Diabetologia 51, 1659–1663 (2008). https://doi.org/10.1007/s00125-008-1083-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00125-008-1083-z