Abstract
Purpose
The optimal duration of immobilization for the conservative treatment of non- or minimally displaced and displaced distal radius fractures remains under debate. This research aims to review studies of these treatments to add evidence regarding the optimal immobilization period.
Methods
A comprehensive database search was conducted. Studies investigating and comparing short (< 3 weeks) versus long (> 3 weeks) immobilizations for the conservative treatment of distal radius fractures were included. The studies were evaluated for radiological and functional outcomes, including pain, grip strength, and range of motion. Two reviewers independently reviewed all studies and performed the data extraction.
Results
The initial database search identified 11.981 studies, of which 16 (involving 1.118 patients) were ultimately included. Patient-reported outcome measurements, grip strength, range of motion, and radiological outcomes were often better after shorter immobilization treatments. Radiological outcomes were better with longer immobilization in two studies and shorter immobilization in one study. Fourteen studies concluded that early mobilization is preferred, while the remaining two studies observed better outcomes with longer immobilization. The data were unsuitable for meta-analysis due to their heterogeneous nature.
Conclusion
Shorter immobilization for conservatively treated distal radius fractures often yield equal or better outcomes than longer immobilizations. The immobilization for non- or minimally displaced distal radius fractures could therefore be shortened to 3 weeks or less. Displaced and reduced distal radius fractures cannot be immobilized shorter than 4 weeks due to the risk of complications. Future research with homogeneous groups could elucidate the optimal duration of immobilization.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Distal radius fractures (DRFs) are one of the most common fractures, and are often observed in young active patients and in patients aged 50 years and older. The overall incidence of DRFs is increasing due to the growing and aging population worldwide. Approximately 50% DRFs are treated conservatively [1,2,3]. However, there is no consensus about the optimal duration of immobilization for the conservative treatment of patients with DRFs.
In recent years, the operative treatment of patients with DRFs, including new minimally invasive surgical techniques, has been investigated [4]. Operative techniques to fixate a DRF include plating, minimally invasive percutaneous plate osteosynthesis, external fixation, and percutaneous pin fixation. There are several guidelines for the treatment and indications for the operative treatment of patients with DRFs [5, 6]. The American Academy of Orthopaedic Surgeons (AAOS) acknowledges that operative treatment leads to improved patient-reported and radiographic outcomes in patients with DRFs aged 65 years and younger, while in older patients, no difference was observed in patient-reported outcome measurements (PROMs) after 1 year whether they were treated operatively or conservatively. No recommendations or guidelines for the conservative treatment of patients with DRFs are provided by the AAOS, indicating the need for a unified treatment protocol [6].
To date, several systematic reviews have investigated the duration of immobilization for the conservative treatment of patients with DRFs. Although recommendations for the duration of immobilization are given, this did not result in a unified protocol. The review of the literature by van Delft et al. [7] included data from 12 articles and offers probably the most comprehensive analysis. These authors concluded that an immobilization period of 3 weeks or less is equally effective compared to longer immobilization, and might be associated with a better functional outcome [7]. Following the research by van Delft et al. [7], additional systematic reviews were performed by Cui et al. [8] and Østergaard et al. [9]. Cui et al. [8] focused their research on the safety of plaster splints compared with traditional small splints, such as wood chips, bamboo chips, or bark [10]. However, these authors also reported that plaster splints are more effective than traditional small splints when the intervention period is shortened (4 weeks compared with less than 4 weeks) [8]. Østergaard et al. [9] studied the benefits and harms of early mobilization after conservatively treating a patient with a DRF, reporting that no evidence supported the superiority of early or delayed mobilization, although the authors remark that longer immobilization may lead to physical inactivity [9].
According to the Dutch guideline for DRFs, primarily non-dislocated DRFs are immobilized for 3 weeks, and reduced DRFs are immobilized for 4 to 5 weeks [5]. There are several studies showing that a plaster cast treatment for a stable and non- or minimally displaced DRF for 1 week is safe and effective [7, 11, 12]. Furthermore, several studies conclude that immobilization of 1 to 3 weeks of plaster is preferred by patients. A feasibility trial from Boersma et al. [13] shows no significant difference in pain, functional outcome, or patient satisfaction between short and long immobilization in non-reduced DRFs, and no difference in occurrence of secondary displacement was found between the intervention and control groups [13].
The aim of this systematic review was to investigate the optimal duration of immobilization for the conservative treatment of DRFs in adults. To investigate whether the duration of immobilization can be safely shortened, special attention will be paid to articles that have not yet been featured in any systematic review regarding this topic. A distinction must be made for the duration of immobilization between the non-reduced and reduced DRF conservative treatments.
Methods
Protocol and registration
This systematic review was performed and reported according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [14]. The registration number in the International Prospective Registration of Systematic Reviews (PROSPERO) is CRD42023417924.
Search strategy
A comprehensive literature search for studies comparing the duration of the conservative treatment of patients with DRFs was performed on January 24th, 2023. The searches were conducted using PubMed, Embase, CINAHL, Cochrane Library, and Web of Science. Index terms were determined for the literature search, and included Medical Subject Headings (MeSH) and closely related words. The following MeSH terms were used: “Radius Fractures,” “Wrist Fractures, “Conservative Treatment,” “Casts Surgical,” and “Splints.” No language or time restrictions were incorporated into the search. Other sources involved the manual screening of reference lists of randomized clinical trials, review articles, and systematic reviews. The Clinical Trial Register was checked for unpublished articles, and their authors were asked to give an update regarding their results. For a full search strategy, see Supplementary 1.
Study selection
The studies retrieved from the searches were imported into Rayyan for Intelligent Systematic Review [15]. After dataset de-duplication, two reviewers (M.B. and L.G.) independently performed title and abstract screening to determine whether each study should be included in this review. Disagreements between the two authors were discussed, and a third reviewer (L.S.) was involved if consensus could not be reached.
Eligibility criteria
All studies, randomized controlled trials (RCT) and otherwise, investigating the duration of conservative treatment for patients with DRFs were eligible for inclusion. The exclusion criteria consisted of (1) studies investigating the operative treatment of patients with DRFs, (2) pediatric patients (age < 18 years), (3) veterinarian studies, (4) the absence of the full text, and (5) case reports, editorials, conference abstracts, and letters to the editor. Studies in languages other than English, Dutch, or German were translated to review the abstracts for eligibility.
Quality assessment
The included articles were assessed for their quality by two reviewers (M.B. and L.G.). The Cochrane Risk of Bias tool 2 (RoB2) was used to assess the risk of bias based on five domains: (1) randomization process, (2) deviations from intended interventions, (3) missing outcome data, (4) measurement of the outcome, and (5) selection of the reported result. The risk of bias was rated as low, some concerns, or high [16]. The Grading of Recommendations Assessment, Development and Evaluation (GRADE) was used to assess the quality of evidence, which was rated as very low, low, moderate, or high [17].
Data extraction
Data extraction was performed independently by two reviewers with the use of a predefined data extraction form. The following characteristics were extracted from the included studies: author, year of publication, study design, number of included patients, follow-up period, non-operative immobilization treatment, reduction or none performed, duration of treatment, and outcome measurements (including wrist function, grip strength, range of motion, pain scores, and radiological outcome).
Analyzed outcome measurements from included articles
Patient-reported outcome measurements
The PROMs were evaluated with the Patient Rated Wrist Evaluation (PRWE); Disabilities of the Arm, Shoulder and Hand (DASH); Gartland and Werley; de Bruijn and the de Bruijn modified, Cooney, Patient-reported Outcome Measurement Information System Pain Interference (PROMIS-PI); and the Mayo Wrist score tools. The PRWE consists of three subscales: pain, function, and cosmetic. Participants are asked to respond to all items using a scale ranging from 0 to 10, with a total score of 100 [18]. The DASH and quick DASH (qDASH) tools assess the functional outcome of the upper extremity on a 5-point scale with 30- or 11-item questionnaires, respectively. Higher overall outcomes on the PRWE and (q-)DASH questionnaires represent a worse functional outcome [19]. The Gartland and Werly score combines subjective and objective items evaluating the wrist and hand function; here, a lower score represents a better functional outcome [20]. The de Bruijn and the modified de Bruijn scoring lists by Christersson et al. [21] evaluate functional outcome; again, a lower outcome represents a better wrist function [22]. The Cooney score assesses the domain’s pain, function, range of motion, and grip strength, with a total score of 100 points. In this score, a higher outcome over all domains represents a better functional outcome [21, 23]. The PROMIS-PI measures the extent to which pain limits a patient’s ability to engage in physical, mental, and social activities, with a lower overall outcome representing less pain interference [24]. Finally, the Mayo Wrist Score represents pain during the active motion of the injured wrist compared to the contralateral wrist and indicates the possibility of resuming daily activities; it is measured on a scale from 0 to 100, where a higher overall outcome represents a better wrist function [25].
Pain scores
Pain scores were either measured using a visual analog scale (VAS) or as a percentage of normal and mild pain.
Grip strength
Grip strength was measured using hand-grip dynamometry. It was expressed as mean grip strength of the injured limb and grip strength of the injured limb as a percentage of the contralateral wrist.
Range of motion
Range of motion was measured by joint extension, flexion, and deviation. It was expressed as degrees of motion, forearm rotation, mean range of motion, mean deviations of the injured wrist expressed as percentages of the uninjured wrist, and as the sum of flexion, extension, and radial and ulnar deviation.
Radiological outcome
Radiological outcome was measured using the Lidström criteria. The results were presented as excellent, good, fair, or poor based on anatomical outcomes expressed as percentages [26]. Measurements of radial and volar angulation in degrees, radial length, and shortening in millimeters were used to determine anatomical differences during treatment.
Statistical analysis
The data were collected and analyzed using the Review Manager software (version 5.3). The protocol and study population were investigated to determine clinical homogeneity. Statistical homogeneity was determined by the use of I2 tests, with values less than 40% considered homogeneous [27]. Funnel plots were generated using Review Manager to determine the publication bias [28].
Results
Study selection
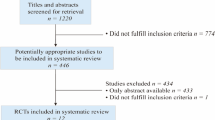
The initial literature search resulted in 11.981 articles. After de-duplication, 5.843 articles were screened for title and abstract, leaving 188 articles to be screened as full texts; however, the full texts of 90 studies were unavailable. Background articles, encompassing a total of 50 studies, which reviewed current treatment approaches, emerging trends in treatment management, or provided background information for DRFs were excluded. A further 32 studies were excluded because they used the wrong study design or study population for this review, mainly focusing on comparisons between the duration of immobilization of surgical treatment and nonsurgical treatment. A total of 16 articles were included in this systematic review (see Fig. 1).
Study characteristics
In total, 1118 patients were included (male/female/unknown gender: 205/860/53). All of the included studies investigated the duration of immobilization of patients with DRFs. One study compared bandages, with an unknown duration of immobilization, with cast immobilization for 5 weeks [29]. Another study retrospectively investigated immobilization of less or more than 6 weeks and was therefore included [30]. All other studies compared the differences between two groups, both of which were treated with less than 6 weeks of immobilization. Groups were divided into either shorter immobilization (< 3 weeks) or longer immobilization (> 3 weeks) periods. An overview of the selected articles, study characteristics, and preferred duration of immobilization concluded by the author is provided in Fig. 2.
Overview of the included articles representing the investigated duration of immobilization within each study. The outer limits of the immobilization durations are marked with black dots. The preferred duration of immobilization according to the authors’ conclusions is marked green. Gray boxes represent unfavorable duration of immobilization. The use of only bandage as a treatment is marked as a striped rounded box. An unknown immobilization duration is presented in red. Abbreviations: ND non- or minimally displaced, DR displaced and reduced, OR operation, RC retrospective cohort, W weeks, * = additional immobilization is given after the removal of the cast
Patient-reported outcome measurements—function
PROMs were reported in 10 studies [11, 13, 21, 22, 29, 31,32,33,34,35]. Four studies showed significantly better functional outcomes for the shorter rather than longer immobilization group in terms of the Gartland and Werley score, PRWE, qDASH, and PROMIS PI [13, 22, 31, 32]. Only one study showed that the longer immobilization group had a significantly better outcome in the Gartland and Werley score at the time of cast removal [11]. All other studies showed no significant differences (see Table 1).
Pain
Pain was described in ten studies, mostly expressed as VAS or as a percentage of normal and mild pain [13, 21, 29,30,31,32,33,34, 36, 37]. Two studies showed a significantly better outcome in the shorter immobilization group [33, 36]. Although not significantly different, most studies with a short immobilization duration showed lower pain scores, except in one study for which a better outcome was reported in the longer immobilization group (see Table 2) [21].
Grip strength
Grip strength was described in nine studies [21, 29, 30, 32, 33, 36,37,38,39]. Four studies showed a significantly better outcome in the shorter immobilization group [29, 33, 36, 38]. Only one study reported a significantly better grip strength in the group with a longer (6 weeks) immobilization [39]. All other studies showed no significant differences (see Table 3).
Range of motion
Range of motion was described in eight studies [21, 29, 30, 33, 36,37,38,39]. Four studies showed a significantly better outcome in the shorter immobilization group [21, 33, 36, 38]. One study reported a better range of motion when given prolonged immobilization [39]. No significant differences were shown in the other studies (see Table 4).
Radiological outcome
Radiological outcome was described in 10 studies [11, 22, 29, 31, 33, 34, 36,37,38, 40]. Three studies reported a significantly better outcome for patients treated with a longer immobilization for displaced and reduced DRFs [22, 34, 38]. Only one study showed a significantly better outcome on the Lidström criteria if a shorter immobilization was performed [36]. All other studies showed no significant differences (see Table 5).
Risk of bias
All studies were assessed with the Cochrane Risk of Bias Tool 2 (RoB2). Two studies were assessed as low risk [13, 31], while 11 studies were assessed to present some concerns [7, 21, 22, 29, 32,33,34, 36,37,38,39]. Three studies were considered to have a high risk of bias [30, 35, 40] (see Fig. 3).
Level of evidence
All studies were assessed with GRADEpro to qualify the level of evidence [17]. A total of 15 studies were qualified as level II evidence [7, 13, 21, 22, 29, 31,32,33,34,35,36,37,38,39,40], and one study was qualified as level I evidence [30] (see Fig. 3).
Discussion
This systematic review summarized and analyzed the optimal duration of immobilization for the conservative treatment of patients with DRFs. The main finding to emerge from the analysis is that 14 of the 16 included studies reported the possible benefit of a shorter immobilization period. The authors concluded that shorter immobilization resulted in the early recovery of range of motion and improved grip strength without increasing discomfort, but did not worsen anatomical outcome and were clinically equivalent to longer immobilization. The recovery of patients with a non- or minimally displaced fracture was favorable when treated with 3 weeks or less of immobilization [11, 13, 22, 29, 32,33,34,35,36,37,38, 40]. The immobilization of displaced and reduced DRFs can be shortened a minimum of 4 weeks. Two studies did not support a shorter immobilization due to treatment failure, reporting better outcomes in their longer immobilization groups, both of which included displaced and reduced DRFs. One study investigated immobilizations of 10 days and 4 weeks, while the other study compared immobilizations of 4 and 6 weeks [21, 39].
The last comprehensive systematic review was performed in 2018 by van Delft et al. [7] and concluded that the period of immobilization for all DRFs should be considered to be shortened to a maximum of 3 weeks [7]. Since 2018, another four studies investigated the duration of immobilization for conservatively treated DRFs [13, 30, 34, 39]. Functional outcome, pain, range of motion, radiological outcomes, and grip strength were the most commonly used outcome measurements. Across all the included studies in this review, these outcome measurements differ in terms of outcome values. Standard deviations and interquartile ranges were often not reported. In addition, studies pooled outcome values for the non- and minimally displaced and displaced DRFs [22, 29, 30, 33, 37, 38]. The finding of this systematic review confirms the conclusion of the last systematic review performed, that there is a lack of clear homogeneous studies and a need for these studies in future research. The present systematic review included four new studies, of which three showed beneficial outcomes using shorter immobilization. Three of the recent studies also had a better risk of bias than the previous studies. This shows that the overall consensus from recent studies leans more towards the use of shorter immobilization for the conservative treatment of patients with DRFs. Due to the heterogeneity of study designs, a meta-analysis could not be performed.
Christersson et al. [21] investigated whether 10 days of immobilization was sufficient for the treatment of patients with reduced DRFs. No significant difference was observed in pain scores or grip strength, but there was a significantly better outcome in range of motion for the longer immobilization group. Furthermore, the treatment with shorter immobilization failed in three patients. One patient received a cast immobilization for another 3 weeks, while two patients were treated surgically due to secondary dislocation. It was concluded that 10 days of immobilization after the reduction of a DRF is not safe and causes more complications [21]. One must be aware that only displaced DRFs that needed fracture reduction were included in this study. This contributes to previous findings that displaced and reduced DRFs cannot be immobilized safely for less than 4 weeks. Distinctions should therefore be made between the non- and minimally displaced fractures in comparison with displaced fractures for the conservative treatment of patients with DRFs.
Olech et al. [34, 39] investigated the duration of immobilization used to treat displaced and reduced DRFs in the elderly population in two studies. The first study (2021) showed a better recovery of muscle strength and range of motion in the group that underwent 6 weeks compared to 4 weeks of immobilization, and the authors concluded that a more intensive rehabilitation process is preferred [39]. The second study (2022) of the same study population explored pain scores and the Mayo wrist function score after 4 weeks of immobilization, concluding that immobilization can be reduced to 4 weeks for conservative DRF treatment [34]. As mentioned by the AAOS, operative treatments of DRFs in the elderly do not lead to functional differences in PROMs compared with conservative treatments [6]. When better functional outcomes can be obtained with shorter immobilization in the elderly, as concluded by Olech et al. (2022), one must consider this the optimal treatment for this specific group of patients.
Boersma et al. [41] investigated 1 week of immobilization in comparison with 4 to 5 weeks, with a total of 40 patients. They found no significant differences in pain between the two groups, while the shorter immobilization led to better functional outcomes after 6 weeks and an overall better patient satisfaction [13]. This feasibility study led to the Cast-OFF 2 study, in which a multicenter randomized controlled trial with a stepped wedge design was used to implement one week of immobilization for the non- or minimally displaced DRFs. This study should provide more evidence from a homogeneous population [41].
One retrospective study by Khashab et al. [30] was included as they investigated the duration of immobilization during the DRF treatments. Non- or minimally displaced, displaced and reduced, or surgically treated DRFs were included and pooled, but no distinction was made between the conservative and surgically treated DRFs. According to Khashab, decreased grip strength and higher pain scores were observed if the immobilization exceeded more than 6 weeks. The duration of prolonged immobilization and the kind of treatment the patients received was unclear however [30]. Furthermore, it should be noted that, due to the retrospective design of this study, the risk of bias was assessed as high, based on the domain of randomization and measurement of the outcome. The RoB2 tool was designed for randomized trials, and this study shows limitations in assessing retrospective studies for this systematic review.
The benefits of early mobilization were not only observed after the conservative treatment of DRFs; rather, this was also concluded after surgical DRF treatment in a systematic review performed by Deng et al. [42]. Nine randomized control trials were investigated to explore the differences between early and late mobilization, respectively after less than 2 weeks or more than 2 weeks of immobilization following the surgical treatment of patients with DRFs. Early mobilization showed better functional outcomes at earlier post-operative stages and similar clinical outcomes during long-term follow-up; however, it must be noted that early mobilization had a higher potential for osteosynthesis failure. It was concluded that early mobilization could be considered, although more research must be performed investigating the optimal rehabilitation protocol for surgically treated DRFs [42].
This systematic review had a few limitations. First, a comprehensive literature search was performed without restriction to screen all eligible studies. Potential language barriers, other than English, Dutch, or German, were translated to screen for eligibility. This could have led to missed inclusions, despite the article selection being performed by two individual reviewers. The full text was not available for a large proportion (48%) of the eligible articles, even after the help and in-depth searching of a librarian. This could have led to potential missed inclusions. Second, only 4 new eligible articles were included since the systematic review performed by van Delft et al. [7], of which 3 of these articles, assessed to have a lower risk of bias, provided more evidence in favor of shorter immobilizations. It was aimed to include more articles with homogeneous studies to perform a meta-analysis. Although these 4 articles mostly did report standard deviations or interquartile ranges, different outcome measurements were used [13, 30, 34, 39]. In combination with the heterogeneous studies from most of the older included articles, which were 20 years old or more, it was not possible to perform a meta-analysis. Third, it must be noted that not all authors conducted a minimal follow-up of 1 year; several studies had a shorter follow-up ranging from 7 weeks to 9 months [11, 29, 32, 40]. There is no established standard for fracture follow-up in clinical research, although a 1-year period is frequently utilized and recommended [43]. Assessments of outcomes at week 6, month 3, month 6, month 9, and month 12 can be crucial for evaluating complications, pain, and functionality. Studies with a follow-up duration of less than 1 year may yield short-term benefits, but may be unfavorable when evaluating long-term outcomes.
The results of this study indicate that the duration of immobilization for the conservative treatment of patients with DRFs is not widely investigated. Of the 16 studies included, ten were published more than 20 years ago. It was not until 2018 that several researchers started to reinvestigate this topic. Future research must be performed with homogeneous studies and outcome measurements to investigate the optimal duration of immobilization. Distinctions should be made between the conservative treatment of the non- or minimally displaced DRFs, and the displaced DRFs. Several studies have investigated this topic, although without published results yet [41, 44,45,46]. Hopefully, these and future studies will lead to a uniform protocol for the optimal duration of immobilization during the conservative treatment of DRFs.
Conclusion
This comprehensive systematic review showed the same or better outcome measurements of shorter immobilization for the non- or minimally displaced DRFs. The duration of immobilization for non- or minimally displaced DRFs can be considered to be shortened to 1 to 3 weeks. Displaced and reduced DRFs cannot be immobilized for less than 4 weeks as this results in more complications. Future large homogeneous randomized controlled trials should provide definitive evidence to reach a consensus on the optimal duration of immobilization.
Data availability
The data utilized for this systematic review is available upon reasonable request.
References
Testa G, Vescio A, Di Masi P, Bruno G, Sessa G, Pavone V. Comparison between surgical and conservative treatment for distal radius fractures in patients over 65 years. J Funct Morphol Kinesiol. 2019;4(2):26.
Yu GS, Lin YB, Le LS, Zhan MF, Jiang XX. Internal fixation vs conservative treatment for displaced distal radius fractures: a meta-analysis of randomized controlled trials. Ulus Travma Acil Cerrahi Derg. 2016;22(3):233–41.
Toon DH, Premchand RAX, Sim J, Vaikunthan R. Outcomes and financial implications of intra-articular distal radius fractures: a comparative study of open reduction internal fixation (ORIF) with volar locking plates versus nonoperative management. J Orthop Traumatol. 2017;18(3):229–34.
Mirarchi AJ, Nazir OF. Minimally invasive surgery: is there a role in distal radius fracture management? Curr Rev Musculoskelet Med. 2021;14(1):95–100.
NVVH. Richtlijnendatabase: Distale radiusfracturen 2021. [Available from: https://richtlijnendatabase.nl/richtlijn/fracturen_bij_kinderen/polsfracturen/behandeling_polsfracturen.html. Accessed 13 Feb 2023
Surgeons AAoO. Management of distal radius fractures evidence-based clinical practice guidelines 2020. Available from: www.aaos.org/drfcpg. Accessed 10 Jan 2023
van Delft EAK, Gelder TGV, Vries R, Vermeulen J, Bloemers FW. Duration of cast immobilization in distal radial fractures: a systematic review. J Wrist Surg. 2019;8(5):430–8.
Cui X, Liang L, Zhang H, Li Y, Cheng H, Liu G, et al. The effectiveness and safety of plaster splint and splints for distal radius fractures: a systematic review and meta-analysis of randomized controlled trials. Medicine (Baltimore). 2020;99(9):e19211.
Østergaard HK, Mechlenburg I, Launonen AP, Vestermark MT, Mattila VM, Ponkilainen VT. The benefits and harms of early mobilization and supervised exercise therapy after non-surgically treated proximal humerus or distal radius fracture: a systematic review and meta-analysis. Curr Rev Musculoskelet Med. 2021;14(2):107–29.
Wei L-Y, Zhang H-W, Dong D-H, Zuo J-Z, Li L, Wang G-Q, et al. Manual reduction with traditional small splints for distal radius fracture in older patients. J Acute Dis. 2021;10(2):78–82.
Jensen MR, Andersen KH, Jensen CH. Management of undisplaced or minimally displaced Colles’ fracture: one or three weeks of immobilization. J Orthop Sci. 1997;2(6):424–7.
Stoffelen D, Broos P. Minimally displaced distal radius fractures: do they need plaster treatment? J Trauma. 1998;44(3):503–5.
Boersma EZ, Hekma EJ, Kraaijvanger N, Mollen R, Nijhuis-van der Sanden MWG, Edwards MJR. Cast-OFF trial: one versus 4 to 5 weeks of plaster cast immobilization for nonreduced distal radius fractures: a randomized clinical feasibility trial. Hand (N Y). 2022;17(1_suppl):60s–9s.
Moher D, Liberati A, Tetzlaff J, Altman DG, The PG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7):e1000097.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210.
Sterne JAC, Savović J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction—GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94.
Kleinlugtenbelt YV, Krol RG, Bhandari M, Goslings JC, Poolman RW, Scholtes VAB. Are the patient-rated wrist evaluation (PRWE) and the disabilities of the arm, shoulder and hand (DASH) questionnaire used in distal radial fractures truly valid and reliable? Bone Joint Res. 2018;7(1):36–45.
Gummesson C, Atroshi I, Ekdahl C. The disabilities of the arm, shoulder and hand (DASH) outcome questionnaire: longitudinal construct validity and measuring self-rated health change after surgery. BMC Musculoskelet Disord. 2003;4:11.
Gartland JJJ, Werley CW. Evaluation of healed Colles’ fractures. JBJS. 1951;33(4):895–907.
Christersson A, Larsson S, Sandén B. Clinical outcome after plaster cast fixation for 10 days versus 1 month in reduced distal radius fractures: a prospective randomized study. Scand J Surg. 2018;107(1):82–90.
de Bruijn HP. Functional treatment of Colles fracture. Acta Orthop Scand Suppl. 1987;223:1–95.
Kwok IH, Leung F, Yuen G. Assessing results after distal radius fracture treatment: a comparison of objective and subjective tools. Geriatr Orthop Surg Rehabil. 2011;2(4):155–60.
Amtmann D, Cook KF, Jensen MP, Chen W-H, Choi S, Revicki D, et al. Development of a PROMIS item bank to measure pain interference. Pain. 2010;150(1):173–82.
Cooney WP, Bussey R, Dobyns JH, Linscheid RL. Difficult wrist fractures. Perilunate fracture-dislocations of the wrist. Clin Orthop Relat Res. 1987;214:136–47.
Lidström A. Fractures of the distal end of the radius: a clinical and statistical study of end results. Acta Orthop Scand. 1959;30(sup41):1–118.
Higgins, JPT, Green S. Cochrane Handbook for Systematic Reviews of Interventions (version 5.1.0): Identifying and measuring hetereogeneity. Chapter 9.5.2. Available from https://handbook-5-1.cochrane.org/chapter_9/9_5_2_identifying_and_measuring_heterogeneity.htm. Accessed 12 Jan 2023
Deeks JJ, Altman DG, Bradburn MJ. Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis, Chapter 15. Syst Rev Health Care 2001;285–312.
Dias JJ, Wray CC, Jones JM, Gregg PJ. The value of early mobilisation in the treatment of Colles’ fractures. J Bone Joint Surg Br. 1987;69(3):463–7.
Khashab M, Alem A, Almuatiri A, Rasheed F, Almehmadi M, Felemabn S, et al. Comparison of the effects of regular periods of immobilization and prolonged immobilization on hand function post distal radial fracture. Cureus. 2022;14(11):e30986.
Bentohami A, van Delft EAK, Vermeulen J, Sosef NL, de Korte N, Bijlsma TS, et al. Non- or minimally displaced distal radial fractures in adult patients: three weeks versus five weeks of cast immobilization-a randomized controlled trial. J Wrist Surg. 2019;8(1):43–8.
Davis TR, Buchanan JM. A controlled prospective study of early mobilization of minimally displaced fractures of the distal radial metaphysis. Injury. 1987;18(4):283–5.
McAuliffe TB, Hilliar KM, Coates CJ, Grange WJ. Early mobilisation of Colles’ fractures. A prospective trial. J Bone Joint Surg Br. 1987;69(5):727–9.
Olech J, Kopczyński B, Tomczyk Ł, Konieczny G, Kazubski K, Morasiewicz P. The functional and radiographic outcomes following distal radius fracture treatment in a cast for 4 and 6 weeks in the elderly: a randomized trial. Adv Clin Exp Med. 2022;31(6):701–6.
Stoffelen D, Broos P. Minimally displaced distal radius fractures: do they need plaster treatment? J Trauma. 1998;44(3):503–5.
Abbaszadegan H, Conradi P, Jonsson U. Fixation not needed for undisplaced Colles’ fracture. Acta Orthop Scand. 1989;60(1):60–2.
Vang Hansen F, Staunstrup H, Mikkelsen S. A comparison of 3 and 5 weeks immobilization for older type 1 and 2 Colles’ fractures. J Hand Surg Br. 1998;23(3):400–1.
Millett PJ, Rushton N. Early mobilization in the treatment of Colles’ fracture: a 3 year prospective study. Injury. 1995;26(10):671–5.
Olech J, Konieczny G, Tomczyk Ł, Morasiewicz P. A randomized trial assessing the muscle strength and range of motion in elderly patients following distal radius fractures treated with 4- and 6-week cast immobilization. J Clin Med. 2021;10(24):5774.
Christensen OM, Christiansen TG, Krasheninnikoff M, Hansen FF. Length of immobilisation after fractures of the distal radius. Int Orthop. 1995;19(1):26–9.
Boersma E, van de Krol E, Tromp T, van der Sanden MN, Edwards M. Cast OFF-2: 1 week of plaster cast immobilization for non-reduced distal radius fractures-a study protocol for an implementation study. Trials. 2021;22(1):936.
Deng Z, Wu J, Tang K, Shu H, Wang T, Li F, et al. In adults, early mobilization may be beneficial for distal radius fractures treated with open reduction and internal fixation: a systematic review and meta-analysis. J Orthop Surg Res. 2021;16(1):691.
Ricci WM, Black JC, Tornetta PI, Gardner MJ, McAndrew CM, Sanders RW. Current opinions on fracture follow-up: a survey of OTA members regarding standards of care and implications for clinical research. J Orthop Trauma. 2016;30(3):e100–5.
van Delft EAK, Bloemers FW, Sosef NL, Bonjer HJ, Schep NWL, Vermeulen J. Dislocated distal radial fractures in adult patients: 4 weeks versus 6 weeks of cast immobilisation following reduction, a multicentre randomised controlled trial, study protocol. BMJ Open. 2019;9(3):e026540.
Hospital CU. Distal radial fractures in adult patients: 4 weeks versus 6 weeks of cast immobilisation following closed reduction. 2021. https://ClinicalTrials.gov/show/NCT05012345. Accessed 8 Mar 2023
Mar PdS. Four or six weeks of immobilization in the conservative treatment of distal radius fractures in elderly population? 2021. https://ClinicalTrials.gov/show/NCT05370365. Accessed 8 Mar 2023
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
This study was a systematic review and therefore did not involve patients, for which the involvement of an ethical review committee would be required.
Competing interests
The authors declare no competing interests.
Systematic review registration number
Prospero CRD42023417924.
Additional information
Note: The study was performed at the Radboud University Medical Center, Nijmegen, The Netherlands.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
de Bruijn, M.A.N., van Ginkel, L.A., Boersma, E.Z. et al. Cast immobilization duration for distal radius fractures, a systematic review. Eur J Trauma Emerg Surg (2024). https://doi.org/10.1007/s00068-024-02494-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00068-024-02494-y